Abstract
Background
Degenerative lumbar spine pathologies such as spinal stenosis and disc herniation constitute the most common causes of back pain and radiculopathy. After the introduction of the operative microscope in the 1970s, microscopic discectomy has become the gold standard of treatment for herniated lumbar disc by many surgeons. A tubular endoscopic approach was first described in 1997 by Foley and Smith as a new minimally invasive technique alternative to open surgical techniques. The objective of this study is to evaluate the outcome and efficacy of microscopic discectomy and endoscopic discectomy for the management of herniated lumbar disc as regard the clinical results, operation time, intraoperative blood loss, and postoperative complications.
Results
This is a retrospective study of 40 patients, with symptomatic lumbar disc herniation managed by the authors either by microscopic discectomy (MD) (n = 20) or by endoscopic discectomy (ED) (n = 20). Patients were followed up and postoperative data was recorded at 1, 6, 12 months after surgery. Clinical scoring systems included the Visual Analog Scale (VAS) for the preoperative and the postoperative low back ache (VAS-B) as well as preoperative and postoperative sciatic pain (VAS-S), in addition to the evaluation of the modified Japanese Orthopedic Association scale (mJOA) over the same time intervals. Significant postoperative improvement in clinical and functional outcome of the two groups was noted, including a statistically significant improvement in postoperative VAS-B and VAS-S as well as the mJOA scores in comparison to the preoperative data (p = 0.001). There was a statistically significant shorter operative time, less blood loss and less rate of operative complications recorded in the microscopic discectomy group as compared with endoscopic discectomy group in our study.
Conclusions
Our study concluded that microscopic lumbar discectomy is as safe and effective as endoscopic lumbar discectomy for the management of symptomatic lumbar disc herniation with a low complication rate, less operative blood loss and operative time. Larger series and further studies would be yet considered with longer follow-up periods.
Similar content being viewed by others
Background
The low back ache and sciatic pain constitute the uncomfortable symptoms most commonly accounting for seeking neurosurgical advice among patients with lumbar disc herniation and subsequent nerve root compression; the rate of lumbar disc prolapse is approximately 2% to 5% in general population [1].
Although most patients with lumbar disc herniation can achieve satisfactory results through conservative management including medical treatment and possibly physical therapy, yet surgical management is still considered particularly for patient with poor response to such conservative approaches [2].
Surgical modalities include open laminectomy and discectomy, microscopic discectomy (MD), and endoscopic discectomy (ED) [3]. The first successful case of open laminectomy and discectomy was described in 1934 [4]. After the introduction of the operative microscope in the 1970’s, microscopic discectomy has become the gold standard for the surgical management of a herniated lumbar disc and has been widely accepted by surgeons [5, 6]. Later on, a variety of minimally invasive approaches was also introduced, and a tubular endoscopic approach, was first described in 1997 by Foley and Smith as a new minimally invasive technique alternative to open surgical techniques gaining a notable popularity among spine surgeons This kind of procedure also provided the advantage of being possibly carried out under the condition of local anesthesia [7]. Despite many researchers have compared the safety and effectiveness of both ED and MD for the management lumbar disc herniation and revealed conflicting outcomes; many systematic reviews described the clinical results of both MD and ED as comparable [8].
The objective of this study is to evaluate the outcome and efficacy of microscopic discectomy and endoscopic discectomy for the management of herniated lumbar disc as regard the clinical results, operation time, intraoperative blood loss, and postoperative complications in order to offer basis for the best clinical approach.
Methods
This is a retrospective study of 40 patients, with symptomatic lumbar disc herniation managed by the authors either by microscopic discectomy (MD) (n = 20) or by endoscopic discectomy (ED) (n = 20) conducted between August 2019 to November 2021. Patients enrolled in this study were followed up and postoperative data was recorded at 1, 6, 12 months after surgery.
Our study inclusion criteria involved patients with symptomatic lumbar disc herniation including sciatica with or without low back pain and/or motor power affection; with radiological results confirming the diagnosis including Plain X-rays (PXR) and Magnetic resonance imaging (MRI). Included subjects should have shown a failed conservative management plan before surgery is decided. Inclusion criteria also involved patients with ipsilateral disc herniation at single level.
