Abstract
Background
Abducens nerve is the most common nerve affected among other cranial nerves in terms of isolated ocular palsy. Despite its prevalence and progression made in neuroimaging, incidence of idiopathic cases continues to rise.
Case presentation
We report a young adult male with no previous illnesses, who presented with sudden onset of binocular diplopia and headache and was later diagnosed with an isolated ipsilateral abducens nerve palsy secondary to an unknown cause and treated with steroids. The palsy and diplopia had resolved in 2-month time but the patient still continued to suffer from a migraine, such as headache.
Conclusion
Although, we labelled the patient as idiopathic initially, another plausible cause for this kind of presentation could be recurrent painful ophthalmoplegic neuropathy (RPON) owing to the nature of the presentation. Cases labelled as idiopathic could be attributed to a defined pathogenesis with detailed history and follow-up. Follow-up is vital for all patients, especially those labelled as idiopathic as recurrence of the illness have the chance of changing the diagnosis if supported by the detailed history and physical examination findings.
Similar content being viewed by others
Background
Abducens nerve palsy is identified to be the most common ocular motor nerve palsy [1]. Owing to its lengthy intracranial course, the nerve is highly susceptible to injury at various anatomic points. Multiple aetiologies of cranial nerve palsy have been recognized, such as traumatic, neoplastic, vascular, infectious, inflammatory, demyelination and idiopathic. In adults above the age of 50 suffering from vascular comorbidities such as diabetes and hypertension, microvascular ischemia (8–36%) is presumed to be the leading cause. However, rates of idiopathic presentations in young adults still remain high (22–30%), despite advances in neuroimaging [2].
Case presentation
A 31-year-old Indian male, not a known case of any medical condition, presented to the emergency department with a 3-day history of sudden onset diplopia and right sided frontal headache.
The headache was constant over the right frontal and retroorbital area, radiating to the nasal side of the right eye, throbbing in nature, not aggravated with light or sound and not associated with any redness or lacrimation. No history of fever, neck stiffness, photophobia, phonophobia, pulsatile tinnitus, seizures, nausea and vomiting. The horizontal diplopia was more prominent upon right lateral gaze and resolved on covering one eye (Binocular diplopia). Left lateral vision was unaffected. No pain on eye movement. Both the headache and horizontal diplopia began simultaneously for the first time.
Patient denied any recent history of travel, viral illness and head injury. There was no similar history of headaches or attacks in the family. Review of systemic and rheumatological systems was insignificant.
Physical examination was significant only for right lateral rectus palsy and left sided horizontal nystagmus. Pupils were equal, round, reactive to light and accommodating. No proptosis, ptosis or facial numbness present. No papilledema appreciated on fundoscopy. Visual acuity, other cranial nerves and upper and lower motor neuron examinations were normal (Fig. 1).
On investigation, full blood count displayed raised WBC’s (13.7 × 109/L) with a left sided neutrophil shift (80.4%), normal lymphocytic count (13.2%), normal hemoglobin (149 g/L) and normal platelets level (246). No elevated inflammatory markers (CRP 0.2 mg/L; ESR 3). Creatinine kinase levels were 742 U/L (normal 35–232). Normal blood glucose levels (5.4 mmol/L). Rheumatological screening showed normal ANA, rheumatoid factor and complement levels. Infectious work up including Lyme and syphilis serologies and CSF analysis were not performed, because patient was not sexually active and no other neurological signs were present.
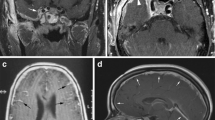
Pre and post contrast CT brain displayed a very small (5 × 6 mm) well-defined rounded peripherally hyperdense isolated lesion in the right frontal region, with central hypodensity. Lesion was suggestive of neurocysticercosis. No surrounding edema, post contrast enhancement, brain parenchymal lesion or evidence of acute cerebrovascular insult (CVA) visualized. Para nasal sinuses appeared unremarkable. MRI and MRV requested to investigate for potential causes of abducens nerve palsy, corresponded to the same area of calcification seen on the previous CT scan, which was thought to be a calcified granuloma, possibly calcified stage of neurocysticercosis. No new abnormalities or lesions and no evidence of cavernous sinus thrombosis or inflammation were discovered.
Due to the young age of our patient and sudden presentation of the headache and ipsilateral abducens nerve palsy, our differentials revolved around space occupying pathologies compressing the sixth nerve, pseudotumor cerebri, inflammatory or infectious lesions. However, physicals were not suggestive of raised intracranial pressure (normal fundoscopy), labs were normal and brain imaging did not reveal any intracranial pathology apart from the incidental neurocysticercosis located in the right frontal lobe but regardless of the discovery, it does not explain the sixth nerve palsy as it is too small in size to be compressing the nerve and they are also not anatomically related. Hence, we labelled the patient as a case of idiopathic right abducens nerve palsy secondary to an undetermined cause.
Patient was commenced on a 5-day course of Albendazole 400 mg and IV Dexamethasone 8 mg for presumed inflammatory causes. Dexamethasone was gradually tapered and patient was discharged on oral dexamethasone 4 mg (once/day) for 5 days. The headache had resolved during hospital admission but the palsy persisted on discharge.
