Abstract
Alzheimer’s disease (AD) is the leading cause of dementia worldwide. Amyloid-beta (Aβ) deposition, is one of the processes involved in the pathophysiology of AD, has inspired interest in targeted therapies, including monoclonal antibodies. Aducanumab acts as a fully human IgG1 monoclonal antibody against Aβ by binding to amyloid plaques and was approved by the Food and Drug Administration (FDA) as the first disease-modifying drug for mild cognitive impairment and mild stages of AD. This accelerated approval, albeit the termination of the two phase III clinical trials of aducanumab due to results of futility analysis, has provoked controversy among the key opinion leaders in the field of cognitive neurology. Aducanumab poses significant financial constraints on patients and healthcare systems. Furthermore, the precise diagnosis of AD stages for appropriate aducanumab initiation remains a formidable challenge. The drug’s administration necessitates specialized infrastructure and medical equipment, and it may induce amyloid-related imaging abnormalities (ARIA), potentially resulting in cerebral edema or hemorrhage. These disadvantages might outweigh the potential benefits of the medication, especially considering the uncertainties regarding its efficacy. This commentary is intended to briefly evaluate the application of aducanumab in developing countries, considering the associated diagnostic challenges, clinical efficacy, cost, and potential adverse effects.
Similar content being viewed by others
Introduction
Alzheimer’s disease (AD), as a disabling neurodegenerative disease, is the most common cause of dementia worldwide. The progressive decline of cognitive functions is the primary clinical manifestation of AD [1].
The pathogenesis of AD, although not fully understood, is believed to have a multifactorial nature. Genetics and family history, environmental factors, some infections, nutritional status, and the patient’s lifestyle have been discussed to play a role in the progression of neurodegenerative diseases, such as AD [2].
Several hypotheses have been suggested to better understand the pathophysiology of AD, such as neuroinflammation, oxidative stress, tau pathology, microbiota–gut–brain axis, mitochondrial cascade hypothesis, calcium homeostasis and NMDA hypotheses, metal ion hypothesis, lymphatic system hypothesis, and last but not least the amyloid hypothesis [3,4,5].
There are several possible mechanisms by which amyloid-beta (Aβ) deposition contributes to AD pathogenesis:
Aβ aggregation: Aβ peptides have the potential to accumulate into oligomers, fibrils, and, in the end, form amyloid plaques. The formation of these aggregates is detrimental to neurons, resulting in synaptic dysfunction and causing neurodegeneration [6].
Neuroinflammation: Aβ accumulation can stimulate and activate microglia, which are the immune cells of the brain, leading to chronic inflammation. This inflammatory response contributes to neuronal damage and neuronal loss [7, 8].
Oxidative stress: Aβ has the potential to provoke oxidative stress through the production of reactive oxygen species (ROS), which can subsequently impair cellular constituents, including lipids, proteins, and DNA. This impairment ultimately results in neuronal malfunction and neuronal death [9].
Synaptic dysfunction and neuroplasticity: Aβ oligomers can interfere with synaptic function, signal mechanism, and long-term potentiation (LTP), a cellular process underlying learning and memory [10].
Tau pathology: Aβ accumulation may also promote the hyperphosphorylation of tau protein, leading to the formation of neurofibrillary tangles (NFTs). Tau pathology contributes to neuronal dysfunction and neurodegeneration in AD [11].
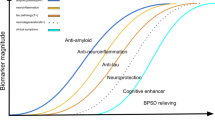
Having these in mind, the amyloid hypothesis has grabbed a significant amount of attention in the recent years for the development of targeted therapy as monoclonal antibodies for the modification of AD [12]. Although the amyloid hypothesis, which suggests that the accumulation of Aβ plaques in the brain is a primary cause of AD, has been widely debated in the scientific community [13, 14]. While aducanumab targets these plaques, it is still unclear whether reducing them will improve cognitive function in patients with AD [15].
AD involves two key molecular features: amyloid peptide production and tau protein aggregation, both contributing to neuronal death. Aβ peptides are produced when beta and gamma secretases cleave the amyloid precursor protein (APP). In pathological conditions, these peptides form toxic oligomers, protofibrils, fibrils, and eventually amyloid plaques. Tau proteins are associated with microtubules, providing structural support for neurons. During AD progression, tau proteins become hyperphosphorylated, detaching from microtubules, and leading to microtubule disassembly. Hyperphosphorylated tau forms oligomers, which contribute to the formation of paired helical filaments and NFTs. A vicious cycle occurs between tau and Aβ. Aβ oligomers increase intraneuronal calcium levels, causing inflammation, microglia recruitment, and further tau aggregation. Meanwhile, hyperphosphorylated tau disrupts microtubules and aggregates. Tau aggregates impair the proteasome system, reducing Aβ peptide degradation. Collectively, these processes culminate in neuronal death, a hallmark of AD [16].