Whereas our study exclusion criteria involved asymptomatic patients, patients who were candidates for conservative management trial in absence of a possible motor weakness, sphincteric disturbance, and saddle anesthesia and showed a subsequent favorable outcome, patients presented with only low back pain without sciatica, associated lumbar spinal canal stenosis, recurrent lumbar disc herniation cases, spinal segmental instability evident on preoperative dynamic PXR lumbosacral spines, and patients with morbid obesity.
Preoperative clinical evaluation included Patients’ demographics (age, sex), relevant past medical and surgical history including that of a relevant back trauma and other comorbidities (for example hypertension, diabetes mellitus, chronic alcoholism, blood thinners), in addition to patients’ Clinical presentation and its duration including neurological examination and the assessment of Visual analogue scale [VAS] for both back (VAS-B) and Sciatic pain (VAS-S) and the assessment of the modified Japanese Orthopedic Association (mJOA) score for every patient [9].
Preoperative radiological investigations included PXR antero-posterior and lateral [standing and dynamic] views to evaluate the anatomy of the pedicles, transverse processes, laminae, and facet joints; or the presence degenerative changes; neural foraminal dimensions, and bone density. Also, to assess stability of the spine on dynamic views where lumbar instability is considered as more than 4.5 mm of translation, and/or 15° to 25° of angular motion between adjacent segments.
The preoperative MRI of the lumbosacral spine without Gadolinium enhancement allowed anatomical evaluation of the spine and spinal canal, nerve roots, and spinal ligaments complex.
Concerning the surgical technique, an informed consent was obtained from all patients or by their first-degree relatives prior to surgery.
This study was completed by the authors according to the standard medical process. General anesthesia was applied for both study groups, and all patients were kept in a prone position.
The MD group
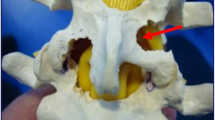
The surgical site was confirmed by immediate preoperative lateral fluoroscopy imaging then accordingly a midline skin incision of 2 cm was applied. The skin was then retracted laterally and guide wire and sequential dilators were placed under the control of lateral fluoroscopy. A tubular retractor was then attached and secured to a flexible arm. Discectomy and foraminotomy were then performed under the microscope (OPMI Vario S88, Zeiss, Germany) then ultimately drainage tubes were placed and secured.
The ED group
In accordance still with the guidance of C-arm fluoroscopy, from the entrance point, a 18-gauge needle was inserted from the entry point before a 22-gauge needle was inserted into the herniated intervertebral disc through the 18-gauge needle, then the contrast agent was injected into the intervertebral disc. Endospine Destandau system, by Storz, Germany was used, sequential insertion of the dilators was done to allow adequate exposure then the blue degenerated disc material is removed by the endoscopic forceps until a full nerve decompression is achieved.
Operative time, complications, and the amount of blood loss were recorded for all the study subjects.
Finally, Closure was performed in a routine fashion. All patients received prophylactic antibiotics perioperatively, and they were transferred to the ward where they could start ambulation on the same day with no need of using a lumbar corset upon ambulation. The suction drains were removed on the second postoperative day.
Clinical outcome was assessed through evaluating the patients’ postoperative neurological outcome by recording the postoperative VAS-B, VAS-S, and mJOA scores for all patients at 1, 6 and 12 months after surgery and comparing the results to preoperative scores.
Data analysis was performed using the Statistical Package for Social Sciences, version 19.0 released 2010 (SPSS Inc, Chicago, IL, USA), and a p value < 0.05 was considered statistically significant. Shapiro–Wilk test was used to evaluate normal distribution of continuous data. Continuous variables are presented as mean and SD values. Categorical variables are presented as numbers of cases and percentages. Chi-square test or Fisher’s exact test was used to analyze categorical variables, while student t test was used for comparing Continuous variables between the two study groups.
Results
All the patients’ preoperative data was studied and analyzed. There were 32 (80%) males and 8 (20%) female patients. Their age ranged from 30 and 60 years, with a mean age of 48.4 (± 7.14 SD) years in the MD group, and a mean age of 45.7 (± 6.41 SD) years in the ED group. Table 1 describes the demographic data and risk factors of the studied patients. The commonest recorded medical risk factor was hypertension which was noted in 16 cases (40%), followed by Diabetes mellitus noted in 8 patients (20%). There was no statistically significant difference found between both groups regarding demographic data of the studied patients.
