Abstract
Background
Carotid cavernous fistula (CCF) is an abnormal arteriovenous shunt between the carotid artery or its branches, with the cavernous sinus. It is still common in developing countries, and is mostly due to traumatic origin. Endovascular treatment has emerged as the primary mode of treatment of CCF. This is the first study describing the clinical manifestation, angiographic characteristic, and the challenges we face in endovascular treatment of CCF cases in Makassar, Indonesia.
Results
This descriptive study was conducted between January 2019 to March 2022. We reviewed medical records and angiograms of all patients diagnosed with CCF at the Wahidin General Hospital, Makassar. Clinical manifestations, angiogram results, treatment, and outcome data were analyzed. A total of 23 patients were included in this study, with 17 (73.9%) direct CCF (Barrow type A) and 6 (26.1%) indirect CCF (Barrow type B, C, D). The mean age of patients were 32 years old. The three most common clinical manifestations were proptosis (n = 21, 91.3%), headache (n = 14, 60.8%), and chemosis (n = 14, 60.8%). The three most common drainage routes were via the superior ophthalmic vein (n = 23, 100%), inferior petrosal sinus (n = 12, 52.1%), and superficial middle cerebral vein (n = 6, 26.0%). All patients with direct CCF (n = 17) had endovascular treatment, resulting in 13 cases with complete occlusion (76.5%), 3 cases with incomplete occlusion (17.6%), and 1 (5.9%) procedure cancelled due to difficult navigation. Occlusion of fistula was best achieved with detachable coil, with a technical success rate of 90%. In indirect CCF (n = 6), 4 patients were treated conservatively and 2 with endovascular treatment, with complete occlusion in 2 patients.
Conclusions
Carotid cavernous fistula patients commonly presented with orbital symptoms, headache, or neuro-ophthalmologic signs. The most common drainage pattern is via anterior route. Posterior, superior and lateral drainage were not found in indirect CCF. Endovascular treatment is an effective method for fistula closure, especially in the case of direct fistula. Challenges in endovascular treatment are related to the anatomy of the fistula and cavernous sinus.
Similar content being viewed by others
Background
Carotid cavernous fistula (CCF) is an abnormal arteriovenous shunt occurring between the carotid artery or its branches, with the cavernous sinus. While its rare in developed countries, the condition is commonly encountered in developing countries, and can occur spontaneously or in association with trauma. In fact, traumatic CCF accounts for 75% of all CCF cases, and was reported in 0.2% of patients with traumatic brain injury and 4% of patients with basilar skull fracture [1].
There are several classification systems for CCF. The most common of which is the Barrow classification, which divides CCF based on the angioarchitecture of the fistula’s arterial portion [2]. Type A is a high flow fistula connecting the cavernous segment of the internal carotid artery directly with cavernous sinus, and is the most common type of CCF, accounting for 75–80% of cases [1]. It is often the result of blunt head trauma, or in several cases caused by rupture of intracavernous aneurysms. Type B is an indirect low flow fistula from meningeal branches of internal carotid artery, while type C is from meningeal branches of the external carotid artery. Type D is indirect low flow fistula from meningeal branches of both internal and external carotid artery [1, 2]. Another important classification for clinical correlation and treatment planning divides CCF based on the draining vein angioarchitecture [3, 4].
In recent decades, endovascular treatment has become the primary mode of treatment for CCF. In direct CCF (Barrow A), endovascular treatment with detachable balloon, coil, or covered stent via transarterial route is effective to occlude the fistula while preserving the parent artery. If the fistula is large, the parent artery may need to be sacrificed provided that the collateral flow to the distal ICA is good. In indirect CCF, endovascular treatment is preferred in the presence of conditions that warrant immediate closure of the fistula, such as progressive visual loss, severe epistaxis, pseudoaneurysm, large varix in the cavernous sinus, cortical vein drainage or thrombosis of venous drainage [5]. Transvenous or transarterial route can be selected for endovascular closure of indirect fistula [5].
