Abstract
Background
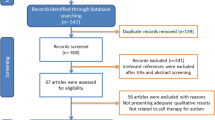
Autism spectrum disorders (ASD) include a group of neurodevelopmental disorders characterised by repetitive behaviours and impairments in communication, emotional and social skills. This review gives an overview of ASD, focusing on the aetiological and clinical aspects. It also discusses the role of neuroinflammation in ASD, critically examines the current evidence on the therapeutic effects of MSCs in ASD and consolidates key findings in this area of research.
Results
Many environmental and genetic factors have been linked to the aetiology of ASD. It has become increasingly evident that neuroinflammation plays a role in ASD. Conventional treatment of ASD revolves around psychosocial approaches whereas recent studies have turned to alternative approaches such as mesenchymal stem cell (MSC)-based therapy, owing to the well-recognised immunomodulatory characteristics of MSCs. Preclinical and clinical studies have shown that MSCs were able to exert anti-inflammatory effects and alleviate ASD symptoms.
Conclusions
There are many preclinical studies that support the use of MSCs in ASD. However, there are relatively fewer clinical studies concerning the safety and efficacy of MSCs in ASD, which warrants more large-scale clinical studies for future research.
Similar content being viewed by others
Introduction
Autism spectrum disorders (ASD) encompass a diverse group of neurodevelopmental disorders, which affect one’s behaviour, ability to communicate and interact socially to varying degrees. ASD manifests early in life and often lasts a lifetime. However, people with ASD show differences in the level of difficulty they face. Some patients with ASD are able to live independently while others may need support from caretakers for life. In the United States (US), the economic burden of ASD (including combined direct medical/non-medical costs and productivity costs) was estimated to be $268 billion and $461 billion for 2015 and 2025, respectively. With an increasing prevalence in ASD, it is likely that by 2025, the costs for ASD will far exceed the costs of attention deficit hyperactivity disorder (ADHD) and diabetes [1]. Moreover, an Egyptian study has associated an increased disease burden on families of ASD with stigma, parental health problems, as well as impaired quality of life. When one of these factors was present, the risk of the other factors would also increase [2].
The exact cause of ASD remains unclear. However, the aetiology of ASD includes a wide array of genetic and environmental factors. Studies have linked ASD with numerous genes, certain drugs (such as valproic acid), maternal infections and maternal antibodies during pregnancy, environmental toxicants (such as pesticides, cigarette smoke and heavy metals) as well as some postnatal factors [3]. It is noteworthy that although some have associated ASD with certain types of vaccine, there is no clear evidence between ASD and vaccination and such publication has led to retraction by the journal in the past [4]. On the other hand, chronic inflammation of the central nervous system (CNS) or neuroinflammation, has been linked to the underlying pathophysiology of several neurodevelopmental disorders, including ASD. Research has demonstrated that neuroinflammation may have an effect on brain development and the social cognitive deficits observed in ASD and other disorders such as schizophrenia [5].
Mesenchymal stem cells (MSCs) are a kind of multipotent stem cells that are found in various sites in the body. The bone marrow is an abundant source of MSCs, but these cells can also be harvested from adipose tissue, amniotic fluid, umbilical cord blood, placenta and dental pulp [6]. MSCs are popular for their immunomodulatory effects and the underlying mechanisms are related to the many soluble factors secreted by these cells. Besides, MSCs also interact with various cells of the immune system such as monocytes/ macrophages, B cells, T cells and natural killer cells [7]. Interestingly, MSCs’ response in inflammation is polarised. When the immune system is under-activated, MSCs exert a proinflammatory effect and when the immune system is over-activated, they exert an anti-inflammatory effect [8]. Therefore, MSCs are a potential therapeutic option in diseases where inflammation is a characteristic feature.
Treatment strategies of ASD often include behavioural-, physical-, occupational- and speech therapy. However, if neuroinflammation truly plays a part in ASD, these approaches alone may not be sufficient to alleviate the underlying inflammatory processes. More recently, researchers have discovered the therapeutic potential of MSCs in ASD. Therefore, this review gives an overview of ASD, particularly from the aetiological and clinical perspectives. It also discusses the role of neuroinflammation in ASD, critically appraises the rationale behind the use of MSCs in ASD and examines the underlying mechanisms of action of MSC-based therapy in ASD.
What are autism spectrum disorders (ASD)?
More than 100 years ago in 1911, a German psychiatrist, Eugen Bleuler published a book titled “Dementia Praecox oder Gruppe der Schizophrenien” [9]. In his publication, Bleuler was the first to coin and create the concept of autism, which he used to describe a symptom in severe schizophrenia. His description of autistic thinking encompassed infantile wishes as a way to avoid unsatisfying realities, which were replaced with hallucinations and fantasies. It was defined as the symbolic “inner life” of the subject not easily accessed by observers [9]. This concept was commonly used and believed by many psychologists and psychiatrists in the early twentieth century. It was not until the 1940s that Leo Kanner first viewed autism as a social and emotional disorder [10] and Hans Asperger described autism as a communication disorder [11].
Today, ASD refers to a group of neurodevelopmental disorders that often manifest and diagnosed in early childhood. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM)-5, there are two main domains of ASD, which are social communication impairments and behavioural problems such as repetitive behaviours and fixated interests [12]. Rather than a single disease, ASD is a spectrum covering three conditions, namely (1) Asperger’s disorder, (2) autistic disorder and (3) pervasive developmental disorder not otherwise specified (PDD-NOS). It is noteworthy that ASD may co-exist with other neurodevelopmental disorders such as ADHD or comorbidities like anxiety, depressive disorders, epilepsy and hearing impairment [13].
Due to a lack of definite biological markers, tracking of the prevalence of ASD is challenging. The heterogeneity in its clinical features and changes in the diagnostic criteria further increase the difficulty in epidemiological studies. A report published in 2018 by the Centre of Disease Control and Prevention (CDC) showed that the overall prevalence of ASD in 11 monitor sites of the US was 16.8 per 1000 (or 1 in 59) for 8-year-old children in 2014. In the same report, the diagnosis of ASD was four times more likely in boys when compared with girls and the median age of earliest known diagnosis was 52 months. Similar number and characteristics of children meeting the DSM-5 and DSM-IV-TR case definition were observed [14].
In a more recent systematic review of 30 studies, it was reported that the prevalence of ASD in the US was 1.70% and 1.85% among children aged 4 and 8 years, respectively, while the prevalence of ASD in Europe was estimated to be 0.38–1.55%. The study also reported an increase in the prevalence of ASD globally [13]. On the other hand, an Egyptian study reported that 2.8% of preschool children (n = 3722) were at high risk for ASD. In Sharkia Governorate, the prevalence of ASD was reported to be 5.4/1000. Several risk factors identified among these children include (1) congenital anomalies, (2) child medication during first year of life, (3) maternal medical conditions during pregnancy and (4) family history of psychiatric disorders [15].
Aetiology of ASD
To this end, the exact cause of autism remains unclear and incomplete. The aetiology of ASD is multifactorial and there are many genetic and environmental factors that have been linked to autism. However, one cannot pinpoint a single, definite causative factor.
