Abstract
Aim
Early assessment of patient preferences has the potential to support shared decisions in personalized precision medicine for patients with rheumatoid arthritis (RA). The aim of this study was to assess treatment preferences of patients with RA (< 5 years) with previous experience of inadequate response to first-line monotherapy.
Method
Patients were recruited (March–June 2021) via four clinics in Sweden. Potential respondents (N = 933) received an invitation to answer a digital survey. The survey included an introductory part, a discrete choice experiment (DCE) and demographic questions. Each respondent answered 11 hypothetical choice questions as part of the DCE. Patient preferences and preference heterogeneity were estimated using random parameter logit models and latent class analysis models.
Results
Patients (n = 182) assessed the most important treatment attributes out of physical functional capacity, psychosocial functional capacity, frequency of mild side effects and likelihood of severe side effects. In general, patients preferred a greater increase in functional capacity and decreased side effects. However, a substantial preference heterogeneity was identified with two underlying preference patterns. The most important attribute in the first pattern was the ‘likelihood of getting a severe side effect’. Physical functional capacity was the most important attribute in the second pattern.
Conclusion
Respondents focused their decision-making mainly on increasing their physical functional capacity or decreasing the likelihood of getting a severe side effect. These results are highly relevant from a clinical perspective to strengthen communication in shared decision making by assessing patients’ individual preferences for benefits and risks in treatment discussions.
Key points
▪ This study reveals that patients with RA (< 5 years) and inadequate response to first-line monotherapy have differing treatment preferences. They focus mainly on increasing functional capacity or on the likelihood of getting a severe side effect.
▪ Therefore, communication in shared decision-making needs to account for heterogeneity in patient preferences in order to increase patient-centeredness in personalized precision medicine.
▪ Future research needs to develop tools to strengthen patients in making shared decisions with health care professionals in order to improve personalized precision medicine.
Similar content being viewed by others
Introduction
Precision medicine aims to predict how patients will respond to a specific therapy. These prediction algorithms are based on individual characteristics such as genetic factors, age, health status, environmental exposure, concurrent therapies, etc. [1]. The main goal of precision medicine in rheumatoid arthritis (RA) is to tailor the treatment strategy based on individual patient characteristics and to help physicians and patients in setting treatment goals [2, 3]. This strategy requires tight disease control with frequent assessments of the patient and adjusting treatment until the goal is reached and sustained [4]. Shared decision-making is important in all aspects of RA care, to increase compliance and improve treatment outcomes [5]. Ideally, the decision to alter treatment should be aligned with both physicians’ clinical recommendations and patients’ personal preferences [6].
Shared decision-making requires patients and physicians to evaluate potential treatment alternatives to align decisions with both clinical and individual treatment goals and preferences [7]. RA is characterised by symptoms of pain, stiffness and fatigue [8]. The chronic and progressive nature of this autoimmune joint disease has a major and long-lasting effect on quality of life. Patients will need life-long pharmacological treatment associated with potential serious side effects [9]. The unpredictable course of the disease may also require patients to adjust to an altered functional capacity, due to limitations in almost all areas of daily life, including work and physical and social activities. In addition to its effect on everyday life, the disease process itself may further influence psychosocial functional capacity due to a direct link between inflammatory processes and depressive symptoms [10].
Assessing patients’ individual preferences is a central part of making shared treatment decisions in personalized precision medicine for patients with early RA and inadequate response to first-line monotherapy to achieve therapeutic success [11]. Identifying how patients with RA trade improvements in functional capacity against potential side effects may be an innovation for shared decision-making that has the potential to support physicians in addressing patient preferences during clinic visits [5]. Therefore, quantitative assessments of patient-relevant benefits and risks have the potential to align precision medicine with patient preferences [12]. The aim of this study was to assess the treatment preferences of patients with RA and inadequate response to first-line monotherapy.
