Abstract
Background
Despite the plethora of pharmacotherapy and acquisition of new AEDs, there is a hard core of patients who persistently fail to respond to optimal treatment and continue to suffer from refractory seizures. We aimed to study the prevalence and risk factors for development of drug-resistant epilepsy (DRE). All adult patients with epilepsy (PWE) who attended the epilepsy outpatient clinic and were maintained on at least two anti-epileptic drugs (AEDs) were profiled for drug response in accordance with the International League against Epilepsy (ILAE) 2010 consensus definition for DRE. Data collected included demographics, detailed history of seizures, medications history, past medical and psychiatric history, electroencephalogram, and brain imaging findings.
Results
The prevalence rate of DRE was 21.3% in the study population. Significant variables on univariate analysis were the following: male gender (OR: 5.409, CI 1.661–17.617, p < 0.005), presence of GTC (OR: 4.187, CI 1.304–13.445, p < 0.016), no change in frequency after AEDs use (OR: 4.465, CI 1.211–16.468, p < 0.025), bad response to first AEDs (OR: 9.000, CI 2.437–33.244, p < 0.001), presence of developmental delay (OR: 10.612, CI 1.347–83.589, p < 0.025), presence of abnormal neurological examination (OR: 4.227, CI 1.145–15.601, p < 0.030), generalized epilepsy (OR: 3.886, CI 1.141–13.233, p < 0.030), presence of structural etiology (OR: 3.467, CI 1.152–10.431, p < 0.027), abnormal EEG findings (OR: 3.467, CI 1.152–10.431, p < 0.027), presence of focal activity in EEG (OR: 5.344, CI 1.155–24.713, p < 0.032), and abnormal imaging findings (OR: 3.524, CI 1.083–11.473, p < 0.036). In the logistic regression analysis, two variables were statistically significant: bad response to the first AED and no change in seizure frequencies with treatment. Our study showed that older age at seizure onset was a protective factor for DRE.
Conclusions
The current study suggests that significant risk factors for DRE are younger age at epilepsy onset, poor response to first AED and lack of change in seizure frequencies after adjusting treatment.
Similar content being viewed by others
Background
According to the World Health Organization, epilepsy is considered as one of the most common neurological diseases worldwide [1]. In the recently published report on the global burden of epilepsy, number of patients with active epilepsy was around 45.9 million globally [2] and about 4.6 million develops the condition each year [3]. Nearly, 80% of those with epilepsy live in low- and middle-income countries (LMIC), where epilepsy prevalence and incidence rates are higher than in high-income countries (HIC) [4].
Despite the plethora of pharmacotherapy and acquisition of new AEDs, there is a hard core of patients who persistently fail to respond to optimal treatment and continue to suffer from refractory seizures [5]. They are classified as having drug-resistant epilepsy, a diagnosis with adverse prognostic implications [6].
Various terms have been used to describe this form of epilepsy in the literature, such as intractable, refractory, or pharmacoresistant. This inconsistency in definitions represented a major obstacle in DRE research; therefore, a unified definition was needed [7]. In 2010, the ILAE published a consensus definition of DRE as failure of adequate trials of 2 tolerated, appropriately chosen, and used AED schedules (whether as monotherapies or in combination) to achieve sustained seizure freedom for 12 months, or 3 times the inter-seizure interval before treatment started whichever is longer [8].
Limited data are available about the proportion of patients with DRE among the Egyptian population. Moreover, the predictors of response to epilepsy treatment are very diverse in different populations. Therefore, having hospital-based data are of paramount importance not only to establish predictive factors of DRE but also to help steering the treatment pathway of high-risk patients toward more individualized and specialized interventions [9, 10].
Therefore, we conducted this study to identify the prevalence of patients with DRE and to determine the predictors of intractability.
Methods
This was a cross-sectional cohort study. We included patients older than 18 years of age who were diagnosed with epilepsy and was taking at least two AED at the time of evaluation. These patients were recruited from the university outpatient clinics.
Ethical approval was obtained from the University ethical committee (EC) which operates according to the International Conference of Harmonization Good Clinical Practice (ICH GCP) and applicable local and institutional regulations and guidelines [11]. Date of the approval 17\9\2020 serial number 0106524.
A written informed consent was obtained from all subjects prior to recruitment to the study.