In MD group subjects, the pathological level was L4–5 in 10 (50%) patients, L5–S1 in 6 (30%) patients, and L3–4 in also 4 (20%) patients; in contrast to 12 (60%) patients in L4–5 level, 5 (25%) patients in L5–S1 level and 3 (15%) patients in L3–4 level among the ED group.
Low back pain was a presenting symptom in all MD group subjects in contrast to 18 (90%) patients among the ED group subjects; whereas sciatic pain was a presenting symptom in all subjects included in our study. The left side was pathological in 16 (80%) patients and the right side accounted for 4 (20%) patients in the MD group; in the ED group, the left side was involved in 15 (75%) patients, and the right side in 5 (25%) patients. Sensory affection was recorded in 15 (75%) patients in the MD group and 14 (70%) patients in the ED group. The prolapsed lumbar disc site was mainly posterolateral among the MD group, being noted in 12 (60%) patients, while it was mainly lateral among the ED group as it was recorded in 13 (65%) patients (Table 2).
Both study groups showed a significant postoperative clinical improvement following surgery denoting a favorable response to both surgical modalities. Considering VAS-B evaluation, the recorded mean values for the preoperative assessment, at the first, sixth, and twelfth months follow-up showed a statistically highly significant improvement of values on comparing between the preoperative and the postoperative results throughout the follow up intervals (p = 0.001); the mean values for VAS-B improved from 6.35 ± 1.14 pre-operatively to 1.2 ± 0.52 twelve months after surgery in the MD group, and from 8.6 ± 1.16 pre-operatively to 1.8 ± 1.32 twelve months after surgery in the ED group (Table 3).
Similarly, the mean values for VAS-S improved from 9.75 ± 0.44 pre-operatively to 0.35 ± 0.49, 12 months after surgery in the MD group, and from 8.58 ± 0.93 pre-operatively to 1.8 ± 1.36, 12 months after surgery in the ED group. These recorded mean values for the preoperative assessment, at the 1st, 6th, and 12th months follow-up subsequently revealed a statistically highly significant improvement of values on comparing between the preoperative and the postoperative results throughout the follow up intervals (p = 0.001) (Table 4).
Table 5 states that on evaluating both the MD and the ED groups regarding the preoperative and the postoperative mJOA score mean values, there was a statistically highly significant improvement of values throughout the follow up intervals following surgery (p = 0.001); the mean values for mJOA improved from 8.1 ± 2.1 pre-operatively to 27.35 ± 1.79 twelve months after surgery in the MD group, and from 13.4 ± 1.5 pre-operatively to 23.1 ± 1.16 twelve months after surgery in the ED group. These recorded mean values for the preoperative assessment, at the 1st, 6th, and 12th months follow-up subsequently revealed a clinically significant improvement on comparing between the preoperative and the postoperative results throughout the follow up intervals in both groups.
Table 6 denotes that there was a statistically highly significant difference between both groups considering the operative time; the mean value for the microscopic discectomy surgery was 65.75 ± 7.99 min (min) in contrast to a mean value of 139.3 ± 55.0 min. for the endoscopic surgery; similarly, there was also a statistically highly significant difference between both groups considering the intraoperative blood loss, being 47.25 ± 14.44 ml (ml) and 88.8 ± 22.1 ml in both groups respectively.
However, there was no statistically significant difference between both groups considering the incidence of postoperative complications, two cases were recorded among the MD discectomy group in contrast to three cases among the ED group. A single patient of each group developed temporary motor weakness and sensory affection on the same side of the operation immediately after surgery in the absence of a distinctive intraoperative event or neural injury, both had conservative medical management and showed complete recovery of motor power within three weeks after surgery.
