Abstract
Background
Early-onset pre-eclampsia with raised blood pressure and protein in the urine before 34 weeks’ gestation is one of the leading causes of maternal deaths in the UK. The benefits to the child from prolonging the pregnancy need to be balanced against the risk of maternal deterioration. Accurate prediction models of risks are needed to plan management.
Methods
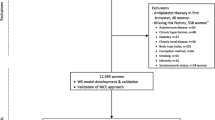
We aim to undertake a multicentre prospective cohort study (Prediction of Risks in Early onset Pre-eclampsia (PREP)) to develop clinical prediction models in women with early-onset pre-eclampsia, for risk of adverse maternal outcomes by 48 h and by discharge. We will externally validate the models in two independent cohorts with 634 and 216 women. In the secondary analyses, we will assess risk of adverse fetal and neonatal outcomes at birth and by discharge.
Discussion
The PREP study will quantify the risk of maternal complications at various time points and provide individualised estimates of overall risk in women with early-onset pre-eclampsia to plan the management.
Trial registration
ISRCTN registry, ISRCTN40384046
Similar content being viewed by others
Background
Pre-eclampsia is a multisystem disorder in pregnancy associated with hypertension and proteinuria [1,2,3] and occurs before 34 weeks in 1% of women, so called early-onset pre-eclampsia [4, 5]. In the UK, hypertensive disease in pregnancy remains a leading cause of direct maternal deaths and contributes to about 20% of all stillbirths [6].
With an increased risk of maternal complications and 20-fold higher maternal mortality, early-onset pre-eclampsia is considered to be pathophysiologically different from the late-onset disease [7,8,9]. The only known cure is delivery of the baby and placenta. However, fetal and neonatal benefits from delaying the pregnancy need to be balanced against the risk of multisystem dysfunction in the mother.
Although the proportion of women with early-onset pre-eclampsia is only 1% of all pregnancies, the complexity of the treatment gives rise to large health care costs [4, 5]. Women are often admitted to tertiary care, and with a third experiencing complications, a stay in an intensive care facility may become necessary [10]. Infants also have longer stays in intensive care facilities for management of complications such as lifelong handicaps arising as a result of prematurity.
One of the key recommendations in the last CEMACH (Confidential Enquiries into Maternal and Child Health) (now known as Centre for Maternal and Child Enquiries (CMACE)) report is the need to adopt an early warning system to help in the timely recognition, referral and treatment of women who have or are developing critical conditions [6]. Early identification of mothers with early-onset pre-eclampsia at risk of complications, and their risks for these at various time points after diagnosis, will allow clinicians to make decisions on commencing interventions such as administration of steroids and, if needed, in utero transfer to a tertiary unit. In mothers considered to be of low risk, they can be monitored as an outpatient, and delivery may be delayed to lower the risk of perinatal complications from prematurity.
We aim to develop prediction models to quantify the overall risk of adverse maternal outcomes in women with early-onset pre-eclampsia and at various time points after diagnosis.
Methods/design
The Prediction of Risks in Early onset Pre-eclampsia (PREP) study will be developed using existing recommendations on prognostic research model development and validation [11,12,13] and reported in line with the Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD) statement [14]. Ethical approval for the study was received from the NRES Committee West Midlands (approval number 11/WM/0248), and the study was registered on ISRCTN registry as per the requirements set out by the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) and the International Committee of Medical Journal Editors (ICMJE) [15] guidelines with registration number ISRCTN40384046 [16].
Objectives
The primary objectives are to develop and internally validate a prediction model in women admitted with early-onset pre-eclampsia from 20 weeks and 0 day to 33 weeks and 6 days of gestation, for assessment of the risk of adverse maternal outcomes at 48 h and by discharge. The 48 h of time interval was chosen to reflect the time recommended for delivery after administration of steroids to lower risks of respiratory distress in newborns. This time period is also considered to be the optimal duration to make decisions on timing and place of delivery and consider in utero transfer to a tertiary care unit if needed. The model will be externally validated in two independent datasets of patients with a diagnosis of early-onset pre-eclampsia. Our secondary objective is to assess the risk of adverse fetal and neonatal outcomes at birth and at any time until discharge.