The diagnosis of DRE was determined according to the ILAE criteria [5] and the patients were categorized into three groups: drug-responsive, drug-resistant, and undefined.
An interview questionnaire was used to gather the data from each patient and the following data were obtained: individual demographics (age, gender, education level, employment, marital status, smoking), Seizure history (age at onset, seizure type, initial seizure frequency, age at diagnosis and years of evolution, presence of neonatal seizures, febrile seizures, status epilepticus, frequency of seizures at the time of evaluation, maximum period of seizure freedom), history of AED use (duration between onset of seizures and start of treatment, anti-epileptic drugs used, dose, frequency, response, adverse effects, add on treatment, interval between each subsequent drug added and change in frequency after each drug added), Family history of epilepsy or consanguinity, history of developmental delay, medical and surgical history, comorbid psychiatric conditions, Information regarding the etiology of epilepsy including any history of CNS infections, head trauma, cerebrovascular disease, cerebral neoplasm malignant or benign, CNS operations, perinatal insults (pregnancy complications, asphyxia during birth, or neonatal hypoxia), Epilepsy syndromes categorized according to ILAE classification and reported as genetic, structural–metabolic, and unknown, all relevant investigations including EEG for all patients, Imaging (CT or MRI) when structural epilepsy was suspected, IQ testing and serum level of anti-epileptic drugs if non-compliance or toxicity was suspected. A complete neurological examination was performed for each patient.
Descriptive statistics were used to assess distribution and frequencies. Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Qualitative data were described using number and percentage. The Kolmogorov–Smirnov test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, standard deviation, median and interquartile range (IQR). Afterward, a logistic regression analysis with drug resistance as dependent variable (drug-resistant versus drug-responsive) was calculated. The significance of the obtained results was judged at the 5% level.
Results
Total number of 352 adult patients with epilepsy were identified during the study period and 34% of these patients (n = 120/352) patients were classified as undefined (insufficient history regarding compliance to medication and seizure frequency) and excluded from the analysis, 142 (40.3%) were drug-responsive, and 90 (25.5%) were drug-resistant.
Table 1 shows the demographic data of the study group. The drug-resistant group consisted of 46 males (51.1%) and 44 females (48.9%). The mean age (in years) was 34.52 ± 13.65. The mean age at onset of epilepsy in the drug-resistant group was significantly lower than the drug-responsive group 13.71 ± 12.92 versus 21.20 ± 12.32, respectively, p < 0.001*.
Initial seizure frequency was significantly higher in the DRE group p = 0.003 *as shown in Table 2.
28.9% presented with status epileptics in the DRE in comparison with only 12% in the drug-responsive group and this was statistically significant p = 0.001*as shown in Table 3.
Abnormal EEG finding were among 71.1% in the DRE group, and this was statistically significant < 0.001*, focal seizures was more prevalent among drug-resistant group than drug-responsive group and this was statistically significant p = 0.028* (Table 4).
The most common manifested seizure type was focal to bilateral tonic–clonic (61.1%). 33 (36.7%) DRE patients and 42 (29.6%) drug-responsive patients had a history of previous neurological insults. In the subgroup analysis, perinatal insults were the most common cause in the DRE group.
The most common etiology of epilepsy was structural–metabolic in the DRE group 53 (58.9%), and 42 (43.8%) in the drug-responsive group (Table 5).
Failure to respond to the first AED was significantly higher in the DRE group compared to the drug-responsive group (60% versus 35.9%) p < 0.001* (Table 6).
Neuroimaging was done in all patients in the DRE group and in 105 patients of the drug-responsive group. 35 (38.9%) DRE patients and 44 (41.9%) drug-responsive patients had abnormal findings. Encephalomalacia was the most common abnormal finding in both groups.
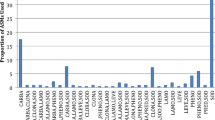
Eighty patients (83.3%) started AED treatment with the onset of seizures or shortly afterward, while the use of AED was delayed in 16 (16.7%) patients. Sodium valproate was the first AED prescribed to 42 patients (43.8%), followed by carbamazepine in 34 (35.4) and levetiracetam in 16 (16.7). The second most common AED prescribed was carbamazepine then levetiracetam, and sodium valproate.