Unintended durotomy also took place in a single patient in each group, a small dural tear was identified intraoperatively in the ED case during root retraction, the dura was not sutured yet a fat graft was applied upon the minute cerebrospinal fluid (CSF) leaking site, and no CSF leak was noticed, this could be attributed to the fall back of tissues which created a physical barrier to the hydrostatic pressure of the intradural space and the small gap is closed so well that there is no space for CSF to accumulate. The MD case unintended durotomy was identified during flavectomy where a small dural leaflet was caught in a Kerrison rongeur, the tear was repaired intraoperatively via dural sutures augmented by a fat graft, then a drain was kept superior to the fascia in a non dependent location with no suction and a stitch was taken at its place when removed; no subsequent collection or leakage was recorded in any of the two cases.
One patient of the ED group had postoperative superficial wound infection that was cured in less than two weeks using oral antibiotics and frequent wound dressings.
Discussion
Lumbar disc prolapse is the most common spinal pathology affecting young age group, particularly between 30 and 50 years old; it accounts for a variety of symptoms including back pain, radicular pain with or without neurological deficit, and eventually patients refractory to conservative management for a minimum of 4 weeks, or having their activities of daily living affected are dealt surgically [10,11,12]. Discectomy performed either through an open approach or by minimally invasive techniques remains the gold standard management solution including hemilaminotomy, flavectomy and discectomy; the success rates of discectomy in the treatment of sciatic pain has been reported to range between 50 and 98% [13,14,15]. Advantages of minimal invasive surgery includes less perioperative pain, early ambulation, shorter hospital stay and early return to work with smaller incision [16,17,18]. Minimally invasive tubular lumbar endoscopic discectomy is a refinement of the standard open microscopic lumbar discectomy technique. Traditional MD surgery requires muscles dissection and retraction which might induce iatrogenic morbidity of the soft tissues in spite of providing greater visualization of dural sac, direct visualization of anatomic structures and obtaining the optimal angle for disc removal; however, ED is associated with tubular retractors which minimizes the tissue injury and ensures that deeper tissues are less exposed to potential pathologic organisms due to restricted surgical field. Despite these claims there is little support in the literature to justify the adoption of ED over standard MD and the issue remains controversial.
It is therefore necessary to discuss the clinical efficacies of both procedures to generate data that might aid surgeons make a better clinical judgement and develop optimal surgical plan. In our study, we tried to evaluate the clinical outcome and efficacy of both microscopic and endoscopic discectomy as minimally invasive approaches for the management of herniated lumbar disc and assess our results in contrast to the literature.
Our study was conducted on 40 patients with symptomatic unilateral lumbar disc prolapse as confirmed on preoperative MRI to whom surgical management was performed through either microscopic or endoscopic approaches then assessed postoperatively.
The mean age of our study cases was 45.7 years; there was a male predominance as of 80% males and 20% female patients.
Follow up assessment for our patients was conducted through the evaluation of the visual analogue score for both back pain and radicular pain, also we used the modified Japanese orthopedic association score evaluation system for lower back pain syndromes.
The mean value of the preoperative VAS for the back pain was recorded 8.6 ± 1.16 for the endoscopic cases and 6.35 ± 1.14 for the microscopic cases, one month postoperatively, there was a statistically highly significant improvement in these mean values being 1.85 ± 1.2 and 2.45 ± 0.51 respectively, yet there was no statistically significant difference on comparing between the two groups; whereas the VAS-B mean values at the end of the postoperative follow up, twelve months after surgery were still showing a statistically highly significant improvement in both groups compared to the preoperative values, they were recorded 1.8 ± 1.32 and 1.2 ± 0.52 respectively denoting a significant postoperative clinical improvement and a favorable surgical outcome, yet there was still no statistically significant difference between both groups.
Our results came in accordance with those stated by Teli et al. [19], and Asati et al. [20]; however, other studies as in Anderson [21] and Arts et al. [22] described a higher incidence of postoperative low back pain in microscopic discectomy in comparison with the endoscopic approach.
Similarly, the mean values for VAS-S 1 month after surgery showed a statistically significant improvement for both groups when compared to the preoperative values, the MD group mean values improved from 9.75 ± 0.44 pre-operatively to 2.15 ± 0.37, 1 month after surgery, in contrast to 8.58 ± 0.93 and 1.2 ± 1.61 respectively in the ED group. Eventually there was a statistically highly significant improvement of VAS-S values in both groups 1 year after surgery compared to the preoperative mean values, being 0.35 ± 0.49 in the MD group, and 1.8 ± 1.36 in the ED group. No statistically significant difference between both groups were recorded.