Neurodegenerative diseases exhibit shared characteristics. Approximately 30% of AD patients develop parkinsonism, while over 30% of Parkinson’s disease (PD) patients experience dementia. Approximately 50% of PD with dementia cases are attributed to comorbidity with AD. Up to 50% of AD patients exhibit TDP-43 proteinopathy, typically associated with amyotrophic lateral sclerosis (ALS). Amyloid deposition occurs in roughly 10% of Creutzfeldt–Jakob disease (CJD) patients. Notably, diffuse intracellular amyloid plaques are linked to aging and HIV-associated neurocognitive disorders (HAND), while secondary neurodegeneration from stroke shares similarities with AD, including abnormal amyloid deposition [17]. Therefore, reducing Aβ accumulation, if demonstrated to exhibit adequate efficacy, could be a potential effective therapeutic approach not only for AD, but also for other neurodegenerative disorders in future research.
Aducanumab (under the brand name of Aduhelm™), a new therapy for AD after 18 years, acts as a fully human IgG1 monoclonal antibody against Aβ by binding to amyloid plaques. Aβ plaques are fragmentized by aducanumab to smaller oligopeptides or soluble amino acids [18]. By clearing Aβ aggregates, aducanumab may help reduce the activation of microglia and the resulting neuroinflammation, which contributes to neuronal damage in AD, and by reducing Aβ levels, aducanumab may help preserve synaptic function and neuroplasticity, which are critical for cognitive processes such as learning and memory [19, 20]. Indeed, lecanemab has recently been granted FDA approval, signifying its introduction as the second medication within the anti-amyloid classification; however, our focus remains on aducanumab, given the abundance of available information [21].
The accelerated approval of aducanumab as the first disease-modifying drug for AD in 2021 by the Food and Drug Administration (FDA) is considered controversial by several cognitive neurologists [22].
Two phase III clinical trials of aducanumab, EMERGE (NCT02484547) and ENGAGE (NCT02477800), were terminated due to the results of futility analyses in March 2019. EMERGE demonstrated a modest benefit in slowing cognitive decline, while ENGAGE failed to show any statistically significant difference between aducanumab and placebo groups [23]. However, Biogen presented the new drug application (NDA) of aducanumab to the FDA after conducting a post hoc analysis that claimed this medication to be efficacious [24]. In this commentary, we aim to discuss the different aspects of this questionable approval and whether aducanumab would be a suitable medication for the treatment of AD in the developing countries like the Middle East.
Discussion
To the best of our knowledge, this is the first article to address the possible utility of aducanumab in the developing countries considering different aspects including its clinical efficacy, diagnostic challenges, affordability, and harms in order to evaluate if the benefits of aducanumab outweigh its potential risks while demanding a highly developed medical infrastructure.
Clinical efficacy and utility
When assessing the controversial approval of aducanumab, there are some points that come to mind:
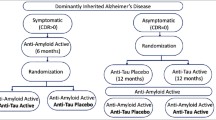
Aducanumab is approved by the FDA for mild cognitive impairment (MCI) and mild stages of AD (Mini-Mental State Examination [MMSE] > 24 and Clinical Dementia Rating [CDR] score of 0.5) and should not be administered in the moderate or severe stages of AD, as well as other types of dementia such as Lewy body dementia and vascular dementia [25].
There are no generally accepted and specified minimum clinically important differences (MCID) in the design and interpretation of the outcomes for AD trials, leading to the use of arbitrary criteria to interpret the results [26, 27]. MCID is defined as the smallest change in the score of a scale of interest for the patient or their caregiver to notice an improvement in the patient’s clinical symptoms and disease management [28]. As a matter of fact, the accelerated approval of aducanumab was based on the drug’s ability to reduce Aβ plaques in the brain, a surrogate endpoint, rather than on its ability to improve cognitive function or slow the progression of AD. In evaluating the effectiveness of medications in many diseases, specific biomarkers related to therapeutic efficiency are used. No such specific biomarker has been found in AD. Although Aβ plaques and NFTs are pathological hallmarks of AD, their correlation with cognitive decline is not perfect. The lack of definitive biomarkers makes it difficult to accurately measure disease progression and evaluate the efficacy of potential treatments [29, 30].