Discussion
Our case describes a young male patient with no comorbidities, presenting with an acute episode of right sided headache and diplopia. Cranial nerve examination showed an ipsilateral right abducens nerve palsy. Neoplastic, inflammatory, ischemic, autoimmune, traumatic and space occupying lesions were excluded as history, laboratory tests and neuroimaging were inconclusive. Therefore, we diagnosed the patient with an idiopathic abducens nerve palsy and managed him with steroids to which he responded well.
Telemedicine follow-up revealed that the palsy and the diplopia had resolved in about 2-month time. The patient has not had any recurrent attacks of diplopia or paresis since then. However, he still continues to suffer from unilateral headaches, appearing most days of the week. The headache has been going on for months, since his release from the hospital and is also accompanied by phonophobia and photophobia that was not present initially.
Recurrent painful ophthalmoplegic neuropathy (RPON), previously known as ophthalmoplegic migraine (OM) can be another probable cause for our patient’s presentation. This rare condition was recognized as a variant of migraine, but then revised to RPON later on as MRI findings showed nerve thickening or gadolinium increase. However, literature indicates a strong history of migraine or a headache with migrainous features in various reported cases [3,4,5,6,7].
According to International Classification of Headache Disorders 3rd edition (2018), diagnostic criteria for RPON is characterized by at least two repeated attacks of unilateral headache associated with ipsilateral paresis of one, two, or three ocular motor nerves. This condition is most commonly seen in children but is also known to occur in adults. Oculomotor nerve is most frequently affected; followed by abducens nerve and trochlear nerve and the condition responds well to steroids. All structural lesions (orbital, parasellar and posterior fossa) should be excluded; and there should be no other diagnosis that could justify the patient’s illness [8].
We are well aware that our patient experienced only one episode of headache associated with an ocular nerve palsy (abducens nerve) and does not meet the diagnostic criteria, but it is a differential that should be considered as the nature of the symptoms described bears resemblance to that of ophthalmoplegic neuropathy and the patient could possibly present with another episode in the future.
This report, however, is subject to a few limitations. First, advanced neuroimaging tests such as MRA, CTA and DSA could not be conducted to eliminate other causes as the patient was unable to pay due to lack of insurance. Second, the history and physical examination did not support the diagnosis of Lyme disease and syphilis which led to omitting CSF analysis from diagnostic tests.
Conclusion
Abducens nerve palsy is the most common isolated ocular nerve palsy. Multiple etiologies are recognized; however, the incidence of cases attributed to idiopathic causes are rising. Cases labelled as idiopathic could be attributed to a defined pathogenesis with detailed history and follow-up. Follow-up is vital for all patients, especially those labelled as idiopathic as recurrence of the illness have the chance of changing the diagnosis if supported by the detailed history and physical examination findings.
Availability of data and materials
Not applicable.
Abbreviations
- RPON:
-
Recurrent painful ophthalmoplegic neuropathy
- OM:
-
Ophthalmoplegic migraine
- DSA:
-
Digital subtraction angiography
References
MA Tamhankar V Biousse GS Ying S Prasad PS Subramanian MS Lee 2013 Isolated third, fourth, and sixth cranial nerve palsies from presumed microvascular versus other causes: a prospective study Ophthalmology 120 11 2264 2269
C Elder C Hainline SL Galetta LJ Balcer JC Rucker 2016 Isolated abducens nerve palsy: update on evaluation and diagnosis Curr Neurol Neurosci Rep 16 8 69
N Celebisoy H Sirin F Gökçay 2005 Ophthalmoplegic migraine: two patients, one at middle age with abducens palsy Cephalalgia 25 2 151 153
Y Kobayashi Y Kondo K Uchibori J Tsuyuzaki 2017 Recurrent painful ophthalmoplegic neuropathy with residual mydriasis in an adult: should it be classified as ophthalmoplegic migraine? Internal Med (Tokyo, Japan) 56 20 2769 2772
AA Gelfand JM Gelfand P Prabakhar PJ Goadsby 2012 Ophthalmoplegic “migraine” or recurrent ophthalmoplegic cranial neuropathy: new cases and a systematic review J Child Neurol 27 6 759 766
V Lal P Sahota P Singh A Gupta S Prabhakar 2009 Ophthalmoplegia with migraine in adults: is it ophthalmoplegic migraine? Headache J Head Face Pain 49 6 838 850
C Huang M Amasanti B Lovell T Young 2017 Recurrent painful ophthalmoplegic neuropathy Pract Neurol 17 4 318
Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
ZI was directly involved in the care of the patient. ZI and RA co-wrote the manuscript and HH supervised and critiqued the final draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study. If the patient was less than 16 years, deceased, or unconscious when consent for publication was requested, written informed consent for the publication of this data was given by their parent or legal guardian.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Husain, Z.I., AlSayegh, R. & Humaidan, H. A case report of isolated abducens nerve palsy: idiopathic or ophthalmoplegic neuropathy?. Egypt J Neurol Psychiatry Neurosurg 57, 162 (2021). https://doi.org/10.1186/s41983-021-00417-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-021-00417-x