Abstract
Background
Although patients with rheumatic and musculoskeletal diseases (RMDs) are at increased risk for adverse outcomes of COVID-19 illness compared to healthy controls, they also have lower rates of willingness to be vaccinated. Previous research has identified reasons for vaccine hesitancy among patients with RMDs (such as concerns about side effects and flares), but little is known about what these reasons mean in the context of patients’ lives, or how vaccine decision making is experienced from a patient perspective. Our objective was to describe decision-making about COVID-19 vaccination among RMD patients.
Methods
Participants in a RMD registry were invited to complete monthly online surveys regarding COVID-19 vaccination from March-June 2021. We qualitatively analyzed comments from two open-ended survey questions reporting general experiences with vaccination and side effects. Comments were coded for attitudes towards COVID-19 vaccination, vaccine access, rheumatologic medication management around vaccination, and vaccine side effects. Themes were identified for the process and context of COVID-19 vaccine decisions, patient motivations for receiving or avoiding vaccination, and consistency of peri-vaccine medication management with current ACR guidelines.
Results
We analyzed 710 comments from 537 respondents. Commenting respondents had a mean age of 64 years, were 87% female, 94% white, and 93% received/intended to receive ≥ 1 dose of a COVID-19 vaccine. Desire for protection and a return to normal routines motivated some commenters to get vaccinated, while concerns about vaccine side effects motivated others to delay or avoid vaccination. Several commenters reported disease flares following vaccination. Some commenters did not consult their providers about vaccination and failed to withhold immunomodulatory medications during vaccination, while others withheld medications more conservatively than recommended by current ACR guidelines, either on their own or directed by their provider.
Conclusions
While most commenters were vaccine-accepting, challenges to COVID-19 vaccine uptake in the RMD population may include fears of side effects, including worsened RMD symptoms, and perceptions that vaccination is unnecessary. Addressing these concerns and beliefs may be critical for promoting vaccination in this population.
Similar content being viewed by others
Background
Patients with rheumatic and musculoskeletal diseases (RMDs) accurately view themselves as particularly vulnerable to adverse outcomes of coronavirus disease 2019 (COVID-19) [1,2,3,4,5]. However, they are also less willing than healthy controls to receive COVID-19 vaccination [4, 6, 7]. A previous survey study of participants in FORWARD, the National Data Bank for Rheumatic Diseases found that reasons for vaccine hesitancy among RMD patients include concern about side effects, lack of trust in the science/government/pharmaceutical companies, lack of testing in patients with rheumatic diseases or other conditions, and fear of flares [8]. However, little is known about the significance of these reasons in the context of RMD patients’ lives or how they make decisions about COVID-19 vaccination.
The American College of Rheumatology (ACR) has consistently recommended COVID-19 vaccination for RMD patients [9,10,11,12,13]. Initial guidelines have been updated to recommend withholding doses and/or altering vaccine timing for patients taking disease-modifying anti-rheumatic drugs (DMARDs) [13]. Knowing how and why DMARD management and vaccine timing may differ from these recommendations may help clinicians ensure optimal COVID-19 protection for RMD patients.
In this study, our objective was to qualitatively examine important considerations and motivations for RMD patients making decisions about COVID-19 vaccination. We conducted a post hoc qualitative analysis of free text comments shared by FORWARD participants who had been surveyed about their attitudes towards and experiences with COVID-19 vaccine from March-June 2021.
Methods
We conducted a post hoc thematic analysis of free-text comments from an online survey about COVID-19 vaccination informed by an interpretative phenomenological approach. Interpretative phenomenological analysis aims to elucidate participants’ lived experience of a phenomenon, while considering the influence of the social and historical context on how individuals make sense of and respond to situations [14,15,16]. This approach is suitable for exploring how patients with chronic conditions engage in a health-related decision [17,18,19,20]. Identification of themes related to peri-vaccination DMARD management was also informed by the ACR guidelines on COVID-19 vaccination [13].
Study population
Study participants were enrollees in FORWARD, a United States-based registry of patients with RMDs [21]. The registry recruits patients through rheumatology providers as well as directly through its website. FORWARD thus includes participants with systemic autoimmune diseases, as well as those with non-systemic rheumatic conditions common in the general population of the United States. FORWARD participants complete questionnaires about their health status and medications bi-annually. From March-June 2021, FORWARD participants were invited to complete monthly online surveys about COVID-19 vaccination [8, 22].
