Abstract
Background
With the rising prevalence of obesity and overweight, increasing number of scholars paid attention to the negative effects on human health and life. Recent years, many studies have focused on the relation of socio-economic factors with the risk of overweight or obesity, but findings have been inconsistent. This study investigated the relationship between socio-economic factors and the risk of overweight and obesity among Chinese adults.
Methods
This study was based on the survey of the China Health and Nutrition Survey in 2015, with 9245 Chinese adults aged 18–65 years old. Overweight and obesity were assessed by physical measurements of weight, height, and waist circumference. Multiple logistic models were used to estimate the odds ratios (ORs) and 95% confidence intervals (CIs) of the association.
Results
Overall, the prevalence rates of general obesity and abdominal obesity were 15.5% and 22.6%, respectively. We found that education and per capita household income were positively associated with overweight and obesity risk in men. However, the association between education and obesity status was negative in women [general obesity: OR = 0.64, 95% CI (0.50–0.81); abdominal obesity: OR = 0.62, 95% CI (0.51–0.76)]. Occupational status was only associated with general overweight in men.
Conclusions
Results suggested that higher education and per capita household income were associated with an increased risk of overweight and obesity among Chinese men, whereas the associations were negative for women. We recommended that men with high levels of education and income, women with low levels of education, can engage in some physical activity, modify dietary, and adopt a new way of life to maintain their weight and general health.
Similar content being viewed by others
Background
Overweight and obesity are defined as abnormal or excessive fat accumulation, which can damage health, and has become a major health burden worldwide [1]. Body mass index (BMI) and waist circumference (WC) can be used to assess the overweight and obesity. A report of the WHO indicated that overweight is one of the top 10 global health risk factors around the world, even among the top 5 global health risk factors in developed countries [2]. Since 1980, mean BMI and the prevalence of overweight and obesity have rapidly increased [3, 4]. One in three people is classified as overweight or obesity among the world population [4]. The number of adults suffering obesity has reached 603.7 million by 2015 worldwide [5]. In China, the prevalence of overweight and obesity showed a trend of increase [6]. According to the prediction of the National Health Commission of China (NHCC), from 2002 to 2015, the prevalence of overweight and obesity in China rose from 7.1% and 22.85% to 11.9% and 30.15%, respectively. Not only is obesity linked to mental health disorder such as attention deficit hyperactivity disorder, but also associated with the risk of chronic diseases such as cardiovascular disease, cancer, and type 2 diabetes [7,8,9,10]. Furthermore, excess weight can lead to musculoskeletal disorders, especially osteoarthritis, a highly disabling degenerative disease of the joints. It leads to a lower quality of life and general health [11]. Concurrently, overweight and obesity may have a considerable impact on healthcare expenditures. A European study found that obesity appeared to account for a significant economic burden in many European countries. Obesity-related healthcare burdens of up to 10.4 billion euros and the economic burdens ranged from 0.09 to 0.61% of each country's gross domestic product (GDP) [12]. By 2030, it is predicted that obesity-related medical expenses in the United States would reach $48 billion to $66 billion annually [13].
Many studies have focused on the relation of socio-economic factors with the risk of overweight or obesity, but findings have been inconsistent [14,15,16,17,18]. Socio-economic factors mainly include income, education, and occupational status, and such factors, which play an important role in the development of overweight and obesity. Fred C and his colleagues concluded that while economic and social development can improve health, it can also increase obesity and expand socioeconomic status disparities in obesity [19]. A large population-based cross-sectional study involving 991,327 women from lower- and middle-income countries found that socio-economic status was positively associated with the risk of overweight and obesity [17]. A cross-sectional multicenter population-based investigation of Russians reported that education was positively associated with the risk of obesity [14]. On the contrary, a German study showed higher education level was associated with a reduced risk of overweight or obesity [16]. Although several previous studies investigated the association of socio-economic factors with overweight and obesity, the inconsistent results still make these associations unclear.
Therefore, in this study, we aimed to evaluate the association between socio-economic factors with the risk of overweight and obesity among 9245 Chinese adults from a large population-based survey. Furthermore, we conducted analyses stratified by gender to explore whether this association could be affected by gender differences. Our study contributed to the development of healthy living guidelines for the Chinese population, as well as providing some theoretical support for the development of relevant public health prevention policies.