Despite many reports of CCF in other countries, there is still limited data on CCF and its treatment in Indonesia. Since 2010, the beginning of endovascular treatment in our institution, we have encountered and successfully managed several cases of CCF, despite some challenges in our institution. We observed that although most cases were similar with those described from outside Makassar, others had varied presentation. Hence, this is the first study to provide a description of the clinical manifestation, angiographic characteristics, and the treatment of CCF patients in Makassar, Indonesia. We also describe some of the challenges faced in the management of several cases.
Methods
This is a descriptive study carried out at Wahidin General Hospital in Makassar between January 2019 to March 2022. After receiving ethics approval, we retrospectively reviewed the medical records and angiograms of all patients diagnosed with CCF. The clinical manifestation, angiographic data and treatment was then recorded. All endovascular procedures were performed by one senior interventional neurologist with more than 10 years of clinical experience. The angiographic suite utilized was the Allura Monoplane Unit (Philips Corporation, United States of America). All patients underwent digital subtraction angiography (DSA). Arterial access was gained from the right femoral artery in most cases, and from the left femoral artery in several cases. DSA was performed using a 5F Judkins Right (JR) 3.5 Catheter (Merit Medical system, United States of America) or the 5F Headhunter Catheter (Terumo Radiofocus, Japan). For better visualization of high flow fistula, we utilized high frame rate image and sometimes performed Heuber or Mehringer Hieshima manuever.
We recorded the CCF location, type and the collateral circulation. Venous drainage was recorded, and classified as follows: (1) anterior if venous drainage occurred via the superior ophthalmic vein (SOV) or inferior ophthalmic vein (IOV); (2) superior if venous drainage occurred via the superficial middle cerebral vein (SMCV); (3) posterior if venous drainage occurred via the basal vein of Rosenthal (BVR) or superior petrosal sinus (SPS); (4) inferior if venous drainage via inferior petrosal sinus (IPS), pterygoid plexus (PP) or clival plexus (CP).
For each case decided to proceed to endovascular treatment of CCF, it was performed several days following diagnostic angiography, under general anaesthesia. A 6F Chaperon™ (Microvention Corporation, United States of America) guiding catheter was navigated to internal carotid artery. Fistula closure was achieved with either coil (Axium 3D™ Helix, eV3 Inc, United States of America; Cosmos Hypersoft™ 3D Helix, MicroVention Corporation, United States of America), detachable balloon (GOLDBAL2, Balt Extrusion, France), liquid embolic material (ethylene vinyl alcohol copolymer or Onyx®, eV3 Inc, United States of Americs), or parent artery sacrifice (endovascular or surgical). In the case of coiling, the Echelon™ microcatheter (eV3 Inc, United States of America) was advanced through the fistula and coil was deployed until there was no blood flow or significant reduction of blood flow in the fistula. In some cases, we used detachable balloon using the MABDTE microcatheter (Balt Extrusion, France). In indirect CCF, we initially opted for conservative treatment using external manual compression, unless there were some conditions that require endovascular treatment. In these cases, we mainly used a microcatheter to deliver the Onyx® liquid embolic material (eV3 Inc, United States of America). Several patients required multiple sessions before complete obliteration of fistula was achieved, while several others required additional surgical ligation of the carotid artery. In our centre, surgical ligation was opted after initial trials of endovascular treatment had failed and was achieved by proximal artery ligation.
Angiographic outcome was measured at the end of each procedure and defined as complete occlusion (CO) if the flow through the fistula is completely absent or diminished greatly and was expected to cease if thrombus was formed. Incomplete occlusion (IO) was defined if there is still high-flow through the fistula and spontaneous thrombosis was not expected without further treatment.
Results
A total of 23 patients were included in this study (Table 1), with 17 (73.9%) direct CCF (Barrow type A) and 6 (26.1%) indirect CCF (Barrow type B, C, D). In direct CCF there were 15 males (88.2%) and 2 females (11.8%), while in indirect CCF, there were 3 males (50%) and 3 females (50%). The mean age of patients were 32 years old. All of direct CCF had traumatic etiology, while most indirect CCF occur spontaneously, with only 1 case (16.6%) presumed to be of traumatic etiology. All patients presented with orbital symptoms as the initial complaint. The most common clinical manifestation in descending order were proptosis (n = 21, 91.3%), headache (n = 14, 60.8%), chemosis (n = 14, 60.8%), visual loss (n = 12, 52.2%), ophthalmoplegia (n = 12, 52.2%), conjunctival injection (n = 7, 30.4%), hemiparesis (n = 2, 8.7%), tinnitus (n = 2, 8.7%), and epistaxis (n = 1, 4.3%). Four (17.4%) patients had bilateral symptoms or signs.