In their study comparing the clinical outcome of both endoscopic and microscopic discectomy, Yang et al. [23] concluded that there were significant intergroup differences in VAS-B recorded values 2 years after surgery being much better among the ED group, the rate of excellent or good outcome was 90.32% with ED group and 78.95% with MD group; they presumed the reason could be because of the lesser surgical trauma in the ED group. However, similar to our study, they found the intergroup differences in VAS-S score mean values two years following surgery to be statistically non significant. Other studies were also in accordance with our results concluding that sciatica in both groups significantly improved and remained satisfactory at the 24-month follow up following surgery [24,25,26].
The mJOA score mean values markedly improved in both groups after surgery, it improved from 8.1 ± 2.1 pre-operatively to 20 ± 2.53 among the MD group 1 month postoperatively, and from 13.4 ± 1.5 to 22.4 ± 2.1 among the ED group, indicating a statistically highly significant improvement; progressive improvement was noted was also noted in both groups 1 year postoperatively where mJOA mean values were recorded 27.35 ± 1.79 and 23.1 ± 1.16 in both groups respectively. These findings point to a significant clinical improvement on comparing between the preoperative and the postoperative results throughout the follow up intervals in both groups. The difference in mJOA score mean values between both groups was statistically non significant. Liu et al. [26] also noted a significant postoperative improvement in the JOA scores, VAS scores of low back pain and leg pain at the last study follow up when compared to the preoperative correlates in all the study groups, also, there was no statistically significant difference among the study groups in JOA scores, and VAS scores for leg pain.
For our patients who underwent endoscopic discectomy, the mean operative time was 139.3 ± 55.0 min while for those who underwent micro-discectomy it was 65.75 ± 7.99 min, this statistically highly significant difference could be attributed to our progressively growing learning curve and surgical experience regarding the endoscopic approach, since we noticed that in our initial ED cases have recorded a mean operative time of 173 min while in late cases it was about 93 min. Comparing our results with the literature, Muramatsu et al. [27] recorded a mean operative time of 105.7 min for their ED cases, whereas Asati et al. [20] reported a significantly shorter operative time being 82.3 min in the ED group compared to our results, in contrast to 71.5 min in the MD group which is close to our study results for the same group. Mayer and Brock [28] noted a significantly shorter operative time of 40.7 ± 11.3 in the ED group and 58.2 ± 15.2 min in the MD group.
The mean values of intraoperative blood loss in our study subjects also revealed a statistically highly significant difference on comparing between both groups. We recorded 47.25 ± 14.44 ml (ml) in the MD group and 88.8 ± 22.1 ml in the ED group, and despite of this significant difference, yet no patient needed intraoperative blood transfusion in any of the groups which is considered a rare event in lumbar surgery; the average blood loss in endoscopic approach according to Asati et al. [20] appeared similar to our recorded value being 82.3 ml, while Wu et al. [29] study results appear significantly less being 44 ml.
Considering the incidence of operative complications, our study concluded there was no statistically significant difference between both groups. Yang et al. [23] reported a higher incidence of complications with ED than with MD, yet they described this difference to be non significant and similar to our study results, no major complications were reported. In their MD group, there was a single case of a dural tear that was repaired during surgery, five cases in their ED group and one case in the MD group had postoperative paresthesia, but the symptom disappeared within 4 weeks after treatment with oral mecobalamin. Phan et al. [30] also noted no statistically significant difference in overall complications, dural tears, root injury or wound infection.
Conclusions
Our study concluded that microscopic lumbar discectomy is as safe and effective as endoscopic lumbar discectomy for the management of symptomatic lumbar disc herniation with a low complication rate, less operative blood loss and operative time. Larger series and further studies would be yet considered with longer follow-up periods.
Availability of data and materials
All the raw data and results of the statistical analysis are available with the authors and ready to be shared with authorized personnel upon request, however, for reasons of patency protection it was not submitted with the manuscript.
