Abstract
Background
Antisocial personality disorder (ASPD) is characterized by a lack of empathy, a sense of guiltlessness and shamelessness, as well as impulsiveness. ASPD is a relatively common psychiatric condition in the general population, whereas individuals with ASPD often have substantial social impairments and a lower quality of life, especially for those who have mental comorbidities. This review gives an overview of the etiological and clinical aspects of ASPD and critically examines ASPD from the structural, functional and biochemical perspectives.
Results
Twin and family studies showed genetic predisposition in ASPD. Some candidate genes associated with ASPD include SLC6A4, COMT, 5-HTR2A, TPH1, DRD2, OXTR, CACNG8, COL25A1 and several serotonergic genes. Environmental factors like adverse childhood experience (ACE) and active empathy deficits in toddlerhood play a role in the etiology of ASPD, whereas low intelligence or attainment, a large family size, a convicted parent, a disrupted family, and a young mother are predictors of antisocial personality. Structural abnormalities involving the corpus callosum, amygdala, putamen, anterior cingulate cortex, as well as orbitofrontal- and dorsolateral frontal cortices have been identified in ASPD. Other observed structural changes include a decrease in grey matter volume, whole-brain volume, and white matter volume and thickness. In addition, functional abnormalities involving autonomic activity, prefrontal functions, as well as brain functional networks like sensorimotor networks, cognitive networks and cortico-striatal connectivity have been reported. Biochemical factors associated with ASPD include fatty acid amide hydrolase (FAAH) reduction in the amygdala, as well as changes in plasma levels of inflammatory biomarkers and neurotropic factors [namely, tumor necrosis factor (TNF)-α, interleukin 10 (IL-10), transforming growth factor (TGF)-β1 and brain-derived neurotrophic factor (BNDF). Increased plasma levels of testosterone, ghrelin and cortisol and decreased levels of leptin have also been implicated in ASPD.
Conclusions
To date, there is no Food and Drug Administration (FDA) approved drugs for ASPD. Understanding the disease from different perspectives is important, as this provides insights into the underlying mechanisms of ASPD, whereas the associated biochemical markers can be used as potential diagnostic and treatment targets for ASPD.
Similar content being viewed by others
Introduction
Personality disorders are mental disorders characterized by dysfunctional or maladaptive patterns of behavior and thoughts that are inflexible and socially or culturally unacceptable. The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) divides personality disorders into four categories, namely, Cluster A, Cluster B, Cluster C and other personality disorders. In general, the characteristics of Cluster A, B and C disorders are (1) odd and eccentric traits, (2) emotional, dramatic and erratic traits and (3) anxious and fearful behaviors, respectively. For a person to be diagnosed with a personality disorder, he or she must exhibit significant self and interpersonal functioning impairments, and that these impairments are generally stable and consistent over time and in different situations. There must also be the presence of certain pathological personality traits for that personality disorder [1].
On the other hand, the International Classification of Diseases 11th revision (ICD-11) by the World Health Organization (WHO) has moved away from the previous categorical classification to a dimensional approach that focuses on the severity of self- and social functioning impairments. Therefore, ICD-11 classifies personality disorders into (1) mild personality disorders, (2) moderate personality disorders, (3) severe personality disorders and (4) personality disorder with unspecified severity. Trait domains like anankastia, borderline pattern, detachment, disinhibition, dissociality and negative affectivity are used to further elaborate on individual features in addition to the severity of the personality disorder [2]. ASPD of DMS-5 share similarities with personality disorder of ICD-11 with dissociality traits.
Individuals with a personality disorder tend to have problems in interpersonal relationships and suffer dysfunctions socially [3]. These disorders can have deteriorating effects on the quality of life and the related burden can be comparable to that experienced in severe somatic diseases [4]. Not only are these disorders having a substantial psychosocial impact on one’s life, but they are also common in the general population. Hence, they warrant close attention of psychiatrists and other health care providers. According to a systematic review and meta-analysis of 46 studies in 26 countries, for any personality disorder, the pooled prevalence was 7.8% worldwide. The study reported global rates of 3.8%, 2.8% and 5.0% for cluster A, B and C personality disorders, respectively. Significant heterogeneity was observed due to differences in study design (one-stage versus two-stage assessment), income (high-income versus low-income countries) and interview administration (trained graduate versus clinician) [5].
This review focusses on antisocial personality disorder (ASPD), which belongs to Cluster B personality disorder, based on the DSM-5 classification. A person with ASPD is characterized by egocentricity and incapacity to love, and is socially irresponsible, manipulative, exploitative and insensitive [6]. While many reviews in the published literature focus mainly on the psychosocial aspects of ASPD, this review discusses the disorder from the etiological and pathological perspectives. It gives an overview of the disorder, followed by a discussion on the etiological factors and pathological aspects of ASPD.
Main text
What is personality?
To understand personality disorders, one must first understand what personality is. There are many definitions of personality in the published literature and there is no one definition that is deemed the best. Psychologists often have difficulties in defining personality because it involves many characteristics of a person such as feelings, behaviors, thinking patterns and traits, whereas most of these characteristics are intangible and hard to measure. In one definition, personality is referred to as “the set of psychological traits and mechanisms within the individual that are organized and relatively enduring and that influence his or her interactions with, and adaptations to, the intrapsychic, physical, and social environments” [7]. Another definition by the Cambridge Dictionary refers personality to as “the special combination of qualities in a person that makes that person different from others, as shown by the way the person behaves, feels, and thinks” [8]. Personality is usually stable over time, and it does not change from one day to another. In fact, changes in personality are often limited and slow and may be due to life experiences that are traumatic or life changing.
There has been a “nature versus nurture” debate over the determinants of personality. One school of thoughts believes that personality is inborn or hereditary, while another believes that one’s personality is shaped by environmental factors, or in other words, it is acquired. In the biological approach of personality, genetics are said to be linked to personality traits. One well-known biological theorist was Hans Eysenck, who focused his works on the biological basis of personality [9]. While some researchers believe that all human behavioral traits are heritable [10, 11], studies have shown that personality is determined by an interplay of genetic and environmental factors. In a meta-analysis by Polderman and colleagues that investigated data from 14,558,903 twin pairs in 2,784 publications, it was concluded that genetic factors accounted for about 50% of any given trait and the rest were due to environmental (particularly, the non-shared environment) factors and error [12]. Hence, the determinants of personality should be viewed as an integration of genetic, social and developmental factors [13].
What is antisocial personality disorder (ASPD)?
According to DSM-5 [1], a person with ASPD is egocentric and derives his self-esteem from sources such as power, pleasure or personal gain. He sets goals mainly based on personal gratification and has problems with conforming to ethical behavior that is lawful or culturally normative. The essential pathological traits in ASPD revolve around disinhibition and antagonism, which are often related to criminal behavior. Therefore, a person with ASPD usually lacks empathy and feels no remorse after hurting or mistreating others. He uses exploitation to relate to others, and hence, is unable to maintain a mutually intimate relationship. He is manipulative, deceitful, callous and hostile. He may also demonstrate irresponsibility, impulsivity and risk-taking behaviors that are unnecessary and even self-damaging [1].