Study design and conduct
PREP is a prospective, multicentre, observational cohort study involving secondary and tertiary care obstetric units in England and Wales. All consecutive women with a suspected or confirmed diagnosis of pre-eclampsia before 34 weeks of gestation will be approached to take part in the study by research midwives and clinicians in antenatal clinics, wards, day assessment units and delivery suites. Clinicians managing the women will be requested to complete the Clinicians Management Plan at baseline to assess the reasons for planned management. The predictors evaluated in the PREP prediction model are routinely performed as part of standard clinical practice in women admitted with early-onset pre-eclampsia. The PREP study does not influence the management of these patients.
Inclusion criteria
Women aged 16 years or over and a diagnosis of new-onset or superimposed pre-eclampsia at gestational age between 20 + 0 and 33 + 6 weeks will be considered for inclusion in the study. Women with a diagnosis of HELLP (haemolysis, elevated liver enzymes, low platelets) syndrome and those with one episode of eclamptic seizures without hypertension or proteinuria will be considered for inclusion. All women will be required to provide written informed consent and must be capable of understanding the information provided. The definitions for the diagnosis of pre-eclampsia are provided in Table 1.
Exclusion criteria
Women will be excluded if any of the outcomes (including recurrent eclamptic seizures) occurs prior to testing or if informed consent could not be obtained on time or if the mother does not have a good understanding of spoken and written English and a translator is unavailable.
Candidate variables for inclusion in the model
Candidate predictor variables will be obtained from patient demographic characteristics and from clinical assessment including clinical history, examination and investigations. The predictors will be clearly defined and standardised to ensure reproducibility and enhance generalisability and application of study results to practice. Data will also be collected on any interventions applied between recruitment and outcome onset that may modify the outcome.
We will choose the candidate predictors a priori to be considered in the prediction model, based on the most promising predictor variables as identified with our previous systematic review [17,18,19,20,21,22]. The full list of variables to be evaluated for prediction of maternal and fetal outcomes is provided in Table 2.
Outcome measures
The primary outcome is a composite adverse maternal outcome including maternal neurological, haematological, cardiorespiratory, hepatic and renal complications and death. We prioritised the outcomes for clinical importance using a Delphi survey of researchers and clinicians. Prior to the analysis, after discussion with the independent Study Steering (SSC) and Data Monitoring (DMC) Committees, we included delivery before 34 weeks as a component of maternal composite outcome to minimise bias due to treatment paradox [23]. The secondary outcome is a composite adverse fetal outcome (Table 3).
Sample size considerations
From our systematic reviews [17], 20% of women with early-onset pre-eclampsia are expected to have adverse maternal outcomes at any time before discharge. Rules of thumb for fitting multivariate models suggest about 10 events for every variable are required to reduce issues with overfitting, and we will work within this constraint [24,25,26]. We initially planned to examine 10 predictor variables and hence planned to recruit 500 women. However, the event rate was lower than predicted, so we revised our plan to recruit sufficient women to obtain 100 events. Subsequent to the inclusion of delivery before 34 weeks as a component of the composite outcome, we revised our plan to include 22 candidate predictor variables, which was approved by the independent study Committees.
Statistical analysis
We will develop two prediction models: a survival model for adverse maternal outcomes at various time points from diagnosis up to 34 weeks of gestation, including by 48 h after admission, and a logistic model for adverse maternal outcomes by discharge. These will both be developed using a general methodological and statistical framework as outlined below.
Model development, apparent performance assessment and internal validation
The predictors of adverse maternal outcomes will be identified to develop and externally validate a simple, interpretable and clinically applicable prediction model with face validity. We will use a transparent process that implements appropriate statistical methods and adheres to current methodological recommendations.
