Abstract
Human umbilical cord blood (CB) and umbilical cord tissue (UC) are attractive sources of somatic stem cells for gene and cell therapies. CB and UC can be obtained noninvasively from donors. CB, a known source of hematopoietic stem cells for transplantation, has attracted attention as a new source of immune cells, including universal chimeric antigen receptor-T cell therapy (CAR-T) and, more recently, universal CAR-natural killer cells. UC-derived mesenchymal stromal cells (UC-MSCs) have a higher proliferation potency than those derived from adult tissues and can be used anon-HLA restrictively. UC-MSCs meet the MSC criteria outlined by the International Society of Gene and Cellular Therapy. UC-MSCs are negative for HLA-DR, CD80, and CD86 and have an immunosuppressive ability that mitigates the proliferation of activated lymphocytes through secreting indoleamine 2,3-dioxygenase 1 and prostaglandin E2, and the expression of PD-L2 and PD-L1. We established the off-the-shelf cord blood/cord bank IMSUT CORD to support novel cell therapy modalities, including the CB-derived immune cells, MSCs, MSCs-derived extracellular vesicles, biological carriers loaded with chemotherapy drugs, prodrug, oncolytic viruses, nanoparticles, human artificial chromosome, combinational products with a scaffold, bio3D printing, and so on.
Similar content being viewed by others
Background
Human umbilical cord blood (CB) has been a well-known source of hematopoietic stem cells (HSCs) for over 25 years. In the present day, CB transplantations are implemented more than 1200 per year in Japan (http://www.jdchct.or.jp/data/report/2022/). However, the number of CB transplantations (CBT) in European countries (EU) is decreasing, instead, the HLA-haploidentical allogeneic HSC transplantation has become popular in the EU rather than CBT. The reason why HLA-haploidentical relatives have become rapidly available sources of HSCs is that prevention methods for acute graft-versus-host disease (aGVHD), mainly post-transplant cyclophosphamide administration, resulting in the removal of alloreactive T cells in the patients [1]. CB is currently the optimal source for immunotherapy using activated T cells, regulatory T cells, and natural killer (NK) cells, with or without genetic modifications. Additionally, there has been an overwhelming interest in mesenchymal stromal cells (MSCs) for immunotherapy and regenerative medicine, although CBs are limited in volume to obtain an adequate number of MSCs. MSCs can be isolated from any tissue in the body, but currently, the major sources of MSCs include the bone marrow (BM), adipose tissue (AD), and umbilical cord (UC) [2]. Among these cell sources, human UC has been rapidly utilized as an abundant source of MSCs worldwide due to its ease of collection, noninvasive collection procedure, and categorization as biological waste at birth. Moreover, it is the youngest nonsenescent human tissue except for ES cells. This review focuses on CB- and UC-derived cells as a source of sustainable material for new modalities in gene and cell therapy.
Characteristics and therapeutic potentials of CB and UC-MSCs
CB has been well-investigated and is known to include a relatively high potential of CD34-positive cells to be expanded, more naïve CD45RA-positive T cell ratios, and more potent suppressor function of regulatory T cells than adult peripheral blood [3, 4].
UC-MSCs meet the criteria of MSCs defined by The International Society for Gene and Cellular Therapy [5, 6]. First, they are plastically adherent when maintained in a standard culture medium supplemented with serum. Second, they are positive for CD105, CD73, and CD90 but negative for CD45, CD34, CD14 or CD11b, CD79α or CD19, and HLA-DR surface molecules. Third, MSCs cannot differentiate into adipocytes, chondrocytes, and osteoblasts in vitro.