Parental age
Increased parental age has been associated with an increased ASD risk. In a meta-analysis of 27 studies, it was reported that the lowest parental age group had a reduced risk of having offspring with autism with adjusted odds ratios (ORs) of 0.89 (95% confidence interval [CI] 0.75–1.06) for mother and 0.81 (95% CI 0.73–0.89) for father, whereas in the highest parental age group the ORs were 1.41 (95% CI 1.29–1.55) for mother and 1.55 (95% CI 1.39–1.73) for father, respectively. On the other hand, an 18% and 21% higher risk for autism was observed with a 10-year increase in maternal and paternal age, respectively [16].
Likewise, in an earlier study, advancing paternal age was significantly associated with ASD risk. Reichenberg and colleagues demonstrated that men ≥ 40 years had 5.75 times (95% CI, 2.65–12.46; p < 0.001) higher risk of having an offspring with ASD than those < 30 years [17]. However, advancing maternal age was not associated with ASD. Other studies also demonstrated a similar relationship between advancing parental age and ASD [18, 19]. More recently, a study reported that grandparental age might also contribute to the risk of ASD. An increased risk was observed in ASD children whose mothers were born to grandparents ≤ 19 years or whose fathers were born to grandparents ≤ 19 years and ≥ 40 years, when compared to grandparents aged 25–29 years, suggesting that the risk of parental or grandparental age might be transmitted across generations [20].
Genetic factors
It is now widely known that genetics play a substantial role in ASD and past research has examined the inheritability and concordance rates of the disorder. Although there is much variability in these studies, the concordance rates remain high, with monozygotic twins (MZ) having rates that are nearly twice that of dizygotic twins in general. For example, Hallmayer and colleagues observed a probandwise concordance of 58% (95% CI, 0.42–0.74) and 21% (95% CI, 0.09–0.43) in male MZ and DZ for strict autism [21]. On the other hand, for female MZ and DZ, respectively, a probandwise concordance of 60% (95% CI, 0.28–0.90) and 27% (95% CI, 0.09–0.69) was observed. In a meta-analysis, correlations of 0.98 (95% CI, 0.96–0.99) and 0.53 (95% CI, 0.44–0.60) were observed in MZ and DZ, respectively, with a substantial meta-analytic heritability estimate of 64–91% [22]. On the other hand, a study conducted by the Baby Siblings Research Consortium reported a recurrence rate of 18.7% in non-twin siblings [23].
Genetic risks of ASD are heterogeneous with numerous genes estimated to be involved, yet there is no single gene that accounts for > 1% of the cases [24], suggesting the involvement of multiple genetic factors, which cannot be explained by a simple single-gene Mendelian pattern of inheritance. Several chromosomal abnormalities and candidate genes have been shown to link to ASD. One chromosomal abnormality is maternal duplication of 15q11.2-q13.1 (Dup15q Syndrome), which increases the risk of ASD and accounts for approximately 1–3% of the cases [25]. There are two types of duplication in Dup15q syndrome, namely, interstitial and isodicentric duplications. Other than features of autism, individuals with Dup15 syndrome also present with central hypotonia, intellectual impairment, seizures and developmental delay [26]. In the published literature, the number of candidate genes that have been associated with autism is overwhelming. Some examples of these genes include UBE3A [27], GABRA5, GABRB3, GABRG3 [28], ENGRAILED 2 (EN2), SEROTONIN TRANSPORTER (5HTT) and REELIN (RELN) [29].
Environmental factors
Numerous environmental factors have been linked to ASD. During pregnancy, maternal physical conditions such as diabetes mellitus, hypertension and infections (including measles, mumps, herpes, pneumonia and chickenpox) have been indicated, whereas maternal mental health problems such as schizophrenia, anxiety and depression have also been associated with ASD. Exposure to certain medications such as sodium valproate (used in treatment of epilepsy and bipolar disorder), some antidepressants, thalidomide, misoprostol, terbutaline have all been connected to an increased risk for ASD (reviewed by Karimi and colleagues) [30]. Perinatal factors such as long duration of delivery, caesarean section, foetal distress and prematurity [31, 32] and postnatal factors such postpartum haemorrhage, low birth weight and brain anomaly have also been identified as risk factors of ASD [32].
Clinical aspects of ASD
ASD begins early in childhood and persists throughout the life of the affected individual. Some children show the symptoms as early as the first few months of life while others remain relatively normal until later in childhood. Although the very experienced specialist may diagnose ASD in infants, most cases are often diagnosed after the age of 3 years [33]. Past research has indicated that an earlier age of diagnosis is associated with a higher socioeconomic status of the parents [34]. The type of disorder in the spectrum has also been indicated to affect the age at diagnosis. For example, Asperger’s syndrome (115.9 months) was reported to be diagnosed much later that autistic disorder (44.9 months) in one study conducted in UK [35].
Often, parents and caretakers bring their children to see a physician because of a delay in developmental milestones, especially in speech. However, it is important to rule out hearing impairment as it also affects a child’s speech development and communication. The diagnosis of ASD is mainly clinical, involving taking a careful history and observing the child over a period, as there are no specific biomarkers or laboratory tests used for making a definitive diagnosis. The disorder mainly affects communication, language and behaviour of the child. While a small number of individuals with ASD have “savant” abilities who have near normal or even above-normal intelligence, a vast majority of autistic individuals suffer significant disabilities that affect their daily life [36].
According to DSM-5, to fulfil the diagnostic criterion of social communication impairments, one must demonstrate deficits in (1) social–emotional reciprocity, (2) non-verbal communications (such as eye contact, reciprocal smiling) and (3) relationships. On the other hand, to fulfil the diagnostic criterion of restricted interests and repetitive behaviours, the child must have two out of four symptoms, namely, (1) fixated interest, (2) hyper- or hyposensitivity to sensory stimuli (for example, unusual reactions how things sound, smell, taste and feel), (3) motor stereotypes (for example, jumping, repetitive hand flapping, making repetitive sounds, spinning) and (4) inflexibility to a change in routine or behaviour. In addition, the symptoms must be present early in one’s developmental life, are clinically significant that they impair social and occupational functioning, and are not otherwise due to intellectual disability or global developmental delay [12].
There is no one-size-fits-all treatment regimen for children with ASD. However, treatment should be started early and it usually takes a psychosocial approach [37, 38] consisting of a combination of speech-, occupational- and behavioural therapies, which aims at equipping those affected with the skills they need to function in the world. Thus far, there are no specific drugs approved for the treatment of ASD core symptoms. However, several pharmacologic agents have been used to relieve some of the associated symptoms. For example, fluoxetine [39] and clomipramine [40] have been used in some clinical trials to reduce repetitive behaviours. Methylphenidate has been shown to be beneficial in children with symptoms of hyperactivity and inattention [41], whereas atomoxetine has also been demonstrated to show improvements in hyperactivity in ASD [42]. The aetiological and clinical aspects of ASD are summarised in Fig. 1.
What is neuroinflammation?