Methods
Data source and study population
In this study, we used the data from the China Health and Nutrition Survey (CHNS) in 2015. The CHNS is a population-based cohort study that used a multistage random-cluster sampling process to survey Chinese residents from 15 provinces in China. The selected provinces (autonomous regions) were representative based on the measurement of various factors and the level of social development in China. This survey was designed to evaluate the health and nutritional status of the Chinese population resulting from the social and economic transformation. Thus far, the CHNS has finished 10 rounds of surveys from 1989 to 2015. Details of the investigation have been described elsewhere [20]. All participants signed informed consent forms. The survey was approved by the institutional review committees of the University of North Carolina at Chapel Hill, the National Institute of Nutrition and Food Safety, and the Chinese Center for Disease Control and Prevention.
This study included 10,640 participants aged from 18 to 65 years old. We excluded participants without height and weight measurement, complete information of education level, household income, or occupation (n = 1322). Because measurements of WC in pregnant or lactating women have no objective significance, we also excluded those who were pregnant or lactating (n = 73). Multiple imputation or both imputation were used for missing covariates. Finally, 9245 participants (4375 men and 4870 women) were included in this cross-sectional study.
Assessment of overweight and obesity
In our study, BMI and WC are measured by CHNS, they can be used to assess the overweight and obesity. Physical measurements are made by professionals using uniform equipment. In all surveys, people's height and weight were assessed while wearing loose clothes, and no shoes and hat. Before the measurement, the reel height measurement instrument was adjusted to zero and participants stood with their back against a wall, looking straight ahead and parallel to the floor. The weight was measured by electronic weight scale, which also needed to be calibrated before measurement [21]. BMI is defined as weight (kg) divided by the square of height (m) (kg/m2). WC (in cm) was measured with a tape measure at the mid-point between the lower edge of the rib cage and the iliac crest [22]. Body weight was measured to the nearest 0.1 kg, height to the nearest 0.1 cm, and WC to the nearest 0.1 cm [23]. According to the guidelines of the Working Groups on Obesity in China (WGOC) [24], BMI was divided into four groups: underweight (BMI < 18.5 kg/m2); normal (BMI ≥ 18.5 kg/m2 but < 24 kg/ m2); overweight (BMI ≥ 24.0 kg/ m2 but < 28 kg/ m2); and obesity (BMI ≥ 28 kg/ m2). WC was categorized into three groups: normal (WC < 80 cm for women and WC < 85 cm for men); overweight (WC ≥ 80 cm but < 90 cm for women, WC ≥ 85 cm but < 95 cm for men); obesity (WC ≥ 90 cm for women and WC ≥ 95 cm for men).
Assessment of socio-economic factors
In this study, we collected three socio-economic factors through the questionnaires, namely, education levels, per capita household income, and occupational status. China implemented 9-year compulsory education in 1986, and the age range of the survey population was between 18 and 65 years old. In order to conform to China's national conditions and actual situation, combined with the original questionnaire design, this study divided the education level into the three groups: less than primary school; less than high school; and higher than high school. Per capita household income was calculated by dividing total household income by the number of people in the household [25]. Participants were ranked by their per capita household income from the smallest to the largest, and divided into four quartile spacing groups: < 8000 CNY; ≥ 8000 and < 17,000 CNY; ≥ 17,000 and < 30,800 CNY; ≥ 30,800 CNY. Occupational status was divided into current working or not working.
Assessment of covariates
Covariates included age, gender (female and male), residence (urban, rural), marital status (never married, married, divorced, or widowed), leisure physical activity (LPA), alcohol intake (never, no more than once a month, once or twice a month, once or twice a week, three or four times a week, almost every day), smoking status (never; former; current), hypertension and type 2 diabetes (T2D). LPA was assessed by multiplying the time an individual spent in each activity (6 items of active activities, 7 items of sedentary activities) by metabolic equivalent (MET) score, which is an indicator of the average intensity of each LPA [26]. Hypertension was ascertained if subjects met at least one of the present criteria: (1) a physician diagnosis of hypertension; (2) antihypertensive treatment; (3) systolic BP ≥ 140 mmHg; (4) diastolic BP ≥ 90 mmHg. T2D was defined as meeting at least one of the following criteria [27, 28] (1) FPG ≥ 7.0 mmol/L; (2) HbA1c ≥ 6.5%; (3) a history of T2D diagnosis; (4) taking any diabetic medication or anti-hyperglycaemic treatment.
Statistical analysis
Continuous variables were described as means and standard deviations (SDs), and categorical variables were presented as frequency with percentage. We used chi-square test for categorical variables and ANOVA for continuous variables to test linear trends across BMI groups and WC groups, separately.