Additionally, immunosuppressive abilities and tissue repair are the most important properties of MSCs for clinical use [7]. However, MSCs are activated to suppress the immune system only upon the inflammatory stimuli, including activated T cells, PHA-L, and IFN-γ. He et al. demonstrated that third-party UC-MSCs suppress the proliferation of CD4 and CD8-positive cells activated by allogeneic dendritic cells or inflammatory reagents [8]. Secreted factors such as indoleamine 2, 3-dioxygenase 1, and PGE2 are induced in UC-MSCs by the inflammatory environment and play a critical role in controlling excess immune system [9]. UC-MSCs constitutively express the PD-L2, while PD-L1 is induced in response to IFN-γ [10]. Furthermore, like BM- and AD-derived MSCs, MSCs are negative for HLA class II expression and the co-stimulatory surface antigens CD80 and CD86, which activate T cells [11]. UC-MSCs remain negative for HLA-DR even in the presence of IFN-γ, while HLA-DR on BM-MSCs can be induced upon IFN-γ stimuli [8]. As a result, these cells escape from activated T cells and are utilized in a non-HLA-restricted manner. Because of these anti-inflammatory properties, MSCs may be useful therapeutic candidates for the treatment of inflammatory disorders.
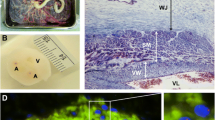
Another important characteristic of UC-MSCs is their ability to repair tissues. Kurtzberg et al. reported that autologous CB may be effective in mitigating the symptoms of cerebral palsy after birth. CD34-positive cells in the CB play a critical role in treating cerebral palsy, and clinical trials using autologous CB for hypoxic–ischemic encephalopathy (HIE) has been performed in Japan [12]. However, collecting adequate amounts of CB for therapeutic interventions is difficult. Recently, allogeneic UC-MSCs have become an attractive source to overcome the disadvantages of CB collection [13]. Causes of cerebral palsy include periventricular leukomalacia (PVL), periventricular hemorrhage, and HIE. However, a common mechanism of cerebral palsy is the early phase of inflammation caused by hypoxia, glucose depletion, and microglia dysfunction with reactive oxygen species, followed by neurogenic damage [13]. The excess inflammation and tissue damage in the pathological cascade are expected to be controlled by MSCs. We previously found that UC-MSCs migrate toward the injured site of the brain after tracking in the lungs, although MSCs do not engraft and disappear after 3 weeks of intravenous injection. UC-MSCs secrete neurotrophic factors such as brain-derived neurotrophic factor and hepatocyte growth factor, and attenuate mice brain injury [14, 15]. These characteristics of UC-MSCs described above are expected to contribute to the development of treatments in the fields of immunotherapy and regenerative medicine.
Umbilical cord blood and cord bank
Establishing a stable supply system for CB- and UC-MSCs is critical for implementing regenerative and immunotherapies. For this purpose, The Institute of Medical Science, The University of Tokyo (IMSUT), has established the cord blood/cord bank IMSUT CORD as a new type of public biobank to supply “off-the-shelf” frozen CB, UC tissues, and UC-derived cells. Briefly, the IMSUT CORD collected both CB and UC data after obtaining informed consent from the guardian of the baby (Fig. 1). In addition to obtaining informed consent, questionnaires about the medical history, genetic history of the baby donor’s family, and history of the mother’s communicable disease risk behavior were collected. CB and UC were collected, and the mother’s blood was tested for infection. These documentation and tests in CB banks can also be referred to as UC banking, although additional infection-related tests for UC banking are strictly required. The collected CB and UC are transported from the hospitals to the CB/UC bank and the IMSUT CORD cryopreserves UC tissue [16] until obtaining confirmation that the baby exhibits healthy, normal development and the mother remains free from infection within at least 6 months after delivery.
The IMSUT CORD processes and freezes CB into frozen enriched cells, while freezes the UC tissue and cultures the frozen-thawed UC tissue into master cells, intermediate cell products, or final cell products, according to the physician’s or company’s requirements of cell modalities.