The most common combinations of drugs were carbamazepine + sodium valproate, carbamazepine + levetiracetam, and sodium valproate + levetiracetam. Change in the seizure frequencies after add-on treatment was observed in 38 (39.5%) who achieved lower frequency, while 58 (60.41%) did not achieve significant change in their frequencies after added treatment.
Regarding univariate analysis of risk factors for DRE. Table 7 shows that from the initial univariate analysis, several variables were found to be significantly associated with developing DRE, these include Age (OR: 0.974, CI 0.955–0.993, p < 0.007), Age of onset (< 10 years) (OR: 4.022, CI 2.152–7.517, p < 0.001). Initial frequency (daily/weekly) (OR: 2.277, CI (1.316–3.941), p < 0.003). Maximum seizure-free period (< 1 year) (OR: 5.501, CI (2.355–12.851), p < 0.001). History of Status epilepticus (OR: 2.987, CI (1.511–5.905), p < 0.002). Bad response to the first AED (OR: 2.676, CI (1.554–4.609), p < 0.001). Structural etiology (OR: 1.848, CI (1.082–3.156), p < 0.024). Abnormal EEG (OR: 3.364, CI (1.913–5.916), p < 0.001).
Regarding multivariate analysis, Table 7 shows that the variables that showed significant association with DRE in the univariate analysis were entered into the multivariate analysis. Only two variables remained significantly associated with DRE: bad response to the first anti-epileptic drug (OR: 4.366, CI (1.111–17.155), p < 0.035) and less than 1-year maximum seizure-free period (OR: 26.738, CI (7.374–96.951), p < 0.001). Further data can be provided upon request.
Discussion
In the current study, the prevalence of DRE was 21.3% of the study population. The percentage was similar to that reported by previous cohort studies conducted in referral centers by Kong and colleagues and by Espinosa and colleagues (both used ILAE DRE definition) in which the prevalence was 21.5% and 27.1%, respectively [12, 13].
It was also congruent to the rate of intractable seizures in a Glasgow study (25%) and a French study (prevalence ranged from 15.6% to 22.5%) [14, 15].
However, it was significantly higher than that reported in a previous community-based study in Egypt by Farghaly and colleagues, in which the prevalence of definite intractable patients was 11.4% [16]. This discrepancy can be explained by the difference in the study setting (clinic-based versus population/community-based) with a strong selection bias in clinic-based studies resulting in higher prevalence rates, especially that patients with more severe and poorly controlled epilepsy are more likely to be followed in specialized centers [17].
Previous studies have reported a slight predominance of epilepsy in males compared to females [18]. In our study, there was slight female predominance; however, male gender was found to be a risk factor for DRE in the univariate analysis but did not remain significant in the multivariate analysis. This result was similar to the findings of Farghaly and colleagues and Chentouf and colleagues [19].
In our study, older age was less associated with DRE, and it remained a significant protective factor in the multivariate analysis. This finding comes in agreement with the existing evidence showing that elderly patients have a lower risk for DRE compared to younger patients and seizure control can often be achieved with lower doses of AEDs in this age group [20, 21].
It is known that the duration of epilepsy has an impact on disease severity. In our study, patients with DRE had 4 years more of evolution in average compared to those without DRE. Similar findings were reported by a study of drug-resistant focal epilepsy (DRE group had 6 years more of evolution) [22] and in another study on patients with generalized epilepsy, where patients with DRE had more years of evolution (24.1 versus 14.7) [23].
Age of epilepsy onset has been suggested to be a major predictor of pharmacoresistance. Multiple studies showed that DRE was associated with younger age at the onset especially in the first year of life [24,25,26]. In our study, age at onset of epilepsy was significantly associated with DRE only in the univariate analysis with marginally negative influence (odds ratio = 0.94).
In this study, the etiology of epilepsy was a significant factor affecting the prognosis. Structural/metabolic etiology was identified in 52% of the intractable group compared to 23% of the controlled group. Moreover, this study demonstrated that the presence of neurological deficit and abnormal imaging findings were associated with DRE. These findings coincide with the results of a systemic review by Sultana and colleagues which found that the most frequent reported correlates and predictors of DRE included symptomatic epilepsy and having a neurological deficit [17].