Multiple logistic regression models were used to estimate the associations with the risk of overweight and obesity of socio-economic factors. The magnitude of the associations was assessed by odds ratios (ORs) and 95% confidence intervals (CIs). We performed two models to examine the association of the socio-economic factors with the overweight and obesity. Model 1 was adjusted for age and residence (urban, rural). Model 2 was adjusted as for basic model and further adjusted for marital status (never married, married, divorced, or widowed), smoking status (never, former, current), alcohol intake (never, no more than once a month, once or twice a week, three or four times a week, almost every day), LPA (categorical variable), history of hypertension type 2 diabetes. All statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). Statistical significance was defined by two-sided p < 0.05 for all tests.
Results
Characteristics of the participants
Our study included 9245 participants, of which 47.3% (N = 4375) were men, and 52.7% (N = 4870) were women. The basic characteristics of the participants is shown in Table 1. Overall, overweight and obesity defined by WC (35.5% and 22.6%) were more prevalent than those defined by BMI (34.3% and 15.5%). Participants with higher BMI or larger WC were more likely to be older, got lower education and higher per capita household income, did less LPA and had higher blood pressure, and had a history of hypertension and type 2 diabetes. Furthermore, participants with higher BMI were more likely to be male and consume more alcohol. Subjects with larger WC were more likely to live in urban areas and be currently working.
The association between education levels and the risk of overweight and obesity
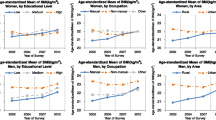
The proportion of overweight and obesity in the different education levels is gradually increasing, and the education level of the largest proportion of people is high school level and above (Fig. 1). The association between the risk of overweight and obesity with education level were significant in men and women. In model 1, we adjust age and residence, and the results showed that higher education level was positively associated with an increased risk of general overweight and obesity in men [overweight: OR (95% CI) 1.33 (1.09–1.64); obesity: OR (95% CI) 1.65 (1.22–2.22)] (Table 2), whereas the associations were negative in women [overweight: OR (95% CI) 0.76 (0.63–0.92); obesity: OR (95% CI) 0.52 (0.40–0.66)] (Table 3). The associations were opposite across genders. In men, the magnitude of the associations weakened after additionally adjusted for health-related factors and history of hypertension and T2D. However, the associations remained stable in women. The relation between education level and abdominal obesity status was also different according to gender. In men, the ORs and 95% CIs of overweight and obesity were respectively 1.20 (0.98–1.47) and 1.42 (1.14–1.76), and 1.36 (1.06–1.74) and 1.77 (1.36–2.29) comparing each group of education level with the lowest level. In women, education level was inversely associated with abdominal obesity [OR (95% CI) 0.62 (0.49–0.79)], whereas no association of education with abdominal overweight risk was observed [OR (95% CI) 0.88 (0.72–1.07].
Percentages of overweight and obesity with different education levels, income groups, occupation status (A: BMI, B: WC). Note: BMI is defined as weight (kg) divided by the square of height (m) (kg/m2), WC (in cm) wasmeasured with a tape measure at the mid-point between the lower edge of the rib cage and the iliac crest
The association between per capita household income and the risk of overweight and obesity
In all samples, those in the ≥ 17,000 and < 30,800 CNY income group had the largest percentage of overweight and obesity (general overweight: 26.2%; general obesity: 26.3%; abdominal overweight: 25.4%; abdominal obesity: 26.7%) (Fig. 1). The association between per capita household income with the risk of overweight and obesity was different for men and women. In men, per capita household income was significantly associated with an increased risk of general overweight and obesity. With additional adjustments in the multivariable model, the association remained significant [overweight: OR (95% CI) 1.49 (1.22–1.82); obesity: OR (95% CI) 1.47 (1.13–1.92)]. In women, no significant associations were found between per capita household income and the risk of general overweight. While the highest income group showed a reduced risk associated with general obesity [OR (95% CI) 0.69 (0.54–0.90)]. In men, a significant linear trend was observed between increased income and abdominal obesity risk (p < 0.001). In women, no significant associations were found between per capita household income and the risk of abdominal overweight or obesity. The highest income group showed approximately 10%, albeit not statistically significant, risk reduction associated with abdominal obesity [OR (95% CI) 0.87 (0.69–1.10)].