A backwards selection procedure will be used to decide which of the candidate predictor variables should be included in the final prediction model (with p < 0.15 taken conservatively to warrant inclusion). Continuous variables will be kept as continuous in the model (rather than dichotomising), to avoid a loss of power [27, 28]. Non-linear trends will also be considered using the multivariable fractional polynomial procedure [29, 30], which uses multivariable models to eliminate weaker predictors and identify transformations of continuous predictors that best predict outcome. Large amounts of missing variable data are not expected, but some will inevitably occur, with not all patients providing all variables of interest. Multiple imputation will be used to impute, with 5 imputations, under a missing at random assumption, missing values so as to avoid excluding patients from the analysis [27].
For survival analysis, failure event is defined as an adverse outcome or delivery occurring before 34 weeks of gestation. We will use a flexible parametric survival model via the Royston-Parmar approach [31,32,33], with the cumulative baseline hazard scale modelled using restricted cubic splines. The number of knots will be chosen by visual inspection. For the binary adverse maternal outcome by discharge, a logistic regression-modelling framework will be undertaken with the logit probability of an adverse outcome being the response variable.
We will assess the apparent performance of the fitted models for discrimination using the C-statistic (Harrell’s C-statistic from the survival model and AUC from the logistic model), with 95% confidence interval, averaging across the same imputed datasets that were used to generate the model. A C-statistic close to 1 indicates excellent discrimination and 0.5 indicates no discrimination beyond chance. The calibration performance of the model (fit of observed to expected risk across all individuals) will be assessed by checking whether the calibration slope is 1. As the model will be developed in the same data, perfect agreement is expected on average across the imputed datasets.
Non-parametric bootstrapping will be used to internally validate and examine the potential for overfitting of our developed models, by repeating the variable selection procedure in 100 bootstrap datasets from each of the 5 multiple imputation datasets, providing a total of 500 datasets. This leads to a new final model being produced in each of the bootstrap samples. We will average the difference in the performance of the models to obtain a single estimate of optimism for the C-statistic and the calibration slope. The optimism-adjusted performance statistics will be obtained by subtracting the above estimate of optimism from the original apparent performance statistics. The optimism-adjusted calibration slope will be taken as the uniform shrinkage, and the final models will be corrected by this shrinkage factor.
External validation
We will externally validate (as far as possible) the models in patients admitted with a diagnosis of early-onset pre-eclampsia in two prospective datasets: The Pre-eclampsia Eclampsia TRial Amsterdam (PETRA), Netherlands, and Pre-eclampsia Integrated Estimate of RiSk for mothers (PIERS), Canada. We will compare the predicted number of events from our model with the observed events in the external datasets to assess calibration for the logistic model and compare the predicted with the observed survival function for the survival model (as described above). We will also calculate the C-statistic curve to assess discriminatory ability.
The models we develop (which use data from women diagnosed with pre-eclampsia) will also be tested in women defined with suspected pre-eclampsia (urine dipstick 1+ on admission but normal 24-h proteinuria, <300 mg/24 h and normal PCR <30 mg/mmol). Such women will have been identified from our recruitment process, and by checking the calibration and discrimination of our models for such patients, we can examine the potential generalisability to a broader set of women.
Discussion
Pre-eclampsia and its complications are still considered to be one of the leading causes of maternal and fetal morbidity and mortality; the condition utilises a large proportion of NHS resources. Accurate prediction and early management can significantly improve these outcomes. However, clinicians and policymakers currently do not have the evidence on which they can base their recommendations.
Timely prediction of complications in women with early-onset pre-eclampsia involves the use of a combination of maternal characteristics, symptoms, physical signs and investigations [21]. These ‘tests’ are to some extent haphazardly performed in all units, due to the absence of a structured approach. The most important determinant of perinatal outcome is gestational age, with more than half the chance of intact fetal survival when this is more than 27 weeks and the birth weight is more than 600 g [34].
A recent Cochrane review [10] has shown that expectant management reduced risk of fetal and neonatal complications without increase in maternal complications. Clinicians are reluctant to promote expectant management due to uncertainties around the scale of maternal risk. One of the main reasons for this lack of confidence in applying risk scores in practice is the absence of sufficient evidence to show the reproducibility and transportability of the model in a different population [11]. A good performing prediction model is one that is accurate, validated in populations and datasets external to those used to develop the model, widely applicable in practice, and acceptable to patients and ultimately improves clinical outcomes by helping clinicians and patients make more informed decisions. With very small numbers of cases and events per variable, early-onset pre-eclampsia contributed little to current published models [8, 35, 36].