On the other hand, presumed idiopathic/genetic etiology is classically considered as a relatively benign condition and has been previously reported as a protective factor that decreases the risk for DRE [27]. Furthermore, according to a retrospective study by Jiyang and colleagues, idiopathic etiology was not associated with poor outcome on both short-term and long-term prognosis in newly diagnosed patients [28]; similarly, in the current work, idiopathic/genetic etiology was a protective factor against intractability (OR: 0.322, CI 0.117–0.888, p 0.028).
The relation between seizure type and intractability has been inconsistent in previous studies, some showing an increased risk in patients with focal epilepsy [17], whereas others have found a relation between DRE and multiple seizure types [29]. In our study, 89% of the intractable group had generalized seizures and this was significantly associated with DRE, as demonstrated by both univariate and logistic regression analysis.
In the current study, intractable cases had higher initial seizure frequencies (10.7% had daily seizures and 34.7% had weekly seizures), and in the univariate analysis, this was significantly associated with drug resistance. These findings come in agreement with Tripathy et.al and Farghaly et.al who found a similar significant association between initial seizure frequency and intractability [29, 30].
Several studies found a relationship between status epilepticus and intractability. These results were consistent for both adults and children [30]. It could be explained in a bidirectional effect as on one hand, intractability leads to more seizures, SE, therefore, more brain damage and on the other hand, SE especially if prolonged leads to neuronal death, epileptogensis and further intractability. However, in the current study, SE was not a predictive factor for DRE. This finding comes in agreement with Tellez-Zenteno and colleagues who found no association [31].
In a systemic review by Xue ping and colleagues in 2019, EEG abnormality (including slow wave and epileptiform discharge) was reported to be a predictor for intractability [17, 29].
In the current study, there was an association between abnormal EEG findings and DRE in the univariate analysis and when EEG abnormalities were analyzed separately, only focal epileptic activity was a predictive factor for DRE and this comes in line with the aforementioned risk factors and points toward the idea that a structural/metabolic etiology of epilepsy especially when it results in neurological or electrophysiological abnormities is predictive of a more severe course of epilepsy [17].
In the current study, the diagnosis of epilepsy and start of treatment were delayed in a minority of cases and this delay was not associated with increased risk of DRE. This comes in concordance with a study by Parviainen and colleagues, who assessed the diagnostic delay in a cohort of newly diagnosed patients with focal epilepsy, and found no statistically significant association between the diagnostic delay and poor prognosis [32].
Failure of response to the first AED is a powerful prognostic factors influencing subsequent evolution and appearance of pharmacoresistance [33]. Kwan and Brodie reported that among patients who failed to respond to the first drug; only 11% of such patients subsequently became seizure-free compared to 40–55% of those who fail due to side effects. Furthermore, only 13% responded to the second AED and only 3% became seizure-free with two drugs [8].
In the current work, 60% of the intractable group failed to respond to the first AED and about 43% did not achieve lower seizures frequency with subsequent drugs. Both factors were predictors of DRE in the univariate analysis; however, no change in seizures frequency with add-on treatment remained statistically significant in the multivariate analysis.
Prescence of developmental delay is one of the most reported predictive factors for DRE in the pediatric population [34]. Some studies have shown that developmental delay is a common co-morbidity in patients with epilepsy compared to the general population [7, 35]. Similar to previous studies in adult patients, developmental delay has been significantly associated with DRE in the current work [23, 36].
Several other clinical variables have been associated with pharmacoresistance in the literature, such as family history of epilepsy, febrile seizures in infancy and psychiatric comorbidities [22]. The current work did not identify a statistically significant association between these factors and DRE.
Conclusion
The current study suggests that significant risk factors for DRE are younger age at epilepsy onset, poor response to first AED and lack of change in seizure frequencies after adjusting treatment.
Availability of data and materials
The research data supporting the results reported in the article are totally available upon request from the authors.
Abbreviations
- PWE:
-
Patients with epilepsy
- AED:
-
Antiepileptic drugs
- DRE:
-
Drug-resistant epilepsy
- EEG:
-
Electro encephalography
- ILAE:
-
International League against Epilepsy
- GTC:
-
Generalized tonic–clonic convulsions.
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- LMIC:
-
Low- and middle-income countries
- HIC:
-
High-income countries
- CNS:
-
Central nervous system
- CT:
-
Computed tomography
- MRI:
-
Magnetic reasoning imaging
- IQ:
-
Intelligence quotient
- IQR:
-
Interquartile range
References
Organization WHO. Global status report on alcohol and health 2018: World Health Organization; 2019.