Data collection
Survey topics included COVID-19 vaccine intentions and decision-making, DMARD management peri-vaccination, and vaccine side effects (see Additional file 1). Two optional open-ended questions provided data for our analysis (see Additional file 2). The study was approved by the Institutional Review Board of Via Christi Hospitals Wichita, Inc (FWA00001005; IRB00001674). Written informed consent was obtained before patients completed surveys.
Data analysis
The unit of analysis was each free text comment. Free-text data was reviewed by four authors (YPS, SH, NN, MS) who proposed a codebook for labeling the comments for relevancy to COVID-19 vaccination and topics of interest, including vaccine intentions, concerns, access, and peri-vaccine medication management. Three authors (SH, NN, and MS) coded the data using Microsoft Excel. Each comment was coded by two authors. Pairs of coders resolved discrepancies in coding by discussing until consensus was reached.
After excluding comments irrelevant to COVID-19 vaccination, thematic analysis was performed by SH, NN, MS and YPS. Team members carefully re-read the comments grouped by codes and took notes about patterns related to vaccine intentions, the patient decision-making process, motivations for vaccine decisions, and DMARD management peri-vaccination. Themes were drafted based on notes and refined through weekly group discussions and further review of comments and note taking.
Results
Out of 14,704 participants invited, 4,265 completed ≥ 1 COVID-19 vaccine questionnaires; 1082 respondents left a total of 1552 free text comments. After excluding irrelevant comments, 710 comments from 537 commenters were analyzed (Fig. 1).
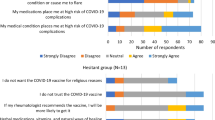
Table 1 shows the characteristics of these 537 commenters. Sixty-four percent were 65 or older, 87% were female, 94% were white, and 15% reported previous COVID-19 illness. Although the majority (93%) received/intended to receive at least one dose of a COVID-19 vaccine, concerns about vaccines were commonly expressed (83%) among both vaccinated and unvaccinated commenters. Concerns included side effects (71%) and the effects of vaccination on DMARD management and flares (20%).
Thematic analysis yielded 15 subthemes organized into four main themes: process and context of vaccine decision-making, motivations for receiving a COVID-19 vaccine, motivations for avoiding vaccination, and peri-vaccine DMARD management. Table 2 presents the themes, subthemes, and illustrative quotes.
Process and context of vaccine decision making
Commenters were categorized into three main groups based on COVID-19 vaccination intentions: (1) intending to get or already vaccinated, (2) unsure about vaccination, and (3) not intending to get vaccinated. Many in group 1 expressed eagerness and optimism about the protection they hoped the vaccine would provide or gratitude and relief about getting vaccinated. Some even positively interpreted perceived side effects as a sign the vaccine was working:
I had a reaction after both vaccine injections which made me very happy! Yippee because it means I mounted an immune response.
In contrast, commenters in group 3 resisted vaccination because they believed vaccines were unsafe or unnecessary, or they wished to avoid unwanted effects on their RMD or other health issues.
Attitudes towards vaccination in group 2, the undecided commenters, were more mixed. Some commenters strongly preferred to avoid vaccination but remained willing to be vaccinated if required. Others were interested in vaccination but wanted input from a health care provider first. Others wanted to wait for more evidence on how the vaccine might affect their health condition(s):
I need it to be tested and studied in folks with fibromyalgia and orthostasis and if it can be used safely used for us with these conditions, then I might get the vaccine, just not until then […]
Subtheme: Ongoing process of weighing risks and benefits
Decision-making about vaccination often involved monitoring factors that evolved throughout the pandemic, such as the local level of COVID-19 transmission, availability of vaccines, and their reported risks. The decision process continued even after commenters were vaccinated. One commenter’s decision was influenced by their experience of side effects after their first vaccine dose:
I got the petechiae about a week after the shot. Because of that, I decided against getting the 2nd dose.
Subtheme: Involvement of health care providers in vaccination decisions
Some commenters made vaccine-related decisions without consulting providers or received provider advice only after their first dose. Others actively sought rheumatologist advice about vaccine choice, timing, and DMARD management. Because vaccine-related knowledge and recommendations were rapidly evolving, instructions from rheumatologists also changed over time:
My rheumatologist for first vaccine told me to wait three days after shot and then resume mtx but no changes in Arava. […] Between first and second vaccine shot, rh academy changed advice and so I was to wait 7 days after vaccine shot.