According to various criteria for evaluating the effectiveness, many researchers consider this medication to have no clinical effect. Examples of the exclusion criteria are the following: patients with significant vascular lesions, unstable cardiovascular or metabolic disorders, history of stroke, myocardial infarction, and patients with concomitant anticoagulants or antiplatelet medications (other than aspirin 81 mg daily) [31]. The majority of patients with AD have at least one of the exclusion criteria above.
On the other hand, based on a study in Asia, less than 7% of patients are diagnosed with AD, and this number accounts for the moderate and severe stages [32]. Therefore, given the present circumstances, only a limited number of patients might benefit from this targeted therapy in developing countries.
In general, the majority of clinical trials for aducanumab are conducted in Western countries with a predominantly Caucasian population. It remains uncertain whether the effectiveness and safety of the medication will be consistent for the diverse ethnic populations living in developing countries. To evaluate the therapeutic effectiveness and potential adverse reactions of aducanumab among distinct global populations, it might be necessary to conduct regionally tailored clinical studies [33].
Diagnostic challenges
For accurate diagnosis and differentiation among subjective cognitive impairment (SCI), MCI, and AD, it is essential to define precise and practical criteria for patient selection. Based on a consensus, amyloid neuroimaging is not considered appropriate in the diagnosis of AD [34], although the presence of amyloid plaques is a requirement for the initiation of aducanumab (low cerebrospinal fluid (CSF) Aβ42 (or Aβ42:Aβ40 ratio) or positive amyloid positron emission tomography (PET) imaging using one of the amyloid PET tracers) [35]. According to the estimates, between 37 and 68% of MCI or mild AD patients have the appropriate amyloid status to start treatment with aducanumab [36]. In developing countries, including Iran, advanced fluorodeoxyglucose-positron emission tomography (FDG-PET) and tau-PET scans are not easily accessible and require considerable costs. The use of specific assessment tools like the Montreal Cognitive Assessment (MoCA) for MCI diagnosis may result in a substantial number of false positives due to its dependence on education and the high illiteracy rates among elderly populations in many developing countries such as the Middle East, particularly among women, who exhibit a greater prevalence of illiteracy and susceptibility to AD. In such contexts, functional evaluation instruments that are not reliant on extensive education, such as the Functional Assessment Staging (FAST) tool, may be more advantageous. Nevertheless, the FAST may not accurately identify MCI cases. The application of age-matched volumetric magnetic resonance imaging (MRI) techniques may provide valuable information.
Affordability
The cost of this medication is $56,000 per year in the United States of America (which was later reduced to $28,200 per year), without considering the physician’s fee and routine imaging. Drug pricing negotiations between the manufacturer and each country can have a significant impact on the cost of aducanumab. However, this expenditure is rather high not only for the developing countries but also for developed Western European and Northern American countries. For example among the sixteen countries in the Middle East with a population of more than 400 million, only three countries with approximately 17 million people have a gross domestic product per capita (GDP per capita) above $56,000. Even with half the price, aducanumab is too expensive for insurance companies, considering the high number of patients with AD. According to the Dementia Forecasting Collaborators, by the year 2050, the Middle East and North Africa will have the highest increase in the number of patients with AD [37].
There are several countries in the Middle East, such as Iran, that have underdeveloped healthcare systems, which may be unable to provide the necessary infrastructure for administering aducanumab via the intravenous route, including specialized infusion centers and medical equipment [38]. Further cost–utility studies should be conducted for decision-making.
In Table 1, the factors contributing to the estimation of aducanumab’s cost–effectiveness are displayed. These factors are computed individually for each nation.
Harms
Researchers have known from the past that amyloid-related imaging abnormalities (ARIA) are caused by anti Aβ monoclonal antibodies [42]. The initial occurrence of ARIA in association with aducanumab was documented during the second phase of the PRIME clinical trial. A dose-dependent relationship was observed, with a higher prevalence of ARIA primarily among APOE ε4 allele carriers [43].