All patients had an anterior drainage pattern through the superior ophthalmic vein (SOV). Other accompanying drainage patterns include the inferior petrosal sinus (IPS, n = 12, 52.1%), superficial middle cerebral vein (SMCV, n = 6, 26%), inferior ophthalmic vein (n = 5, 21.7%), superior petrosal sinus (n = 5, 21.7%), intercavernous sinus (n = 5, 21.7%), basal vein of Rosenthal (n = 3, 13.0%), pterygoid plexus (PP, n = 3, 13.0%), and the clival plexus (CP, n = 3, 13.0%). The drainage pattern of each CCF subtype is presented in Table 2.
All patients presented with an anterior drainage pattern, accompanied with orbital symptoms (proptosis, chemosis, conjunctival injection, visual loss). Of the six patients that had superior drainage via the SMCV, two had hemiparesis, and four complained of headache. Among the 3 patients with inferior drainage via the pterygoid plexus, one had severe epistaxis. Five patients had contralateral drainage, while four had bilateral symptoms. Of the two patients with tinnitus, both had drainage via the SOV, IPS and CP.
All patients with direct CCF (n = 17) were initially planned for endovascular treatment (Tables 1, 3). Of all the patients who underwent endovascular treatment for direct CCF (n = 17), 13 had complete occlusion (76.5%), 3 had incomplete occlusion (17.6%), and 1 (5.9%) procedure was cancelled due to difficult navigation. Five patients (29.4%) had parent artery occlusion, three with endovascular combined with surgical ligation, and two with endovascular technique. On the other hand, among the patients with indirect CCF (n = 6), conservative treatment were opted for 4 patients, and 2 patients were planned for endovascular treatment. Complete occlusion was achieved in 2 of the conservative treatment (50%), while none of the endovascular treatment had complete occlusion.
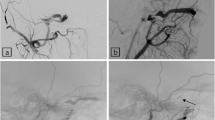
Of all direct CCF patients undergoing endovascular treatment, detachable balloon was used in three cases, with only one case that resulted in complete occlusion (Case example presented in Fig. 1). One case resulted only in incomplete occlusion, while in the third case, the balloon was slightly deflated so we combined it with coil to achieve complete fistula occlusion. Transarterial delivery of detachable coil is our preferred technique for direct CCF. With this technique, we achieved complete occlusion in 90% of cases (Case example presented in Fig. 2). In indirect CCF two cases were opted for endovascular treatment, both via transarterial route with liquid embolic agent and one patient combined with detachable coil.
Case 11, 17-year-old male developed progressive visual loss, proptosis, chemosis, cavernous sinus syndrome at his right eye (A) and left hemiparesis after motor vehicle accident. Initial angiogram (B lateral view; C anteroposterior view) revealed Barrow type A CCF draining via the superior ophthalmic vein, superficial middle cerebral vein (arrows), basal vein of Rosenthal (arrowheads), superior petrosal sinus (white arrowheads), and inferior petrosal sinus (white arrows). After two episodes of embolization with detachable coil, there was immediate resolution of proptosis and chemosis, and his angiogram showed flow reduction through the fistula
Discussion
In this study, we provide a description on the clinical and angiographic characteristic of CCF patients treated in our institution. Most direct CCF patients were young male patients (male:female ratio 15:2). This is consistent with the fact that head trauma is the most common etiology of direct CCF. There are several traumatic mechanisms that could cause CCF [1, 6] such as basilar skull fracture that could directly puncture or tear the cavernous segment of ICA. A retrospective study reported that 3.8% of basilar skull fracture patients had traumatic CCF, with the highest incidence found in fractures of the middle cranial fossa [7]. Interestingly, however, other studies have found no basilar skull fractures in traumatic CCF cases, suggesting a possible alternative mechanism besides direct tear from bony fragments. Some have suggested that the sudden intraluminal pressure increase within the ICA may be responsible for rupture in a majority of traumatic CCF cases. The most common site of rupture is in the proximal vertical segment and the horizontal portion of cavernous ICA [8]. In indirect CCF, male and female were affected equally (male:female ratio 1:1), and most cases were spontaneous.
