Abstract
Background
A mixed pulmonary infection of Mycobacterium bacteremicum and three different isolates of nontuberculous mycobacteria (NTM) is an unusual clinical manifestation and have not yet been indicated. In this case report, we reported four isolates of NTM using phenotypic and genotypic test of pulmonary sample in Tehran, Iran.
Case presentation
We report a case of severe pulmonary disease in a 19-year-old male patient with productive cough, shortness of breath, and low-grade fever for several weeks. The C-reactive protein (CRP) level (80.2 mg/L) and erythrocyte sedimentation rate (ESR) (95 mm/h) were high. The computed tomographic scan indicated bronchiectasis, nodular opacities, consolidation, and cavitary lesions on both sides. The result of purified protein derivative (PPD) test was equal to 15 mm. The sequences of hsp65, rpoB, and 16S rDNA genes indicated more than 99% homology to four isolates of nontuberculous mycobacteria (NTM), including Mycobacterium fortuitum, M. chelonae, M. mucogenicum, and M. bacteremicum. We found that all four strains were susceptible to amikacin, cefoxitin, ciprofloxacin, clarithromycin, imipenem, and linezolid. The patient was treated with ciprofloxacin, clarithromycin, and amikacin, along with Montelukast, for five months.
Conclusion
We report a case of severe pulmonary infection by four isolates of NTM. After treatment, the patient reported complete resolution of the signs and a weight gain of 5 kg; also, the CRP and ESR were normal. Nine months after the infection diagnosis, a new CT scan revealed further improvements.
Similar content being viewed by others
Background
Nontuberculous mycobacteria (NTMs) have been isolated around the world and are being increasingly identified as human pathogens. Lung disease is the most common manifestation of NTM [1]. Overall, rapidly growing mycobacteria (RGM) are a major cause of NTM infections, particularly in Asia. Among RGM, the most common ones include Mycobacterium (M.) abscessus, M. fortuitum group and M. chelonae [2]. Here, we present a case of severe mixed pulmonary infection, caused by four isolates of NTM.
Case presentation
The patient was a 19-year-old male with productive cough, shortness of breath, and low-grade fever for several weeks in Iran. His history showed that he kept many birds at home and also fed a cockatiel mouth-to-mouth for several years. He had shown axillary lymph node involvement when he was 16 years old. After seven months, he complained of joint involvement, and two months later, he presented with shortness of breath, sputum, weight loss (8 kg), chest pain, and night perspiration. Bronchoscopy was carried out, while polymerase chain reaction (PCR), acid-fast staining, and culture for M. tuberculosis were all negative. Treatment with many drugs, including doxycycline, ceftriaxone, cefixime, co-amoxiclav, was initiated at different intervals; however, it was not successful.
Six months later, the patient’s status gradually deteriorated. He presented with shortness of breath with 92% oxygen saturation in ambient air, besides productive cough; the C-reactive protein (CRP) level (80.2 mg/L) and erythrocyte sedimentation rate (ESR) (95 mm/h) were also determined. The result of purified protein derivative (PPD) test was equal to 15 mm.
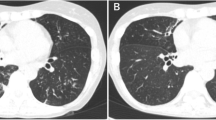
The computed tomographic (CT) scan indicated bronchiectasis, nodular opacities, consolidation, and cavitary lesions on both sides. Newly collected three sputum and three bronchoalveolar lavage samples were sent for further evaluation of the presence of mycobacterial infections. Contrary to previous findings, the results of acid-fast staining and culture on Lowenstein-Jensen medium were positive for all six samples. We observed four different colonies with rapidly growing mycobacteria (one scotochromogen and three nonchromogens) in the Lowenstein-Jensen medium (Fig. 1).
The hsp65, rpoB and full 16S rDNA genes were used for molecular identification, as previously described in the literature [3]. The sequencing results of four isolates of colonies showed more than 99% similarity with M. fortuitum, M. chelonae, M. mucogenicum, and M. bacteremicum.
We then performed drug susceptibility testing (DST), according to the Clinical & Laboratory Standards Institute (CLSI) guidelines [4] for amikacin, levofloxacin, clarithromycin, cefoxitin, ciprofloxacin, doxycycline, linezolid, imipenem, minocycline, trimethoprim sulfamethoxazole, and vancomycin. We found that all four strains were susceptible to amikacin, cefoxitin, ciprofloxacin, clarithromycin, imipenem, and linezolid. Based on the susceptibility data for all four NTM isolates, treatment was initiated with ciprofloxacin, clarithromycin, and amikacin, along with Montelukast, for five months. The patient reported complete resolution of the signs and a weight gain of 5 kg; also, the CRP and ESR were normal. Nine months after the infection diagnosis, a new CT scan revealed further improvements. Also, the culture and smear results for the presence of NTM was negative.
Discussion and conclusion
Generally, mixed NTM infections are correlated with immune suppression, especially in HIV patients. A retrospective study demonstrated mixed infections with other NTM, such as M. abscessus, M. fortuitum, M.chelonae, and M. simiae in 29% of M. avium complex patients [5, 6]. However, to the best of our knowledge, pulmonary infection, caused by four isolates of NTM isolates, has not been previously reported, particularly with M. bacteremicum.
Several studies have suggested that RGM, especially M. fortuitum, M. chelonae, and M. mucogenicum, can cause a variety of diseases, including pulmonary infection [7, 8].
Mycobacterium bacteremicum is a scotochromogenic RGM isolated from 10 young patients, two of whom were immunosuppressed. In three and one cases, the strain grew from the blood and the central catheter, respectively [9, 10]; there was no report of pulmonary infection by this isolate. As its name suggests, M. bacteremicum is mostly recovered from the blood [9].