It is currently difficult to identify those mothers with early-onset pre-eclampsia who are at increased risk of developing complications, and this risk cannot be graded. There is a need for a prognostic model to include the predictive role of more than one test results on the outcome with individualised risk assessment. Provision of individualised risk estimates for adverse maternal outcomes through the PREP study will help clinicians make suitable decisions after discussion with the parents.
Ideally, to develop a prediction model, we would like to observe outcomes in a cohort of women who receive no clinical management at all to be able to predict the likelihood of an adverse outcome independent of clinical management. Clearly, this is unethical and all women who present with pre-eclampsia receive clinical management, but such clinical decisions also affect maternal outcomes. Thus, in the development of our prediction model, we must recognise the importance of accounting for current clinical management; however, this is currently an under-researched methodological issue. By including effective treatment measures such as use of anti-hypertensives and magnesium sulphate predictor variables, and delivery before 34 weeks as a component of the composite outcome, we plan to negate some of the bias arising from treatment paradox in prediction models [23].
There is no obvious single outcome measurement that determines clinical management in early-onset pre-eclampsia. As the risk of more than one outcome needs evaluation simultaneously, we have chosen a composite measure consisting of several complications [37]. The composite outcomes are constructed by including those components whose underlying biology is similar [38].
To show that the PREP prognostic model is valuable, it is not sufficient to show that it successfully predicts outcome in the initial development data even after having it being internally validated. We need evidence that the model performs well for other (external) patients. The resulting geographical and domain validation will enable us to assess the prognostic performance and the generalisability of the model.
Our prediction model plans to use rigorous statistical methods to develop the model and assess accuracy; undertake a formal validation in external datasets (PIERS and PETRA); use unambiguous definitions of predictors and reproducible measurements using methods available in clinical practice; adjust for current clinical management; obtain input from patient focus groups and produce personalised estimates of risk, which enable patients and clinicians to make more informed decisions on management aspects like continuing the pregnancy or delivery of a preterm baby.
Abbreviations
- AUC:
-
Area under the curve (C-statistic)
- BP:
-
Blood pressure
- CEMACH:
-
Confidential Enquiries into Maternal and Child Health
- CMACE:
-
Centre for Maternal and Child Enquiries
- CTG:
-
Cardiotocography
- HELLP:
-
Haemolysis, elevated liver enzymes, low platelets
- PCR:
-
Protein-creatinine ratio
- PETRA:
-
The Pre-eclampsia Eclampsia TRial Amsterdam
- PIERS:
-
Pre-eclampsia Integrated Estimate of RiSk for mothers
- PREP:
-
Prediction of Risks in Early onset Pre-eclampsia
- RIND:
-
Reversible ischemic neurological deficit
References
Brown MA, Hague WM, Higgins J, et al. The detection, investigation and management of hypertension in pregnancy: executive summary. Aust N Z J Obstet Gynaecol. 2000;40(2):133–8.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Report of the National High Blood Pressure Education Program Working Group on high blood pressure in pregnancy. Am J Obstet Gynecol. 2000;183(1):s1–s22.
Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Obstet Gynecol. 2003;102(1):181–92.
Murphy DJ, Stirrat GM. Mortality and morbidity associated with early-onset preeclampsia. Hypertens Pregnancy. 2000;19(2):221–31.
Sibai BM, Ramadan MK, Usta I, Salama M, Mercer BM, Friedman SA. Maternal morbidity and mortality in 442 pregnancies with hemolysis, elevated liver enzymes, and low platelets (HELLP syndrome). Am J Obstet Gynecol. 1993;169(4):1000–6.
Lewis, G (ed) 2007. The Confi dential Enquiry into Maternal and Child Health (CEMACH). Saving Mothers’ Lives: reviewing maternal deaths to make motherhood safer - 2003-2005. The Seventh Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. London: CEMACH.