Neuroinflammation is a term used to describe inflammatory response in the CNS mediated by substances such as chemokines, cytokines, second messengers and reactive oxygen species. There are positive and negative aspects of neuroinflammation. For example, transient and low levels of neuroinflammatory signalling may be beneficial in normal memory and learning. However, high levels of neuroinflammation in traumatic CNS injury and chronic neuroinflammation associated with aging and neurodegenerative diseases are harmful [43].
There are two major types of cells in the CNS, which are the neurons and glial cells. The former are the cells that carry out the neurological functions of the CNS while the latter include cells such as the astrocytes, microglia, and oligodendrocytes [44]. Research has shown that microglia (and to a lesser extent, mast cells and astrocytes) are the key players in neuroinflammation. On the other hand, glial cells, immune cells and endothelial cells are the main cells that release neuroinflammatory mediators [43].
Microglia are cells that originate from the mesoderm and function as resident macrophages in the CNS. More recently, there is a growing body of research that supports the role of microglia involvement during neuroinflammation in various conditions affecting the CNS such as Alzheimer’s disease [45], Parkinson’s disease [46], brain injury [47] and multiple sclerosis [48]. Interestingly, microglia activation is polarised, which plays a dualistic role in neuroinflammation. The M1 phenotype activated via the classical pathway is proinflammatory, whereas the M2 phenotype activated via the alternative pathway is anti-inflammatory [49].
In addition, it has become increasingly evident that there exists a link between neuroinflammation and mental disorders. As early as 1991, Smith proposed the “macrophage theory of depression” and suggested over-secretion of monokines by macrophages as a cause of depression [50]. When mice were subjected to chronic mild stress, they exhibited anxiety- and depressive-like behaviour, which was linked to microglial activation and hippocampal neuroinflammation. The hippocampus of the stressed mice demonstrated upregulation of several inflammatory mediators like interleukin-1β (IL-1β), IL-6, and IL-18 and activation of NOD-like receptor protein 3 (NLRP3) inflammasome, whereas neuroinflammation was relieved by minocycline (an antibiotic with anti-inflammatory effects) treatment [51]. Similarly, post-mortem evidence points to neuroinflammation in the frontal cortex of individuals with schizophrenia, with increased macrophages and altered gene expression of endothelial cells in the brain [52].
It is noteworthy that neuroinflammation in several conditions may have a genetic link. For neuroinflammation in Alzheimer’s disease, research has identified the involvement of genes related to immune responses, many of which encode for proteins expressed in microglia [53]. A decrease in homeostatic microglial genes has also been implicated in microglia-induced neuroinflammation and the pathogenesis of Alzheimer’s disease involving neuronal loss in mouse models [54]. In addition, the behavioural and inflammatory effects induced by neuroinflammation were found to be associated with gene expression changes in mice injected with lipopolysaccharide [55].
Neuroinflammation in ASD
The role of neuroinflammation in ASD has become increasingly evident in the published literature. However, it is not certain whether neuroinflammation leads to ASD or is a consequence of ASD. An earlier study by Vargas and colleagues reported evidence of neuroinflammation in brain tissues obtained from autopsy. Neuroinflammation was observed in the cerebral cortex and white matter, and particularly in the cerebellum of patients with ASD. Immunocytochemically, there was prominent microglia and astroglia activation, whereas cytokine profiling revealed an abundance of neuroglia-derived macrophage chemoattractant protein (MCP)-1 and tumour growth factor (TGF)–β1. Furthermore, cerebrospinal fluid (CSF) of living patients with ASD demonstrated a proinflammatory cytokine profile with increased levels of MCP-1. These findings indicate that innate neuroimmune responses may play a role in the pathogenesis of ASD [56].
In another study, brain tissues from the dorsolateral prefrontal cortex of individuals with ASD were found to exhibit marked microglia activation immunohistochemically. Microglia activation was observed in samples from individuals as young as < 6 years of age. Morphological changes in microglia included enlargement of soma, retraction and thickening of processes and filopodia extension from processes. In the white matter, there was a significant increase in microglial somal volume, whereas in the grey matter, a significant increase in microglial cell density was observed. These findings suggest that microglia activation occurs early in life. It can play a role in the pathogenesis of ASD or may represent a response to disruptions in the neuronal network in ASD [57].
Using positron emission tomography (PET) and a microglia radiotracer ([11C](R)-PK11195), Suzuki and colleagues demonstrated significantly higher radiotracer binding potential values for patients with ASD than those of the control in various parts of the brain. Although there was a similar distribution pattern for radiotracer binding potential for the ASD and control groups, the magnitude of the binding potential was greater in the ASD group. The brain regions with elevated binding potentials were anterior cingulate cortex, orbitofrontal cortex, fusiform gyri, cerebellum, pons and midbrain. These findings suggest an increased microglia activation in multiple regions of the brain of subjects with ASD [58].
Translocator protein (TSPO), a mitochondrial protein expressed on microglia and astrocytes, is involved in several processes such as mitochondrial homeostasis and immune modulation. One study has investigated the expression of TSPO in young adult males with ASD using simultaneous magnetic resonance–positron emission tomography (MR–PET) scan. The study revealed a lower expression of TSPO in several brain regions of ASD patients when compared with the control. Some examples of these brain regions include the (1) angular gyrus, (2) bilateral insular cortex, (3) lateral occipital cortex, (4) left postcentral gyrus, (5) orbitofrontal cortex, (6) precuneus/posterior cingulate cortex, (7) putamen, (8) superior temporal gyrus and (9) supramarginal gyrus. In addition, a higher symptom severity correlated with a lower TSPO expression. The study inferred that the lower TSPO expression in ASD patients might indicate mitochondrial dysfunction or neuroimmune abnormalities [59]. Another study has also reported similar findings using [18F]FEPPA, a specific ligand for TSPO to investigate neuroinflammation in ASD patients. The study reported a significant lower [18F]FEPPA total volume of distribution in ASD patients when compared to the control (p = 0.02) [60].
Lucchina and Depino reported signs of chronic glial activation in mice administered subcutaneous valproic acid, particularly in the cerebellum and hippocampus. When autistic mice were given lipopolysaccharides (LPS) via the intraperitoneal route, they demonstrated an exaggerated inflammatory response peripherally with increased levels of blood corticosterone. LPS stimulation also resulted in increased neuroinflammation when compared to the control group. In the hippocampus, there was increased microglia, whereas the cerebellum demonstrated increased proinflammatory cytokines. These findings support the role of neuroinflammation and altered immune response in ASD [61].
In a mouse model, Choi and colleagues demonstrated increased IL-17a in pregnant mothers subjected to maternal immune activation (MIA) was accompanied by an increase in IL-17a mRNA expression in the foetal brain. Offspring of MIA mice also showed abnormal cortical development due to maternal IL-17a and abnormal behaviours resembling those of ASD. However, maternal pre-treatment of IL-17a blocking antibodies inhibited IL-17a mRNA expression in the foetal brain, suggesting that upregulation of foetal brain IL-17a was mediated via maternal IL-17a pathway and that proinflammatory maternal IL-17a played a role in the pathogenesis of ASD in mice offspring [62].