Methods
A discrete choice experiment (DCE) was used to quantify patient preferences by revealing the relative importance of treatment attributes and underlying patterns of preferences [13]. Patients with RA (< 5 years) received an invitation by post to respond to a digital patient preference survey assessing treatment preferences.
Respondents and recruitment
Patients with RA were recruited via four rheumatology clinics in Sweden. Potential respondents were eligible for the study if they had an established RA diagnosis (< 5 years), were between 18 and 80 years of age, had inadequate response to first-line monotherapy with Methotrexate by lack of sufficient treatment effect or unbearable side effects, and were able to read and understand the questions on their own. The rationale for this inclusion was the aim to assess patients’ preferences by giving the respondents hypothetical choice scenarios of needing to change treatment due to inadequate response to first line-treatment, by using the discrete choice experiment method (DCE). We included respondents that had real experience within the last 5 years to be part of the real scenario, i.e., they had a previous inadequate response to Methotrexate, and they had to change treatment strategy.
As a first step, eligible patients were identified via the Swedish Rheumatology Quality Register. Second, an invitation to participate in the digital survey was sent out by post between March and June 2021. The invitation included information about the study, a link to the digital survey and a unique password. The invitation letter went out to around 933 potential respondents. This survey was approved by the regional ethics review board in Uppsala, Sweden (Reg no. 2020/00556). Data collection and recording, storage, and dissemination were governed by the General Data Protection Regulation and Uppsala University’s data protection and security policies. All respondents gave informed consent.
Discrete choice experiment
The main part of this survey was the DCE, used to assess treatment preferences of patients with early RA (< 5 years) and previous inadequate response to first-line monotherapy in Sweden [13]. This method is grounded in random utility theory, which suggests that individuals make rational choices to maximise utility for themselves. A value is assigned, defined as the sum of an individual's utilities of predefined attributes. This value is estimated as a function of underlying features [14]. Respondents in this DCE had to make repeated choices between two alternatives (i.e., choice questions) that were characterised by different attribute levels.
DCE development
Attributes were identified and selected in co-creation with patients and health care professionals, based on methodological recommendations [15]. Attributes were initially identified through a scoping literature review. The review encompassed articles relevant for assessing preferences among patients with RA, to get an insight into commonly used attributes. In total, 373 article abstracts were screened for potential attributes. Of these, 23 were eligible for inclusion in attribute identification after full review [6, 16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37].
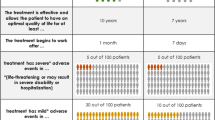
Patient-relevant attributes were further filtered and validated with patient research partners (MH, IE), health care professionals (BAE and external members of the team) and preference researchers (KB, JVJ). In April 2020, nine potential attributes were ranked by patients with RA (N = 185) using a mobile application (www.elsa.science.se), to further guide the selection of attributes. The attributes ranked were: route of administration, reduced inflammation, improved functional capacity, reduced pain and fatigue, risk of mild side effects, risk of side effects changing appearance, risk of psychological side effects, risk of severe side effects and risk of long-term damage. Semi-structured interviews were conducted with patients with RA (N = 10) to further select and frame the most important attributes and levels to be assessed in the DCE. The interviews revealed two dimensions (physical and psychosocial) of the highest ranked attribute ‘functional capacity’. Through the ranking exercise and interviews, mild and severe side effects were also identified as being among the most important attributes that patients considered in treatment decisions [38]. Refinement of the potential attributes and levels was carried out through discussions within the research team (i.e., including patients, health care professionals and researchers) and with four external rheumatologists. A total of four attributes with 3–4 levels each were selected for inclusion in the DCE (Table 1). Respondents were instructed to imagine themselves in a position of not having a well-functioning treatment and to select the alternative (treatment A or B) that best aligned with their individual preferences.