Subtheme: Vaccine access
Vaccine access was an important contextual factor shaping commenters’ choices. Throughout March-June 2021, when comments were submitted, COVID-19 vaccine supplies were limited, and availability depended on the commenter’s location and date of response. While some commenters had early access to vaccines, e.g. through work, many others reported frustration with the difficulty of obtaining vaccination and criticized local policies affecting vaccine access. For example, one commenter complained about Canada’s policy of delaying second vaccine doses until most people received a first dose. Commenters were also frustrated that people with RMDs were not prioritized for vaccination along with other high-risk groups.
Commenters preferred certain vaccines for safety or convenience reasons. Some even delayed vaccination due to dissatisfaction with available options in their region:
Very nervous about having my vaccine shots with having Lupus. the aftereffects [sic] of the second shot can be severe. waiting for the J &J shot. they are supposed to be safer.
Subtheme: Previous or current COVID-19 illness
Some commenters who contracted COVID-19 were advised to wait before receiving a vaccine:
Was diagnosed with COVID-19 in March, spent 10 days in the hospital, doctor said to wait 6 months before trying to get the vaccine.
Others were fearful of the vaccine due to their experiences with COVID-19 illness:
I had a bad cough, fever, and could not sleep in my bed because I couldn't breathe when I laid down, so I slept in my recliner. I coughed for nearly 6 weeks […] I am doing very well now and do not want to risk the virus shot.
Motivations for receiving a COVID-19 vaccine
Subtheme: Desire for safety
Many commenters sought vaccination to protect themselves from COVID-19. Some perceived themselves as especially vulnerable due to their health conditions:
In addition to RA I am also immuno-compromised due to subtotal colectomy, chronic kidney disease, fibromyalgia, anemic, a [sic] several other conditions. I have been fearful of coming down with the Covid virus.
Other commenters voiced concern about exposure to COVID-19 at work: “I am 67 and working full time as a Nurse Leader in a medical center and see COVID patients occasionally in Perinatal.”
Subtheme: Desire to return to normal routines
During the pandemic, commenters paused treatment routines and daily activities to reduce risk of COVID-19 illness and severe outcomes. Vaccination was seen as the pathway to safely resuming needed treatments for RMDs and valued activities:
I am hoping that after my second vaccine I can go back to the gym.
Subtheme: External pressures to vaccinate
External pressures were also important motivators, especially for those uncertain about vaccination. Some commenters were willing to consider vaccination if it was required/mandated, or if requested by family or friends:
If there comes a point where we all must produce vaccine passports in order to travel internationally, then I will get the vaccine but until then, I don't plan on getting it.
If I am forced to get one because of other people's fears, ie. wouldn't be able to see family members if I don't get one […] I will consider it […]
Motivations for avoiding COVID-19 vaccination
Subtheme: Concerns about side effects
Vaccine side effects were an important concern for many commenters, even those planning to be vaccinated. Commenters were afraid of serious side effects (e.g. blood clots and severe allergic reactions) as well as long-term consequences:
I’m afraid of the long term effects that can be serious to us and what harm it will do to our young children. I wish I had not gotten it.
Others were afraid the vaccine would weaken their immune system: “not interested in getting a vaccine thay [sic] may affect my body's immune system.” Some commenters were not willing to risk facing vaccine side effects in addition to existing health problems:
As time progresses, I am receiving more and more diagnoses. […] I just don't want to add side effects from a vaccine to make my life even more miserable, especially when these vaccines don't stop COVID-19, they just reduce the severity of it.
Even those who got vaccinated were apprehensive about their second dose, which was believed to have greater side effects than the first dose. Some concerns were based on other vaccine experiences:
10 years ago I had a very bad reaction to a pneumonia shot. I have mailed a lot of information to my rheumatologist and internist and am waiting on their advice.
Subtheme: Concerns about DMARD management/flares
Concerns about DMARD management and RMD flares were important for many commenters, regardless of vaccination intention. Some commenters did not want to interrupt their DMARD treatment for vaccination:
My rheumatologist said I would have to be off the orencia infusion for 3 months to complete the vaccination process. I'm just not willing to do that at this point. I am finally feeling a little better.
In this case, the rheumatologist’s recommendation was more conservative than ACR guidelines and resulted in the commenter’s decision against vaccination. Commenters also wanted to avoid flares to maintain social and employment roles:
I feel it is more important for me to be strong enough to care for her [mother-in-law] than to risk having a flare [from vaccination] that could debilitate me for weeks.
Some commenters who chose to get vaccinated also reported negative experiences with post-vaccination flares. Some directly attributed their flare symptoms to vaccination: “I had the worst flare up that I've had in years following the vaccine.” Others were concerned about vaccination triggering disease progression or worsening:
Yesterday was the two-week point after my second shot, yet I still felt chills and debilitating fatigue. I hope this is temporary and not because the vaccination caused my fibromyalgia symptoms to re-emerge.