In the present case report, our patient had close contact with birds. Infection might have been transmitted through birds, especially when the patient fed the birds orally. However, mycobacteria should be taken seriously by birds living near humans, as they can be a potential reservoir of infections by mycobacteria that are resistant to some antibacterial agents [11]. Because of mixed infection with four types of NTM isolates, DST was performed for the best treatment. The patient responded well to the selected regimen, including ciprofloxacin, clarithromycin, and amikacin. Overall, there is no information concerning the treatment of M. bacteremicum, while several reports have shown the successful treatment of M. fortuitum, M. chelonae, and M. mucogenicum with the aforementioned drugs [8, 9]. Considering the complete resolution of symptoms and improvements after appropriate treatment in our patient, this study confirmed the risk of pulmonary infection caused by M. bacteremicum, accompanied by three well-known NTM.
Because different NTM may mimic each other, many cases of mixed NTM infection are likely to be missed or misdiagnosed as a single-organism NTM infection, leading to inappropriate antibiotic prescriptions.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- NTM:
-
Nontuberculous mycobacteria
- RGM:
-
Rapidly-growing mycobacteria
- PCR:
-
Polymerase chain reaction
- CT:
-
Computed tomographic
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- WBC:
-
White blood cells
- AFB:
-
Acid-fast bacillus
- RGM:
-
Rapidly-growing mycobacteria
- DST:
-
Drug susceptibility pattern
- CLSI:
-
Clinical and Laboratory Standards Institute
References
Donohue MJ. Epidemiological risk factors and the geographical distribution of eight Mycobacterium species. BMC Infect Dis. 2021;21:1–11. https://doi.org/10.1186/s12879-021-05925-y.
Tang S, Lye D, Jureen R, et al. Rapidly growing mycobacteria in Singapore, 2006–2011. Clin Microbiol Infect. 2015;21:236–41. https://doi.org/10.1016/j.cmi.2014.10.018.
Davari M, Irandoost M, Sakhaee F, et al. Genetic diversity and prevalence of nontuberculous mycobacteria isolated from clinical samples in Tehran. Iran Microb Drug Resist. 2019;25:264–70. https://doi.org/10.1089/mdr.2018.0150.
Woods GL, Brown-Elliott BA, Conville PS, et al. Susceptibility Testing of Mycobacteria, Nocardiae, and Other Aerobic Actinomycetes [Internet]. 2nd Ed. Wayne (PA): Clinical and Laboratory Standards Institute; 2011. (CLSI publication / Clinical and Laboratory Standards Institute, No. 31.5.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK544374/
Kim JS, Tanaka N, Newell JD, et al. Nontuberculous mycobacterial infection: CT scan findings, genotype, and treatment responsiveness. Chest. 2005;128:3863–9. https://doi.org/10.1378/chest.128.6.3863.
Kurahara Y, Tachibana K, Tsuyuguchi K, Suzuki K. Mixed pulmonary infection with three types of nontuberculous mycobacteria. Intern Med. 2013;52:507–10. https://doi.org/10.2169/internalmedicine.52.8907.
Shrivastava K, Kumar C, Singh A, et al. An overview of pulmonary infections due to rapidly growing mycobacteria in South Asia and impressions from a subtropical region. Int J Mycobacteriol. 2020;9:62–70. https://doi.org/10.4103/ijmy.ijmy_179_19.
Irandoost M, Ghanbari MZ, Sakhaee F, et al. High rates of Mycobacterium fortuitum isolation in respiratory samples from Iranian patients with suspected tuberculosis: is it clinically important? J Med Microbiol. 2018;67:1243–8. https://doi.org/10.1099/jmm.0.000814.
Brown-Elliott BA, Wallace RJ Jr, Petti CA, et al. Mycobacterium neoaurum and Mycobacterium bacteremicum sp. nov. as causes of mycobacteremia. J Clin Microbiol. 2010;48:4377–85. https://doi.org/10.1128/JCM.00853-10.
Tortoli E. Microbiological features and clinical relevance of new species of the genus Mycobacterium. Clin Microbiol Rev. 2014;27:727–52. https://doi.org/10.1128/CMR.00035-14.
Ledwoń A, Napiorkowska A, Augustynowicz-Kopeć E, Szeleszczuk P. Drug susceptibility of non-tuberculous strains of Mycobacterium isolated from birds from Poland. Pol J Microbiol. 2018;67:487–92. https://doi.org/10.21307/pjm-2018-057.
Acknowledgements
We thank the patient for granting us permission to publish this information.
Funding
None.
Author information
Authors and Affiliations
Contributions
FS, ST, MRZ and MM: performed the experiments; FV, FRJ and SDS: analyzed and interpreted data; AF: designed and supervised clinical study, interpreted data, read and approved manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was in compliance with the 1975 Declaration of Helsinki and local regulations. It was also approved by the Ethics Committee of Pasteur Institute of Iran (IR.PII.REC.1394.54). Written informed consent was obtained from the patient.
Consent for publication
Patient’s written informed consent to publish potentially identifying images and clinical details was obtained.
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Masoumi, M., Sakhaee, F., Zolfaghari, M.R. et al. Mixed pulmonary infection with four isolates of nontuberculous mycobacteria: a case report of mycobacterium bacteremicum infection. Pneumonia 14, 7 (2022). https://doi.org/10.1186/s41479-022-00100-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41479-022-00100-6