All of our patients had orbital or neuro-ophthalmologic sign or symptoms. Proptosis was the most common sign and is the main chief complaint among our patients. Other clinical manifestations include headache, chemosis, visual loss, ophthalmoplegia, conjunctival injection, hemiparesis, tinnitus, and epistaxis. Understanding of the venous drainage pattern is crucial, as it correlates with the clinical manifestation and treatment strategy for CCF [4, 9]. The most common venous drainage pattern in direct CCF (type A) and indirect CCF (Type B, C, D) is via the superior or inferior ophthalmic vein. The SOV is the largest and most constant orbital vein, which under normal condition, drains venous blood toward the cavernous sinus [10]. In the case of CCF, high pressure within the cavernous sinus results in reversed venous blood flow in the SOV, leading to orbital vein congestion. Orbital vein congestion impairs aqueous humor drainage, which may lead to secondary glaucoma, and visual loss. This is also the mechanism responsible for the development of the classic Dandy’s triad of CCF, which are proptosis, chemosis, and orbital bruit [5, 11, 12]. This is consistent with the patients of our case series, who all presented with an anterior drainage pattern via the SOV, along with a high incidence of proptosis, chemosis and visual loss.
Venous drainage in other directions via the superior, inferior, posterior and contralateral routes were also noted in direct CCF, but were less common in indirect CCF. We stipulate that other drainage routes, especially superior and posterior routes, were recruited later on, as anterior and inferior drainage routes eventually fail to accommodate the pressure increase in the cavernous sinus. This is also implicated by other reports which noted that superior and posterior drainage were found only in long-standing high-flow CCF [9].
Involvement of either the superior drainage route via the superficial middle cerebral vein (SMCV) or the posterior drainage route via the basal vein of Rosenthal (BVR) can cause severe clinical manifestations, such as hemiparesis, seizure, or decreased level of consciousness, due to venous infarction in the cerebral convexity, deep nucleus or posterior fossa structure [9, 13, 14]. Hemiparesis can also be caused by the steal phenomenon in direct high flow fistula [15]. Inferior drainage via the pterygoid plexus, IPS, and clival plexus may cause epistaxis or cranial nerve palsy [6, 9]. Drainage via the intercavernous sinus can cause either ipsilateral, contralateral, or bilateral symptoms [6]. This variation is probably due to compartmentalization within the cavernous sinus [9]. We did not find posterior, superior or contralateral drainage in indirect CCF and not all patients with intercavernous drainage had bilateral clinical manifestations.
Endovascular treatment is now the preferred method for fistula closure, due to its effectiveness and safety profile [5, 16, 17]. Technical success rate of initial treatment varies between 60% and 100% in direct CCF and 77–86.5% in indirect CCF [17,18,19,20]. Ducruet and colleagues prospectively reviewed 100 cases of CCF, and found that the initial obliteration rate was 82% for direct CCF and 77% for indirect CCF, with 8% morbidity and 2% mortality. Additional 10% of patients with direct CCF demonstrated thrombosis in follow-up angiography [17]. Common complications include ischemia, cranial nerve palsy, and infection [16, 17].
In direct CCF, the preferred technique is transarterial delivery of detachable balloons, coil, or liquid embolic material [5, 10]. Detachable balloons used to be the preferred endovascular treatment method for fistula occlusion, but has now decreased in popularity due to several issues. Although relatively simple and inexpensive, it can be difficult to navigate into ideal position in patients with complex fistula anatomy [21]. We used detachable balloon in three cases, with one case that resulted in complete occlusion. Balloon might still be considered as an alternative to coil in cases of medium or large fistula which can accommodate full balloon inflation, since large fistulas require larger number of coils thereby leading to higher costs.