MRI can detect two types of ARIA: ARIA-E (edema) and ARIA-H (hemorrhage). ARIA-E is characterized by the presence of vasogenic edema, a form of brain swelling resulting from the leakage of fluid from blood vessels into brain tissue. Symptoms of ARIA-E may include headache, confusion, dizziness, nausea, and, in severe cases, seizures or focal neurological manifestations, depending on the affected brain region. ARIA-H, on the other hand, is identified by the presence of small areas of bleeding within the brain. Depending on the location and severity, ARIA-H can either be asymptomatic or induce mild to moderate symptoms [42].
It is argued by many critics that these side effects may outweigh the potential benefits of the drug, particularly since it is unclear whether or not it is effective [26].
As mentioned above, the likelihood of developing ARIA is elevated in the patients possessing a particular genetic variant, the APOE ε4 allele. This might mean that genetic testing might be necessary before initiating this medication to adjust the dosing for APOE ε4 carriers in case of adverse events.
During clinical trials, the majority of ARIA incidents were of mild to moderate severity and resolved without persistent consequences [42]. Nonetheless, severe cases may lead to significant complications. Therefore, it is essential to closely monitor patients receiving aducanumab through routine brain MRIs to detect the most concerning potential adverse effects throughout the treatment period [31, 32, 44].
The need for routine monitoring that should be interpreted by trained cognitive neurologists, alongside the high cost of this medication, mandates careful consideration of healthcare policy makers in the developing countries, in order to keep the healthcare system from exhaustion.
Although not an original research, this article might help facilitate future research by attracting the attention of researchers in these countries to conduct cost–utility and cost–effectiveness studies on aducanumab.
Further investigations and cautious contemplation are required before administering this medication to individuals with AD in developing countries.
Conclusions
In conclusion, aducanumab offers potential hope for the patients with AD and their caregivers, but diagnostic challenges and controversies remain among cognitive neurology scholars. Accurately distinguishing SCI, MCI, and AD is critical for patient selection when considering aducanumab treatment. Although PET neuroimaging is not typically recommended for AD diagnosis, it is required for initiating aducanumab. In developing countries, limited access to advanced PET neuroimaging technologies, such as tau-PET and FDG-PET scans, and the high costs associated with them pose significant barriers. The use of neuropsychological scales alone is insufficient; instead, multiple clinical criteria, neuroimaging procedures, and genetic tests should be employed. Region-specific challenges, such as high illiteracy rates, may necessitate alternative assessment tools like FAST. Additional clinical trials are required to resolve uncertainties regarding aducanumab’s effectiveness, while cost–utility and cost–effectiveness analyses can aid in evaluating its potential advantages and disadvantages across various populations.
Availability of data and materials
Not applicable.
Abbreviations
- Aβ:
-
Amyloid-beta
- AD:
-
Alzheimer’s disease
- ALS:
-
Amyotrophic lateral sclerosis
- APP:
-
Amyloid precursor protein
- ARIA-E:
-
Amyloid-related imaging abnormalities-vasogenic edema
- ARIA-H:
-
Amyloid-related imaging abnormalities-hemorrhage
- CDR:
-
Clinical Dementia Rating
- CJD:
-
Creutzfeldt–Jakob disease
- CSF:
-
Cerebrospinal fluid
- DNA:
-
Deoxyribonucleic acid
- FAST:
-
Functional Assessment Staging
- FDA:
-
Food and Drug Administration
- FDG-PET:
-
Fluorodeoxyglucose-positron emission tomography
- GDP:
-
Gross domestic product
- HAND:
-
HIV-associated neurocognitive disorders
- ICER:
-
Incremental cost–effectiveness ratio
- LTP:
-
Long-term potentiation
- MCI:
-
Mild cognitive impairment
- MCID:
-
Minimum clinically important differences
- MMSE:
-
Mini-Mental State Examination
- MoCA:
-
Montreal Cognitive Assessment
- MRI:
-
Magnetic resonance imaging
- NDA:
-
New drug application
- NFTs:
-
Neurofibrillary tangles
- PET:
-
Positron emission tomography
- QALY:
-
Quality-adjusted life year
- ROS:
-
Reactive oxygen species
- SCI:
-
Subjective cognitive impairment
- TDP-43:
-
TAR DNA-binding protein 43
References
Wilson RS, Segawa E, Boyle PA, Anagnos SE, Hizel LP, Bennett DA. The natural history of cognitive decline in Alzheimer’s disease. Psychol Aging. 2012;27(4):1008–17.
Tanaka M, Vécsei L. Editorial of special issue ‘dissecting neurological and neuropsychiatric diseases neurodegeneration and neuroprotection’. Int J Mol Sci. 2022;23(13):6991.