The association between occupational status and the risk of overweight and obesity
As to occupational status, people in current working status are more likely to be overweight and obesity (general overweight: 57.2%; general obesity: 55.8%; abdominal overweight: 56.6%; abdominal obesity: 52.9%) (Fig. 1). Results in men showed that there is an association between employed and general/abdominal overweight and obesity. Especially in the basic model, the association between male general overweight and obesity is positive [overweight: OR (95% CI) 1.21 (1.05–1.40); obesity: OR (95% CI) 1.35 (1.11–1.64)]. However, in the multilevel model that adjusts for confounding factors, such association becomes insignificant. Employed men were more likely to be general/abdominal obesity compared to those unemployed [general obesity: OR (95% CI) 1.45 (1.18–1.78); abdominal obesity: OR (95% CI) 1.23 (1.02–1.47)]. In women, occupational status was inversely associated with obesity [general obesity: OR (95% CI) 0.80 (0.67–0.97); abdominal obesity: OR (95% CI) 0.82 (0.69–0.97)], whereas no association of occupational status with the risk of overweight.
Discussion
In this population-based cross-sectional study of Chinese adults, the association between socio-economic factors and the risk of overweight and obesity differed by gender. Education level was positively associated with the risk of overweight and obesity in men, whereas the results were opposite to women. In men, higher per capita household income was significantly associated with an increased risk of general overweight, abdominal overweight and abdominal obesity. In women, per capita household income was associated with a reduced risk of general obesity and abdominal overweight/obesity, albeit not statistically significant. A positive association between occupational status and general obesity was observed in men, while such association was not found in women.
Results showed that higher education level was positively associated with the risk of overweight and obesity in men, whereas inverse associations were observed in women. Education was a well-known factor of obesity development. Thus far, many studies have evaluated the relationship between education and obesity status. However, the findings have been inconsistent. An Indian cross-sectional study found that higher education level was associated with the risk of overweight and obesity in men and women [29], whereas a Chinese study proposed an inverse association between education and weight [30]. Moreover, a representative population-based study on Burmese population did not find a significant association between education level and the risk of overweight or obesity [31]. This study found that the association between education level and obesity status was different from men and women. Several previous studies showed similar results to our findings. In a review including 333 studies on the relation between socio-economic status and obesity, 63% of the studies found that socio-economic status was negatively associated with obesity risk in women whilst only 37% of these studies found such association in men [32]. A study on the Chinese population reported that higher education level was associated with an increased risk of obesity in men, whereas education was found to be associated with a reduced obesity risk in women [33]. However, findings of some studies were opposite to current study [34, 35]. There were several possible reasons to explain the opposite results for men and women. The sociology of Bourdieu and his theory elaborated on sex differences in body size [36]. For women, those with higher education levels are more likely to get a thinner body, which may be socially valued and materially viable to a greater extent. For men, larger body size is likely to be valued as a sign of physical dominance and prowess. In other words, women pay more attention to physical beauty than men do. Compared with men, women with higher education level are more likely to adhere to a healthier diet, characterized by consuming more of a variety of food and thus have higher quality diets [37].
We found higher per capita household income was associated with an increased risk of overweight and obesity in participants. Two previous studies were in line with our results [30, 38]. A study conducted in rural southwest China reported that household income was positively associated with the prevalence of central obesity [30]. Another study in a rural Han Chinese supported the results of the current study [38]. However, a study involving Tianjin residents found that higher income was associated with a reduced risk of overweight and obesity [33], which is totally opposite to the current finding. A review indicated that the impact of income on weight might follow an inverted U-shape [39]. A possible reason of the current findings was that men with higher income in developing countries were more likely to consume energy dense foods, do a sedentary job, and have few physical activities; all were risk factors related to overweight and obesity. There was a lack of comparability between the results of previous studies and the current study because the study population and regional development level were different in various studies.
Occupational status was associated with the risk of general obesity in men whilst no significant association was noted in women. Thus far, there is no consistent conclusion about the impact of occupation on overweight or obesity. Sedentary works comprise a major part of jobs today [40]. That kind of job would take a long sedentary time and reduce the time of physical activity resulting in weight gain. Physical activity is composed of three main components: occupational activity, household activity such as gardening, cleaning and food preparation; and leisure time activity [41]. However, this study did not include traffic time, or sedentary time, which might result in bias of current finding. Furthermore, the current study categorized occupational status as current working or not working. This classification was different from some previous studies that categorized it into specific types of job. Accurate classification of occupational status was needed in future study to increase comparability between studies.