Abbreviations
- MD:
-
Microscopic discectomy
- ED:
-
Endoscopic discectomy
- N:
-
Number of patients
- PXR:
-
Plain X-rays
- MRI:
-
Magnetic resonance imaging
- VAS:
-
Visual analogue scale
- VAS-B:
-
Visual analogue scale for low back pain
- VAS-S:
-
Visual analogue scale for sciatic pain
- mJOA:
-
The modified Japanese Orthopedic Association score
- SPSS:
-
SPSS Statistical package for the social sciences
- SD:
-
Standard deviation
- pre:
-
Preoperatively
- post:
-
Postoperatively
- min:
-
Minutes
- ml:
-
Milliliters
- CSF:
-
Cerebrospinal fluid
References
Zhong M, Liu JT, Jiang H, Mo W, Yu PF, Li XC, Xue RR. Incidence of spontaneous resorption of lumbar disc herniation: a meta-analysis. Pain Phys. 2017;20(1):E45–52.
Hofstee DJ, Gijtenbeek JM, Hoogland PH, van Houwelingen HC, Kloet A, Lötters F, Tans JT. Westeinde sciatica trial:randomized controlled study of bed rest and physiotherapy for acute sciatica. J Neurosurg. 2002;96(1 Suppl):45–9.
Peul WC, Van Houwelingen HC, van den Hout WB, Brand R, Eekhof JAH, Tans JTJ, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356(22):2245–56.
Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. J Neurosurg. 1964;21(1):74–81.
Clark AJ, Safaee MM, Khan NR, Brown MT, Foley KT. Tubular microdiscectomy: techniques, complication avoidance, and review of the literature. Neurosurg Focus. 2017;43(2):E7.
Yasargil MG. Microsurgical operation of herniated lumbar disc. In Lumbar disc adult hydrocephalus. New York: Springer; 1977. p. 81.
Destandau J. Technical features of endoscopic surgery for lumbar disc herniation: 191 patients. Neurochirurgie. 2004;50(1):6–10.
Yao Y, Zhang H, Wu J, et al. Minimally invasive transforaminal lumbar interbody fusion versus percutaneous endoscopic lumbar discectomy: revision surgery for recurrent herniation after microendoscopic discectomy. Comparative Study. 2017;99:89–95.
Benzel EC, Lancon J, Kesterson L, Hadden T. Cervical laminectomy and dentate ligament section for cervical spondylotic myelopathy. J Spinal Disord. 1991;4(3):286–95.
Jensen MP, Karoly P, O’Riordan EF, Bland F Jr, Burns RS. The subjective experience of acute pain. An assessment of the utility of 10 indices. Clin J Pain. 1989;5(2):153–9.
Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine (Phila Pa 1976). 2008;33(22):2464–72.
Nikaido T, Kikuchi S, Yabuki S, Otani K, Konno S. Surgical treatment assessment using the Japanese orthopedic association cervical myelopathy evaluation questionnaire in patients with cervical myelopathy: a new outcome measure for cervical myelopathy. Spine (Phila Pa 1976). 2009;34(23):2568–72.
Javedan S, Sonntag VKH. Lumbar disc herniation: microsurgical approach. Neurosurgery. 2003;52(1):160–4.
McGirt MJ, Ambrossi GLG, Datoo G, Sciubba DM, Witham TF, Wolinsky J-P, et al. Recurrent disc herniation and long-term back pain after primary lumbar discectomy: review of outcomes reported for limited versus aggressive disc removal. Neurosurgery. 2009;64(2):338–45.
Tait MJ, Levy J, Nowell M, Pocock C, Petrik V, Bell BA, et al. Improved outcome after lumbar microdiscectomy in patients shown their excised disc fragments: a prospective, double blind, randomised, controlled trial. J Neurol Neurosurg Psychiatry. 2009;80(9):1044–6.
Kotil K, Tunckale T, Tatar Z, Koldas M, Kural A, Bilge T. Serum creatine phosphokinase activity and histological changes in the multifidus muscle: a prospective randomized controlled comparative study of discectomy with or without retraction. J Neurosurg Spine. 2007;6(2):121–5.