Experimental design
An experimental design for the DCE was constructed in NGene 1.0 (ChoiceMetrics, 2011). Each respondent was asked to answer 11 hypothetical choice questions (Fig. 1). Each choice question included two pairwise comparisons that were characterised by different attribute levels. Three patients with RA were interviewed to improve and validate survey comprehension and relevance before the pilot. Then, an invitation was sent by email to patients with RA, with a link to the survey. The interviewees answered the survey during a digital meeting with the first author KSB, to improve comprehension and framing of the attributes and levels. The respondents were encouraged to ‘think aloud’ while answering the survey. Based on the data retrieved in the pilot test (n = 24), a multinomial logit (MNL) model was fitted. Beta estimates were used to assign priors for the final experimental d-efficient (Bayesian) design [15]. The final design included 33 choice questions divided into three blocks and was implemented in a DCE using Lighthouse Studios v 9.8.1.
Statistical analysis
Demographic questions were analysed using descriptive analyses and presented as frequencies and percentages. Patient preferences were estimated using multivariate methods: a MNL model, a random parameter logit (RPL) model and latent class models [39]. SPSS and Nlogit were used for statistical analyses. Statistical tests were conducted at the 5% significance level and corresponding 95% confidence intervals were presented. All the attributes were dummy-coded (i.e., normalised to 0). Likelihood ratio tests and the Akaike information criterion were used to check the accuracy of the models, to determine the most appropriate model and to test for parameters that might improve the model fit [40].
A MNL model was created to account for the multilevel structure of the data. The MNL model revealed that all the attribute estimates significantly contributed to the decision-making process of respondents. The RPL model allowed further analysis of heterogeneities within the individual attributes and levels. The RPL model took unobserved heterogeneities between the survey participants into account. Because the RPL model adopted ‘random parameters’, it allowed an analysis of heterogeneities within the individual attributes and levels within the model. The extent of heterogeneous preferences within the sample was inferred from the standard deviations (SDs). The RPL model revealed significant SDs for most levels, as a result of heterogenous preferences within the sample. Therefore, exploratory analysis was generated by means of latent class models [39]. The latent class analysis (LCA) divided the population into underlying ‘latent’ preference classes with a probability of belonging to a certain class [41]. Several demographic and disease-related variables were tested for their potential impact on class membership in the LCA: age, gender, occupation, education, numeracy, health literacy, RA duration, treatment, side effects, health status, pain, worry and compliance (see Supplementary file).
The relative importance of each attributes was calculated as the difference between the highest and lowest estimates of the level for that attribute. The largest difference value was given a 1, representing the most important attribute. All other values were divided by the largest difference value (i.e., 1), resulting in a relative distance between all attributes.
Results
In total, 182 patients with RA (< 5 years) and previous inadequate response to first-line monotherapy were included in the analysis out of the 933 that received the invitation (17%). Respondents were included if they answered to the whole questionnaire and excluded if they finished the survey under 5 min. Most of the respondents were female (74%), highly educated (59%) and diagnosed with RA 2–4 years before the study (Table 2). The age span ranged from 18 to 80 years and the majority of the respondents reported the time to drug effect as < 12 months. Most of the respondents (88%) had tried at least one first-line synthetic DMARD. Respondents had experienced mild side effects (68%), side effects affecting appearance (43%), psychological side effects (39%) and severe side effects (11%).
Patient preferences in RA treatment
Respondents in general preferred increased functional capacity and decreased side effects (i.e., the sign of the beta indicated that functional capacity had a positive impact on patient choices and side effects had a negative impact). The most important attribute (based on the relative importance (RI) scored from the RPL model, see Table 3) was ‘increase in physical functional capacity’ (RI = 1), followed by ‘likelihood of severe side effects’ (RI = 0.78), ‘increase in psychosocial functional capacity’ (RI = 0.35), and ‘frequency of mild side effects’ (RI = 0.33) (Table 3).
