Abstract
Background
The value of somatostatin-analogon PET tracers in theranostics in cranial meningioma has been demonstrated in several studies however, the value of semi-quantitative parameters for therapy and patient outcome is still unclear.
Methods
A retrospective study was performed comparing measured semi-quantitative 68Ga-DOTANOC PET/CT parameters (maximum standardized uptake value = SUVmax, mean standardized uptake value = SUVmean, and metabolic tumor volume = MTV) and calculated ratios (SUVmax tumor/to pituitary gland, SUVmax tumor to superior sinus sagittalis), versus WHO grades and overall outcome. Patients with histological confirmed meningioma or high probability for meningioma in previous cranial MRI were eligible.
Results
Thirty-two patients from January 2018 to February 2023 were retrospectively included. WHO grade I meningioma was confirmed in 17 patients, WHO grade II in five patients, WHO grade III in two patients, while in eight patients diagnosis was solely based on MRI and 68Ga-DOTANOC PET/CT findings. In 12 cases stable disease was present, in 15 cases radiation therapy was chosen, in three cases neurosurgery was preferred while in two cases palliative care was chosen. Median SUVmax values increased with WHO grade (15.84, 17.22, and 28.4, p = 0.134, Kruskal–Wallis-test) and no statistically significant difference was present for MTV, SUVmax, and calculated ratios, although the ratio for SUVmax tumor to superior sinus sagittalis had the lowest value of p = 0.067.
Conclusion
Increased SUVmax values in the tumor in 68Ga-DOTANOC PET/CT are associated with higher WHO grade, although further studies including larger patient collectives are needed to solidify this hypothesis.
Similar content being viewed by others
Introduction
Meningiomas are the most common intracranial tumor, evolving from a mesodermal line. They account for approximately 13–26% of all central nervous tumors (Vernooij et al. 2007; Marosi et al. 2008). Although generally considered benign entities with a slow growth rate, they can show invasive growth and high recurrence rate. Meningiomas are divided into three histological sub-types according to the World Health Organization (WHO) classification: grade I: benign, grade II: atypical, and grade III: anaplastic or malignant. Recurrence rates increase from up to 25% for grade I to up to 94% for grade III. While five-year survival rate for grade I exceeds 80%, it is poorer for malignant and atypical meningiomas at less than 60% (Marosi et al. 2008). Treatment is usually surgical when localized and radiotherapy in more widespread lesions, while peptide receptor radionuclide therapy (PRRT) could achieve stable disease in up to 66.6% (Filippi et al. 2022; Pirisino et al. 2022). Although seen as gold standard in grade III, radiotherapy is debated for grade II and generally not indicated for grade I when resectable (Maggio et al. 2021).
According to the current European Association of Neuro-Oncology (EANO) guideline (Goldbrunner et al. 2021), the diagnosis of intracranial meningioma can be based on MRI and CT scans with high probability in most cases. PET using somatostatin analogs can delineate meningiomas expressing somatostatin receptor 2, although this is not available as standard practice yet. Furthermore, for surgery guidance PET images should be integrated especially for intraosseous meningioma. The most commonly used somatostatin analogs or somatostatin receptor (SSTR) ligands are [68Ga-DOTA0-Tyr3] octreotide (68Ga-DOTATOC), [68Ga-DOTA0-Tyr3] octreotide (68Ga-DOTATATE), and [68Ga-DOTA0-1NaI3] octreotide (68Ga-DOTANOC). Gallium-68has a physical half-life of 68min and can be obtained from a Germanium-68/Gallium-68generator system, enabling in-house production without the need for a cyclotron (Galldiks et al. 2017). Since SSTR ligands do not cross the blood/brain barrier, high contrast and excellent target-to-background contrast are provided, enhancing the diagnostic abilities of PET/CT.
Objective
To determine the value of semi-quantitative parameters in 68Ga-DOTANOC PET/CT in intracranial meningiomas in a retrospective single-center study.