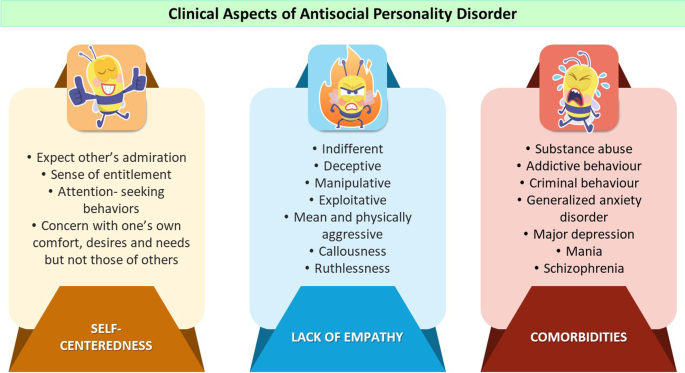
The ICD-11 does not use the term “antisocial personality disorder”. Instead, it includes dissociality as a trait domain for personality disorder or personality difficulty, which shares many similarities with ASPD in terms of clinical manifestations. The key characteristic of the dissociality trait domain is ignoring the feelings and rights of others, which include manifestations of lack of empathy and self-centeredness [14]. Some examples of manifestations of self-centeredness include a sense of entitlement, attention seeking behavior and a concern about one’s own comfort while neglecting the needs of others. On the other hand, the manifestations of lack of empathy include ruthlessness, indifference, callousness as well as being mean, exploitative, deceptive and manipulative [2].
It is noteworthy that ASPD is not the same as psychopathy, despite the fact that the two conditions share many similarities. Although psychopathy is relevant particularly in forensic psychiatry, it is not well defined in clinical practice, as it is not incorporated in any psychiatric diagnostic guidelines such as DSM-5 or ICD-11. Therefore, psychopathy is not a diagnosis officially but rather a personality abnormality that is non-specific. Research has also shown that not every individual who has ASPD is a psychopath and vice versa. In fact, only approximately one third of ASPD patients fulfill the criteria for psychopathy. It is also worth mentioning that some manifestations of psychopathy do not meet the criteria for ASPD but coincide with other Cluster B personality disorders [15]. Psychopathy is beyond the scope of this review, which focusses mainly on various aspects of ASPD.
In the general population, estimates from earlier studies indicate that the lifetime prevalence of ASPD ranges from 1–4%, and the disorder is three times more prevalent in male than female [16, 17]. In one study, it was shown that childhood hyperactivity and conduct disorder were predictors of ASPD and criminal activities in adulthood, whereas lower intelligence quotient (IQ) and reading difficulties were related to childhood and adolescent antisocial behavior [18]. The characteristics of ASPD are manifested in many areas of the patient’s life. The disorder is life-long, and often begins in the early years of an individual, as early as the age of 8 years, and is fully manifested in early adulthood. In childhood, before the age of 15 years, the disorder is diagnosed as conduct disorder. With the persistence of the antisocial behaviors, it will be converted to ASPD at the age of 18 years [19].
A recent study reported an increase in ASPD prevalence through early adulthood, which peaked at 3.91% in younger adults and decreased to 0.78% in those aged ≥ 65 years. The diagnosis of medical conditions and psychiatric disorders like generalized anxiety disorder, major depression, mania and substance abuse is more likely in older patients with ASPD. The presence of psychiatric and medical comorbidities, on the other hand, adds to the challenge of diagnosing and treating this group of patients [20].
Not uncommonly, mental disorders have been related to the commission of crime in past research. This also holds true for patients with ASPD, especially in the existence of a comorbid condition such as schizophrenia [21]. They are often involved in drug addiction or misuse, and face problems with the judiciary system due to violation of the rights of others or the law [22]. In one study consisting of 1052 drug abusers, it was reported that the likelihood of those with ASPD to be charged with theft only and other multiple types of crime were 2.16 (p < 0.001) and 2.44 (p < 0.001) times higher than those without ASPD, respectively [23].
Interestingly, one study showed the clinical and demographic factors for two different groups of ASPD patients namely, ASPD outpatients (non-incarcerated) and incarcerated ASPD individuals. The first group of ASPD patients were different from the second group in that: (1) they were older, (2) they were less likely to be married, (3) they had psychiatric comorbidity before the onset of ASPD, (4) they had more psychiatric hospitalizations previously and (5) they had a decreased likelihood of receiving lifetime psychotherapy. The findings indicate that previous psychiatric comorbidity prior to the onset of ASPD (hence early access to mental health care), might have prevented ASPD individuals from imprisonment [24]. The clinical aspects of ASPD are summarized in Fig. 1.
Etiology of ASPD
The exact etiology of ASPD is unknown and is most likely multifactorial. This section discusses the etiological factors under two broad subheadings, namely, genetic factors and environmental factors. It is noteworthy that these factors may or may not occur in isolation. Most often than not, there exists an interplay between genetic predisposition and a high-risk environment. When both factors are present, the observation of a greater pathology would be expected.
Genetic factors
Like many other psychiatric disorders, ASPD has been shown to demonstrate a strong hereditary component. Previous research in genetic epidemiology suggested that genetic factors help explain as much as 56% of variances observed, whereas shared environmental factors and specific individual environmental factors help explain the remaining 11% and 31% of the variances, respectively. It was also reported that compared to adults, genetic factors had a greater predictive power for ASPD in young individuals. However, it is noteworthy that other than the genetic influences, environmental factors such as unique life experiences, also play an important role in the disorder [25].
A longitudinal twin study comprising 2,600 twins from a Swedish registry investigated the role of genetics in antisocial behavior using structural equation modeling. The twins were divided into 4 different age groups: (1) 8–9, (2) 13–14, (3) 16–17 and (4) 19–20 years old. It was shown that 67% of the total variance was due to a common genetic influence, whereas the remaining 26% and 7% was explained by the shared environment and non-shared environment, respectively. For the second group of twins, the influence of age-specific environmental factors was found to be significant, indicating that common experiences such as peers play a role in the antisocial behavior for this age group [26].
Studies on the genetic factors influencing ASPD generally take two approaches. The first involves family studies from the perspectives of the hereditability of the disorder in twins or within the family tree. The second involves the identification of candidate genes that are related to the disorder. In one study, 1226 subjects with ASPD were investigated for family histories of behavior problems across multiple generations. The study identified three classes of family tree among the subjects. It was reported that 70.3% of the subjects belong to the first group where the family history of problem behaviors was minimal, and they had a higher socioeconomic functioning. The second group (9.4%) which had parental and progeny behavior problems, showed psychopathology, substance use and criminal behaviors. The third group of the subjects (20.3%) had a multi-generational history of behavior problems, and the subjects were reported to demonstrate psychopathology and the involvement of alcoholism and versatile criminal offending [27].
Serotonin (5-HT) is a neurotransmitter that regulates aggression, mood and social behavior. Studies have shown that serotonergic genes are linked to ASPD. One widely studied gene, known as the Solute Carrier Family 6 Member 4 (SLC6A4) has been indicated in ASPD. Located on chromosome17q11.1–17q12, this gene encodes a serotonin transporter, which takes part in the reuptake of serotonin into presynaptic neurons and is therefore, an important target of selective serotonin reuptake inhibitors (SSRIs) [28]. The SLC6A4 gene has a polymorphism in the promoter region known as serotonin-transporter-linked polymorphic region (5HTTLPR), which has been widely studied for its association with psychiatric disorders, including personality disorders [29]. Garcia and colleagues reported that an incremental effect for genetic risk in ASPD existed when the 5HTTLPR polymorphism was combined with another polymorphism known as 5-HTT variable number of tandem repeats (5-HTTVNTR) [30]. On the other hand, Sah and colleagues reported a significantly lower level of SLC6A4 expression in Turkish criminals with ASPD when compared to subjects in the control group [31].