On the other hand, a number of studies have reported proinflammatory substances in the serum, plasma, cerebrospinal fluid (CSF) and brain of patients with ASD. Some examples of these substances include interleukins (IL) (such as IL-2 and IL-6), chemokines (such as MCP-1 and osteopontin), tumour necrosis factor (TNF)-α, interferon (IF)- γ and growth factors [such ah transforming growth factor (TGF)-β, epidermal growth factor (EPF), brain-derived neurotrophic factor (BDNF)] (reviewed by Xu and colleagues) [63]. Other factors that may be associated with neuroinflammation in ASD include atopic diseases [64] and maternal inflammatory states during pregnancy like maternal infections, autoimmune diseases and gestational diabetes mellitus [65]. Table 1 summarises evidence for neuroinflammation in ASD.
MSCs and their immunomodulatory properties
Numerous studies have documented the clinical use of MSCs in various medical conditions. Some reasons for their popularity among researchers and clinicians include (1) they can be harvested from many locations in the body, (2) they are relatively easy to culture in the laboratory and (3) there are less ethical issues when compared to the use of other types of stem cells such as embryonic stem cells [66]. In addition, MSCs are well known for their immunomodulatory properties and are potential therapeutic options in a wide range of immune-mediated conditions such as autoimmune diseases [67] and graft-versus-host disease [68].
Research has found that the immunomodulatory effects of MSCs can be bidirectional; they promote inflammation when the immune system is under-activated and they suppress inflammation when the immune system is over-activated [8]. MSCs are also immune-privileged cells that are well-tolerated when transplanted in patients. Therefore, both autologous MSCs [69] and allogeneic MSCs [70] have been used clinically without serious adverse events. Several underlying mechanisms of action have been suggested for the immunomodulatory effects of MSCs. Other than exerting their beneficial effects by direct cell-to-cell contact, MSCs are also capable of secreting soluble factors such as growth factors, chemokines and cytokines, which act in a paracrine manner. More recently, researchers have turned their attention to extracellular vesicles (EVs) released by MSCs as they are a rich source of substances that possess immunomodulatory properties [71]. Therefore, a number of studies have explored the clinical application of MSC secretome and MSC-derived EVs in different diseases.
Therapeutic potential of MSCs or secretory products of MSCs in ASD
MSCs’ exact mechanism of action on the CNS remains largely unclear. Some of the proposed mechanisms of MSCs’ therapeutic effects in neurological conditions include synaptogenesis, neurogenesis and neuroprotection [72]. However, in view of a growing body of research on local and systemic immune abnormalities in ASD, the immunomodulatory properties of MSCs make these cells potential therapeutic candidates in conditions where inflammation is a feature, including ASD. The immune properties of MSCs have been studied in other neurological conditions such as multiple sclerosis, Alzheimer’s disease, CNS injuries and stroke [73]. As for ASD, a number of studies have explored the safety profile of MSCs, as well as the potential therapeutic benefits. Researchers have also explored the use of MSCs in ASD using MSCs from different sources and via different administration routes in preclinical and clinical studies.
Preclinical studies
In vitro studies have demonstrated that MSCs may modulate neuroinflammation. When BV2 microglia (a microglia cell line) and primary microglia derived from the brains of C57BL/6 mice were cultured in MSC-conditioned medium (MSC-CM), there was a significant reduction in mRNA expressions of proinflammatory TNF-α and IL-6 in LPS-activated microglia. MSC-CM cultured activated microglia also demonstrated a reduction of JNK, NFκB and c-Jun mRNA expression, as well as an increased NO production and iNOS, MKP-1 and IL-10 mRNA expression. The study inferred that the immunomodulatory effects on microglial activities were mediated through paracrine effects [74].
In another study, MSC-derived microvesicles (MVs) have been shown to modulate immune LPS-induced inflammation in microglia using a BV2 cell line and primary microglia. When activated microglia were co-cultured with MSC-EVs, the latter inhibited upregulation of IL-1β, TNF-α, prostaglandin endoperoxide synthase 2, nitric oxide synthase isoforms and activation markers (for example, CD45 and CD11b). Phosphorylation of c-Jun N-terminal kinases and p38 MAP kinase in LPS-treated microglia was also suppressed by MSC-EVs. These findings suggest that MSC-MVs may exert immunomodulatory effects on microglia [75].
BTBR mouse model is an acceptable animal model of ASD that demonstrates several features of ASD such as behavioural abnormalities that fit the diagnostic criteria, reduction in signalling mediated by brain-derived neurotrophic factor (BDNF) and decreased neurogenesis in the hippocampus. In an earlier study, Segal-Gavish and colleagues transplanted MSCs via the intracerebroventricular route and demonstrated stereotypical behaviour reduction, social behaviour improvement and cognitive rigidity reduction. After MSC transplantation, higher levels of BNDF proteins and increased neurogenesis in the hippocampus were also observed in the MSC-treated animals when compared with sham-treated animals, suggesting that BDNF may play a role in the underlying mechanism of action for the observed findings [76].
Exosomes (exo) are extracellular vesicles (EVs) secreted by almost all types of eukaryotic cells, including MSCs. MSC-derived exosomes (MSC-exo) have been reported to play a role in immunoregulation, tissue repair and regeneration, as well as angiogenesis [77]. Perets and colleagues studied the effects of intranasal MSC-exo in BTBR mice, and reported improvement in male-to-male social interaction and reduction in repetitive behaviours when compared to BTBR mice treated with saline. However, such observations were not observed when neural stem cell-derived exosomes (NSC-exo) were used. Improvements in male-to-female ultrasonic vocalisations and pulp retrieval were also observed in the MSC-exo group when compared with the saline-treated group. Fluorescent brain imaging revealed the presence of MSC-exo in brain cells, suggesting brain parenchymal penetration of MSC-exo. When the membrane proteins in MSC-exo were removed using protease K, the previously observed effects of MSC-exo were no longer present, suggesting that the efficacy and migration of MSC-exo were dependent on the membrane proteins present in them [78].
In another study, MSC-exo administered via the intranasal route resulted in behavioural improvement in a mouse model of autism (Shank3B KO mice). In particular, there was a reduction in repetitive behaviours and an increase in ultrasonic vocalisation in experimental mice. MSC-exo was found to cross the blood–brain barrier (BBB) and accumulate in the cerebellum and cortex of these mice. In the frontal cortex, there was also an increased RNA expression of GABA Rb1 receptors. These findings suggest that the therapeutic effects may be mediated by the exosomes secreted by MSCs, although the exact underlying mechanisms await further investigation [79].
Similarly, behavioural improvements were observed in offspring of mice treated with valproic acid (VA) showing autism-like features. In one study, Liang and colleagues administered exosomes derived from human umbilical cord (hUC)-MSCs via the intranasal route and observed social ability restoration and correction of repetitive stereotyped behaviours and other autism-related abnormal phenotypes in offspring of VA-treated mice. MSC-exo were found to enter the brain tissues efficiently via the intranasal route. The study concluded that the therapeutic effects of MSC-exo might be partially due to the anti-inflammatory effects of the exosomes [80].