Patients and methods
This retrospective single-center study included patients undergoing 68Ga-DOTANOC PET/CT scans at our division from January 2018 to February 2023 for the diagnosis of suspected intracranial meningioma or the restaging of remnant and/or recurrent meningioma. Patients from both sexes and from all ages were eligible.
The Gallium-68labelled DOTANOC ligand was prepared in-house according to the established EANM guideline on current good radiopharmacy practice (cGRPP) (Aerts et al. 2014; Gillings et al. 2022). Gallium-68was obtained from a Germanium-68/Gallium-68Generator (Galli Ad, IRE, Fleurus, Belgium). Quality control was successfully carried out according to the European Pharmacopeia. All prepared products were apyrogenic and sterile with a radiochemical purity > 91%.
All PET/CT examinations were performed on three dedicated PET/CT systems in 3D mode (Discovery MI, GE Healthcare, Milwaukee, WI, U.S.A.; Discovery ST, GE Healthcare, Milwaukee, WI, U.S.A.; and Biograph mCT, Siemens, Erlangen, Germany); patients were unsystematically referred to each scanner. Target dose was 2 MBq kg body weight range 80–200 MBq according to established EANM dose recommendations (Jacobs et al. 2005).
Images of the skull were acquired over 10 min scan time 60 min after i.v. injection while additional images of the body-stem from skull base to mid-thighs were acquired in selected cases due to suspicion of 68Ga-DOTANOC avid extracranial malignancy by discontinuously craniocaudal bed movement and an acquisition time of 2 min per bed position afterwards regardless of BMI values. Transmission CT scans for attenuation correction were acquired using helical mode without the use of a contrast agent. Both PET and CT scans were reconstructed with a slice thickness of 3.75 mm. All studies were interpreted by two experienced Nuclear Medicine physicians in consensus reading.
68Ga-DOTANOC positive tumor lesions were visually identified as focal uptake significantly higher than adjacent background activity, not associated with physiological uptake in the pituitary gland as recommend by the generally accepted international EANM/SNMMI criteria (Bozkurt et al. 2017). Volumes of interest (VOI) to acquire SUVmax, SUVmean and MTV were manually drawn over pathological uptake in the tumor, avoiding the very high physiological activity in the pituitary gland. VOIs were also drawn to acquire SUVmax values in the pituitary gland (SUVpit) and superior sinus sagittalis (SUVsss) to obtain raw data for calculating the SUVmax ratio tumor/pituitary gland (SUVRpit) and SUVmax ratio tumor/superior sinus sagittalis (SUVRsss).
Image analysis and semi-quantitative data for both primary tumor and metastasis were acquired on the manufacturer supplied workstation (AW Server 3.2 Ext. 4.0, GE Healthcare, Milwaukee, WI, U.S.A.) using the manufacturer provided auto-snake tool with automatic threshold definition pre-set to 42% of SUVmax. The Kruskal–Wallis-test was used to compare SUVmax, SUVmean, SUVRpit, SUVRsss, and MTV between WHO grades in meningioma. Statistical examination was performed with IBM™ SPSS™ Statistics version 29.0 (Chicago, Ill, U.S.A.).
Results
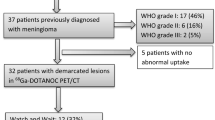
From January 2018 to February 2023, 1309 68Ga-DOTANOC PET/CT examinations were performed at our division. The absolute and relative number of examinations increased over time. In 32/1309 selected cases (2.44%, 26 female) intracranial meningioma was already known or highly suspected. (See Table 1 for patient characteristics and demographics).