Langevin and colleagues investigated 11 candidate serotonergic genes with regard to their protective effects and cumulative risk in ASPD patients aged 6 to 23 years. The genes were selected based on their linkage to ASPD and knowledge of their associated physiological processes. It was reported that the genetic variations of serotonergic genes, inherited together on a single chromosome (known as haplotypes) contributed to the variance in the cumulative risk and protective effects observed in certain behaviors in adolescence (such as general delinquency) and early adulthood (such as property/violent crimes and physical partner violence), as measured by the multilocus genetic profile risk/protection scores (MGPRS/ MGPPS). The findings suggest that haplotypes of multiple serotonergic genes are linked to an increased or decreased antisocial behavior (ASB) risk [32].
In a study that examined the epistatic interactions in 10 candidate genes for ASPD, Cuartas Arias and colleagues reported that the L allele of catechol-O-methyltransferase (COMT) gene was found to be associated with symptoms of ASPD, whereas a significant interaction was observed between the genetic variant of the COMT, 5-HTR2A and TPH1 genes. The findings of the study suggested that ASPD is linked with not just one candidate gene but is the result of the interplay of multiple alleles and polymorphic variants [33]. Another study by Lu and colleagues investigated the role of two genes, namely, ALDH2*1*1 and DRD2/ANKK1 TaqI A1A1 in ASPD and reported that subjects with the DRD2 A1/A1 and the ALDH2*1/*1 genotypes had a 5.39 times higher risk for ASPD (without alcoholism), compared with healthy controls [34].
Genetic differences in oxytocin (OXT) signaling have been shown to influence social behavior. For example, polymorphisms in the human oxytocin receptor gene (OXTR) have been linked antisocial behavior. Research has shown that in response to angry facial expressions, men rather than women with the OXTR rs 1042778 TT genotype showed an elevated right amygdala reactivity. In addition, the OXTR rs 1042778 TT genotype was linked to higher levels of ASB among men. These findings indicate that genetic variations on OXT signaling play a part in gender differences in amygdala functions and antisocial behavior in men [35].
Alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors (AMPARs) in the brain play a role in mediating rapid excitatory neurotransmission. The dysfunction of AMPARs has been linked to psychiatric disorders. The activity of AMPARs is regulated by a group of proteins called transmembrane AMPAR regulatory protein (TARP). Peng and colleagues reported that a single nucleotide polymorphism (SNP), rs10420324G found in the human TARP γ-8 gene (also called calcium voltage-gated channel auxiliary subunit gamma [CACNG8] gene), was associated with ASPD. A higher frequency of rs10420324G was observed in individuals with ASPD when compared to the control, whereas TARP γ-8 knockout mice showed ASPD behaviors. Decreased TARP γ-8 expression was linked to impaired AMPAR functions, particularly involving the pyramidal neurons in the prefrontal cortex, which has a role in aggression [36].
Comorbidity of addiction and ASPD is not uncommon in the published literature. Past research has investigated candidate genes which are responsible for both addictive and antisocial behaviors. Li and colleagues studied patients with or without substance dependence using 627 single nucleotide polymorphisms (SNPs) located in 179 candidate genes for addiction. It was reported that one SNP (rs13134663) located in the collagen XXV alpha 1 gene (COL25A1, located at chromosome 4q25) showed a significant association with ASPD in African Americans (p = 0.0002) and European Americans (p = 0.0004), particularly in the context of substance dependence [37]. The COL25A1 gene encodes a membrane-associated collagen, which is brain specific and is expressed in neurons. It has been demonstrated in vivo to be related to an Alzheimer’s-like pathology [38].
Environmental factors
A diagnosis of conduct disorder before the age of 15 years is one of the diagnostic criteria of ASPD. This means that ASPD has an early course during childhood. Therefore, childhood experiences have an influence in the development of ASPD [39]. Factors such as a person’s upbringing, family-, peer-, community-, school- and media factors are important players in shaping a child’s behavior. Environmental influences on ASPD can be viewed from two perspectives, namely, shared environment and unique environment. The first refers to the environment shared by siblings who are reared within the same family, which includes parenting practices, parental education and socioeconomic status. On the other hand, the unique environment is also known as the non-shared environment, which includes such factors as peer influences.
One study has reported that genetic and environmental influences vary with age. The study examined twin pairs in three different age groups: (1) 9–10 years, (2) 13–18 years and (3) 16–65 years. For children, it was observed that genetic factor and shared environmental factors accounted for 43% and 44% of the variance of conduct problems, respectively. However, during adolescence and adulthood, such variance was equally explained by genetic and unique environmental factors. The study, therefore, concluded that the shared environment is an important factor during childhood, whereas genetic factors are important and stable at all ages in conduct and antisocial personality problems [39].
Many environmental factors have been associated with personality disorders. In the past, studies have examined such factors as adverse childhood experiences (ACEs) and revealed that they are risk factors of these disorders. ACEs are common worldwide and have serious effects on a child’ physical and mental health. In a series of meta-analyses, the prevalence rates of various types of child maltreatment worldwide were reported to be high. For self-reported studies, the estimated prevalence rates were 12.7%, 22.6% and 36.3% for sexual-, physical- and emotional abuse, respectively, and 16.3% and 18.4% for physical- and emotional neglect, respectively. As for studies using informants, the estimated prevalence rates were 0.4% for sexual- and 0.3% for physical and emotional abuse, respectively [40].
One study reported that ACEs and victimization were more frequent among a cohort of 1396 male prisoners with a personality disorder than those without. Certain temperamental features were also associated with personality disorders. The likelihood of such disorders increased with the combination of a difficult temperament and childhood adversity [41]. On the other hand, another study that monitored 411 South London males from 8 years of age revealed that adult criminal and antisocial behaviors can be predicted in childhood. The study investigated psychosocial risk factors such as low intelligence or attainment and family factors such as a large family size, a convicted parent and child-rearing factors like a disrupted family or a young mother, as predictors of adult convictions and antisocial personality. The findings were surprising, as for boys with a convicted parent at the age of 10 years, nearly 50% were antisocial at the age of 32 years, whereas for the remainder, only 1 in 6 showed antisocial behavior. More than 60% of boys who were identified as having a high-risk at age of 8–10 years were found to be antisocial at age of 32 years [42].
Interestingly, one study that examined 203 (14.7%) participants with ASPD reported that the 5-HTTLPR genotype moderated the effects of ACEs on risk of ASPD among African American (AA) women. In the same study, it was also observed that being male and having a history of ACE significantly predicted ASPD in European Americans (EA) and that among AA men, the odds of ASPD was significantly increased with each additional ACE, irrespective of their 5-HTTLPR genotype. Hence, the study concluded that childhood maltreatment is a predictor of ASPD with moderation by the 5-HTTPLR genotype in AA women [43].
Yazgan and colleagues explored the relationship between cumulative early childhood adversity (CECA) (since birth to 7 years of age) and late adolescence ASB (through 18 years of age) using data from 585 subjects. Path analysis showed that CECA predicted impaired passive avoidance (IPA) later during adolescence, which mediated the relation between CECA and later ASB in adolescence. Hence, the study concluded that poor neurocognition such as IPA may be a target for neurocognitive intervention due to its link to CECA and later antisocial behavior [44].