This study has several strengths, including a representative population-based Chinese sample, and we adjusted for potential confounding factors in models. At the same time, we used the multiple logistic models to analyze the association from a gender discrepancy perspective, to reduce the potential impact of gender differences. Despite the innovations and strengths of this study, the study also has several limitations. First, our study is the cross-sectional design, which is inadequate to confirm the causal association between socio-economic factors and the risk of overweight and obesity. Second, the results may be affected by other factors, such as synergy of genetic inheritance, lifestyle or potential residual confounding factors. Third, our study did not collect dietary data, which is an important factor for obesity development, future research can further incorporate these aspects, and with prudent design is warranted to verify these findings.
Conclusions
The study revealed that the association between the prevalence of overweight and obesity and socio-economic factors. The results of this study provided important epidemiological evidence for the prevention of overweight and obesity, and can provide a reference for the further research in the future. In view of the serious phenomenon of overweight and obesity and the results of this paper, the following two opinions are put forward to prevent the occurrence of overweight and obesity in the future. First, we should energetically develop health knowledge publicity and sports undertakings. Secondly, we should make progress on social medical and health services. And we also recommended that men with high levels of education and income, women with low levels of education, can do some physical exercises, adjust dietary and change lifestyle to maintain their weight levels and health.
Availability of data and materials
All data generated or analysed during this study are included in this manuscript.
Abbreviations
- BMI:
-
Body mass index
- WC:
-
Waist circumference
- NHCC:
-
National Health Commission of China
- CVD:
-
Cardiovascular disease
- GDP:
-
Gross domestic product
- CHNS:
-
China Health and Nutrition Survey
- WGOC:
-
Working Groups on Obesity in China
- LPA:
-
Leisure physical activity
- T2D:
-
Type 2 diabetes
- MET:
-
Metabolic equivalent
- SD:
-
Standard deviation
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Jagadeesan M, Prasanna Karthik S, Kannan R, Immaculate Bibiana C, Kanchan N, Siddharthan J, Vinitha M. A study on the knowledge, attitude and practices (KAP) regarding obesity among engineering college students. Int J Adv Med. 2017;4(6):1681.
WHO. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: WHO; 2013.
Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377(9765):557–67.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9945):766–81.
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, Naghavi M, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27.
NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016;387(10026):1377–96.
Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Peñalver C, Rohde LA, Faraone SV. Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(1):34–43.
Koliaki C, Liatis S, Kokkinos A. Obesity and cardiovascular disease: revisiting an old relationship. Metabolism. 2019;92:98–107.
Avgerinos KI, Spyrou N, Mantzoros CS, Dalamaga M. Obesity and cancer risk: emerging biological mechanisms and perspectives. Metabolism. 2019;92:121–35.
Piché ME, Tchernof A, Després JP. Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res. 2020;126(11):1477–500.
Tiantian W, He C. Pro-inflammatory cytokines: the link between obesity and osteoarthritis. Cytokine Growth Factor Rev. 2018;44:38–50.
Müller-Riemenschneider F, Reinhold T, Berghöfer A, Willich SN. Health-economic burden of obesity in Europe. Eur J Epidemiol. 2008;23(8):499–509.
Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–25.
Kontsevaya A, Shalnova S, Deev A, Breda J, Jewell J, Rakovac I, Conrady A, Rotar O, Zhernakova Y, Chazova I, et al. Overweight and obesity in the Russian population: prevalence in adults and association with socioeconomic parameters and cardiovascular risk factors. Obes Facts. 2019;12(1):103–14.
Chukwuonye II, Chuku A, Okpechi IG, Onyeonoro UU, Madukwe OO, Okafor GO, Ogah OS. Socioeconomic status and obesity in Abia State, South East Nigeria. Diabetes Metab Syndr Obes. 2013;6:371–8.
Kuntz B, Lampert T. Socioeconomic factors and obesity. Dtsch Arztebl Int. 2010;107(30):517–22.
Neuman M, Finlay JE, Davey Smith G, Subramanian SV. The poor stay thinner: stable socioeconomic gradients in BMI among women in lower- and middle-income countries. Am J Clin Nutr. 2011;94(5):1348–57.
Seubsman SA, Lim LL, Banwell C, Sripaiboonkit N, Kelly M, Bain C, Sleigh AC. Socioeconomic status, sex, and obesity in a large national cohort of 15–87-year-old open university students in Thailand. J Epidemiol. 2010;20(1):13–20.
Pampel FC, Denney JT, Krueger PM. Obesity, SES, and economic development: a test of the reversal hypothesis. Soc Sci Med. 2012;74(7):1073–81.