Transarterial delivery of detachable coil is our preferred technique for direct CCF, by which we achieved complete occlusion in 90% of cases, and reduced blood flow through the fistula in the remaining cases. Detachable coil is easy to adjust and allows precise placement of coil to ensure complete occlusion of fistula. This technique is effective and safe particularly in small fistula track or cavernous sinus [21]. The disadvantage is that detachable coil is relatively more expensive, is non-thrombogenic, and to achieve complete occlusion, multiple coils are usually required in offer to be packed dense enough. The advent of hydrogel coil partially relieved this issue [21]. Several complications associated with detachable coil include thromboemboli, parent vessel compromise, and dissection [5].
Several challenges may make it difficult to achieve complete fistula occlusion. To illustrate, in case 3, we were unable to achieve complete occlusion of fistula in one session due to the spacious compartment in front of fistula and the presence of septa near the fistula. After deploying multiple large coils, blood flow was significantly reduced but still persisted. Another challenge is in our institution, the number of coil use is limited by healthcare insurance coverage policies. The use of detachable balloon might solve this problem, but unfortunately detachable balloon was not available at that time. We decided to stage the treatment and the patient was planned for another session of embolization. In case 7, we initially attempted transarterial endovascular treatment using detachable coil, but we failed to navigate the microcatheter into ideal position within the cavernous sinus. Due to the fistula location in the posterior part of the cavernous internal carotid artery, and the high flow toward IPS, the microcatheter was always forced to point backward toward the IPS. We decided to withhold treatment, because if we proceeded, we risked diverting the blood flow to anterior, and exacerbate ocular symptoms. The patient was then followed and planned for another session of treatment. Difficult catheter navigation into the fistula was also reported by Ducruet and colleagues, one of which due to very small direct CCF and no adequate venous access [17].
If endovascular closure of the fistula failed, our usual approach is to combine with parent artery sacrifice either via surgical ligation or endovascular trapping. All the surgical ligation were done after one or two failed endovascular attempts, by proximal artery ligation provided the distal one was already occluded with endovascular approach. In case 1, despite the successful occlusion of fistula immediately after several sessions of endovascular embolization combined with surgical ligation, the follow-up angiogram revealed recanalization of the fistula and angiogenesis through the proximal ligation site.
For indirect CCF, we mainly opted for endovascular treatment if conservative treatment with external compression failed or if there were compelling indications. Four patients were planned for conservative treatment and two were planned for endovascular treatment. Spontaneous occlusion was achieved in 2 of 4 cases (50%) with conservative treatment, whereas both patients planned for endovascular treatment had incomplete occlusion. Endovascular treatment was performed using transarterial approach with EVOH and in one patient combined with coil. The reason for the failure to achieve complete occlusion was difficulty of access, due to the feeder artery’s small diameter. Several authors have suggested transvenous routes as the preferred technique in indirect CCF, and an alternative technique in direct CCF [5, 17]. Several reports showed good outcome with this technique, with good safety profile [22]. It has advantages over the transarterial route due to lower thromboembolic rates, higher cure rates, and the relatively simple procedure. The most common route is via the inferior petrosal sinus (IPS), and less common routes include the superior petrosal sinus, pterygoid plexus, or superior ophthalmic vein [5]. Despite the preference of transvenous route of endovascular treatment for indirect CCF in most literature, we opted transarterial route in both cases due to the difficulty of access caused by thrombosed IPS in one patient and small and stenotic IPS in the other. The patients were regularly monitored afterward, while being advised to perform manual external compression.
The result of our study has some similarities to the study by Arifin and colleagues, which described endovascular treatment outcome of 31 CCF patients in Indonesia. In direct CCF, they achieved complete occlusion in all patients treated with detachable coil but only in 40% of cases with detachable balloon. In their study, detachable coil were delivered either transarterial or transvenous, while in our study, we used only transarterial route. In one case of indirect CCF treated with endovascular treatment using EVOH, the occlusion was incomplete [18]. Another study by Hamid and colleagues reported 26 patients with CCF, with 23 direct and 3 indirect CCF. The difference from our study was they mainly used detachable balloons (19 cases). The technical success rate of endovascular treatment was 92.3%. In one case, the detachable balloon deflated 2 h after deployment, which required them to deploy another larger balloon [16].