Beghi E, Giussani G, Nichols E, Abd-Allah F, Abdela J, Abdelalim A, et al. Global, regional, and national burden of epilepsy, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(4):357–75.
Fiest KM, Sauro KM, Wiebe S, Patten SB, Kwon C-S, Dykeman J, et al. Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies. Neurology. 2017;88(3):296–303.
Espinosa-Jovel C, Toledano R, Aledo-Serrano Á, García-Morales I, Gil-Nagel A. Epidemiological profile of epilepsy in low income populations. Seizure. 2018;56:67–72.
Chen Z, Brodie MJ, Liew D, Kwan P. Treatment outcomes in patients with newly diagnosed epilepsy treated with established and new antiepileptic drugs: a 30-year longitudinal cohort study. JAMA Neurol. 2018;75(3):279–86.
Tomson T, Beghi E, Sundqvist A, Johannessen SI. Medical risks in epilepsy: a review with focus on physical injuries, mortality, traffic accidents and their prevention. Epilepsy Res. 2004;60(1):1–16.
Téllez-Zenteno JF, Hernández-Ronquillo L, Buckley S, Zahagun R, Rizvi S. A validation of the new definition of drug-resistant epilepsy by the International League Against Epilepsy. Epilepsia. 2014;55(6):829–34.
Kwan P, Arzimanoglou A, Berg AT, Brodie MJ, Allen Hauser W, Mathern G, et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Wiley Online Library; 2010.
Gidey K, Chelkeba L, Gemechu TD, Daba FB. Treatment response and predictors in patients with newly diagnosed epilepsy in Ethiopia: a retrospective cohort study. Sci Rep. 2019;9(1):1–7.
Löscher W, Potschka H, Sisodiya SM, Vezzani A. Drug resistance in epilepsy: clinical impact, potential mechanisms, and new innovative treatment options. Pharmacol Rev. 2020;72(3):606–38.
. ICH GCP. ICH GCP (Good Clinical Practice) Training Course. Published 2011. https://ichgcp.net/. Accessed 4 Apr 2020.
Kong ST, Ho CS, Ho PC, Lim S-H. Prevalence of drug resistant epilepsy in adults with epilepsy attending a neurology clinic of a tertiary referral hospital in Singapore. Epilepsy Res. 2014;108(7):1253–62.
Jovel CAE, Salazar SR, Rodríguez CR, Mejía FES. Factors associated with quality of life in a low-income population with epilepsy. Epilepsy Res. 2016;127:168–74.
Brodie MJ. Road to refractory epilepsy: the Glasgow story. Epilepsia. 2013;54:5–8.
Picot MC, Baldy-Moulinier M, Daurès JP, Dujols P, Crespel A. The prevalence of epilepsy and pharmacoresistant epilepsy in adults: a population-based study in a Western European country. Epilepsia. 2008;49(7):1230–8.
Farghaly WM, El-Tallawy HN, Rageh TA, Mohamed EM, Metwally NA, Shehata GA, et al. Epidemiology of uncontrolled epilepsy in the Al-Kharga District, New Valley, Egypt. Seizure. 2013;22(8):611–6.
Sultana B, Panzini M-A, Carpentier AV, Comtois J, Rioux B, Gore G, et al. Incidence and prevalence of drug-resistant epilepsy: a systematic review and meta-analysis. Neurology. 2021;96(17):805–17.
Hu Y, Shan Y, Du Q, Ding Y, Shen C, Wang S, et al. Gender and socioeconomic disparities in global burden of epilepsy: an analysis of time trends from 1990 to 2017. Front Neurol. 2021;12: 643450.
Chentouf A. Early predictors of refractory epilepsy in Oran, Algeria: a case-control study. Int J Neurol Brain Disord. 2016;3(2):1–5.
Ferlazzo E, Sueri C, Gasparini S, Aguglia U. Challenges in the pharmacological management of epilepsy and its causes in the elderly. Pharmacol Res. 2016;106:21–6.
Hernández-Ronquillo L, Adams S, Ballendine S, Téllez-Zenteno JF. Epilepsy in an elderly population: classification, etiology and drug resistance. Epilepsy Res. 2018;140:90–4.