Clinical trials using UC-MSCs for severe acute GVHD and others
Table 1 shows the reports of clinical trials for severe acute graft-versus-host disease (aGVHD) using UC-MSCs [10, 17]. Not like BM-MSCs, there are only two studies to treat severe aGVHD using UC-MSCs including the author’s one. Here, we introduce our physician-initiated clinical trial for severe aGVHD using allogeneic UC-MSCs (IMSUT-CORD) manufactured in serum-free medium and cryoprotectant from 2018 to 2020 in Japan [10]. In a phase I dose-escalation clinical trial, IMSUT-CORD was administered 1 × 106 cells/kg or 2 × 106 cells /kg intravenously twice per week over 2 cycles. Patients with no adverse effects, partial response (PR), or mixed response (MR) underwent up to two additional cycles. No severe adverse events were observed; at 16 weeks after the initial IMSUT-CORD infusion, one patient showed no response, while one showed MR, two showed PR, and three showed a complete response (CR). The overall response was 71.4% (90% CI 34.1–94.7%), while the overall survival was 85.7% (90% CI 62.2–100%). The continuous CR/PR rate was 100% for > 28 days after CR/PR, while the survival rate was 85.7% on day 100 (90% CI 62.2–100). The overall response rate (ORR) of 70% reported by Soder RP. et al. was similar that of ours. These high ORR and less toxicity show the necessity of conducting further clinical trials. Table 1 shows the reports of clinical trials using UC-MSCs. The overall response rate (ORR) of 70% reported by Soder RP., et al. was similar that of ours. These high ORR and less toxicity show the necessity of conducting further clinical trials.
Other implementations of clinical trials using IMSUT-CORD include phase I clinical trial for COVID-19-related acute respiratory distress syndrome (ARDS), phase I clinical trial for cerebral palsy, and phase II clinical for post-hematopoietic transplantation non-infectious pulmonary complication in Japan. While all three clinical trials were closed, the results have not been published yet.
In our COVID-19-related ARDS study, there are six publications in the world (Table 2) [18,19,20,21,22,23]. Among three phase II clinical trials for COVID-19-related ARDS, one showed an improvement in survival rate significantly [19], while two did not [18, 20].
In clinical trials for cerebral palsy, there is only one publication of phase I, a pilot study, for moderate to severe hypoxic ischemic encephalopathy (HIE) [24]. Six neonates with moderate (4) or severe (2) HIE were enrolled and received one dose of UC-MSCs during HIE and 2 received a 2nd dose 2 months later. All babies survived with average to low-average developmental assessment standards scores for ages between 12 and 17 postnatal months. No severe adverse events were reported in all papers, although 5/6 babies developed low titer anti-HLA antibodies.
As for post-hematopoietic transplantation non-infectious pulmonary complication, no report was found.
CB and UC for exploring new cell modalities
CB and UC-MSCs
Although the use of CB for hematopoietic stem cell transplantation has decreased recently in the world [1], new technologies have promoted the use of expanded CD34 + cells for HSCT [25], regulatory T cells to induce tolerance in HSCT [26, 27], universal chimeric antigen receptor-T cell therapy (CAR-T) [28], and universal CAR-NK cells [29,30,31,32] for hematological malignancies.
In addition to the clinical trials using UC-MSCs introduced in Tables 1 and 2, there are accumulating early-phase clinical trials using UC-MSCs [17, 20, 23, 33,34,35] for engraftment facilitation in HSCT for aplastic anemia [36], neurogenic injuries, diabetes mellitus (DM), heart and angioplasty, liver damage including liver cirrhosis, inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis, prevention of acute rejection in renal transplantation, and collagen diseases [33]. The number of relevant clinical trials on the NIH clinical trial website (https://00m.in/HHVJP) has increased up to 95 trials, including complete, recruiting, and not-yet-recruiting status, as of the end of May 2023.