Rhee and colleagues investigated the association between ASPD and psychopathy with two aspects of empathy, namely concern for others (passive deficits) and disregard for others (active deficits). It was reported that disregard for others observed during toddlerhood correlated with aggression and ASPD symptoms, as well as psychopathy factor 1 in adulthood, mediated by conduct problems during childhood or adolescence. These findings imply that antisocial behavior is linked to active empathy deficits and that early detection of empathy deficits during toddlerhood may help in identification of individuals at risk of ASPD and psychopathy later in adulthood [45]. Table 1 summarizes the etiological factors of ASPD.
Pathology of ASPD
Advances in neuroscience and imaging have allowed researchers to uncover the neural basis of ASPD by studying the structural and functional abnormalities in the brain of patients with ASPD, as well as their underlying mechanisms. This knowledge has important implications in the context of medicine, law and the society. There are some interesting views on how the neurological evidence of brain abnormalities can affect the legal system, which raise some difficult questions. For instance, if one has a brain dysfunction or lesion that leads to ASPD, should this be used as a reason for mitigation of punishment? On the other hand, if one has the biological risk factors and abnormalities that give rise to antisocial behavior, should they be the reasons for exacerbation of punishment, since these may increase the risk of re-offense?
Structural and functional abnormalities
Emerging imaging techniques have enabled researchers to probe into the structural brain abnormalities in ASPD. One common finding is decreased gray matter volume in the fronto-temporal regions. For example, Raine and colleagues compared the gray and white matter volumes of subjects with ASPD and those in the control group using structural magnetic resonance imaging (MRI). It was found that when compared to the control group, the group with ASPD had an 11% lower prefrontal gray matter volume. A reduction of autonomic activity was also observed with the introduction of a stressor. The study concluded that abnormalities in the prefrontal region might help explain the reduced arousal, poor decision-making, impaired fear conditioning and lack of conscience that are characteristic of antisocial behavior [46].
Structural abnormalities in the corpus callosum were correlated to antisocial personality. Using structural MRI, Raine and colleagues demonstrated that psychopathic antisocial individuals had increased estimated white matter volume in the corpus callosum and reduced corpus callosum thickness. Larger callosal volumes were linked to (1) interpersonal and affective deficits, (2) low spatial ability and (3) low reactivity in autonomic stress. However, psychosocial deficits and abnormalities in the corpus callosum were not related. An increased functional interhemispheric connectivity was also observed in the same study. Findings of the study suggested atypical neurodevelopmental processes in psychopathic antisocial individuals, which may involve increased white matter myelination or early axonal pruning [47].
Another study investigated the brain structural abnormalities in patients with schizophrenia and ASPD. When compared with healthy subjects, MRI revealed a volume reduction involving the (1) whole brain, (2) temporal lobe, and (3) increased putamen volume for both ASPD and schizophrenic patients. Schizophrenic patients with/without a history of violence further showed an elevated lateral ventricle volume, whereas those without a history of violence exhibited hippocampal volume reduction and increased putamen size [48]. On the other hand, a meta-analysis consisting of 43 imaging studies of the brain demonstrated a significant reduction in both prefrontal structure and function in individuals with ASPD, with the involvement of the anterior cingulate cortex, as well as orbitofrontal- and dorsolateral frontal cortices [49].
Other than gray matter abnormalities, white matter microstructural impairments have also been reported, using diffusion tensor imaging (DTI). Jiang and colleagues studied DTI measures such as radial diffusivity (RD), fractional anisotropy (FA), and axial diffusivity (AD) in individuals with ASPD and correlated them with impulsivity and risky behavior scores. It was demonstrated that many major white matter fiber bundles connecting the fronto-parietal control network and fronto-temporal network showed a reduction in FA. AD/RD deficits were identified in some extra white matter tracks not detected by FA. The AD and RD values, instead of the FA values, were correlated to impulsivity and risky behavior scores, in several regions such as the left posterior corona radiate/posterior thalamic radiate, splenium of corpus callosum,, left inferior- and right superior longitudinal fasciculus [50].
In another study, Jiang and colleagues investigated the changes in brain functional topological organization in individuals with ASPD using functional magnetic resonance imaging at rest (R-fMRI) [51]. The functional connectome of 35 normal controls and 32 ASPD patients were examined using such network properties as small-worldness, modularity and connectivity. A reduction in the global integration ability of whole-brain functions was observed as indicated by the small-world analysis, which showed an increase in path length and a reduction in network efficiency. Based on modularity analysis, there was a reduction in overall frontal region modularity, intra- and inter-module connectivities, and merged network modules in ASPS patients. An internal sub-network with 16 nodes and 16 edges, was found to be affected significantly in ASPD patients, as indicated by network-based statistics. These findings suggest a decrease in brain integration and topological organization segregation of brain functional networks, especially in the fronto-parietal control network, which may help explain the cognitive and behavioral disturbances in ASPD [51].
In a recent study, researchers used MRI scans to evaluate differences in brain structures between different subject groups. The 672 subjects were men and women aged 45 years, whom researchers have closely monitored from 3 years of age. When comparing subjects with life-course-persistent antisocial behavior (ASB) and those having low ASB, the former had a significantly smaller mean surface area (p < 0.0001) and mean cortical thickness (p < 0.020). Areas involved include temporal and frontal regions of the brain, which are associated with affect regulation, motivation and executive function. When comparing the adolescence-limited ASB group with (1) life-course-persistent ASB group or (2) non-ASB group, researchers did not observe widespread brain surface morphometric differences. These findings suggest that brain surface morphometric differences are mainly linked to life-course-persistent ASB but not adolescence-limited ASB. Hence, prospective longitudinal studies are important in evaluating the different patterns of ASB development [52].
Aggressive behavior (AB) and ASB are affected by genetic factors, which are common features of disruptive behavior disorders (DBDs). AB and ASB are also commonly observed in individuals with attention deficit hyperactivity disorder (ADHD). Kleine Deters and colleagues investigated the link between polygenic risk scores (PRS) for AB and ASB and amygdala morphology. The study found that changes in the shape, rather than the volume of the left basolateral amygdala, were associated with ABS-PRS in the presence of DBD, and that this association was independent of the severity of the ADHD symptoms and ADHD-PRS. The findings suggest that there exists an overlap in the genetic risks for ASB and DBDs, which are related to alterations in amygdala shape, which points to the potential use of vertex-based shape analyses in genetic studies of DBDs and ASB [53].
Jiang and colleagues investigated the disruption in neural circuits and reported that ASB was associated with reduced dynamic functional connectivity using resting-state fMRI, particularly in sensorimotor and high-order cognitive functional networks, which help explain the impairment in emotional processing and executive control. As such, dynamic functional connectivity from fMRI can be a potential tool in assessment and treatment of ASB [54]. On the other hand, Simard and colleagues investigated altered spectral power in antisocial male offenders and reported abnormalities in the neural oscillations within selected resting-state networks (RSNs), whereas the abnormal neural oscillations were associated with cocaine use [55].
Researchers have also studied the functional connectivity differences between patients with ASPD and healthy subjects. In one study, Kolla and colleagues demonstrated differences in the functional connectivity between the dorsal striatum and other structures in the brain, such as the anterior cingulate gyrus and the frontal pole among individuals with ASPD and healthy subjects. Differences in the relationship between aggressive behavior and superior ventral striatal–angular gyrus functional connectivity were also observed in those with ASPD. The findings suggest that these differences in functional connectivity were associated with the patients’ monoamine oxidase A (MAO-A) genotype [56].