MacKay AP, Berg CJ, Atrash HK. Pregnancy-related mortality from preeclampsia and eclampsia. Obstet Gynecol. 2001;97(4):533–8.
von Dadelszen P, Menzies JM, Payne B, Magee LA, Group PS. Predicting adverse outcomes in women with severe pre-eclampsia. Semin Perinatol. 2009;33(3):152–7.
von Dadelszen P, Magee LA, Roberts JM. Subclassification of preeclampsia. Hypertens Pregnancy. 2003;22(2):143–8.
Churchill D, Duley L. Interventionist versus expectant care for severe pre-eclampsia before term. Cochrane Database Syst Rev. 2002;3:CD003106.
Altman DG, Vergouwe Y, Royston P, Moons KG. Prognosis and prognostic research: validating a prognostic model. BMJ. 2009;338:b605.
Moons KG, Royston P, Vergouwe Y, Grobbee DE, Altman DG. Prognosis and prognostic research: what, why, and how? BMJ. 2009;338:b375.
Royston P, Moons KG, Altman DG, Vergouwe Y. Prognosis and prognostic research: developing a prognostic model. BMJ. 2009;338:b604.
Moons KG, Altman DG, Reitsma JB, et al. Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med. 2015;162(1):W1–W73.
Why is trial registration important? World Health Organization - International Clinical Trials Registry Platform (ICTRP). http://www.who.int/ictrp/trial_reg/en/. Accessed 7 Feb 2015.
Khalid K. Prediction of Risks in Early onset Pre-eclampsia (PREP). ISRCTN40384046. ISRCTN registry. 2011. http://www.isrctn.com/ISRCTN40384046. Accessed 10 May 2015.
Thangaratinam S, Coomarasamy A, O’Mahony F, et al. Estimation of proteinuria as a predictor of complications of pre-eclampsia: a systematic review. BMC Med. 2009;7:10.
Thangaratinam S, Coomarasamy A, Sharp S, et al. Tests for predicting complications of pre-eclampsia: a protocol for systematic reviews. BMC Pregnancy Childbirth. 2008;8:38.
Thangaratinam S, Datta A, Ismail KMK, Khan KS. What is the accuracy of blood pressure in predicting complications in pre-eclampsia? Archives of Disease in Childhood - Fetal and Neonatal Edition. 2011;96(Supplement 1):Fa101-Fa.
Thangaratinam S, Gallos ID, Meah N, et al. How accurate are maternal symptoms in predicting impending complications in women with preeclampsia? A systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2011;90(6):564–73.
Thangaratinam S, Ismail K, Sharp S, et al. Prioritisation of tests for the prediction of preeclampsia complications: a Delphi survey. Hypertens Pregnancy. 2007;26(1):131–8.
Thangaratinam S, Ismail KM, Sharp S, Coomarasamy A, Khan KS, Tests in Prediction of Pre-eclampsia Severity review group. Accuracy of serum uric acid in predicting complications of pre-eclampsia: a systematic review. BJOG. 2006;113(4):369–78.
Cheong-See F, Allotey J, Marlin N, et al. Prediction models in obstetrics: understanding the treatment paradox and potential solutions to the threat it poses. BJOG. 2016.
Peduzzi P, Concato J, Feinstein AR, Holford TR. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol. 1995;48(12):1503–10.
Vergouwe Y, Steyerberg EW, Eijkemans MJ, Habbema JD. Substantial effective sample sizes were required for external validation studies of predictive logistic regression models. J Clin Epidemiol. 2005;58(5):475–83.
Westerhuis ME, Schuit E, Kwee A, et al. Prediction of neonatal metabolic acidosis in women with a singleton term pregnancy in cephalic presentation. Am J Perinatol. 2012;29(3):167–74.
Little RJA, Rubin DB. Statistical analysis with missing data. 2nd ed. New York: John Wiley; 2002.
Royston P, Sauerbrei W. Building multivariable regression models with continuous covariates in clinical epidemiology—with an emphasis on fractional polynomials. Method Inform Med. 2005;44(4):561–71.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55.