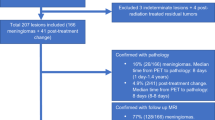
Previous treatment was performed in 30 patients (81.1%), including neurosurgery and /or radiation therapy, while histologically proven meningioma was available in 25 patients (67.6%). Regarding the WHO histological classification WHO grade I was present in 17 cases (45.9%), WHO grade II in 6 cases (16.2%) and WHO grade III in only 2 cases (5.4%). In 12 cases (32.4%) stable disease was present, in 15 cases (40.5%) proton beam radiation therapy was chosen, in three cases (8.1%) neurosurgery was preferred, while in two cases (5.4%) palliative care was chosen due to multiple recurrent intracranial lesions. All depicted meningiomas showed a significant 68Ga-DOTANOC uptake with a median SUVmax value of 17.3 (range: 6.12–64.78) a median SUVmean of 8.4 (range: 1.78–24.06) and a median MTV of 4.89cm3 (range: 0.16–76.4 cm3) (See Fig. 1 for graphic display).
Significant 68Ga-DOTANOC uptake with a good contrast to the surrounding tissue and a sharply demarcated tumor border was present in all meningiomas, confirming the value of 68Ga-DOTANOC PET/CT in the diagnosis of meningioma. No significant differences between visual appearance of tumor volume and extension and semi-automated acquisition of MTV were observed (See Figs. 2, 3, and 4 for a representative case). In protocols with additional scans from skull base to mid-thighs no pathological extracranial uptake was present.
68Ga-DOTANOC PET/CT showing meningioma of the left olfactory nerve with intra- and extracranial tumor masses. Patient was a 64-year-old male neurosurgical treated before PET/CT. Stable disease and WHO grade II allowed a “watch and wait” strategy. Arrow: Physiological tracer uptake in the pituitary gland a PET images, b fused images in three planes
68Ga-DOTANOC PET/CT showing meningioma of the right alisphenoidal and petrous bone in a 47-year-old female patient with resected WHO grade I meningioma (arrow). Due to the large tumor masses extended radiation therapy was scheduled. a PET images, b fused images in three planes, c transversal T2 MRI image, d transversal contrast-enhanced T1 MRI image
WHO grade III meningioma in a 74-year-old female patient with multiple operations. Arrow shows two meningioma next to the post-surgical bone defect. Maximum intensity projection (MIP) mode in panel c and d shows multiple meningeal lesions. Due to the widespread disease and the elevated age of the patient palliative care was chosen. a transversal PET image, b transversal fused PET/CT image, c anterior view of MIP mode, d right lateral view of MIP mode, e transversal MRI T2 image, f transversal contrast-enhanced MRI T1 image
Analysis of semi-quantitative parameters, the main objective of this study, showed an increase of median SUVmax in the tumor associated with WHO grade while no association was present for median MTV (15.84 in WHO grade I, 17.22 in WHO grade II, and 28.4 in WHO grade III and 5.26, 3.23, 18.59, respectively), however no significance could be demonstrated (p = 0.134 for SUVmax and p = 0.216 for MTV). No statistical significance was present between 68Ga-DOTANOC uptake using SUVmean values in the tumor and WHO grade (p = 0.180), and for calculated tumor to superior sinus sagittalis ratio (median 6.24, 4.34, and 16.47; p = 0.067, while the tumor to pituitary gland ratio did not differ (0.98, 1.10, 0.95; p = 0.405) (See Table 2).
Discussion
Diagnosis and determination of topographic extension of intracranial tumors is based on neuroimaging consisting mainly MRI and seldom cranial CT with or without contrast agent. However, these radiological modalities have limitations, especially when posttherapeutic changes are present (Galldiks et al. 2017). 68Ga-DOTANOC PET/CT has the potential to present a meaningful alternative if previous MRI findings are unclear as proven in a recently published systematic review (Filippi et al. 2022). Meningioma unlike other intracranial tumors has a high incidence of somatostatin receptors posing a potential target for both diagnosis and therapy (Dutour et al. 1998). Furthermore, a retrospective study by Milosevic et al. (Milosevic et al. 2023) showed no diagnostic improvement for detection and differentiation of meningioma using PET/MRI and a dedicated MRI protocol.