Biochemical abnormalities
Other than structural and functional abnormalities in the brain, certain chemical substances have also been linked to the psychopathology of ASPD in past research. One such substance is monoamine oxidase-A enzyme (MAO-A), which breaks down several neurotransmitters like serotonin, epinephrine, noradrenaline, and dopamine. A previous study has observed an association between the superior and inferior ventral striatal MAO-A enzyme levels and functional connectivity among 19 impulsive ASPD males using [(11)C] harmine positron emission tomography (PET) scanning, R-fMRI and self-reported impulsivity measures. Results of the study revealed a link between ventral striatal MAO-A level with the functional connectivity of striatal regions associated with impulsive behavior in ASPD [57].
Another chemical, serotonin, was related to callous-unemotional traits among antisocial boys. Individuals with such traits lack empathy, as well as a sense of shame and guilt. Moul and colleagues examined serum serotonin levels (n = 66) with or without serotonin system single nucleotide polymorphisms (SNP) using a saliva or blood sample from boys (n = 157) with ASB between 3 and 16 years. It was reported that callous-unemotional traits were associated with functional SNPs from the serotonin 1b receptor gene (HTR1B) and 2a receptor gene (HTR2A). On the hand, serum serotonin levels significantly predicted callous-unemotional traits, in which boys with high callous-unemotional traits had significantly lower levels than those with low callous-unemotional traits [58].
The dopaminergic system has been linked to the pathophysiology of ASPD. Dopamine transporter (DAT) is a transmembrane protein that pumps dopamine from the synaptic cleft back to the presynaptic neurons [59]. This process is crucial in the regulation of dopamine levels in the brain, which has a role in decision-making. In one study, Rafei and Kolla investigated the relationship between the DAT1 genotypes and decision-making in ASPD and reported that ASPD patients with low DAT activity genotypes made poorer decisions as measured by the Iowa Gambling Task (IGT). The opposite was true for healthy subjects with low DAT activity genotypes, who demonstrated better IGT performance. The findings suggested that the dopamine levels in the brain, mediated by the DAT1 gene, were associated with poor decision-making in ASPD patients [60].
Godar and colleagues reported that genetic–environmental interactions involving serotonin, were associated with antisocial behavior in a mouse model. Mice that were subjected to postnatal stress were shown to exhibit abnormal responses to stress, aggressive behavior and social deficits, which were accompanied by significant upregulation of the gene for serotonin 5-HT2A receptor in the prefrontal cortical region. These observations were reduced in the presence of a 5-HT2 receptor antagonist. The findings suggest that the interactions between environmental factors such as early-life stress, result in upregulation in certain genes (such as 5-HT2A receptor in this case), which play a part in the underlying mechanism of antisocial behavior [61].
Besides serotonin and dopamine, another neurotransmitter that has been linked to ASPD is glutamate. In the central nervous system, glutamate is the key excitatory neurotransmitter that is measured together with glutamine (Glx). Through proton magnetic resonance spectroscopy. Smaragdi and colleagues showed that left dorsolateral prefrontal cortical Glx levels were higher in ASPD patients when compared with the Glx levels of patients with bipolar disorder and healthy subjects. Among patients with ASPD, a positive correlation between Glx levels and aggression was observed [62].
The human body produces naturally occurring substances called endocannabinoids, which have similar structures like compounds found in the cannabis plant. The endocannabinoid system (ECS) is a complex system consisting of endocannabinoids, enzymes and receptors [63]. An example of an enzyme in the ECS is fatty acid amide hydrolase (FAAH), which is involved in the degradation of the endocannabinoid, anandamide. Research has associated the brain’s ECS with ASPD and aggressive behavior. Using [11C]CURB PET scans, Kolla and colleagues demonstrated that when compared with normal subjects, a reduced level of fatty FAAH density was observed in the amygdala of ASPD patients, whereas the expression of FAAH in the striatum and cerebellum was linked to a reduction in impulsivity. An inverse relationship between cerebellar FAAH levels and assaultive aggression was also observed. Therefore, the researchers concluded that further exploration in FAAH expressions in different parts of the brain may be a promising therapeutic target for certain ASPD symptoms [64].
Testosterone is a hormone that plays a role in brain development, reproductive physiology, as well as behavior. Tajima-Pozo and colleagues explored the relationship between plasma testosterone levels and personality traits. In both genders, a positive correlation was observed between basal plasma testosterone levels and (1) antisocial personality traits (r = 0.336 and P < 0.018), (2) criminal thinking traits (r = 0. 376, P < 0.05) and (3) Millon compulsive traits (r = 0.386, P < 0.010) [65]. These findings are in tandem with those reported by an earlier study, in which plasma testosterone levels correlated significantly with hostility among violent male subjects. Among those diagnosed with ASPD, the plasma testosterone levels also significantly correlated with the unweighted ASPD symptom count. The study, therefore, concluded that males with antisocial behaviors and high hostility tend to have elevated levels of testosterone [66].
Certain inflammatory markers and neurotrophic factors have been shown to play a part in ASPD and substance use disorders (SUDs). For example, Wang and colleagues observed significantly higher levels of tumor necrosis factor (TNF)-α (P < 0.001) and lower levels of transforming growth factor (TGF)-β1 and brain-derived neurotrophic factor (BDNF) among patients with (1) ASPD, (2) SUDs and (3) ASPD + SUDs. On the other hand, higher levels of interleukin (IL)-10 were observed in patients with (1) SUDs and (2) ASPD + SUDs when compared with IL-10 levels of (1) ASPD patients and (2) healthy controls. Among the SUD subgroups, opioid use disorder (OUD) was shown to have significantly higher levels of IL-10. For examples, patients with (1) OUD, (2) OUD + ASPD had higher levels of IL-10 than other subgroups of SUDs (P ≤ 0.001). These findings suggest that inflammation and loss of certain neurotrophic factors (such as BDNF and TGF-β1) may be involved in the pathogenesis of ASPD. [67].
Ghrelin and leptin are two hormones influenced by cortisol, which plays an important role in the regulation of the stress response. Other than food intake, metabolism and energy expenditure, studies have also linked ghrelin and leptin to aggression and impulsivity. In one study, Tasci and colleagues compared the anxiety, aggressiveness, depression and impulsivity scores in patients with ASPD and healthy subjects using various instruments. The study found that the scores for all four parameters were significantly higher for the former. It was also reported that patients with ASPD had decreased serum levels of leptin and increased serum levels of ghrelin when compared to healthy subjects and that both hormones were positively correlated with aggression and impulsivity. The findings indicate that ghrelin and leptin may play a part in the pathophysiology of ASPD [68].
The interaction between the hypothalamic–pituitary–adrenal (HPA) axis and the autonomic nervous system (ANS) has an influence on behavior and the stress response. The coordination of the HPA and ANS can be measured by using cortisol and alpha amylase (AA), respectively. A study by Chen reported that offenders showed stronger cortisol-AA stress coordination compared to non-offenders. Furthermore, a positive correlation was detected between cortisol-AA stress coordination and 1) ASB and 2) negative urgency. Collectively, these findings suggest that the stronger cortisol-AA stress coordination may be due to an overactive ANS in the presence of high levels of emotional stress, which give new insight in the interplay between the stress response and behavioral problems [69]. Table 2 summarizes the structural, functional and biochemical abnormalities in ASPD.
Conclusions
Personality disorders, including ASPD, are common in the general population. ASPD has an early onset in childhood, which begins with the diagnosis of conduct disorder and is commonly associated with criminal behavior, as well as comorbidities such as other psychiatric disorders like schizophrenia and addiction. Hence, the disorder has many implications in the context of medicine, law and society. Although ASPD is highly heritable, both genetic and environmental factors play an important role and there is interplay between the two domains.