Du X, Wang X, Geng M. Alzheimer’s disease hypothesis and related therapies. Transl Neurodegener. 2018;7(1):2.
Liu PP, Xie Y, Meng XY, Kang JS. History and progress of hypotheses and clinical trials for Alzheimer’s disease. Signal Transduct Target Ther. 2019;4:29.
Wiatrak B, Balon K, Jawień P, Bednarz D, Jęśkowiak I, Szeląg A. The role of the microbiota–gut–brain axis in the development of Alzheimer’s disease. Int J Mol Sci. 2022;23(9):4862.
Balupuri A, Choi KE, Kang NS. Aggregation mechanism of Alzheimer’s amyloid β-peptide mediated by α-strand/α-sheet structure. Int J Mol Sci. 2020;21(3):1094.
Heneka MT, Carson MJ, El Khoury J, Landreth GE, Brosseron F, Feinstein DL, et al. Neuroinflammation in Alzheimer’s disease. Lancet Neurol. 2015;14(4):388–405.
Kinney JW, Bemiller SM, Murtishaw AS, Leisgang AM, Salazar AM, Lamb BT. Inflammation as a central mechanism in Alzheimer’s disease. Alzheimers Dement (N Y). 2018;4:575–90.
Tönnies E, Trushina E. Oxidative stress, synaptic dysfunction, and Alzheimer’s disease. J Alzheimers Dis. 2017;57(4):1105–21.
Jackson J, Jambrina E, Li J, Marston H, Menzies F, Phillips K, et al. Targeting the synapse in Alzheimer’s disease. Front Neurosci. 2019. https://doi.org/10.3389/fnins.2019.00735.
Rajmohan R, Reddy PH. Amyloid-beta and phosphorylated tau accumulations cause abnormalities at synapses of Alzheimer’s disease neurons. J Alzheimers Dis. 2017;57(4):975–99.
Barrera-Ocampo A, Lopera F. Amyloid-beta immunotherapy: the hope for Alzheimer disease? Colomb Med (Cali). 2016;47(4):203–12.
Morris GP, Clark IA, Vissel B. Inconsistencies and controversies surrounding the amyloid hypothesis of Alzheimer’s disease. Acta Neuropathol Commun. 2014;2(1):135.
Morris GP, Clark IA, Vissel B. Questions concerning the role of amyloid-β in the definition, aetiology and diagnosis of Alzheimer’s disease. Acta Neuropathol. 2018;136(5):663–89.
Selkoe DJ, Hardy J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol Med. 2016;8(6):595–608.
Vignon A, Salvador-Prince L, Lehmann S, Perrier V, Torrent J. Deconstructing Alzheimer’s disease: how to bridge the gap between experimental models and the human pathology? Int J Mol Sci. 2021;22(16):8769.
Tanaka M, Toldi J, Vécsei L. Exploring the etiological links behind neurodegenerative diseases: inflammatory cytokines and bioactive kynurenines. Int J Mol Sci. 2020;21(7):2431.
Arndt JW, Qian F, Smith BA, Quan C, Kilambi KP, Bush MW, et al. Structural and kinetic basis for the selectivity of aducanumab for aggregated forms of amyloid-β. Sci Rep. 2018;8(1):6412.
Dong Y, Li X, Cheng J, Hou L. Drug development for Alzheimer’s disease: microglia induced neuroinflammation as a target? Int J Mol Sci. 2019;20(3):558.
Silvestro S, Valeri A, Mazzon E. Aducanumab and its effects on tau pathology: is this the turning point of amyloid hypothesis? Int J Mol Sci. 2022;23(4):2011.
Hoy SM. Lecanemab: first approval. Drugs. 2023;83(4):359–65.
U.S. Food & Drug Administration, Drugs@FDA: FDA-Approved Drugs, Aducanumab. Reference ID 4822820. 2021. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=761178.
Kuller LH, Lopez OL. ENGAGE and EMERGE: truth and consequences? Alzheimers Dement. 2021;17(4):692–5.
Knopman DS, Jones DT, Greicius MD. Failure to demonstrate efficacy of aducanumab: an analysis of the EMERGE and ENGAGE trials as reported by Biogen, December 2019. Alzheimers Dement. 2021;17(4):696–701.
FDA Grants Accelerated Approval for Alzheimer’s Drug. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-grants-accelerated-approval-alzheimers-drug. Accessed 30 May 2022.