The time from symptom onset to diagnosis in our data set varied from between 3 days to as long as 4 years. Time from symptom onset to treatment plays a significant role in patient outcome [7]. The patient described in case 1, who had the longest delay to treatment indeed proved to be the most difficult to treat. After multiple endovascular treatment with coil combined with surgical ligation, the fistula still persisted through angiogenesis, connecting the part of the vessel proximal to ligation site with its distal counterpart. This case emphasizes the need for strong collaborations with primary care physicians, or other departments, for screening of CCF cases and immediate consultation with experts to achieve good clinical outcome.
Conclusion
In our population, the most common clinical manifestations of CCF are orbital manifestations, such as proptosis, chemosis, and visual loss in addition to headache, and neuro-opthalmologic symptoms. These clinical manifestations are related to the venous drainage pattern, with the anterior route being the most frequently encountered pattern in this study. Posterior, superior, and contralateral routes were absent in indirect CCF. Endovascular treatment is an effective modality for both direct and indirect CCF. Although the transarterial route is effective to achieve complete fistula closure for direct CCF, it is less effective in indirect CCF. The challenges we face during endovascular treatment are mainly due to the unfavourable location of the fistula or the anatomy of the cavernous sinus and its drainage pattern. A strong collaborative approach with other clinicians may be needed to achieve complete occlusion of fistula and improve the outcome for patients.
Availability of data and materials
All data sets generated during the study are available by request to the corresponding author.
Abbreviations
- BVR:
-
Basal vein of Rosenthal
- CCF:
-
Carotid cavernous fistula
- CP:
-
Clival plexus
- DSA:
-
Digital subtraction angiography
- ICA:
-
Internal carotid artery
- IOV:
-
Inferior ophthalmic vein
- IPS:
-
Inferior petrosal sinus
- PP:
-
Pterygoid plexus
- SOV:
-
Superior ophthalmic vein
- SMCV:
-
Superficial middle cerebral vein
- SPS:
-
Superior petrosal sinus
References
Ellis J, Goldstein H, Conolly E, Meyers P. Carotid-cavernous fistulas. Neurosurg Focus. 2012;32(5):E9.
Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985;62(2):248–56.
Thomas A, Chua M, Fusco M, Ogilvy C, Tubbs R, Harrigan M, et al. Proposal of venous drainage-based classification system for carotid cavernous fistulae with validity assessment in a multicenter cohort. Neurosurgery. 2015;77(3):380–5.
Leone G, Renieri L, Enriquez-Marulanda A, Dmytriw AA, Nappini S, Laiso A, et al. Carotid cavernous fistulas and dural arteriovenous fistulas of the cavernous sinus: validation of a new classification according to venous drainage. World Neurosurg. 2019;128:e621–31.
Korkmazer B, Kocak B, Tureci E, Islak C, Kocer N, Kizilkilic O. Endovascular treatment of carotid cavernous sinus fistula: A systematic review. World J Radiol. 2013;5(4):143–55.
Fattahi TT, Brandt MT, Jenkins WS, Steinberg B. Traumatic carotid-cavernous fistula: pathophysiology and treatment. J Craniofac Surg. 2003;14(2):240–6.
Liang W, Xiaofeng Y, Weiguo L, Wusi Q, Gang S, Xuesheng Z. Traumatic carotid cavernous fistula accompanying basilar skull fracture: a study on the incidence of traumatic carotid cavernous fistula in the patients with basilar skull fracture and the prognostic analysis about traumatic carotid cavernous fistula. J Trauma Acute Care Surg. 2007;63(5):1014–20.
Helmke K, Krüger O, Laas R. The direct carotid cavernous fistula: a clinical, pathoanatomical, and physical study. Acta Neurochir (Wien). 1994;127(1–2):1–5.