In terms of the pathology of the condition, structural and functional brain abnormalities, as well as certain chemicals, such as enzymes, hormones, inflammatory markers, neurotrophic factors and neurotransmitters have been linked to ASPD. Therefore, psychologists, psychiatrists, health care professionals and other caretakers should be aware of these neurobiological predispositions and pathological considerations when dealing with ASPD patients to minimize their social impairments and improve their quality of life.
Thus far, research has found that there is insufficient evidence for psychological interventions in ASPD in adults [70, 71]. Although drug therapy is sometimes used for comorbidities such as depression and panic disorder or used “off label” to treat the associated aggression and impulsivity in ASPD, to this point, there are no Food and Drug Administration (FDA) approved drugs for the treatment of ASPD [71]. Therefore, it is important to understand the etiological and pathological aspects of ASPD. Future research should explore the underlying pathogenic mechanisms of the disease, which may give insights into new therapeutic approaches. The chemicals that are involved in the pathophysiology of ASPD can also be promising biomarkers for early detection of the disorder or potential therapeutic targets.
Availability of data and materials
Not applicable.
Abbreviations
- 5HTTLPR:
-
Serotonin-transporter-linked polymorphic region
- 5-HTTVNTR:
-
5-HTT variable number of tandem repeats
- AA:
-
Alpha amylase
- AB:
-
Aggressive behavior
- ACE:
-
Adverse childhood experiences
- AD:
-
Axial diffusivity
- ADHD:
-
Attention deficit hyperactivity disorder
- ADHD-PRS:
-
Attention-deficit/hyperactivity disorder polygenic risk score
- ASB:
-
Antisocial behavior
- ASPD:
-
Antisocial personality disorder
- BDNF:
-
Brain-derived neurotrophic factor
- CACNG8 :
-
Calcium voltage-gated channel auxiliary subunit gamma 8 gene
- CECA:
-
Cumulative early childhood adversity
- COL25A1 :
-
Collagen XXV alpha 1 gene
- COMT :
-
Catechol-O-methyltransferase gene
- DSM-5:
-
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders
- DTI:
-
Diffusion tensor imaging
- HTR1B :
-
Serotonin 1b receptor gene
- HTR2A :
-
Serotonin 2a receptor gene
- ECS:
-
Endocannabinoid system
- FAAH:
-
Fatty acid amide hydrolase
- FDA:
-
Food and Drug Administration
- Glx:
-
Glutamine
- ICD-11:
-
The International Classification of Diseases 11th revision
- IPA:
-
Impaired Passive Avoidance
- MAO-A:
-
Monoamine oxidase-A enzyme
- FA:
-
Fractional anisotropy
- MRI:
-
Magnetic resonance imaging
- OUD:
-
Opioid use disorder
- OXT:
-
Oxytocin
- OXTR :
-
Oxytocin receptor gene
- PET:
-
Positron emission tomography
- PRS:
-
Polygenic risk score
- RD:
-
Radial diffusivity
- R-fMRI:
-
Functional magnetic resonance imaging at rest
- SLC6A4 :
-
Solute Carrier Family 6 Member 4 gene
- SNP:
-
Single nucleotide polymorphism
- SSRI:
-
Selective serotonin reuptake inhibitors
- SUD:
-
Substance use disorder
- TARP γ-8:
-
Transmembrane AMPAR regulatory protein γ-8
- TNF:
-
Tumor necrosis factor
- TGF:
-
Tumor growth factor
- THP1 :
-
Tryptophan hydroxylase 1 gene
- WHO:
-
World Health Organization
References
American Psychiatric Association. DSM-5: Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Association; 2013.
Bach B, First MB. Application of the ICD-11 classification of personality disorders. BMC Psychiatry. 2018;18(1):351. https://doi.org/10.1186/s12888-018-1908-3.
Tyrer P, Reed GM, Crawford MJ. Classification, assessment, prevalence, and effect of personality disorder. Lancet. 2015;385:717–26. https://doi.org/10.1016/S0140-6736(14)61995-4.
Soeteman DI, Verheul R, Busschbach JJ. The burden of disease in personality disorders: diagnosis-specific quality of life. J Pers Disord. 2008;22(3):259–68. https://doi.org/10.1521/pedi.2008.22.3.259.
Winsper C, Bilgin A, Thompson A, Marwaha S, Chanen AM, Singh SP, et al. The prevalence of personality disorders in the community: a global systematic review and meta-analysis. Br J Psychiatry. 2020;216(2):69–78. https://doi.org/10.1192/bjp.2019.166.
de Farias MSJA, Gomes ARF, Calheiros MB, Cavalcante HPA, Lessa MMM, Neto VLM. The antisocial personality disorder and its characteristics, changes and advances: a challenge. Int J Collab Res Intern Med Public Health. 2013;5(1):95–102.
Larsen RR, Buss DM. Personality psychology: domains of knowledge about human nature. 3rd ed. New York: McGraw-Hill; 2018. p. 4.
Cambridge Dictionary. Personality. 2019. https://dictionary.cambridge.org/dictionary/english/personality. Accessed 24 Jun 2022.
Eysenck HJ. The biological basis of personality. Springfield: Charles C Thomas Publisher; 1967.
Turkheimer E, Gottesman II. Is H2=0 a null hypothesis anymore? Behav Brain Sci. 1991;14(3):410–1.
Turkheimer E. Three laws of behaviour genetics and what they mean. Curr Dir Psychol Sci. 2000;9(5):160–4.
Polderman TJ, Benyamin B, de Leeuw CA, Sullivan PF, van Bochoven A, Visscher PM, et al. Meta-analysis of the heritability of human traits based on fifty years of twin studies. Nat Genet. 2015;47(7):702–9. https://doi.org/10.1038/ng.3285.
Barlow FK. Nature vs. nurture is nonsense: on the necessity of an integrated genetic, social, developmental, and personality psychology. Aust J Psychol. 2019;71:68–79.
World Health Organization. Dissociality in personality disorder or personality difficulty. In: International Classification of Diseases, Eleventh Revision (ICD-11). 2022. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1913158855 Accessed 11 Jul 2022
Abdalla-Filho E, Völlm B. Does every psychopath have an antisocial personality disorder? Braz J Psychiatry. 2020;42(3):241–2. https://doi.org/10.1590/1516-4446-2019-0762.
Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;62(6):553–64. https://doi.org/10.1016/j.biopsych.2006.09.019.
Trull TJ, Jahng S, Tomko RL, Wood PK, Sher KJ. Revised NESARC personality disorder diagnoses: gender, prevalence, and comorbidity with substance dependence disorders. J Pers Disord. 2010;24(4):412–26. https://doi.org/10.1521/pedi.2010.24.4.412.
Simonoff E, Elander J, Holmshaw J, Pickles A, Murray R, Rutter M. Predictors of antisocial personality. Continuities from childhood to adult life. Br J Psychiatry. 2004;184:118–27. https://doi.org/10.1192/bjp.184.2.118.
Black DW. The natural history of antisocial personality disorder. Can J Psychiatry. 2015;60(7):309–14. https://doi.org/10.1177/070674371506000703.
Holzer KJ, Vaughn MG, Loux TM, Mancini MA, Fearn NE, Wallace CL. Prevalence and correlates of antisocial personality disorder in older adults. Aging Ment Health. 2022;26(1):169–78. https://doi.org/10.1080/13607863.2020.1839867.
Maghsoodloo S, Ghodousi A, Karimzadeh T. The relationship of antisocial personality disorder and history of conduct disorder with crime incidence in schizophrenia. J Res Med Sci. 2012;17(6):566–71.