Ebell MH, Barry HC. Why physicians should not prescribe aducanumab for Alzheimer disease. Am Fam Physician. 2022;105(4):353–4.
Liu KY, Schneider LS, Howard R. The need to show minimum clinically important differences in Alzheimer’s disease trials. Lancet Psychiatry. 2021;8(11):1013–6.
Andrews JS, Desai U, Kirson NY, Zichlin ML, Ball DE, Matthews BR. Disease severity and minimal clinically important differences in clinical outcome assessments for Alzheimer’s disease clinical trials. Alzheimers Dement (N Y). 2019;5:354–63.
Hampel H, O’Bryant SE, Molinuevo JL, Zetterberg H, Masters CL, Lista S, et al. Blood-based biomarkers for Alzheimer disease: mapping the road to the clinic. Nat Rev Neurol. 2018;14(11):639–52.
Henriksen K, O’Bryant SE, Hampel H, Trojanowski JQ, Montine TJ, Jeromin A, et al. The future of blood-based biomarkers for Alzheimer’s disease. Alzheimers Dement. 2014;10(1):115–31.
Cummings J, Aisen P, Apostolova LG, Atri A, Salloway S, Weiner M. Aducanumab: appropriate use recommendations. J Prev Alzheimers Dis. 2021;8(4):398–410.
Lang L, Clifford A, Wei L, Zhang D, Leung D, Augustine G, et al. Prevalence and determinants of undetected dementia in the community: a systematic literature review and a meta-analysis. BMJ Open. 2017;7(2): e011146.
Oh SS, Galanter J, Thakur N, Pino-Yanes M, Barcelo NE, White MJ, et al. Diversity in clinical and biomedical research: a promise yet to be fulfilled. PLoS Med. 2015;12(12): e1001918.
Johnson KA, Minoshima S, Bohnen NI, Donohoe KJ, Foster NL, Herscovitch P, et al. Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer’s Association. Alzheimers Dement. 2013;9(1): e-1-16.
Cummings J, Salloway S. Aducanumab: appropriate use recommendations. Alzheimers Dement. 2022;18(3):531–3.
Doraiswamy PM, Sperling RA, Johnson K, Reiman EM, Wong TZ, Sabbagh MN, et al. Florbetapir F 18 amyloid PET and 36-month cognitive decline: a prospective multicenter study. Mol Psychiatry. 2014;19(9):1044–51.
Nichols E, Steinmetz JD, Vollset SE, Fukutaki K, Chalek J, Abd-Allah F, et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2022;7(2):e105–25.
Katoue MG, Cerda AA, García LY, Jakovljevic M. Healthcare system development in the Middle East and North Africa region: challenges, endeavors and prospective opportunities. Front Public Health. 2022;10:1045739.
Sinha P, Barocas JA. Cost-effectiveness of aducanumab to prevent Alzheimer’s disease progression at current list price. Alzheimers Dement (N Y). 2022;8(1): e12256.
Chung SD, Liu SP, Sheu JJ, Lin CC, Lin HC, Chen CH. Increased healthcare service utilizations for patients with dementia: a population-based study. PLoS ONE. 2014;9(8): e105789.
Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–103.
Sperling RA, Jack CR Jr, Black SE, Frosch MP, Greenberg SM, Hyman BT, et al. Amyloid-related imaging abnormalities in amyloid-modifying therapeutic trials: recommendations from the Alzheimer’s Association Research Roundtable Workgroup. Alzheimers Dement. 2011;7(4):367–85.
Sevigny J, Chiao P, Bussière T, Weinreb PH, Williams L, Maier M, et al. The antibody aducanumab reduces Aβ plaques in Alzheimer’s disease. Nature. 2016;537(7618):50–6.
Salloway S, Chalkias S, Barkhof F, Burkett P, Barakos J, Purcell D, et al. Amyloid-related imaging abnormalities in 2 phase 3 studies evaluating aducanumab in patients with early Alzheimer disease. JAMA Neurol. 2022;79(1):13–21.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
DHF and AK were major contributors in writing the manuscript. MN contributed to the generation of idea to write the manuscript and critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hazegh Fetratjoo, D., Kargar, A. & Noroozian, M. Aducanumab: an uprising hope with vague horizons. Egypt J Neurol Psychiatry Neurosurg 59, 85 (2023). https://doi.org/10.1186/s41983-023-00684-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00684-w