Preference heterogeneity among RA patients
A substantial preference heterogeneity, with two latent preference patterns, was identified using the LCA model (Table 4). The preference pattern in the first group (43%) was characterised by a very high rating of the likelihood of getting a severe side effect, followed by increase in physical functional capacity, frequency of getting mild side effects, and increase in psychosocial functional capacity. In the other pattern (57%), increase in physical functional capacity was the most important attribute, followed by increase in psychosocial functional capacity, frequency of mild side effects and likelihood of severe side effects. None of the disease-related variables that were tested had an impact on class membership in the LCA (see supplementary file for covariate estimates).
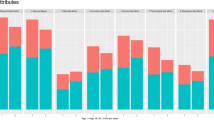
Relative importance and different aspects of RA treatment
On average (i.e., relative importance adjusted for class probability), the most important attribute was increase in physical functional capacity, followed by likelihood of getting a severe side effect (Fig. 2). Preference heterogeneity in the two latent preference patterns was estimated by calculating the RI scores. The likelihood of getting a severe side effect (infection or allergic reaction) was the most important attribute in class 1 (0.34%) respondents. The following order of attributes was normalised to the most important (i.e., 1): increase in physical functional capacity (0.50), frequency of mild side effects (0.13) and increase in psychosocial functional capacity (0.10). In class 2 respondents, the most important attribute was increase in physical functional capacity (1), followed by increase in psychosocial functional capacity (0.36), frequency of mild side effects (0.34) and likelihood of severe side effects (0.31).
Discussion
The aim of this study was to assess the treatment preferences of patients with RA (< 5 years) and previous inadequate response to first-line monotherapy. The results of the study suggested that patients with RA (< 5 years) had differing treatment preferences.
The most important treatment attribute in latent class 1 was the ‘likelihood of getting a severe side effect’ when weighted against all other treatment attributes in the DCE. In latent class 2, the ‘increase in psychosocial functional capacity’ was the most important treatment attribute. These results are highly relevant from a clinical perspective as patient preferences are recognised as essential components of shared decision-making in international treatment guidelines for RA [9].
Although general treatment guidelines provide a framework to inform treatment decisions and underline the importance of shared decision-making between patients and health care professionals, communication often fails due to differing standpoints [42]. Such preference heterogeneity (Fig. 2) underlines the importance of physicians recognising individuals’ own preferences (not the average preferences of the patient population) and accounting for that in communication about treatment goals and strategies.
Making shared treatment decisions is important because of the potential to improve clinical outcomes, overcome patients’ resistance to altering treatment and improve treatment compliance and satisfaction [5]. A shared understanding that involves tight assessments of disease activity, treatment strategies and individual preferences may improve communication between patients and clinicians and might lead to higher decision quality. Results from our study could support communication in shared decision making to account for heterogeneity in individual patients preferences’ by addressing the multidimensional span of treatment goals (i.e., physical and psychosocial) affecting everyday life, to achieve a sense of ‘a normal life’ despite the presence of chronic illness [43].
Multidimensional intervention programmes are needed to increase shared decision-making in treatment decisions, which is particularly important given the chronic nature of RA, where patients usually administer their own treatment [44]. Such interventions could focus on self-efficacy and patients’ belief in their own ability to administer treatment and be involved in treatment decisions. High self-efficacy is associated with good patient-doctor communication and patients feeling more capable of taking medications appropriately [45]. Our study has revealed significant aspects (functional capacity and side effects) to focus on when designing such intervention programmes.
Multidimensional intervention programmes also need to educate patients about treatment alternatives and promote reflection on individual treatment preferences for shared decision-making to work in clinical practice. As seen in recent shared decision interventions, digital decision aids, such as mobile health applications, may be used to inform patients about potential treatment alternatives and support patients in reflecting on their individual treatment preference and goals as a part of self-management [44]. Digital decision aids have supported patients with RA in making informed decisions when they have little or no experience with the choice situation [23]. The results from our study highlighting patients’ different treatment preferences should be considered when designing shared decision interventions, to account for individual treatment goals and preferences.