Dinwiddie SH, Daw EW. Temporal stability of antisocial personality disorder: blind follow-up study at 8 years. Compr Psychiatry. 1998;39(1):28–34. https://doi.org/10.1016/s0010-440x(98)90029-3.
Fridell M, Hesse M, Jaeger MM, Kühlhorn E. Antisocial personality disorder as a predictor of criminal behaviour in a longitudinal study of a cohort of abusers of several classes of drugs: relation to type of substance and type of crime. Addict Behav. 2008;33(6):799–811. https://doi.org/10.1016/j.addbeh.2008.01.001.
Esposito CM, Ceresa A, Auxilia AM, Zanelli Quarantini F, Caldiroli A, Capuzzi E, et al. Which clinical and demographic factors are related to incarceration in male patients with antisocial personality disorder? Int J Offender Ther Comp Criminol. 2022. https://doi.org/10.1177/0306624X221139073.
Ferguson CJ. Genetic contributions to antisocial personality and behavior: a meta-analytic review from an evolutionary perspective. J Soc Psychol. 2010;150(2):160–80. https://doi.org/10.1080/00224540903366503.
Tuvblad C, Narusyte J, Grann M, Sarnecki J, Lichtenstein P. The genetic and environmental etiology of antisocial behavior from childhood to emerging adulthood. Behav Genet. 2011;41(5):629–40. https://doi.org/10.1007/s10519-011-9463-4.
Vaughn MG, Salas-Wright CP, DeLisi M, Qian Z. The antisocial family tree: family histories of behavior problems in antisocial personality in the United States. Soc Psychiatry Psychiatr Epidemiol. 2015;50(5):821–31. https://doi.org/10.1007/s00127-014-0987-9.
Ramamoorthy S, Bauman AL, Moore KR, Han H, Yang-Feng T, Chang AS, et al. Antidepressant- and cocaine-sensitive human serotonin transporter: molecular cloning, expression, and chromosomal localization. Proc Natl Acad Sci U S A. 1993;90(6):2542–6. https://doi.org/10.1073/pnas.90.6.2542.
Blom RM, Samuels JF, Riddle MA, Joseph Bienvenu O, Grados MA, Reti IM, et al. Association between a serotonin transporter promoter polymorphism (5HTTLPR) and personality disorder traits in a community sample. J Psychiatr Res. 2011;45(9):1153–9. https://doi.org/10.1016/j.jpsychires.2011.03.003.
Garcia LF, Aluja A, Fibla J, Cuevas L, García O. Incremental effect for antisocial personality disorder genetic risk combining 5-HTTLPR and 5-HTTVNTR polymorphisms. Psychiatry Res. 2010;177(1–2):161–6. https://doi.org/10.1016/j.psychres.2008.12.018.
Sah I, Yukseloglu EH, Kocabasoglu N, Bayoglu B, Cirakoglu E, Cengiz M. The effects of 5-HTTLPR/rs25531 serotonin transporter gene polymorphisms on antisocial personality disorder among criminals in a sample of the Turkish population. Mol Biol Rep. 2021;48(1):77–84. https://doi.org/10.1007/s11033-021-06137-y.
Langevin S, Mascheretti S, Côté SM, Vitaro F, Boivin M, Turecki G, et al. Cumulative risk and protection effect of serotonergic genes on male antisocial behaviour: results from a prospective cohort assessed in adolescence and early adulthood. Br J Psychiatry. 2019;214(3):137–45. https://doi.org/10.1192/bjp.2018.251.
Cuartas Arias JM, Palacio Acosta CA, Valencia JG, Montoya GJ, Arango Viana JC, Nieto OC, et al. Exploring epistasis in candidate genes for antisocial personality disorder. Psychiatr Genet. 2011;21(3):115–24. https://doi.org/10.1097/YPG.0b013e3283437175.
Lu RB, Lee JF, Huang SY, Lee SY, Chang YH, Kuo PH, et al. Interaction between ALDH2*1*1 and DRD2/ANKK1 TaqI A1A1 genes may be associated with antisocial personality disorder not co-morbid with alcoholism. Addict Biol. 2012;17(5):865–74. https://doi.org/10.1111/j.1369-1600.2010.00268.x.
Waller R, Corral-Frías NS, Vannucci B, Bogdan R, Knodt AR, Hariri AR, et al. An oxytocin receptor polymorphism predicts amygdala reactivity and antisocial behavior in men. Soc Cogn Affect Neurosci. 2016;11(8):1218–26. https://doi.org/10.1093/scan/nsw042.
Peng SX, Wang YY, Zhang M, Zang YY, Wu D, Pei J, et al. SNP rs10420324 in the AMPA receptor auxiliary subunit TARP γ-8 regulates the susceptibility to antisocial personality disorder. Sci Rep. 2021;11(1):11997. https://doi.org/10.1038/s41598-021-91415-9.
Li D, Zhao H, Kranzler HR, Oslin D, Anton RF, Farrer LA, et al. Association of COL25A1 with comorbid antisocial personality disorder and substance dependence. Biol Psychiatry. 2012;71(8):733–40. https://doi.org/10.1016/j.biopsych.2011.12.011.
Forsell C, Björk BF, Lilius L, Axelman K, Fabre SF, Fratiglioni L, et al. Genetic association to the amyloid plaque associated protein gene COL25A1 in Alzheimer’s disease. Neurobiol Aging. 2010;31(3):409–15. https://doi.org/10.1016/j.neurobiolaging.2008.04.009.
Wesseldijk LW, Bartels M, Vink JM, van Beijsterveldt CEM, Ligthart L, Boomsma DI, et al. Genetic and environmental influences on conduct and antisocial personality problems in childhood, adolescence, and adulthood. Eur Child Adolesc Psychiatry. 2018;27(9):1123–32. https://doi.org/10.1007/s00787-017-1014-y.
Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LR, van Ijzendoorn MH. The prevalence of child maltreatment across the globe: review of a series of meta-analyses. Child Abuse Rev. 2015;24:37–50.
Roberts A, Yang M, Zhang T, Coid J. Personality disorder, temperament, and childhood adversity: findings from a cohort of prisoners in England and Wales. J Forens Psychiatry Psychol. 2008;19:460–83.
Farrington DP. Psychosocial predictors of adult antisocial personality and adult convictions. Behav Sci Law. 2000;18(5):605–22. https://doi.org/10.1002/1099-0798(200010)18:5%3c605::aid-bsl406%3e3.0.co;2-0.
Douglas K, Chan G, Gelernter J, Arias AJ, Anton RF, Poling J, et al. 5-HTTLPR as a potential moderator of the effects of adverse childhood experiences on risk of antisocial personality disorder. Psychiatr Genet. 2011;21(5):240–8. https://doi.org/10.1097/YPG.0b013e3283457c15.
Yazgan I, Hanson JL, Bates JE, Lansford JE, Pettit GS, Dodge KA. Cumulative early childhood adversity and later antisocial behavior: The mediating role of passive avoidance. Dev Psychopathol. 2021;33(1):340–50. https://doi.org/10.1017/S0954579419001809. (PMID: 32200772).
Rhee SH, Woodward K, Corley RP, du Pont A, Friedman NP, Hewitt JK, Hink LK, Robinson J, Zahn-Waxler C. The association between toddlerhood empathy deficits and antisocial personality disorder symptoms and psychopathy in adulthood. Dev Psychopathol. 2021;33(1):173–83. https://doi.org/10.1017/S0954579419001676.