Roy PL, Ronquillo LH, Ladino LD, Tellez-Zenteno JF. Risk factors associated with drug resistant focal epilepsy in adults: a case control study. Seizure. 2019;73:46–50.
Voll A, Hernández-Ronquillo L, Buckley S, Téllez-Zenteno JF. Predicting drug resistance in adult patients with generalized epilepsy: a case–control study. Epilepsy Behav. 2015;53:126–30.
Berg AT, Wusthoff C, Shellhaas RA, Loddenkemper T, Grinspan ZM, Saneto RP, et al. Immediate outcomes in early life epilepsy: a contemporary account. Epilepsy Behav. 2019;97:44–50.
Boonluksiri P, Visuthibhan A, Katanyuwong K. Clinical prediction rule of drug resistant epilepsy in children. J Epilepsy Res. 2015;5(2):84.
Fray S, Kchaou M, Chebbi S, Belal S. Predictors factors of refractory epilepsy in childhood. Revue Neurologique. 2015;171(10):730–5.
Orozco-Hernández JP, Quintero-Moreno JF, Marín-Medina DS, Valencia-Vásquez A, Villada HC, Lizcano A, et al. Multivariable prediction model of drug resistance in adult patients with generalized epilepsy from Colombia: a case–control study. Epilepsy Behav. 2018;88:176–80.
Jiang Y-L, Yuan F, Yang F, Sun X-L, Yang X-A, Song L, et al. Prognostic analysis for short-and long-term outcomes of newly diagnosed epilepsy. Seizure. 2017;47:92–8.
Xue-Ping W, Hai-Jiao W, Li-Na Z, Xu D, Ling L. Risk factors for drug-resistant epilepsy: a systematic review and meta-analysis. Medicine. 2019;98(30).
Tripathi M, Padhy UP, Vibha D, Bhatia R, Srivastava MP, Singh MB, et al. Predictors of refractory epilepsy in North India: a case–control study. Seizure. 2011;20(10):779–83.
Yuan F, Jia R, Gao Q, Yang F, Yang X, Jiang Y, et al. Early predictors of drug-resistant epilepsy development after convulsive status epilepticus. Eur Neurol. 2018;79:325–32.
Parviainen L, Kälviäinen R, Jutila L. Impact of diagnostic delay on seizure outcome in newly diagnosed focal epilepsy. Epilepsia Open. 2020;5(4):605–10.
Hernández-Ronquillo L, Buckley S, Ladino LD, Wu A, Moien-Afshari F, Rizvi SA, et al. How many adults with temporal epilepsy have a mild course and do not require epilepsy surgery? Epileptic Disord. 2016;18(2):137–47.
Yildiz EP, Gunes D, Bektas G, Aksu Uzunhan T, Tatli B, Caliskan M, et al. Predictive factors of drug-resistant epilepsy in children presenting under 2 years of age: experience of a tertiary center in Turkey. Acta Neurol Belg. 2018;118:71–5.
Aaberg KM, Bakken IJ, Lossius MI, Lund Søraas C, Håberg SE, Stoltenberg C, et al. Comorbidity and childhood epilepsy: a nationwide registry study. Pediatrics. 2016;138(3).
Muche EA, Ayalew MB, Abdela OA. Assessment of quality of life of epileptic patients in Ethiopia. Int J Chron Dis. 2020;2:2020.
Acknowledgements
Not applicable.
Author contributions
H.M: idea of the research; L.A: collection of cases; A.E.F: revision of manuscript and results; D.E.G: revision of the results and the manuscript and the corresponding author. All authors have read and approved the manuscript.
Funding
No funding for this research was obtained. No funding body interfered with the design of the study and collection, analysis and interpretation of data or the writing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Ethics Committee (EC) of Faculty of Medicine which is constituted and operates according to the International Conference on Harmonization-Good Clinical Practice ICH GCP guidelines (Food and Drug Administration guideline) and applicable local and institutional regulations and guidelines which govern EC operation. Date of the approval 17\9\2020 serial number 0106524. Written informed consent was obtained from all participants prior to the onset of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Marouf, H., Mohamed, L.A., El Ftatary, A. et al. Prevalence and risk factors associated with drug-resistant epilepsy in adult epileptic patients. Egypt J Neurol Psychiatry Neurosurg 59, 153 (2023). https://doi.org/10.1186/s41983-023-00750-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00750-3