In other cases, commenters felt that withholding DMARDs during vaccination might have worsened RMD symptoms:
Definitely missed the dose of my Cimzia. It was delayed by 3 weeks due to vaccinations. Also had my epidural injections delayed by 5 weeks due to the vaccinations. Very hard to move around without pain and sciatic involvement.
A few commenters reported severe post-vaccination flares that impacted daily functioning:
As with the first dose, I had one day of overall body aches that felt like an RA flare. But then a couple of days later, the missing Xeljanx hit me HARD. Everything hurt, I had little energy, and I was nauseated (a fairly typical RA flare presentation for me, but far worse). I even took a half-day off from work, which is rare for me […] It was a horrid experience, and I'll be hesitant to take similar advice again.
Subtheme: Perception of low risk
The perception that COVID-19 posed little risk contributed to some commenters viewing vaccination as unnecessary. Some believed they were unlikely to become infected because of precautions they were taking, or because their immune system would protect them:
During the pandemic last February I traveled throughout SE Asia. I was in rooms with thousands of people in Seoul airport, in many crowds of people in Vietnam and Burma […] all with no politically correct masks. Having a healthy immune system via a plant-based lifestyle is more important than subjecting your body to experimental drugs.
Some commenters thought the risk of COVID-19 illness was exaggerated (“The survival rate is very high for most people”) or trusted they could be successfully treated if infected (“I have 2 doctors with 100 percent success rate treating COVID. No need for an experimental biological agent”).
Subtheme: Doubts about vaccine effectiveness
Doubts about vaccine effectiveness caused some commenters to question whether vaccines were worthwhile. Some believed vaccines were ineffective for preventing COVID-19 illness: “don’t want to risk and add more to my problems especially since the vaccine DOES not prevent or cure Covid.” One commenter wondered whether vaccines benefited patients with previous COVID-19 illness:
I have heard nothing from doctors or scientists to show why people who had Covid should get a vaccine. Some say that the antibodies only last in the body for a few months, so why does the vaccine last longer? What evidence shows the length of time the vaccine lasts?
Many commenters also wondered whether RMD treatments would reduce vaccine effectiveness, although this concern typically did not dissuade commenters from vaccination. A few commenters were worried by negative antibody test results following vaccination: “Others I know on meds for autoimmune diseases are also testing negative for antibodies. What a false sense of protection since Feb./March.”
Subtheme: Mistrust
Mistrust reinforced commenters’ fears about potential side effects of COVID-19 vaccines. Misconceptions about the nature of the vaccines and how they work, as well as the vaccine testing and approval process, contributed to commenters’ suspicions. Some cited a lack of trust in political leaders, health authorities, or pharmaceutical companies:
I don't mind vaccines in general, but this particular vaccine I don't trust. You would expect mild side effects from vaccines like the flu. Not the serious side effects of the COVID vaccine, or even deaths. Don't trust the drug companies for this specific vaccine.
Commenters mistrusted mRNA vaccines, which were perceived as a new and unfamiliar technology: “There is zero short or long term data on manipulating the immune system to generate a non human protein. We have no idea what will happen to the masses who took the mRNA or DNA injections.” Commenters also worried about becoming a ‘guinea pig’ by taking vaccines perceived as ‘experimental’ and inadequately tested or reviewed:
I would never jeopardize my health and well-being by talking [sic] the experimental gene therapy shot they have mislabeled as a vaccine.
They went through FDA processes to approval to [sic] fast for my liking.
Peri-vaccine DMARD management
Subtheme: Need for guidance on DMARD management
Commenters wanted to know whether DMARDs could reduce vaccine effectiveness, and how to manage DMARDS peri-vaccination. They often sought input from rheumatologists or other providers, such as infusion center staff and pharmacists. Commenters were sometimes confused about DMARD management peri-vaccination, either due to inadequate information or because the advice they received conflicted with how they usually managed DMARDs around other vaccinations:
I’m a little confused about the timing of receiving a Covid vaccination between Remicade infusions. My rheumatologist’s office gave me the impression I could get the vaccination any time but in the past I was told to time vaccinations half way between infusions so I’m waiting until then.
Subtheme: Failure to withhold DMARDs
Most DMARD management practices discussed by commenters were consistent with current ACR guidelines. However, in some cases, failure to withhold DMARDs or to withhold them for long enough may have reduced vaccine immunogenicity. For example, one commenter suspected that taking methotrexate during vaccination contributed to inadequate vaccine response:
I was vaccinated and still got COVID. I think that I was on methotrexate when vaccinated may have had something to do with me getting sick.