Raine A, Lencz T, Bihrle S, LaCasse L, Colletti P. Reduced prefrontal gray matter volume and reduced autonomic activity in antisocial personality disorder. Arch Gen Psychiatry. 2000;57(2):119–27. https://doi.org/10.1001/archpsyc.57.2.119.
Raine A, Lencz T, Taylor K, Hellige JB, Bihrle S, Lacasse L, et al. Corpus callosum abnormalities in psychopathic antisocial individuals. Arch Gen Psychiatry. 2003;60(11):1134–42. https://doi.org/10.1001/archpsyc.60.11.1134.
Barkataki I, Kumari V, Das M, Taylor P, Sharma T. Volumetric structural brain abnormalities in men with schizophrenia or antisocial personality disorder. Behav Brain Res. 2006;169(2):239–47. https://doi.org/10.1016/j.bbr.2006.01.009.
Yang Y, Raine A. Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: a meta-analysis. Psychiatry Res. 2009;174(2):81–8. https://doi.org/10.1016/j.pscychresns.2009.03.012.
Jiang W, Shi F, Liu H, Li G, Ding Z, Shen H, et al. Reduced white matter integrity in antisocial personality disorder: a diffusion tensor imaging study. Sci Rep. 2017;7:43002. https://doi.org/10.1038/srep43002.
Jiang W, Shi F, Liao J, Liu H, Wang T, Shen C, et al. Disrupted functional connectome in antisocial personality disorder. Brain Imaging Behav. 2017;11(4):1071–84. https://doi.org/10.1007/s11682-016-9572-z.
Carlisi CO, Moffitt TE, Knodt AR, Harrington H, Ireland D, Melzer TR, et al. Associations between life-course-persistent antisocial behaviour and brain structure in a population-representative longitudinal birth cohort. The Lancet Psychiatry. 2020;7(3):245–53. https://doi.org/10.1016/S2215-0366(20)30002-X.
Kleine Deters R, Ruisch IH, Faraone SV, Hartman CA, Luman M, Franke B, et al. Polygenic risk scores for antisocial behavior in relation to amygdala morphology across an attention deficit hyperactivity disorder case-control sample with and without disruptive behavior. Eur Neuropsychopharmacol. 2022;62:63–73. https://doi.org/10.1016/j.euroneuro.2022.07.182.
Jiang W, Zhang H, Zeng LL, Shen H, Qin J, Thung KH, et al. Dynamic neural circuit disruptions associated with antisocial behaviors. Hum Brain Mapp. 2021;42(2):329–44. https://doi.org/10.1002/hbm.25225.
Simard I, Denomme WJ, Shane MS. Altered power spectra in antisocial males during rest as a function of cocaine dependence: a network analysis. Psychiatry Res Neuroimaging. 2021;309:111235. https://doi.org/10.1016/j.pscychresns.2020.111235.
Kolla NJ, Dunlop K, Meyer JH, Downar J. Corticostriatal connectivity in antisocial personality disorder by MAO-A genotype and its relationship to aggressive behavior. Int J Neuropsychopharmacol. 2018;21(8):725–33. https://doi.org/10.1093/ijnp/pyy035.
Kolla NJ, Dunlop K, Downar J, Links P, Bagby RM, Wilson AA, et al. Association of ventral striatum monoamine oxidase-A binding and functional connectivity in antisocial personality disorder with high impulsivity: a positron emission tomography and functional magnetic resonance imaging study. Eur Neuropsychopharmacol. 2016;26(4):777–86. https://doi.org/10.1016/j.euroneuro.2015.12.030.
Moul C, Dobson-Stone C, Brennan J, Hawes D, Dadds M. An exploration of the serotonin system in antisocial boys with high levels of callous-unemotional traits. PLoS ONE. 2013;8(2):e56619. https://doi.org/10.1371/journal.pone.0056619.
Vaughan RA, Foster JD. Mechanisms of dopamine transporter regulation in normal and disease states. Trends Pharmacol Sci. 2013;34(9):489–96. https://doi.org/10.1016/j.tips.2013.07.005.
Rafiei D, Kolla NJ. DAT1 polymorphism associated with poor decision-making in males with antisocial personality disorder and high psychopathic traits. Behav Sci Law. 2021;39(5):583–96. https://doi.org/10.1002/bsl.2537.
Godar SC, Mosher LJ, Scheggi S, Devoto P, Moench KM, Strathman HJ, et al. Gene-environment interactions in antisocial behavior are mediated by early-life 5-HT2A receptor activation. Neuropharmacology. 2019;159:107513. https://doi.org/10.1016/j.neuropharm.2019.01.028.
Smaragdi A, Chavez S, Lobaugh NJ, Meyer JH, Kolla NJ. Differential levels of prefrontal cortex glutamate+glutamine in adults with antisocial personality disorder and bipolar disorder: a proton magnetic resonance spectroscopy study. Prog Neuropsychopharmacol Biol Psychiatry. 2019;93:250–5. https://doi.org/10.1016/j.pnpbp.2019.04.002.
Lu HC, Mackie K. An Introduction to the endogenous cannabinoid system. Biol Psychiatry. 2016;79(7):516–25. https://doi.org/10.1016/j.biopsych.2015.07.028.
Kolla NJ, Boileau I, Karas K, Watts JJ, Rusjan P, Houle S, et al. Lower amygdala fatty acid amide hydrolase in violent offenders with antisocial personality disorder: an [11C]CURB positron emission tomography study. Transl Psychiatry. 2021;11(1):57. https://doi.org/10.1038/s41398-020-01144-2.
Tajima-Pozo K, Bayón C, Díaz-Marsá M, Carrasco JL. Correlation between personality traits and testosterone concentrations in healthy population. Indian J Psychol Med. 2015;37(3):317–21. https://doi.org/10.4103/0253-7176.162956.
Aromäki AS, Lindman RE, Eriksson CJP. Testosterone, aggressiveness, and antisocial personality. Aggressive Behav. 1999;25(2):113–23.
Wang TY, Lee SY, Hu MC, Chen SL, Chang YH, Chu CH, et al. More inflammation but less brain-derived neurotrophic factor in antisocial personality disorder. Psychoneuroendocrinology. 2017;85:42–8. https://doi.org/10.1016/j.psyneuen.2017.08.006.
Tasci G, Kaya S, Kalayci M, Atmaca M. Increased ghrelin and decreased leptin levels in patients with antisocial personality disorder. J Affect Disord. 2022;317:22–8. https://doi.org/10.1016/j.jad.2022.08.048.
Chen FR. The association between cortisol-AA coordination in response to stress, negative urgency, and antisocial behavior in an urban adult sample. Psychoneuroendocrinology. 2022;142:105799. https://doi.org/10.1016/j.psyneuen.2022.105799.
Black DW. The treatment of antisocial personality disorder. Curr Treat Options Psych. 2017;4:295–302. https://doi.org/10.1007/s40501-017-0123-z.
Gibbon S, Khalifa NR, Cheung NH, Völlm BA, McCarthy L. Psychological interventions for antisocial personality disorder. Cochrane Database Syst Rev. 2020;9(9):CD007668. https://doi.org/10.1002/14651858.CD007668.pub3.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
The author contributed solely to the writing and submission of this article. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wong, R.SY. Psychopathology of antisocial personality disorder: from the structural, functional and biochemical perspectives. Egypt J Neurol Psychiatry Neurosurg 59, 113 (2023). https://doi.org/10.1186/s41983-023-00717-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00717-4