Before discussing the results concerning the meningiomas it is noteworthy that a higher variability between the physiological tracer uptakes in the pituitary gland with a SUVpit (SUVmax values) ranging from minimum 5.57 to maximum 52.52 (median 18.19) than in the superior sinus sagittalis with a SUVsss (SUVmax values) ranging from minimum 0.94 to maximum 4.69 (median 2.37) was found. This finding is consistent to findings reported by Campos Neto et al. (2022) reporting a range from 12.75 to 32.03.
A similar approach to this topic was performed by Kim et al. (2022) evaluating semi-quantitative parameters in 68Ga-DOTATATE PET/MRI in 166 meningiomas. Interestingly, in this study the SUVmax values showed the highest sensitivity, while the SUVRsss values showed the highest specificity. The lack of reproducibility in our study may be caused by the smaller and possibly more heterogeneous patient collective.
Current guidelines including the 2017 EANM guideline for PET/CT imaging of neuroendocrine neoplasms (Bozkurt et al. 2017) mention the usability of radiolabeled somatostatin analogues for the diagnosis of meningioma without going into detail or describing the value of semi-quantitative parameters. No further amendments concerning this topic were made in a 2023 preprint SNMMI procedure standard/EANM practice guideline for SSTR receptor PET (https://www.eanm.org/publications/guidelines/oncology/). A different and more concise approach is stated in the current EANO guideline (Goldbrunner et al. 2021) on meningioma were the value of somatostatin receptor PET for distinguishing tumor from healthy tissue and postoperative tissue changes is mentioned, however PET/CT is still not seen as standard practice due to the limited availability. Despite the recent advances in hybrid imaging and the widespread use of CT for attenuation correction there are still pitfalls and limitation due to patient movement during the examination. Radiation exposure poses an additional limiting factor especially in children (Salmon et al. 2015).
The manufacturer supplied automatic set threshold of 42% of SUVmax proved adequate for tumor volume determination and MTV which is contradictory to the findings described by Kriwanek et al. (Kriwanek et al. 2022) examining the inter-observer variability of target delineation of meningioma were a threshold of 14% of SUVmax was deemed adequate. In the same study, a general increase in delineated tumor volume was present for most physicians, although a major drop was seen in one physician.
This small retrospective study has several limitations: First, the number of patients is limited, so a larger patient collective could produce more stable results. Secondly, a prospective setting comparing the same patient collective, and outcome would produce more valid data, however this would be more time consuming especially regarding the individual patient outcome.
Conclusion
68Ga-DOTANOC PET/CT plays a key-role in the diagnosis and determination of the topographic extension in intracranial meningioma. Significant 68Ga-DOTANOC uptake with a good contrast to the surrounding tissue and a sharply demarcated tumor border was present in all meningiomas. Increased SUVmax and MTV values in the tumor in 68Ga-DOTANOC PET/CT are associated with higher WHO grade. No correlation was present for calculated tumor to pituitary gland and tumor to superior sinus sagittalis ratios, although the ratio for SUVmax tumor to superior sinus sagittalis had the lowest value of p = 0.067. Nevertheless, further studies including larger patient collectives are needed to solidify this hypothesis.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Aerts J, Ballinger JR, Behe M et al (2014) Guidance on current good radiopharmacy practice for the small-scale preparation of radiopharmaceuticals using automated modules: a European perspective. J Label Comp Radiopharm 57:615–620
Bozkurt MF, Virgolini I, Balogova S et al (2017) Guideline for PET/CT imaging of neuroendocrine neoplasms with 68Ga-DOTA-conjugated somatostatin receptor targeting peptides and 18F–DOPA. Eur J Nucl Med Mol Imaging 44:1588–1601