Limitations
Some limitations of this study should be recognised. The response rate was as expected (~ 20%), but it was not possible to identify any drivers of the preferences. This may be related to the narrow inclusion criteria (RA < 5 years and previous inadequate response to first-line monotherapy). The basis for the selected inclusion criteria was to assess ‘proxy’ preferences of patients ‘eligible for personalizing their treatment’ in patient-doctor communication. By revealing preferences of relatively newly diagnosed patients with RA that had previous experience in changing treatment pathway due to inadequate response. Because common clinical practice in Sweden is to initiate treatment with Methotrexate once the RA diagnosis is established. Patients will need to change treatment pathway if they experience inadequate response to treatment effect or if they experience unbearable side effects. Therefore, the results from this study should be considered to be representative of the targeted patient population, not the general RA population in Sweden. The preference patterns (of the latent class analysis) could not be associated with any of the demographic questions (i.e., age, gender, occupation, education, numeracy, health literacy, RA duration, treatment, side effects, health status, pain, worry and compliance). A possible explanation may be that the sample was too small. Quantitative preference elicitation studies with greater sample sizes may be able to find associations between patient characteristics and preferences. The results may not be generalizable to other countries as the health care systems are different. Aspects of costs and accessibility were not included in this study because treatment of RA is covered by the reimbursement system in Sweden. Further research is needed to develop intervention programmes to support patients in making shared treatment decisions in precision medicine.
In summary, this study revealed that patients have different views on what is most important in RA treatment. This study highlights the importance of understanding the heterogeneity of patient preferences. Understanding how patients weigh treatment goals against one another can inform patient-physician communication in making treatment decisions and can identify patient education needs regarding RA treatment alternatives.
Conclusions
Patients with RA (< 5 years) and inadequate response to first-line monotherapy have differing treatment preferences. They focus mainly on increasing functional capacity or on the likelihood of getting a severe side effect. Therefore, communication in shared decision-making needs to account for heterogeneity in patient preferences in order to increase patient-centeredness in personalized precision medicine. Future research needs to develop tools to strengthen patients in making shared decisions with health care professionals in order to improve personalized precision medicine.
Availability of data and material
Data from the current study are available from the corresponding author on reasonable request.
References
Giacomelli R, et al. The growing role of precision medicine for the treatment of autoimmune diseases; results of a systematic review of literature and Experts’ Consensus. Autoimmun Rev. 2021;20(2):102738.
Aletaha D. Precision medicine and management of rheumatoid arthritis. J Autoimmun. 2020;110:102405.
van Vollenhoven R. Treat-to-target in rheumatoid arthritis - are we there yet? Nat Rev Rheumatol. 2019;15(3):180–6.
Burmester GR, Pope JE. Novel treatment strategies in rheumatoid arthritis. Lancet. 2017;389(10086):2338–48.
Barton JL, Décary S. New galaxies in the universe of shared decision-making and rheumatoid arthritis. Curr Opin Rheumatol. 2020;32(3):273–8.
Durand C, et al. Patient preferences for disease-modifying antirheumatic drug treatment in rheumatoid arthritis: a systematic review. J Rheumatol. 2020;47(2):176–87.
Charles C, Gafni A. The vexing problem of defining the meaning, role and measurement of values in treatment decision-making. J Comp Eff Res. 2014;3(2):197–209.
Aletaha D, Smolen JS. Diagnosis and management of rheumatoid arthritis: a review. JAMA. 2018;320(13):1360–72.
Smolen JS, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79(6):685–99.
van Middendorp H, Evers AW. The role of psychological factors in inflammatory rheumatic diseases: from burden to tailored treatment. Best Pract Res Clin Rheumatol. 2016;30(5):932–45.
Chan SJ, et al. What are the preferences of patients with rheumatoid arthritis for treatment modification? A scoping review. patient. 2020.
Voshaar MJ, et al. Patient-centred care in established rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2015;29(4–5):643–63.