Zhang B, Zhai FY, Du SF, Popkin BM. The China Health and Nutrition Survey, 1989–2011. Obes Rev. 2014;15(Suppl 1):2–7.
Zhen S, Ma Y, Zhao Z, Yang X, Wen D. Dietary pattern is associated with obesity in Chinese children and adolescents: data from China Health and Nutrition Survey (CHNS). Nutr J. 2018;17(1):68.
Albrecht SS, Gordon-Larsen P, Stern D, Popkin BM. Is waist circumference per body mass index rising differentially across the United States, England, China and Mexico? Eur J Clin Nutr. 2015;69(12):1306–12.
Li J, Yang Q, An R, Sesso HD, Zhong VW, Chan KHK, Madsen TE, Papandonatos GD, Zheng T, Wu WC, et al. Famine and trajectories of body mass index, waist circumference, and blood pressure in two generations: results from the CHNS From 1993–2015. Hypertension. 2022;79(3):518–31.
Chen C, Lu FC. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17(Suppl):1–36.
Ma S, Xi B, Yang L, Sun J, Zhao M, Bovet P. Trends in the prevalence of overweight, obesity, and abdominal obesity among Chinese adults between 1993 and 2015. Int J Obes (Lond). 2021;45(2):427–37.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, Leon AS. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–81.
American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36(Suppl 1):S11–66.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–69.
Rengma MS, Sen J, Mondal N. Socio-economic, demographic and lifestyle determinants of overweight and obesity among adults of northeast India. Ethiop J Health Sci. 2015;25(3):199–208.
Cai L, He J, Song Y, Zhao K, Cui W. Association of obesity with socio-economic factors and obesity-related chronic diseases in rural southwest China. Public Health. 2013;127(3):247–51.
Hong SA, Peltzer K, Lwin KT, Aung S. The prevalence of underweight, overweight and obesity and their related socio-demographic and lifestyle factors among adult women in Myanmar, 2015–16. PLoS ONE. 2018;13(3):e0194454.
McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29:29–48.
Zhang H, Xu H, Song F, Xu W, Pallard-Borg S, Qi X. Relation of socioeconomic status to overweight and obesity: a large population-based study of Chinese adults. Ann Hum Biol. 2017;44(6):495–501.
Abrha S, Shiferaw S, Ahmed KY. Overweight and obesity and its socio-demographic correlates among urban Ethiopian women: evidence from the 2011 EDHS. BMC Public Health. 2016;16:636.
Scali J, Siari S, Grosclaude P, Gerber M. Dietary and socio-economic factors associated with overweight and obesity in a southern French population. Public Health Nutr. 2004;7(4):513–22.
Power EM. An introduction to Pierre Bourdieu’s key theoretical concepts. J Study Food Soc. 2015;3(1):48–52.
Hiza HA, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet. 2013;113(2):297–306.
Jin MJ, Chen BB, Mao YY, Zhu YM, Yu YX, Wu YY, Zhang MW, Zhu SK, Chen K. Prevalence of overweight and obesity and their associations with socioeconomic status in a rural Han Chinese adult population. PLoS ONE. 2013;8(11):e79946.
Cawley J. An economy of scales: a selective review of obesity’s economic causes, consequences, and solutions. J Health Econ. 2015;43:244–68.
Yuan F, Gong W, Ding C, Li H, Feng G, Ma Y, Fan J, Song C, Liu A. Association of physical activity and sitting time with overweight/obesity in chinese occupational populations. Obes Facts. 2021;14(1):141–7.
Salmon J, Owen N, Bauman A, Schmitz MK, Booth M. Leisure-time, occupational, and household physical activity among professional, skilled, and less-skilled workers and homemakers. Prev Med. 2000;30(3):191–9.
Acknowledgements
This research uses data from the China Health and Nutrition Survey (CHNS). We thank the China National Institute of Nutrition and Food Safety; the China Center for Disease Control; the National Institutes of Health [Grant Numbers R01HD30880, P30DK056350, R21DK089306, R01HL108427, and R01HD38700]; the Fogarty International Center of the National Institutes of Health.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors conceived, written and edited the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, K., Wu, C., Yao, Y. et al. Association between socio-economic factors and the risk of overweight and obesity among Chinese adults: a retrospective cross-sectional study from the China Health and Nutrition Survey. glob health res policy 7, 41 (2022). https://doi.org/10.1186/s41256-022-00274-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41256-022-00274-y