Campos Neto GC, Amaro Junior E, Weltman E et al (2022) Comparative analysis of somatostatin analog uptake between successfully irradiated and non-irradiated meningiomas. Einstein (sao Paulo) 20:0104
Dutour A, Kumar U, Panetta R et al (1998) Expression of somatostatin receptor subtypes in human brain tumors. Int J Cancer 76:620–627
Filippi L, Palumbo I, Bagni O et al (2022) Somatostatin receptor targeted PET-imaging for diagnosis, radiotherapy planning and theranostics of meningiomas: a systematic review of the literature. Diagnostics 12:1666
Galldiks N, Albert NL, Sommerauer M et al (2017) PET imaging in patients with meningioma-report of the RANO/PET group. Neuro Oncol 19:1576–1587
Gillings N, Hjelstuen O, Behe M et al (2022) EANM guideline on quality risk management for radiopharmaceuticals. Eur J Nucl Med Mol Imaging 49:3353–3364
Goldbrunner R, Stavrinou P, Jenkinson MD et al (2021) EANO guideline on the diagnosis and management of meningiomas. Neuro Oncol 23:1821–1834
Jacobs F, Thierens H, Piepsz A et al (2005) Optimised tracer-dependent dosage cards to obtain weight-independent effective doses. Eur J Nucl Med Mol Imaging 32:581–588
Kim SH, Roytman M, Madera G et al (2022) Evaluating diagnostic accuracy and determining optimal diagnostic thresholds of different approaches to [68Ga]-DOTATATE PET/MRI analysis in patients with meningioma. Sci Rep Nat Res 12:9256
Kriwanek F, Ulbrich L, Lechner W et al (2022) Impact of SSTR PET on inter-observer variability of target delineation of meningioma and the possibility of using threshold-based segmentations in radiation oncology. Cancers (basel) 14:4435
Maggio I, Franceschi E, Tosoni A et al (2021) Meningioma: not always a benign tumor. A review of advances in the treatment of meningiomas. CNS Oncol 10(2):CNS72
Marosi C, Hassler M, Roessler K et al (2008) Meningioma. Crit Rev Oncol Hematol 67:153–171
Milosevic A, Styczen H, Grueneisen J et al (2023) Evaluation of [68Ga]-DOTATOC PET/MRI in patients with meningioma of the subcranial and intraorbital space. J Nucl Med 64:1185–1190
Pirisino R, Filippi L, D’Agostini A et al (2022) Management of a patient with metastatic gastrointestinal neuroendocrine tumor and meningioma submitted to peptide receptor radionuclide therapy with 177 Lu-DOTATATE. Clin Nucl Med 47:E692–E695
Salmon E, Bernard Ir C, Hustinx R (2015) Pitfalls and Limitations of PET/CT in Brain Imaging. Semin Nuclear Med 45:541–551
Vernooij MW, Arfan Ikram M, Tanghe HL, et al (2007) Incidental findings on brain MRI in the general population from the departments of epidemiology abstract. N Engl J Med. Available from: www.nejm.org
Funding
This paper has received no funds, grants, or other support from any funding source.
Author information
Authors and Affiliations
Contributions
All contributing authors have contributed equivocally to the paper, read the paper, approved the contents and meet the criteria for authorship as established. The authors believe that the article represents honest work, and can verify the validity of the results reported.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee (Ethikkommission der Medizinischen Universität Graz—Ethics Committee at Medical University of Graz (Application Number: 35–317 ex 22/23, approval date: July 7th, 2023)). Being a retrospective study the need for written informed consent was waived by the Ethics Committee at Medical University of Graz.
Consent for publication
All contributing authors have contributed equivocally to the paper, read the paper, approved the contents and meet the criteria for authorship as established.
Competing interests
All the authors confirm that there is no conflict of interest—financial or otherwise—to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weitzer, F., Stanzel, S., Plhak, E. et al. Clinical value of semi-quantitative parameters in 68Ga-DOTANOC PET/CT in treatment and diagnostics of cranial meningioma in a single-center retrospective analysis. EJNMMI Rep. 8, 13 (2024). https://doi.org/10.1186/s41824-024-00204-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41824-024-00204-w