Subtheme: Withheld DMARDs more conservatively than recommended by current ACR guidelines
Others withheld DMARDs more conservatively than recommended by ACR guidelines. This was sometimes in addition to having stopped DMARDs due to concerns about immunosuppression as a risk factor for severe COVID-19 illness:
I have been compliant with all my RA meds for over 20 years, but as of December 2020 I stopped taking my Enbrel because my white blood cell count was very low…I was afraid if I got Covid I would not be able to fight it. I had no flare so I stayed off my meds (enbrel/methotrexate) until I received my vaccine.
Prolonged periods without regular DMARD use sometimes led to RMD symptoms worsening. For example, one commenter withheld both methotrexate and adalimumab:
[…] both [my medications] are on hold until two weeks after my second vaccine. I most definitely see a pain increase because of this, but feel the vaccine is quite important.
Discussion
Our qualitative analysis highlights how various factors affect perceptions of vaccine risks and benefits among RMD patients. Commenters made decisions about COVID-19 vaccination through an ongoing process of weighing need for vaccination (risks of COVID-19, perceived vaccine effectiveness) against vaccine-related concerns (side effects and potential health impact, especially with respect to their RMD). This is consistent with the Necessity Concerns Framework (NCF), which posits that beliefs about medication necessity and concerns about adverse effects influence adherence behavior [23, 24]. The NCF was previously used to conceptualize COVID-19 vaccine willingness in young adults [25]. While most commenters were open to vaccination, many reluctant to get vaccinated had concerns about side effects and the potential for RMD flares, which they felt outweighed vaccine benefits. As mentioned in the results Sects. 3.3.1 (subtheme: concerns about side effects) and 3.3.2 (subtheme: concerns about DMARD management/flares), we found that even patients who intend to get vaccinated often have concerns about COVID-19 vaccines. It is important for rheumatologists to address patient concerns about COVID-19 vaccination, since patients must be willing to undergo periodic boosters in order to maintain protection against COVID-19. Patients whose concerns outweigh their perception of the benefits may ultimately decide not to get vaccinated for COVID-19 in the future, even if they have been willing to get vaccinated in the past. Rheumatology providers can help facilitate patient decision making about vaccines by providing information to promote more accurate perceptions of the risks and benefits of COVID-19 vaccination. Attitudes towards COVID-19 vaccines can change over time [26], and provider endorsement may increase vaccine uptake among the reluctant [27].
We identified motivations for resisting COVID-19 vaccines consistent with those previously reported [6, 7, 27, 28]. RMD patients may fear the vaccine’s impact on their health or mistrust those promoting vaccination. They may also doubt the vaccine’s effectiveness or prefer non-medical alternatives. Patients may also need time to consider vaccination, as they may be unconvinced by current safety data or overwhelmed while navigating multiple information sources. Some commenters had negative attitudes shaped by misinformation, as described in previous qualitative research. Reported examples of misinformation included rumors about minorities being targeted as ‘guinea pigs’, the idea that COVID-19 and/or vaccines were part of a conspiracy to control the population, and the belief that vaccines cause COVID-19 [29,30,31].
Commenters reported experiencing RMD flares following COVID-19 vaccination; these were attributed to withholding DMARDs, to direct effects of vaccination, or to a combination of both. Surveys of RMD patients found that 3–15% experience flares following COVID-19 vaccination, but most do not limit daily functioning [32,33,34,35,36].
As mentioned in the results Sect. 3.1.2 (subtheme: involvement of health care providers in vaccination decisions), patients sometimes looked to their rheumatologists and other health care providers for advice regarding COVID-19 vaccination, and it appears that a provider’s recommendation for vaccination or lack thereof was influential on patients’ decisions about vaccination. In a previous quantitative analysis of our survey responses, among unvaccinated patients, approximately 10% reported that lack of recommendation from the rheumatologist contributed to their reluctance to be vaccinated [8]. Among the cohort analyzed in this study, 140/238 (58.8%) reported that their rheumatologist recommended COVID-19 vaccination. However, commenters did not always seek provider input on coordinating vaccines with DMARDs. Commenters reported both failure to withhold and unnecessary withholding of DMARDs which potentially worsened RMD symptoms. Changing recommendations about DMARD management during our data collection period likely contributed to these experiences. Previous research supports our findings. A survey of vaccinated RMD patients found 18% of participants did not communicate with their provider about vaccination, and 71% did not withhold DMARDs peri-vaccination [36]. The prevalence of pandemic-period DMARD nonadherence is between 7.5 and 14.8% [37, 38]. To maximize vaccine effectiveness, it is important for rheumatologists to communicate with patients about coordination of DMARDs peri-vaccination. Patients want reassurance from health care providers about vaccine effectiveness and safety, and guidance about DMARD management.