Clinical studies
An earlier phase I/II study examined the efficacy and safety of human cord blood mononuclear cells (CBMNCs) and UCMSCs in autism. Thirty-seven children (3–12 years) were divided into three groups: (1) control (n = 14; rehabilitation therapy only), (2) CBMNC (n = 14; rehabilitation therapy + CBMNCs) and (3) combination group (n = 9; rehabilitation therapy + CBMNCs + UCMSCs). Weekly IV and intrathecal stem cell infusions were given four times. Assessment of treatment efficacy was done using three instruments, namely, the Aberrant Behaviour Checklist (ABC), Clinical Global Impression scale (CGI) and Childhood Autism Rating Scale (CARS). Significant reduction in the ABC scores was observed in all three groups 24 weeks after treatment (p < 0.05). However, the combination group had the highest percentage reduction (59.9%) when compared to the CBMNC group (38.0%) and control group (17.4%). For the CGI, the combination group showed the most significant improvements (p < 0.05) using various subscales (CGI-SI, CGI-GI and CGI-EI) when compared to the CBMNC and control groups. There were significant differences in the reduction of CARS scores 24 weeks after treatment, when comparing the combination group (37.9% reduction) with the CBMNC group (20.0% reduction) and control group (13.7% reduction; p < 0.05) [81].
On the other hand, the vital signs of all subjects were normal throughout the treatment course. Only five participants reported low-grade fever. However, they recovered without any medical intervention. No significant safety issues were reported. After treatment, there were no significant changes from the baseline in terms of the laboratory findings (such as liver and renal functions, serum glucose, lipid profile, complete blood count and immunological parameters). These findings suggest that both CBMNCs and UCMSCs are safe and efficacious. However, a combination of UCMSCs and CBMNCs demonstrated a larger therapeutic effect than that of CBMNCs alone [81].
Sun and colleagues conducted a phase 1 study on children with ASD between 4 and 9 years old (n = 12) using IV infusions of allogeneic human cord tissue-derived mesenchymal stromal cells (hCT-MSCs). Three measures were used to assess the clinical and psychological outcomes of the treatment. These include (1) VABS-3 Socialization Subscale Score (assessment for social communication skills), (2) PDDBI Autism Composite (assessment for severity of autism symptoms) and (3) expert clinical judgement (CGI-I). Assessments were done at baseline, as well as 6 months and 12 months post-infusion. Out of 12 children, 6 showed an improvement in ≥ 2 measures and out of these 6 children, 4 showed an improvement in all three measures [82]. Among the non-serious adverse events (AEs), agitation during the procedure was the most frequently reported AE. The frequency of the non-serious AEs increased with the number of doses of treatment administered. However, the increase in frequency was not statistically significant. New class I anti-human leukocyte antigen (anti-HLA) antibodies were detected in 5 children. However, the presence of these new anti-HLA antibodies did not lead to any clinical manifestations. The study concluded that IV infusions of hCT-MSCs were safe and a feasible treatment option for ASD [82].
Another study evaluated the safety and efficacy of human allogeneic UC-MSCs on two children. CARS score and clinical outcomes were assessed to determined treatment efficacy. In the first case, a 5-year-old boy was given six IV injections of UC-MSCs. Improvements were observed in verbal and non-verbal communication abilities, particularly in expressive language and listening. In the second case, four IV injections of UC-MSCs were given to a 6-year-old boy. Improvements in eye contact, verbal and non-verbal communication abilities and abnormal behaviours were observed post-treatment. Both patients demonstrated a reduction of CARS scores and no serious adverse events were reported [83]. Table 2 summarises the applications of MSCs in ASD.
Conclusions
There is an increasing prevalence of ASD globally, which incurs a huge economic burden in the healthcare system. Although the exact cause of ASD is unclear, there is abundant evidence to suggest an interplay of genetic and environmental factors. Studies have also shown that neuroinflammation plays a role in ASD, but it is unsure whether neuroinflammation leads to ASD or is a result of ASD. Several proinflammatory markers have been associated with neuroinflammation in animal models, whereas proinflammatory markers are detected in the serum, plasma and CSF samples of patients with ASD. Microglial activation involving different regions of the brain have also been demonstrated in animal models and patients with ASD.
The conventional treatment of ASD involves a combination of behavioural-, occupational- and speech therapy. However, these approaches alone may not be sufficient to address the neuroinflammation in ASD. There is a growing body of research in favour of the therapeutic potential of MSCs in ASD. This is not surprising because MSCs are well known for their immunomodulatory properties. Thus far, preclinical studies show that MSC-CM and MSC-MVs could modulate inflammation in vitro, whereas MSC-exo and MSC transplantation via various routes of administration exerted anti-inflammatory effects and alleviated symptoms of ASD in animal models. However, there are only a handful of clinical studies on the safety and efficacy of MSCs in ASD. Although these clinical studies reported encouraging results, they only involved a small number of patients and the underlying mechanism of action was not well delineated. Based on the current evidence, more larger-scale clinical trials are needed to support the clinical use of MSC in the treatment of ASD.
Availability of data and materials
Not applicable.
Abbreviations
- ABC:
-
Aberrant Behaviour Checklist
- Anti-HLA Ab:
-
Anti-HLA antibodies
- ASD:
-
Autism spectrum disorders
- BBB:
-
Blood–brain barrier
- BM-MSCs:
-
Bone marrow-derived mesenchymal stem cells
- BNDF:
-
Brain-derived neurotrophic factor
- CAR:
-
Childhood Autism Rating Scale
- CBMNCs:
-
Cord blood mononuclear cells
- CGI:
-
Clinical global impression
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- DSM-5:
-
Diagnostic and statistical manual of mental disorders 5
- hCT-MSCs:
-
Human cord tissue-derived mesenchymal stromal cells
- EPF:
-
Epidermal growth factor
- IL:
-
Interleukin
- IF:
-
Interferon
- LPS:
-
Lipopolysaccharides
- MIA:
-
Maternal immune activation
- hUC-MSCs:
-
Human umbilical cord-derived mesenchymal stem cells
- MSC-CM:
-
Mesenchymal stem cell conditioned medium
- MPC-1:
-
Macrophage chemoattractant protein-1
- MR:
-
Magnetic resonance
- MSC-exo:
-
Mesenchymal stem cell-derived exosomes
- MSC-MV:
-
Mesenchymal stem cell-derived microvesicles
- PET:
-
Positron emission tomography
- TGF–β1:
-
Tumour growth factor-β1
- TNF-α:
-
Tumour necrosis factor-α
- TSPO:
-
Translocator protein
References
Leigh JP, Du J. Brief Report: Forecasting the economic burden of autism in 2015 and 2025 in the United States. J Autism Dev Disord. 2015;45(12):4135–9. https://doi.org/10.1007/s10803-015-2521-7.
Gabra RH, Hashem DF, Ahmed GK. The possible relation between stigma, parent psychiatric symptoms, quality of life and the disease burden in families of children with autism spectrum disorder in Egypt: a multicentre study. Egypt J Neurol Psychiatry Neurosurg. 2021;57:170. https://doi.org/10.1186/s41983-021-00426-w.
Amaral DG. Examining the Causes of Autism. Cerebrum. 2017; 2017:cer-01-17.