Sauerbrei W, Royston P. Building multivariable prognostic and diagnostic models: transformation of the predictors by using fractional polynomials. J R Stat Soc A Stat Soc. 1999;162(1):71–94.
Lambert PC, Royston P. Further development of flexible parametric models for survival analysis. Stata J. 2009;9(2):265–90.
Royston P, Lambert PC. Flexible parametric survival analysis using Stata: beyond the Cox model. Texas: Stata Press; 2011.
Royston P, Parmar MK. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat Med. 2002;21(15):2175–97.
von Dadelszen P, Magee LA, Lee SK, et al. Activated protein C in normal human pregnancy and pregnancies complicated by severe preeclampsia: a therapeutic opportunity? Crit Care Med. 2002;30(8):1883–92.
Ganzevoort W, Rep A, Bonsel GJ, De Vries JI, Wolf H, PETRA investigators. A randomized trial of plasma volume expansion in hypertensive disorders of pregnancy: influence on the pulsatility indices of the fetal umbilical artery and middle cerebral artery. Am J Obstet Gynecol. 2005;192(1):233–9.
von Dadelszen P, Payne B, Li J, Ansermino JM, Broughton-Pipkin F, Cote AM, Douglas MJ, Gruslin A, Hutcheon JA, Joseph KS, Kyle PM, Lee T, Loughna P, Menzies JM, Merialdi M, Millman AL, Moore MP, Moutquin JM, Ouellet AB, Smith GN, Walker JJ, Walley KR, Walters BN, Widmer M, Lee SK, Russell JA, Magee LA, PIERS Study Group. Prediction of adverse maternal outcomes in pre-eclampsia: development and validation of the fullPIERS model. Lancet. 2011;377(9761):219–27.
International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH harmonised tripartite guideline: statistical principles for clinical trials. Stat Med. 1999;18:1905–42.
Montori VM, Permanyer-Miralda G, Ferreira-Gonzalez I, et al. Validity of composite end points in clinical trials. BMJ. 2005;330(7491):594–6.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. The Lancet. 1974;304(7872):81–4.
Acknowledgements
We are thankful to all the research teams at the participating hospital for promoting and managing the study within their hospitals. We are also thankful to all the women who have agreed to participate in the study (and those yet to participate), without whom this study would not be possible.
Funding
This study is supported by the National Institute for Health Research Health Technology Assessment Programme.
Availability of data and materials
At the end of the study, the entire study data will be stored at QMUL data repository as per sponsor guidelines and can be requested by contacting Prof Shakila Thangaratinam.
Authors’ contributions
ST designed and led the project, provided clinical direction and developed the protocol. JA oversees the day-to-day management of the study and assisted in preparing the draft and final version of the protocol. NM will perform the statistical analysis of the study and contributed to the write-up of the analysis plan of the protocol. BWM provides clinical direction and contributed to the write-up of the protocol. PvD is providing the PIERS dataset to be used for validation of the PREP model. JAk is providing the PETRA dataset to be used for validation of the PREP model. WG is providing the PETRA dataset to be used for validation of the PREP model. AA contributed to the protocol and study development. JDn contributed to the write-up of the protocol JDe contributed to the protocol and study development. KI contributed to the protocol and study development. AMB provided lay input and contributed to the write-up of the protocol. JDo oversees the study coordinator, provided input and edited the protocol. SK provides management to the statistician, oversees the statistical analysis and edited the final version of the protocol. CM provides statistical guidance on analysis of data and presentation of the results and contributed to the write-up of the protocol. RDR provides statistical guidance, contributed to the analysis plan for the study and edited the protocol. KSK designed the project, provided clinical and overall direction, contributed to and edited the protocol. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The study received ethical approval from the NRES Committee West Midlands (approval number 11/WM/0248).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Allotey, J., Marlin, N., Mol, B.W. et al. Development and validation of prediction models for risk of adverse outcomes in women with early-onset pre-eclampsia: protocol of the prospective cohort PREP study. diagn progn res 1, 6 (2017). https://doi.org/10.1186/s41512-016-0004-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41512-016-0004-8