The strengths of our study were our opportunity to collect comments from a large population of survey participants (4265) and that comments captured diverse attitudes towards vaccination. Our study also has limitations related to our data source. Commenters were all internet users, mostly elderly, white residents of the United States, and findings may not reflect attitudes of RMD patients with other sociodemographic characteristics. The majority of patients included in the analysis (56%) had rheumatoid arthritis, and many had non-systemic rheumatologic conditions. These characteristics of our study cohort limit the transferability of our findings to patients with other systemic autoimmune diseases, minorities, and younger patients. Future studies are needed to explore the attitudes of other RMD patient populations, including those in other parts of the world. Our results may also be affected by self-selection bias, since commenters may differ in important ways from those who did not respond or share comments. Since this was a post-hoc analysis of survey data, we did not have the opportunity to design a sampling strategy to focus on perspectives of subgroups of interest, such as patients with specific rheumatic diseases or the vaccine hesitant. The post-hoc nature of this analysis also precluded designing open-ended questions to capture perspectives in greater depth and with more consistency across respondents.
Conclusions
Our qualitative analysis described RMD patient perspectives on COVID-19 vaccination, including the decision-making process, factors that encourage/discourage vaccination, and peri-vaccine DMARD management. Patients who are reluctant to vaccinate may perceive the risks of vaccination to be greater than the benefits. RMD flares are an important concern for patients both when deciding whether to receive vaccination as well as when evaluating their experience post-vaccination. There is a need for rheumatology providers to address concerns about COVID-19 vaccination, and to support patients in managing subsequent flares. Providing patients with accurate information about the risks and benefits of vaccines may enable the vaccine-hesitant to reevaluate their perceptions and make informed decisions about vaccination.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RMD:
-
Rheumatic and musculoskeletal diseases
- COVID-19:
-
Coronavirus disease 2019
- ACR:
-
American College of Rheumatology
- DMARD:
-
Disease-modifying anti-rheumatic drugs
- NCF:
-
Necessity Concerns Framework
References
D’Silva KM, Jorge A, Cohen A, McCormick N, Zhang Y, Wallace ZS, et al. COVID-19 outcomes in patients with systemic autoimmune rheumatic diseases compared to the general population: a US multicenter. Comp Cohort Study Arthritis Rheumatol. 2021;73(6):914–20.
England BR, Roul P, Yang Y, Kalil AC, Michaud K, Thiele GM, et al. Risk of COVID-19 in rheumatoid arthritis: a national veterans affairs matched cohort study in at-risk individuals. Arthritis Rheumatol. 2021;73:2179–88. https://doi.org/10.1002/art.41800.
Bachiller-Corral J, Boteanu A, Garcia-Villanueva MJ, de la Puente C, Revenga M, Diaz-Miguel MC, et al. Risk of severe COVID-19 infection in patients with inflammatory rheumatic diseases. J Rheumatol. 2021;48(7):1098–102.
Priori R, Pellegrino G, Colafrancesco S, Alessandri C, Ceccarelli F, Di Franco M, et al. SARS-CoV-2 vaccine hesitancy among patients with rheumatic and musculoskeletal diseases: a message for rheumatologists. Ann Rheum Dis. 2021;80(7):953–4.
Cook C, Cox H, Fu X, Zhang Y, Stone JH, Choi HK, et al. Perceived risk and associated shielding behaviors in patients with rheumatoid arthritis during the coronavirus 2019 pandemic. ACR Open Rheumatol. 2021;3(12):834–41.
Yurttas B, Poyraz BC, Sut N, Ozdede A, Oztas M, Uğurlu S, et al. Willingness to get the COVID-19 vaccine among patients with rheumatic diseases, healthcare workers and general population in Turkey: a web-based survey. Rheumatol Int. 2021;41:1–10.
Gaur P, Agrawat H, Shukla A. COVID-19 vaccine hesitancy in patients with systemic autoimmune rheumatic disease: an interview-based survey. Rheumatol Int. 2021;41:1–5.