Aralasmak A, Karaali K, Cevikol C, Senol U, Sindel T, Toprak H, et al. Venous drainage patterns in carotid cavernous fistulas. Int Sch Res Not. 2014;2014:89.
Harrigan M, Deveikis J. Handbook of Cerebrovascular Disease and Neurointerventional Technique. New York: Humana Press; 2018.
Ropper A, Samuels M, Klein J, Prasad S. AdamAdams and Victor’s PRINCIPLES OF NEUROLOGY. eleventh. New York: McGraw Hill; 2019.
Henderson A, Miller N. Carotid-cavernous fistula: current concepts in aetiology, investigation, and management. Eye. 2018;32(2):164–72.
Murata H, Kubota T, Murai M, Kanno H, Fujii S, Yamamoto I. Brainstem congestion caused by direct carotid-cavernous fistula—case report—. Neurol Med Chir (Tokyo). 2003;43(5):255–8.
Suh DC, Lee JH, Kim SJ, Chung SJ, Choi CG, Kim HJ, et al. New concept in cavernous sinus dural arteriovenous fistula: correlation with presenting symptom and venous drainage patterns. Stroke. 2005;36(6):1134–9.
Kato M, Ikegame Y, Toyoda I, Ogura S, Kitajima H, Yoshimura S, et al. Hemispheric laminar necrosis as a complication of traumatic carotid-cavernous sinus fistula—case report—. Neurol Med Chir (Tokyo). 2009;49(1):26–9.
Hamid RS, Ul Haq T, Shamim MS, Kazim SF, Salam B. Endovascular approach as primary treatment for traumatic carotid cavernous fistula: local experience from Pakistan. JPMA J Pak Med Assoc. 2011;61(10):989.
Ducruet AF, Albuquerque FC, Crowley RW, McDougall CG. The evolution of endovascular treatment of carotid cavernous fistulas: a single-center experience. World Neurosurg. 2013;80(5):538–48.
Arifin MT, Akbar MA, Illyasa W, Prihastomo KT. Neuro-endovascular intervention in traumatic carotico-cavernous fistulae: a single-center experience. Int J Gen Med. 2020;13:917.
Alexander MD, Halbach VV, Hallam DK, Cooke DL, Ghodke BV, Dowd CF, et al. Long-term outcomes of endovascular treatment of indirect carotid cavernous fistulae: superior efficacy, safety, and durability of transvenous coiling over other techniques. Neurosurgery. 2019;85(1):E94-100.
Barber SM, Rangel-Castilla L, Zhang YJ, Klucznik R, Diaz O. Mid-and long-term outcomes of carotid-cavernous fistula endovascular management with Onyx and n-BCA: experience of a single tertiary center. J Neurointerventional Surg. 2015;7(10):762–9.
Luo CB, Teng MMH, Chang FC, Lin CJ, Guo WY, Chang CY. Transarterial detachable coil embolization of direct carotid-cavernous fistula: immediate and long-term outcomes. J Chin Med Assoc. 2013;76(1):31–6.
Morton RP, Tariq F, Levitt MR, Nerva JD, Mossa-Basha M, Sekhar LN, et al. Radiographic and clinical outcomes in cavernous carotid fistula with special focus on alternative transvenous access techniques. J Clin Neurosci. 2015;22(5):859–64.
Acknowledgements
We would like to thank all patients who have participated in this study.
Funding
The study received no specific funding.
Author information
Authors and Affiliations
Contributions
AB conceptualized and supervised the study, collected, and analyzed the data, drafted and finalized the manuscript. AG, JP, and GS performed the data collection and analysis, revised, and finalized the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the Faculty of Medicine, Hasanuddin University (Ethics number UH20090539).
Consent for publications
All subjects have provided consent for publication.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bahar, A., Pranata, J., Gunawan, A. et al. Clinical characteristics, angiographic findings and treatment outcomes of carotid cavernous fistula in Makassar, Indonesia: a single-centre experience. Egypt J Neurol Psychiatry Neurosurg 59, 29 (2023). https://doi.org/10.1186/s41983-023-00630-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-023-00630-w