Eggertson L. Lancet retracts 12-year-old article linking autism to MMR vaccines. CMAJ. 2010;182(4):E199-200. https://doi.org/10.1503/cmaj.109-3179.
Nakagawa Y, Chiba K. Involvement of neuroinflammation during brain development in social cognitive deficits in autism spectrum disorder and schizophrenia. J Pharmacol Exp Ther. 2016;358(3):504–15. https://doi.org/10.1124/jpet.116.234476.
Vedenko A, Barretta J, Hare J, Hatzistergos K. Mesenchymal stem cells: characterization, properties and therapeutic potential. Reference Module in Biomedical Sciences 2019:25–34
Weiss ARR, Dahlke MH. Immunomodulation by mesenchymal stem cells (MSCs): mechanisms of action of living, apoptotic, and dead MSCs. Front Immunol. 2019;10:1191. https://doi.org/10.3389/fimmu.2019.01191.
Waterman RS, Tomchuck SL, Henkle SL, Betancourt AM. A new mesenchymal stem cell (MSC) paradigm: polarization into a pro-inflammatory MSC1 or an immunosuppressive MSC2 phenotype. PLoS ONE. 2010;5(4): e10088. https://doi.org/10.1371/journal.pone.0010088.
Bleuler E. Dementia Praecox oder Gruppe der Schizophrenien. Leipzig: Deuticke; 1911.
Kanner L. Autistic disturbances of affective contact. Nervous Child. 1943;2:217–50.
Asperger H. Die “autistischen Psychopathen” im Kindesalter. Archiv fu¨r Psychiatrie und Nervenkrakheiten 1944; 117: 76–136.
American Psychiatric Association. DSM-5: diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Association; 2013.
Bougeard C, Picarel-Blanchot F, Schmid R, Campbell R, Buitelaar J. Prevalence of autism spectrum disorder and co-morbidities in children and adolescents: a systematic literature review. Front Psychiatry. 2021;12:744709. https://doi.org/10.3389/fpsyt.2021.744709.
Baio J, Wiggins L, Christensen DL, Maenner MJ, Daniels J, Warren Z, et al. Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveill Summ. 2018;67(6):1–23. https://doi.org/10.15585/mmwr.ss6706a1.
Yousef AM, Roshdy EH, Abdel Fattah NR, Said RM, Atia MM, Hafez EM, et al. Prevalence and risk factors of autism spectrum disorders in preschool children in Sharkia, Egypt: a community-based study. Middle East Curr Psychiatry. 2021;28:36. https://doi.org/10.1186/s43045-021-00114-8.
Wu S, Wu F, Ding Y, Hou J, Bi J, Zhang Z. Advanced parental age and autism risk in children: a systematic review and meta-analysis. Acta Psychiatr Scand. 2017;135(1):29–41. https://doi.org/10.1111/acps.12666.
Reichenberg A, Gross R, Weiser M, Bresnahan M, Silverman J, Harlap S, et al. Advancing paternal age and autism. Arch Gen Psychiatry. 2006;63(9):1026–32. https://doi.org/10.1001/archpsyc.63.9.1026.
Hultman CM, Sandin S, Levine SZ, Lichtenstein P, Reichenberg A. Advancing paternal age and risk of autism: new evidence from a population-based study and a meta-analysis of epidemiological studies. Mol Psychiatry. 2011;16(12):1203–12. https://doi.org/10.1038/mp.2010.121.
Sandin S, Schendel D, Magnusson P, Hultman C, Surén P, Susser E, et al. Autism risk associated with parental age and with increasing difference in age between the parents. Mol Psychiatry. 2016;21(5):693–700. https://doi.org/10.1038/mp.2015.70.
Gao Y, Yu Y, Xiao J, Luo J, Zhang Y, Tian Y, et al. Association of grandparental and parental age at childbirth with autism spectrum disorder in children. JAMA Netw Open. 2020;3(4): e202868. https://doi.org/10.1001/jamanetworkopen.2020.2868.
Hallmayer J, Cleveland S, Torres A, Phillips J, Cohen B, Torigoe T, et al. Genetic heritability and shared environmental factors among twin pairs with autism. Arch Gen Psychiatry. 2011;68(11):1095–102. https://doi.org/10.1001/archgenpsychiatry.2011.76.
Tick B, Bolton P, Happé F, Rutter M, Rijsdijk F. Heritability of autism spectrum disorders: a meta-analysis of twin studies. J Child Psychol Psychiatry. 2016;57(5):585–95. https://doi.org/10.1111/jcpp.12499.
Ozonoff S, Young GS, Carter A, Messinger D, Yirmiya N, Zwaigenbaum L, et al. Recurrence risk for autism spectrum disorders: a Baby Siblings Research Consortium study. Pediatrics. 2011;128(3):e488–95. https://doi.org/10.1542/peds.2010-2825.
Abrahams BS, Geschwind DH. Advances in autism genetics: on the threshold of a new neurobiology. Nat Rev Genet. 2008;9(5):341–55. https://doi.org/10.1038/nrg2346.
Veenstra-Vanderweele J, Christian SL, Cook EH Jr. Autism as a paradigmatic complex genetic disorder. Annu Rev Genomics Hum Genet. 2004;5:379–405. https://doi.org/10.1146/annurev.genom.5.061903.180050.
Kalsner L, Chamberlain SJ. Prader-Willi, Angelman, and 15q11-q13 duplication syndromes. Pediatr Clin North Am. 2015;62(3):587–606. https://doi.org/10.1016/j.pcl.2015.03.004.
Vatsa N, Jana NR. UBE3A and its link with autism. Front Mol Neurosci. 2018;11:448. https://doi.org/10.3389/fnmol.2018.00448.
Kim SA, Kim JH, Park M, Cho IH, Yoo HJ. Association of GABRB3 polymorphisms with autism spectrum disorders in Korean trios. Neuropsychobiology. 2006;54(3):160–5. https://doi.org/10.1159/000098651.
Bartlett CW, Gharani N, Millonig JH, Brzustowicz LM. Three autism candidate genes: a synthesis of human genetic analysis with other disciplines. Int J Dev Neurosci. 2005;23(2–3):221–34. https://doi.org/10.1016/j.ijdevneu.2004.10.004.
Karimi P, Kamali E, Mousavi SM, Karahmadi M. Environmental factors influencing the risk of autism. J Res Med Sci. 2017;22:27. https://doi.org/10.4103/1735-1995.200272.
Hadjkacem I, Ayadi H, Turki M, Yaich S, Khemekhem K, Walha A, et al. Prenatal, perinatal and postnatal factors associated with autism spectrum disorder. Jornal de Pediatria. 2016;92(6):595–601. https://doi.org/10.1016/j.jped.2016.01.012.
Wang C, Geng H, Liu W, Zhang G. Prenatal, perinatal, and postnatal factors associated with autism: a meta-analysis. Medicine. 2017;96(18):e6696. https://doi.org/10.1097/MD.0000000000006696.
Mandell DS, Morales KH, Xie M, Lawer LJ, Stahmer AC, Marcus SC. Age of diagnosis among Medicaid-enrolled children with autism, 2001–2004. Psychiatr Serv. 2010;61(8):822–9. https://doi.org/10.1176/ps.2010.61.8.822.