Lancsar E, Louviere J, Flynn T. Several methods to investigate relative attribute impact in stated preference experiments. Soc Sci Med. 2007;64(8):1738–53.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–77.
Bridges JF, et al. Conjoint analysis applications in health–a checklist: a report of the ISPOR good research practices for conjoint analysis task force. Value Health. 2011;14(4):403–13.
Alten R, et al. Examining patient preferences in the treatment of rheumatoid arthritis using a discrete-choice approach. Patient Prefer Adherence. 2016;10:2217–28.
Aletaha D, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–81.
Augustovski F, et al. Patient preferences for biologic agents in rheumatoid arthritis: a discrete-choice experiment. Value Health. 2013;16(2):385–93.
Harrison M, et al. Societal preferences for rheumatoid arthritis treatments: evidence from a discrete choice experiment. Rheumatology (Oxford). 2015;54(10):1816–25.
Bansback N, Harrison M, Marra C. Does introducing imprecision around probabilities for benefit and harm influence the way people value treatments? Med Decis Making. 2016;36(4):490–502.
Constantinescu F, et al. Racial disparities in treatment preferences for rheumatoid arthritis. Med Care. 2009;47(3):350–5.
Fraenkel L, et al. Patient preferences for treatment of rheumatoid arthritis. Ann Rheum Dis. 2004;63(11):1372–8.
Fraenkel L, Nowell WB, Michel G, Wiedmeyer C. Preference phenotypes to facilitate shared decision-making in rheumatoid arthritis. Ann Rheum Dis. 2018;77(5):678–83. https://doi.org/10.1136/annrheumdis-2017-212407.
Fraenkel L, et al. Unwillingness of rheumatoid arthritis patients to risk adverse effects. Rheumatology (Oxford). 2002;41(3):253–61.
Hazlewood GS, et al. Treatment preferences of patients with early rheumatoid arthritis: a discrete-choice experiment. Rheumatology (Oxford). 2016;55(11):1959–68.
Husni ME, et al. Benefit-risk trade-offs for treatment decisions in moderate-to-severe rheumatoid arthritis: focus on the patient perspective. Rheumatol Int. 2017;37(9):1423–34.
Louder AM, et al. Patient preferences regarding rheumatoid arthritis therapies: a conjoint analysis. Am Health Drug Benefits. 2016;9(2):84–93.
Nolla JM, et al. Patients’ and rheumatologists’ preferences for the attributes of biological agents used in the treatment of rheumatic diseases in Spain. Patient Prefer Adherence. 2016;10:1101–13.
Poulos C, et al. Patients’ willingness to trade off between the duration and frequency of rheumatoid arthritis treatments. Arthritis Care Res (Hoboken). 2014;66(7):1008–15.
van der Elst K, et al. Unraveling patient-preferred health and treatment outcomes in early rheumatoid arthritis: a longitudinal qualitative study. Arthritis Care Res (Hoboken). 2016;68(9):1278–87.
van Tuyl LH, et al. The patient perspective on absence of disease activity in rheumatoid arthritis: a survey to identify key domains of patient-perceived remission. Ann Rheum Dis. 2017;76(5):855–61.
van Heuckelum M, et al. Preferences of patients with rheumatoid arthritis regarding disease-modifying antirheumatic drugs: a discrete choice experiment. Patient Prefer Adherence. 2019;13:1199–211.
Loyola-Sanchez A, et al. Qualitative study of treatment preferences for rheumatoid arthritis and pharmacotherapy acceptance: indigenous patient perspectives. Arthritis Care Res (Hoboken). 2020;72(4):544–52.
Hsiao B, et al. Preference phenotypes can be used to support shared decision-making at point-of-care for patients with rheumatoid arthritis: A proof of concept study. Arthritis Care Res (Hoboken). 2018;70:343–52.
Scalone L, et al. Patients’, physicians’, nurses’, and pharmacists’ preferences on the characteristics of biologic agents used in the treatment of rheumatic diseases. Patient Prefer Adherence. 2018;12:2153–68.