UC-MSCs-derived extracellular vesicles (EVs)
EVs derived from MSCs might be expected to have effects comparable to those of their parental cells. When parental cells exert therapeutic potency, their EVs may carry the key functional molecules by priming [37, 38]. EV therapy is an emerging type of next-generation cell therapy, but properly testing the safety and efficacy of EVs is challenging. Recently, Rohde et al. proposed clinical testing for the manufacture and characterization of EVs derived from UC-MSCs [39]. The number of preclinical proof-of-concept reports using EVs derived from UC-MSCs is increasing. Chu M. et al. reported the result of a phase 1 clinical trial of nebulization of UC-MSCs derived exosome for patients with COVID-19 pneumonia [40]. The dose of exosome was the same amount of MSCs proportional to the patient’s body weight (1 × 106 cells/kg), and the concentration of exosomes for nebulization ranged from 7.66e + 0.8 to 7.00e + 0.7 particles/ml based on NanoSight. Promoted the absorption of pulmonary lesions and reduced the duration of hospitalization for mild cases of COVID-19 pneumonia were observed with no adverse events.
Other clinical trials using exosomes from UC-MSCs listed on Clinicaltrials.gov are summarized in Table 3. Target diseases are various, such as COVID-19-related diseases, multiple organ dysfunction syndrome after surgical repair of acute type A aortic dissection liver cirrhosis, and retinitis. Out of six clinical trials, one is in a phase II/III study, and another one is in a phase II study. The exosome therapies may be developed rapidly in the near future.
Other modalities
Although UC-MSCs differentiate into osteocytes less frequently than BM-MSCs, tissue engineering with scaffolds such as poly (D, L-lactide-co-glycolide) has been shown to facilitate UC-MSC osteogenesis in a mouse model [41].
Recently, Ikeguchi et al. reported the first clinical application of a Bio three-dimensional (3D) nerve conduit made from a spheroid of human fibroblasts [42] using a bio 3D printer to treat peripheral nerve injury [43], although not yet constructed with UC-MSCs.
UC-MSCs or UC-derived cells can be modified by gene transfer; however, this has not yet been achieved at the clinical level. Meshizuka et al. demonstrated that the CRISPR/Cas9- and AAV-mediated insertion of the beta2 microglobulin-HLA-G fusion gene protected UC-MSCs from allogeneic rejection in a GVHD setting in vitro [44].
MSCs migrate to the tumor microenvironment (TME) and promote tumor cell generation, mainly through the cross-talk of tumor parenchymal cells, tumor-associated fibroblasts, cytokines, and chemokines in the TME, secreting transforming growth factor-β and VEGF recruiting regulatory T cells. Owing to their accessibility, UC-MSCs may be modified and processed into effective biological carriers for loading with chemotherapy drugs, prodrugs, oncolytic viruses [45,46,47], nanoparticles, and human artificial chromosomes [48].
Many studies have been conducted to determine the efficacy of proof-of-concept in treating unmet diseases using CB and UC-MSCs, or their new modality cells.
Conclusions
Both human umbilical CB and UC can serve as effective “off-the-shelf” sustainable sources for gene and cell therapies in immunotherapies and regenerative medicine.
Availability of data and materials
The review does not include patient data; however, data and materials related to banking are made available. Requests may be sent to crc-bank@ims.u-tokyo.ac.jp.
Abbreviations
- AD:
-
Adipose tissue
- aGVHD:
-
Acute graft-versus-host disease
- ARDS:
-
Acute respiratory distress syndrome
- BM:
-
Bone marrow
- CAR-T:
-
Chimeric antigen receptor-T cell therapy
- CB:
-
Umbilical cord blood
- CR:
-
Complete response
- DM:
-
Diabetes mellitus
- EVs:
-
Extracellular vesicles
- HIE:
-
Hypoxic–ischemic encephalopathy
- HSCs:
-
Hematopoietic stem cells
- HSCT:
-
Hematopoietic stem cell transplantation
- IMSUT CORD:
-
The Institute of Medical Science cord blood/cord bank
- MR:
-
Mixed response
- MSCs:
-
Mesenchymal stromal cells
- NK:
-
Natural killer
- PR:
-
Partial response
- TME:
-
Tumor microenvironment UC, umbilical cord
- UC:
-
Umbilical cord tissue
- UC-MSC:
-
Umbilical cord-derived mesenchymal stromal cells
References
Shi PA, Luchsinger LL, Greally JM, Delaney CS. Umbilical cord blood: an undervalued and underutilized resource in allogeneic hematopoietic stem cell transplant and novel cell therapy applications. Curr Opin Hematol. 2022;29(6):317–26.