Mazurek MO, Handen BL, Wodka EL, Nowinski L, Butter E, Engelhardt CR. Age at first autism spectrum disorder diagnosis: the role of birth cohort, demographic factors, and clinical features. J Dev Behav Pediatr. 2014;35(9):561–9. https://doi.org/10.1097/DBP.0000000000000097.
Williams E, Thomas K, Sidebotham H, Emond A. Prevalence and characteristics of autistic spectrum disorders in the ALSPAC cohort. Dev Med Child Neurol. 2008;50(9):672–7. https://doi.org/10.1111/j.1469-8749.2008.03042.x.
Zachariah SM, Oommen SP, Koshy B. Clinical features and diagnosis of autism spectrum disorder in children. Curr Med Issues. 2017;15(1):6–16. https://doi.org/10.4103/0973-4651.200297.
Kim HS. Psychosocial treatments for children with autism spectrum disorder. Hanyang Med Rev. 2016;36:27–37. https://doi.org/10.7599/hmr.2016.36.1.27.
Politte LC, Howe Y, Nowinski L, Palumbo M, McDougle CJ. Evidence-based treatments for autism spectrum disorder. Curr Treat Options Psychiatry. 2015;2:38–56. https://doi.org/10.1007/s40501-015-0031-z.
Hollander E, Soorya L, Chaplin W, Anagnostou E, Taylor BP, Ferretti CJ, et al. A double-blind placebo-controlled trial of fluoxetine for repetitive behaviors and global severity in adult autism spectrum disorders. Am J Psychiatry. 2012;169(3):292–9. https://doi.org/10.1176/appi.ajp.2011.10050764.
Gordon CT, State RC, Nelson JE, Hamburger SD, Rapoport JL. A double-blind comparison of clomipramine, desipramine, and placebo in the treatment of autistic disorder. Arch Gen Psychiatry. 1993;50(6):441–7. https://doi.org/10.1001/archpsyc.1993.01820180039004.
Sturman N, Deck L, van Driel ML. Methylphenidate for children and adolescents with autism spectrum disorder. Cochrane Database Syst Rev. 2017. https://doi.org/10.1002/14651858.CD011144.pub2.
Arnold LE, Aman MG, Cook AM, Witwer AN, Hall KL, Thompson S, et al. Atomoxetine for hyperactivity in autism spectrum disorders: placebo-controlled crossover pilot trial. J Am Acad Child Adolesc Psychiatry. 2006;45(10):1196–205. https://doi.org/10.1097/01.chi.0000231976.28719.2a.
DiSabato DJ, Quan N, Godbout JP. Neuroinflammation: the devil is in the details. J Neurochem. 2016;139(Suppl 2):136–53. https://doi.org/10.1111/jnc.13607.
Jäkel S, Dimou L. Glial cells and their function in the adult brain: a journey through the history of their ablation. Front Cell Neurosci. 2017;11:24. https://doi.org/10.3389/fncel.2017.00024.
Fan Z, Brooks DJ, Okello A, Edison P. An early and late peak in microglial activation in Alzheimer’s disease trajectory. Brain. 2017;140(3):792–803. https://doi.org/10.1093/brain/aww349.
Badanjak K, Fixemer S, Smajić S, Skupin A, Grünewald A. The contribution of microglia to neuroinflammation in Parkinson’s disease. Int J Mol Sci. 2021;22(9):4676. https://doi.org/10.3390/ijms22094676.
Izzy S, Liu Q, Fang Z, Lule S, Wu L, Chung JY, et al. Time-dependent changes in microglia transcriptional networks following traumatic brain injury. Front Cell Neurosci. 2019;8(13):307. https://doi.org/10.3389/fncel.2019.00307.
Howell OW, Rundle JL, Garg A, Komada M, Brophy PJ, Reynolds R. Activated microglia mediate axoglial disruption that contributes to axonal injury in multiple sclerosis. J Neuropathol Exp Neurol. 2010;69(10):1017–33. https://doi.org/10.1097/NEN.0b013e3181f3a5b1.
Dong R, Huang R, Wang J, Liu H, Xu Z. Effects of microglial activation and polarization on brain injury after stroke. Front Neurol. 2021;12: 620948. https://doi.org/10.3389/fneur.2021.620948.
Smith RS. The macrophage theory of depression. Med Hypotheses. 1991;35(4):298–306. https://doi.org/10.1016/0306-9877(91)90272-z.
Wang YL, Han QQ, Gong WQ, Pan DH, Wang LZ, Hu W, et al. Microglial activation mediates chronic mild stress-induced depressive- and anxiety-like behavior in adult rats. J Neuroinflammation. 2018;15(1):21. https://doi.org/10.1186/s12974-018-1054-3.
Cai HQ, Catts VS, Webster MJ, Galletly C, Liu D, O’Donnell M, et al. Increased macrophages and changed brain endothelial cell gene expression in the frontal cortex of people with schizophrenia displaying inflammation. Mol Psychiatry. 2020;25(4):761–75. https://doi.org/10.1038/s41380-018-0235-x.
Villegas-Llerena C, Phillips A, Garcia-Reitboeck P, Hardy J, Pocock JM. Microglial genes regulating neuroinflammation in the progression of Alzheimer’s disease. Curr Opin Neurobiol. 2016;36:74–81. https://doi.org/10.1016/j.conb.2015.10.004.
Sobue A, Komine O, Hara Y, Endo F, Mizoguchi H, Watanabe S, Murayama S, Saito T, Saido TC, Sahara N, Higuchi M, Ogi T, Yamanaka K. Microglial gene signature reveals loss of homeostatic microglia associated with neurodegeneration of Alzheimer’s disease. Acta Neuropathol Commun. 2021;9(1):1. https://doi.org/10.1186/s40478-020-01099-x.
Bonow RH, Aïd S, Zhang Y, Becker KG, Bosetti F. The brain expression of genes involved in inflammatory response, the ribosome, and learning and memory is altered by centrally injected lipopolysaccharide in mice. Pharmacogenomics J. 2009;9(2):116–26. https://doi.org/10.1038/tpj.2008.15.
Vargas DL, Nascimbene C, Krishnan C, Zimmerman AW, Pardo CA. Neuroglial activation and neuroinflammation in the brain of patients with autism. Ann Neurol. 2005;57(1):67–81. https://doi.org/10.1002/ana.20315.
Morgan JT, Chana G, Pardo CA, Achim C, Semendeferi K, Buckwalter J, et al. Microglial activation and increased microglial density observed in the dorsolateral prefrontal cortex in autism. Biol Psychiatry. 2010;68(4):368–76. https://doi.org/10.1016/j.biopsych.2010.05.024.
Suzuki K, Sugihara G, Ouchi Y, Nakamura K, Futatsubashi M, et al. Microglial activation in young adults with autism spectrum disorder. JAMA Psychiat. 2013;70(1):49–58. https://doi.org/10.1001/jamapsychiatry.2013.272.