Fayad F, et al. Patient preferences for rheumatoid arthritis treatments: results from the national cross-sectional LERACS study. Patient Prefer Adherence. 2018;12:1619–25.
Mathijssen EG, et al. A discrete choice experiment on preferences of patients with rheumatoid arthritis regarding disease-modifying antirheumatic drugs: the identification, refinement, and selection of attributes and levels. Patient Prefer Adherence. 2018;12:1537–55.
Bywall KS, Esbensen BA, Lason M, Heidenvall M, Erlandsson I, Johansson JV. Functional capacity vs side effects: treatment attributes to consider when individualising treatment for patients with rheumatoid arthritis. Clin Rheumatol. 2022;41(3):695–704. https://doi.org/10.1007/s10067-021-05961-8.
Greene W, Hensher D. A latent class model for discrete choice analysis: contrasts with mixed logit. Transp Res B Methodol. 2003;37:681–98.
Dziak J, et al. Sensitivity and specificity of information criteria. Briefings in bioinformatics. 2020.
Zhou M, Thayer WM, Bridges JFP. Using latent class analysis to model preference heterogeneity in health: a systematic review. Pharmacoeconomics. 2018;36(2):175–87.
Gibofsky A, et al. Comparison of patient and physician perspectives in the management of rheumatoid arthritis: results from global physician- and patient-based surveys. Health Qual Life Outcomes. 2018;16(1):211.
Hulen E, et al. Patient goals in rheumatoid arthritis care: a systematic review and qualitative synthesis. Musculoskeletal Care. 2017;15(4):295–303.
Mollard E, Michaud K. Self-management of rheumatoid arthritis: mobile applications. Curr Rheumatol Rep. 2020;23(1):2.
Oshotse C, et al. Self-efficacy and adherence behaviors in rheumatoid arthritis patients. Prev Chronic Dis. 2018;15:E127.
Acknowledgements
The Swedish Rheumatology Quality Register supported identification of eligible patients for this study. The authors would like to thank the Swedish Rheumatism Association for its support as a research partner. Our sincere gratitude to external members of the research team who have provided input in the selection and framing of the attributes and levels: Johan Askling, Lars Klareskog, Viking Huss, Kristin Waldenlind, Liselotte Tidblad and Viktor Molander.
Funding
Open access funding provided by Mälardalen University. This project was supported by Vinnova, Innovationsfonden and The Research Council of Norway, under the frame of Nordforsk (Grant agreement no. 90825, Project NORA). The funding agreement ensured the authors’ independence in designing the study, interpreting the data and writing and publishing the report. MH and IE is supported as research partners by the Swedish Rheumatism Association. ML is employed at ELSA Science.
Author information
Authors and Affiliations
Contributions
Authors KSB, BAE, MH, IE, ML, MGH and JVJ have made substantial contributions to the conceptualisation, the design of the work and the analysis and interpretation of data. Authors KSB, BAE, MH, IE, ML, MGH and JVJ authors contributed to drafting of the work and substantively revised it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Review Authority in Sweden (Dnr 2020–00556). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual respondents included in the study. The authors confirm that all patient/personal identifiers have been removed or altered so the patient(s)/person(s) described cannot be identified through the details provided.
Consent for publication
Not Applicable.
Competing interests
The authors KSB, MGH and JVJ declare no competing interests.
BAE has received speaking fees from Pfizer and Lilly.
MH and IE are supported by the Swedish Rheumatism Association as patient research partners. ML is employed at ELSA Science.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Table 1.
Latent class analysis with covariates tested for potential impact on class membership.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bywall, K.S., Esbensen, B.A., Heidenvall, M. et al. Physical function and severe side effects matter most to patients with RA (< 5 years): a discrete choice experiment assessing preferences for personalized RA treatment. BMC Rheumatol 7, 17 (2023). https://doi.org/10.1186/s41927-023-00341-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41927-023-00341-y