Mukai T, Sei K, Nagamura-Inoue T. Mesenchymal stromal cells perspective: new potential therapeutic for the treatment of neurological diseases. Pharmaceutics. 2021;13(8):1159.
D’Arena G, Musto P, Cascavilla N, Di Giorgio G, Fusilli S, Zendoli F, et al. Flow cytometric characterization of human umbilical cord blood lymphocytes: immunophenotypic features. Haematologica. 1998;83(3):197–203.
Huang S, Law P, Young D, Ho AD. Candidate hematopoietic stem cells from fetal tissues, umbilical cord blood vs. adult bone marrow and mobilized peripheral blood. Exp Hematol. 1998;26(12):1162–71.
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315–7.
Horwitz EM, Le Blanc K, Dominici M, Mueller I, Slaper-Cortenbach I, Marini FC, et al. Clarification of the nomenclature for MSC: the International Society for Cellular Therapy position statement. Cytotherapy. 2005;7(5):393–5.
Nagamura-Inoue T, He H. Umbilical cord-derived mesenchymal stem cells: their advantages and potential clinical utility. World J Stem Cells. 2014;6(2):195–202.
He H, Nagamura-Inoue T, Takahashi A, Mori Y, Yamamoto Y, Shimazu T, et al. Immunosuppressive properties of Wharton’s jelly-derived mesenchymal stromal cells in vitro. Int J Hematol. 2015;102(3):368–78.
He H, Takahashi A, Mukai T, Hori A, Narita M, Tojo A, et al. The immunomodulatory effect of triptolide on mesenchymal stromal cells. Front Immunol. 2021;12:686356.
Nagamura-Inoue T, Kato S, Najima Y, Isobe M, Doki N, Yamamoto H, et al. Immunological influence of serum-free manufactured umbilical cord-derived mesenchymal stromal cells for steroid-resistant acute graft-versus-host disease. Int J Hematol. 2022;116(5):754–69.
Weiss ML, Anderson C, Medicetty S, Seshareddy KB, Weiss RJ, VanderWerff I, et al. Immune properties of human umbilical cord Wharton’s jelly-derived cells. Stem cells. 2008;26(11):2865–74.
Tsuji M, Sawada M, Watabe S, Sano H, Kanai M, Tanaka E, et al. Autologous cord blood cell therapy for neonatal hypoxic-ischaemic encephalopathy: a pilot study for feasibility and safety. Sci Rep. 2020;10(1):4603.
Nabetani M, Mukai T, Shintaku H. Preventing brain damage from hypoxic-ischemic encephalopathy in neonates: update on mesenchymal stromal cells and umbilical cord blood cells. Am J Perinatol. 2022;39(16):1754–63.
Mukai T, Mori Y, Shimazu T, Takahashi A, Tsunoda H, Yamaguchi S, et al. Intravenous injection of umbilical cord-derived mesenchymal stromal cells attenuates reactive gliosis and hypomyelination in a neonatal intraventricular hemorrhage model. Neuroscience. 2017;355:175–87.
Mukai T, Tojo A, Nagamura-Inoue T. Umbilical cord-derived mesenchymal stromal cells contribute to neuroprotection in neonatal cortical neurons damaged by oxygen-glucose deprivation. Front Neurol. 2018;9:466.