Wipfler K, Cornish A, Freifeld A, Katz P, Michaud K. Factors associated with COVID-19 vaccine hesitancy among individuals with rheumatic disease. Arthritis Rheumatol. 2021;73(Suppl 10).
ACR COVID-19 Vaccine Clinical Guidance Task Force. COVID-19 vaccine clinical guidance summary for patients with rheumatic and musculoskeletal diseases [Internet]. 2021 [cited 2021 Aug 19]. Available from: https://www.rheumatology.org/Portals/0/Files/COVID-19-Vaccine-Clinical-Guidance-Rheumatic-Diseases-Summary.pdf
Curtis JR, Johnson SR, Anthony DD, Arasaratnam RJ, Baden LR, Bass AR, et al. American College of Rheumatology Guidance for COVID-19 vaccination in patients with rheumatic and musculoskeletal diseases: version 1. Arthritis Rheumatol. 2021;73(7):1093–107.
Curtis JR, Johnson SR, Anthony DD, Arasaratnam RJ, Baden LR, Bass AR, et al. American College of Rheumatology Guidance for COVID-19 vaccination in patients with rheumatic and musculoskeletal diseases: version 2. Arthritis Rheumatol. 2021;73(8):e30-45.
Curtis JR, Johnson SR, Anthony DD, Arasaratnam RJ, Baden LR, Bass AR, et al. American College of Rheumatology Guidance for COVID-19 Vaccination in Patients With Rheumatic and Musculoskeletal Diseases: Version 3. Arthritis Rheumatol. 2021;73(10):e60-75.
ACR COVID-19 Vaccine Clinical Guidance Task Force. COVID-19 vaccine clinical guidance summary for patients with rheumatic and musculoskeletal diseases: Version 5. [Internet]. 2022 [cited 2022 Feb 28]. Available from: https://www.rheumatology.org/Portals/0/Files/COVID-19-Vaccine-Clinical-Guidance-Rheumatic-Diseases-Summary.pdf
Rodriguez A, Smith J. Phenomenology as a healthcare research method. Evid Based Nurs. 2018;21(4):96–8.
McInally W, Gray-Brunton C. Research made simple: using multiperspective interpretative phenomenological analysis to explore healthcare phenomena. Evid Based Nurs. 2021;24(3):71–3.
Sibeoni J, Verneuil L, Manolios E, Révah-Levy A. A specific method for qualitative medical research: the IPSE (Inductive Process to analyze the Structure of lived Experience) approach. BMC Med Res Methodol. 2020;20:216.
Greenfield BH, Jensen GM. Understanding the lived experiences of patients: application of a phenomenological approach to ethics. Phys Ther. 2010;90(8):1185–97.
Lundy TL. Exploring the lived experience of decision-making among family caregivers of black older adults with advanced chronic illnesses [Internet]. City University of New York; 2020 [cited 2022 Feb 28]. Available from: https://academicworks.cuny.edu/cgi/viewcontent.cgi?article=4781&context=gc_etds
Sudlow AC, Pournaras DJ, Heneghan H, Bodnar Z, le Roux CW, McGillicuddy D. An exploration of the patient lived experience of remission and relapse of type 2 diabetes following bariatric surgery. Obes Surg. 2021;31(9):3919–25.
Chan NN, Ong KW, Siau CS, Lee KW, Peh SC, Yacob S, et al. The lived experiences of a COVID-19 immunization programme: vaccine hesitancy and vaccine refusal. BMC Public Health. 2022;22(1):296.
Wolfe F, Michaud K. The National Data Bank for rheumatic diseases: a multi-registry rheumatic disease data bank. Rheumatol Oxf Engl. 2011;50(1):16–24.
Michaud K, Cornish A, Freifeld A, Katz P, Wipfler K. COVID-19 mRNA vaccine side effects among individuals with rheumatic disease. Arthritis Rheumatol. 2021;73(suppl 10).
Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–67.
Horne R, Chapman SCE, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the necessity-concerns framework. PLoS ONE. 2013;8(12):e80633.
Vollmann M, Salewski C. To get vaccinated, or not to get vaccinated, that is the question: Illness representations about COVID-19 and perceptions about COVID-19 vaccination as predictors of COVID-19 vaccination willingness among young adults in The Netherlands. Vaccines. 2021;9(9):941.
Kirzinger A, Sparks G, Brodie M. KFF COVID-19 Vaccine Monitor: In Their Own Words, Six Months Later [Internet]. 2021 Jul [cited 2021 Sep 21]. Available from: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-in-their-own-words-six-months-later/
Putman M, Kennedy K, Sirotich E, Liew JW, Sattui SE, Moni TT, et al. COVID-19 vaccine perceptions and uptake: results from the COVID-19 Global Rheumatology Alliance Vaccine Survey. Lancet Rheumatol. 2022;4(4):e237–40.