Zürcher NR, Loggia ML, Mullett JE, Tseng C, Bhanot A, Richey L, et al. [11C]PBR28 MR-PET imaging reveals lower regional brain expression of translocator protein (TSPO) in young adult males with autism spectrum disorder. Mol Psychiatry. 2021;26(5):1659–69. https://doi.org/10.1038/s41380-020-0682-z.
Simpson D, Gharehgazlou A, Da Silva T, Labrie-Cleary C, Wilson AA, Meyer JH, et al. In vivo imaging translocator protein (TSPO) in autism spectrum disorder. Neuropsychopharmacology. 2022;47(7):1421–7. https://doi.org/10.1038/s41386-022-01306-4.
Lucchina L, Depino AM. Altered peripheral and central inflammatory responses in a mouse model of autism. Autism Res. 2014;7(2):273–89. https://doi.org/10.1002/aur.1338.
Choi GB, Yim YS, Wong H, Kim S, Kim H, Kim SV, et al. The maternal interleukin-17a pathway in mice promotes autism-like phenotypes in offspring. Science. 2016;351(6276):933–9. https://doi.org/10.1126/science.aad0314.
Xu N, Li X, Zhong Y. Inflammatory cytokines: potential biomarkers of immunologic dysfunction in autism spectrum disorders. Mediators Inflamm. 2015;2015:531518. https://doi.org/10.1155/2015/531518.
Theoharides TC, Tsilioni I, Patel AB, Doyle R. Atopic diseases and inflammation of the brain in the pathogenesis of autism spectrum disorders. Transl Psychiatry. 2016;6(6): e844. https://doi.org/10.1038/tp.2016.77.
Han VX, Patel S, Jones HF, Nielson TC, Mohammad SS, Hofer MJ, et al. Maternal acute and chronic inflammation in pregnancy is associated with common neurodevelopmental disorders: a systematic review. Transl Psychiatry. 2021;11(1):71. https://doi.org/10.1038/s41398-021-01198-w.
Kim HJ, Park JS. Usage of human mesenchymal stem cells in cell-based therapy: advantages and disadvantages. Dev Reprod. 2017;21(1):1–10. https://doi.org/10.12717/DR.2017.21.1.001.
Pistoia V, Raffaghello L. Mesenchymal stromal cells and autoimmunity. Int Immunol. 2017;29(2):49–58. https://doi.org/10.1093/intimm/dxx008.
Kelly K, Rasko JEJ. Mesenchymal stromal cells for the treatment of graft versus host disease. Front Immunol. 2021;12: 761616. https://doi.org/10.3389/fimmu.2021.761616.
Petrou P, Kassis I, Levin N, Paul F, Backner Y, Benoliel T, et al. Beneficial effects of autologous mesenchymal stem cell transplantation in active progressive multiple sclerosis. Brain. 2020;143(12):3574–88. https://doi.org/10.1093/brain/awaa333.
Shokati A, Naser Moghadasi A, Nikbakht M, Sahraian MA, Mousavi SA, Ai J. A focus on allogeneic mesenchymal stromal cells as a versatile therapeutic tool for treating multiple sclerosis. Stem Cell Res Ther. 2021;12(1):400. https://doi.org/10.1186/s13287-021-02477-5.
Song N, Scholtemeijer M, Shah K. Mesenchymal stem cell immunomodulation: mechanisms and therapeutic potential. Trends Pharmacol Sci. 2020;41(9):653–64. https://doi.org/10.1016/j.tips.2020.06.009.
Gesundheit B, Ashwood P, Keating A, Naor D, Melamed M, Rosenzweig JP. Therapeutic properties of mesenchymal stem cells for autism spectrum disorders. Med Hypotheses. 2015;84(3):169–77. https://doi.org/10.1016/j.mehy.2014.12.016.
Andrzejewska A, Dabrowska S, Lukomska B, Janowski M. Mesenchymal stem cells for neurological disorders. Adv Sci (Weinh). 2021;8(7):2002944. https://doi.org/10.1002/advs.202002944.
Ooi YY, Dheen ST, Tay SS. Paracrine effects of mesenchymal stem cells-conditioned medium on microglial cytokines expression and nitric oxide production. NeuroImmunoModulation. 2015;22(4):233–42. https://doi.org/10.1159/000365483.
Jaimes Y, Naaldijk Y, Wenk K, Leovsky C, Emmrich F. Mesenchymal stem cell-derived microvesicles modulate lipopolysaccharides-induced inflammatory responses to microglia cells. Stem Cells. 2017;35(3):812–23. https://doi.org/10.1002/stem.2541.
Segal-Gavish H, Karvat G, Barak N, Barzilay R, Ganz J, Edry L, et al. Mesenchymal stem cell transplantation promotes neurogenesis and ameliorates autism related behaviors in BTBR mice. Autism Res. 2016;9(1):17–32. https://doi.org/10.1002/aur.1530.
Wei W, Ao Q, Wang X, Cao Y, Liu Y, Zheng SG, et al. Mesenchymal stem cell-derived exosomes: a promising biological tool in nanomedicine. Front Pharmacol. 2021;11: 590470. https://doi.org/10.3389/fphar.2020.590470.
Perets N, Hertz S, London M, Offen D. Intranasal administration of exosomes derived from mesenchymal stem cells ameliorates autistic-like behaviors of BTBR mice. Mol Autism. 2018;9:57. https://doi.org/10.1186/s13229-018-0240-6.
Perets N, Oron O, Herman S, Elliott E, Offen D. Exosomes derived from mesenchymal stem cells improved core symptoms of genetically modified mouse model of autism Shank3B. Mol Autism. 2020;11(1):65. https://doi.org/10.1186/s13229-020-00366-x.
Liang Y, Duan L, Xu X, Li X, Liu M, Chen H, et al. Mesenchymal stem cell-derived exosomes for treatment of autism spectrum disorder. ACS Appl Bio Mater. 2020;3(9):6384–93. https://doi.org/10.1021/acsabm.0c00831.
Lv YT, Zhang Y, Liu M, Qiuwaxi JN, Ashwood P, Cho SC, et al. Transplantation of human cord blood mononuclear cells and umbilical cord-derived mesenchymal stem cells in autism. J Transl Med. 2013;11:196. https://doi.org/10.1186/1479-5876-11-196.
Sun JM, Dawson G, Franz L, Howard J, McLaughlin C, Kistler B, et al. Infusion of human umbilical cord tissue mesenchymal stromal cells in children with autism spectrum disorder. Stem Cells Transl Med. 2020;9(10):1137–46. https://doi.org/10.1002/sctm.19-0434.
Lee SY, Ahn H, Jung W, Ahn J, Lee KH. A case study on autism spectrum disorder treatment using allogenic mesenchymal stem cells derived from the human umbilical Cord. Case Rep. 2020;5(106):1–7. https://doi.org/10.17303/croa.2020.5.106.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
The author contributed solely to the writing and submission of this article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wong, R.S.Y. Neuroinflammation in autism spectrum disorders: potential target for mesenchymal stem cell-based therapy. Egypt J Neurol Psychiatry Neurosurg 58, 91 (2022). https://doi.org/10.1186/s41983-022-00525-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-022-00525-2