Schick U, Döhnert J, Richter A, König A, Vitzthum H. Microendoscopic lumbar discectomy versus open surgery: an intraoperative EMG study. Eur spine J. 2002;11(1):20–6.
Shin DA, Kim KN, Shin HC. The efficacy of microendoscopic discectomy in reducing iatrogenic muscle injury. J Neurosurg Spine. 2008;8(1):39–43.
Teli M, Lovi A, Brayda-Bruno M, Zagra A, Corriero A, Giudici F, et al. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur spine J. 2010;19(3):443–50.
Asati S, Jain S, Kundnani VG. Tubular discectomy versus conventional microdiscectomy for the treatment of lumbar disc herniation: a comparative study. J Minim Invasive Spine Surg Tech. 2020;5(2):51–6.
Anderson PA. Tubular discectomy resulted in greater leg and back pain and a lower rate of recovery than conventional microdiscectomy for sciatica. J Bone Jt Surg Am. 2010;92(2):475.
Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RHMA, Peul WC, et al. Tubular diskectomy vs conventional microdiskectomy for sciatica: a randomized controlled trial. JAMA. 2009;302(2):149–58.
Yang F, Ren L, Ye Q, Qi J, Xu K, Chen R, Fan X. Endoscopic and microscopic interlaminar discectomy for the treatment of far-migrated lumbar disc herniation: a retrospective study with a 24-month follow-up. J Pain Res. 2021;14:1593–600.
Choi KC, Kim JS, Park CK. Percutaneous endoscopic lumbar discectomy as an alternative to open lumbar microdiscectomy for large lumbar disc herniation. Pain Phys. 2016;19(2):E291–300.
Li Q, Zhou Y. Comparison of conventional fenestration discectomy with transforaminal endoscopic lumbar discectomy for treating lumbar disc herniation: minimum 2-year long-term follow-up in 1100 patients. BMC Musculoskelet Disord. 2020;21(1):628.
Liu X, Yuan S, Tian Y, et al. Comparison of percutaneous endoscopic transforaminal discectomy, microendoscopic discectomy, and microdiscectomy for symptomatic lumbar disc herniation: minimum 2-year follow-up results. J Neurosurg Spine. 2018;28(3):317–25.
Muramatsu K, Hachiya Y, Morita C. Postoperative magnetic resonance imaging of lumbar disc herniation: comparison of microendoscopic discectomy and Love’s method. Spine (Phila Pa 1976). 2001;26(14):1599–605.
Mayer HM, Brock M. Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993;78:216–25.
Wu X, Zhuang S, Mao Z, Chen H. Microendoscopic discectomy for lumbar disc herniation: surgical technique and outcome in 873 consecutive cases. Spine (Phila Pa 1976). 2006;31(23):2689–94.
Phan K, Xu J, Schultz K, Alvi MA, Lu VM, Kerezoudis P, Maloney PR, Murphy ME, Mobbs RJ, Bydon M. Full-endoscopic versus micro-endoscopic and open discectomy: a systematic review and meta-analysis of outcomes and complications. Clin Neurol Neurosurg. 2017;154:1–12.
Acknowledgements
Not applicable.
Funding
The authors received no external funding for the design of the study, for the collection, analysis and interpretation of data or for writing the manuscript.
Author information
Authors and Affiliations
Contributions
OEFA: main author and corresponding author. STEM: co-author. AMES: co-author. The study design, execution and follow up of the clinical cases, data analysis and results formulation, and writing of the manuscript, were all the joint work of all the authors. The manuscript has not been published, or submitted for publication elsewhere. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was conducted upon obtaining the approval of the ethical committee of the Faculty of Medicine- Ain Shams University, in July 2019.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Reference number
Not available.
Informed consent
Since this study involved human subjects, an informed written consent was signed and acquired from all the participants or their legal guardians in accordance with the ethical committee recommendations. This work was entirely carried out by the authors without any external contributions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmed, O.E.F., Molla, S.T.E. & Sabaa, A.M.E. Minimally invasive surgical management of symptomatic lumbar disc herniation: can the endoscope replace the microscope?. Egypt J Neurol Psychiatry Neurosurg 58, 107 (2022). https://doi.org/10.1186/s41983-022-00539-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-022-00539-w