Shimazu T, Mori Y, Takahashi A, Tsunoda H, Tojo A, Nagamura-Inoue T. Serum- and xeno-free cryopreservation of human umbilical cord tissue as mesenchymal stromal cell source. Cytotherapy. 2015;17(5):593–600.
Soder RP, Dawn B, Weiss ML, Dunavin N, Weir S, Mitchell J, et al. A phase I study to evaluate two doses of wharton’s jelly-derived mesenchymal stromal cells for the treatment of de novo high-risk or steroid-refractory acute graft versus host disease. Stem Cell Rev Rep. 2020;16(5):979–91.
Monsel A, Hauw-Berlemont C, Mebarki M, Heming N, Mayaux J, Nguekap Tchoumba O, et al. Treatment of COVID-19-associated ARDS with mesenchymal stromal cells: a multicenter randomized double-blind trial. Crit Care. 2022;26(1):48.
Dilogo IH, Aditianingsih D, Sugiarto A, Burhan E, Damayanti T, Sitompul PA, et al. Umbilical cord mesenchymal stromal cells as critical COVID-19 adjuvant therapy: a randomized controlled trial. Stem Cells Transl Med. 2021;10(9):1279–87.
Gorman EA, Rynne J, Gardiner HJ, Rostron AJ, Bannard-Smith J, Bentley AM, et al. Repair of acute respiratory distress syndrome in COVID-19 by stromal cells (REALIST-COVID Trial): a multicentre, randomised, controlled trial. Am J Respir Crit Care Med. 2023;208(3):256–69.
Lanzoni G, Linetsky E, Correa D, Messinger Cayetano S, Alvarez RA, Kouroupis D, et al. Umbilical cord mesenchymal stem cells for COVID-19 acute respiratory distress syndrome: a double-blind, phase 1/2a, randomized controlled trial. Stem Cells Transl Med. 2021;10(5):660–73.
Kaffash Farkhad N, Sedaghat A, Reihani H, Adhami Moghadam A, Bagheri Moghadam A, Khadem Ghaebi N, et al. Specific clinical and immunological changes following mesenchymal stem cell transplantation in COVID-19-induced acute respiratory distress syndrome patients: a phase-I clinical trial. Iran J Allergy Asthma Immunol. 2022;21(6):687–703.
Shaz BH, Kraft BD, Troy JD, Poehlein E, Chen L, Cheatham L, et al. Feasibility study of cord tissue derived mesenchymal stromal cells in COVID-19-related acute respiratory distress syndrome. Stem Cells Transl Med. 2023;12(4):185–93.
Cotten CM, Fisher K, Malcolm W, Gustafson KE, Cheatham L, Marion A, et al. A pilot phase I trial of allogeneic umbilical cord tissue-derived mesenchymal stromal cells in neonates with hypoxic-ischemic encephalopathy. Stem Cells Transl Med. 2023;12(6):355–64.
Sakurai M, Ishitsuka K, Ito R, Wilkinson AC, Kimura T, Mizutani E, et al. Chemically defined cytokine-free expansion of human haematopoietic stem cells. Nature. 2023;615(7950):127–33.
Motwani K, Peters LD, Vliegen WH, El-Sayed AG, Seay HR, Lopez MC, et al. Human regulatory T cells from umbilical cord blood display increased repertoire diversity and lineage stability relative to adult peripheral blood. Front Immunol. 2020;11:611.
Seay HR, Putnam AL, Cserny J, Posgai AL, Rosenau EH, Wingard JR, et al. Expansion of human tregs from cryopreserved umbilical cord blood for GMP-compliant autologous adoptive cell transfer therapy. Mol Ther Methods Clin Dev. 2017;4:178–91.
Hu K, Huang Y, Hu Y, Huang H. Progress on CAR-T cell therapy for hematological malignancies. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2022;51(2):192–203.
Shah N, Li L, McCarty J, Kaur I, Yvon E, Shaim H, et al. Phase I study of cord blood-derived natural killer cells combined with autologous stem cell transplantation in multiple myeloma. Br J Haematol. 2017;177(3):457–66.