Felten R, Dubois M, Ugarte-Gil MF, Chaudier A, Kawka L, Bergier H, et al. Cluster analysis reveals 3 main patterns of behavior towards SARS-CoV-2 vaccination in patients with autoimmune and inflammatory diseases. Rheumatol Oxf Engl. 2021;keab432.
Geana MV, Anderson S, Ramaswamy M. COVID-19 vaccine hesitancy among women leaving jails: a qualitative study. Public Health Nurs. 2021. https://doi.org/10.1111/phn.12922.
Lockyer B, Islam S, Rahman A, Dickerson J, Pickett K, Sheldon T, et al. Understanding COVID-19 misinformation and vaccine hesitancy in context: Findings from a qualitative study involving citizens in Bradford, UK. Health Expect. 2021;24(4):1158–67.
Fadda M, Suggs LS, Albanese E. Willingness to vaccinate against Covid-19: a qualitative study involving older adults from Southern Switzerland. Vaccine X. 2021;8:100108.
Barbhaiya M, Levine JM, Bykerk VP, Jannat-Khah D, Mandl LA. Systemic rheumatic disease flares after SARS-CoV-2 vaccination among rheumatology outpatients in New York City. Ann Rheum Dis. 2021;80(10):1352–4.
Connolly CM, Ruddy JA, Boyarsky BJ, Barbur I, Werbel WA, Geetha D, et al. Disease flare and reactogenicity in patients with rheumatic and musculoskeletal diseases following two-dose SARS-CoV-2 messenger RNA vaccination. Arthritis Rheumatol. 2021;74:28–32.
Machado PM, Lawson-Tovey S, Hyrich K, Carmona L, Gossec L, Mateus E, et al. Lb0002 covid-19 vaccine safety in patients with rheumatic and musculoskeletal disease. Ann Rheum Dis. 2021;80(Suppl 1):199–200.
Felten R, Kawka L, Dubois M, Ugarte-Gil MF, Fuentes-Silva Y, Piga M, et al. Tolerance of COVID-19 vaccination in patients with systemic lupus erythematosus: the international VACOLUP study. Lancet Rheumatol. 2021;3(9):e613–5.
Sattui SE, Liew JW, Kennedy K, Sirotich E, Putman M, Moni TT, et al. Early experience of COVID-19 vaccination in adults with systemic rheumatic diseases: results from the COVID-19 Global Rheumatology Alliance Vaccine Survey. RMD Open. 2021;7(3): e001814.
Rebić N, Park J, Garg R, Ellis U, Kelly A, Davidson E, et al. A rapid review of medication taking (‘adherence’) among patients with rheumatic diseases during the COVID-19 pandemic. Arthritis Care Res. 2021.
Dharia T, Venkatachalam S, Baker JF, Banerjee S, Curtis D, Danila MI, et al. Medication interruptions and subsequent disease flares during the COVID-19 pandemic: a longitudinal online study of patients with rheumatic disease. Arthritis Care Res. 2021;2151–4658.
Acknowledgements
Not applicable.
Funding
This was an unfunded study. Support for SH and NN was provided by the University of Michigan Undergraduate Research Opportunity Program, and support for MS was provided by the University of Nebraska Medical Center Summer Undergraduate Research Program. The University of Michigan and University of Nebraska had no role in design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Individual author contributions: YS (study design, analysis, drafting and revising the manuscript), SH (analysis, manuscript review and revision), NN (analysis, manuscript review and revision), MS (analysis, manuscript review and revision), KW (data collection, analysis, manuscript review and revision), BIW (study design, interpretation of data, manuscript review and revision), KM (study design, interpretation of data, manuscript review and revision). All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of Via Christi Hospitals Wichita, Inc (FWA00001005; IRB00001674). Written informed consent was obtained before patients completed surveys. All methods were performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. COVID-19 vaccine questionnaire. Questionnaire about COVID-19 vaccination that was administered to study participants online.
Additional file 2
. Open ended survey questions. Free text responses to these open ended survey questions provided data for our analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shaw, Y.P., Hustek, S., Nguyen, N. et al. Rheumatic disease patient decision-making about COVID-19 vaccination: a qualitative analysis. BMC Rheumatol 6, 76 (2022). https://doi.org/10.1186/s41927-022-00307-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41927-022-00307-6