Rafei H, Daher M, Rezvani K. Chimeric antigen receptor (CAR) natural killer (NK)-cell therapy: leveraging the power of innate immunity. Br J Haematol. 2020;193(2):216–30.
Khanmohammadi S, Rezaei N. CAR-NK cells: a promising cellular immunotherapy in lymphoma. Expert Opin Biol Ther. 2023;23(1):37–47.
Li H, Song W, Li Z, Zhang M. Preclinical and clinical studies of CAR-NK-cell therapies for malignancies. Front Immunol. 2022;13:992232.
Nagamura-Inoue T, Nagamura F. Umbilical cord blood and cord tissue bank as a source for allogeneic use. IntechOpen. 2021;Chapter 3:31–55.
Keklik M, Deveci B, Celik S, Deniz K, Gonen ZB, Zararsiz G, et al. Safety and efficacy of mesenchymal stromal cell therapy for multi-drug-resistant acute and late-acute graft-versus-host disease following allogeneic hematopoietic stem cell transplantation. Ann Hematol. 2023;102(6):1537–47.
Couto PS, Al-Arawe N, Filgueiras IS, Fonseca DLM, Hinterseher I, Catar RA, et al. Systematic review and meta-analysis of cell therapy for COVID-19: global clinical trial landscape, published safety/efficacy outcomes, cell product manufacturing and clinical delivery. Front Immunol. 2023;14:1200180.
Wu Y, Cao Y, Li X, Xu L, Wang Z, Liu P, et al. Cotransplantation of haploidentical hematopoietic and umbilical cord mesenchymal stem cells for severe aplastic anemia: successful engraftment and mild GVHD. Stem Cell Res. 2014;12(1):132–8.
Kim DS, Jang IK, Lee MW, Ko YJ, Lee DH, Lee JW, et al. Enhanced immunosuppressive properties of human mesenchymal stem cells primed by interferon-gamma. EBioMedicine. 2018;28:261–73.
Fernandez-Santos ME, Garcia-Arranz M, Andreu EJ, Garcia-Hernandez AM, Lopez-Parra M, Villaron E, et al. Optimization of Mesenchymal Stromal Cell (MSC) Manufacturing processes for a better therapeutic outcome. Front Immunol. 2022;13:918565.
Rohde E, Pachler K, Gimona M. Manufacturing and characterization of extracellular vesicles from umbilical cord-derived mesenchymal stromal cells for clinical testing. Cytotherapy. 2019;21(6):581–92.
Chu M, Wang H, Bian L, Huang J, Wu D, Zhang R, et al. Nebulization therapy with umbilical cord mesenchymal stem cell-derived exosomes for COVID-19 pneumonia. Stem Cell Rev Rep. 2022;18(6):2152–63.
Stanton E, Feng J, Kondra K, Sanchez J, Jimenez C, Brown KS, et al. A murine calvarial defect model for the investigation of the osteogenic potential of newborn umbilical cord mesenchymal stem cells in bone regeneration. Plast Reconstr Surg. 2023. Online ahead of print.
Ikeguchi R, Aoyama T, Tanaka M, Noguchi T, Ando M, Yoshimoto K, et al. Nerve regeneration using the Bio 3D nerve conduit fabricated with spheroids. J Artif Organs. 2022;25(4):289–97.
Ando M, Ikeguchi R, Aoyama T, Tanaka M, Noguchi T, Miyazaki Y, et al. Long-term outcome of sciatic nerve regeneration using Bio3D conduit fabricated from human fibroblasts in a rat sciatic nerve model. Cell Transplant. 2021;30:9636897211021356.
Meshitsuka S, Ninomiya R, Nagamura-Inoue T, Okada T, Futami M, Tojo A. CRISPR/Cas9 and AAV mediated insertion of beta2 microglobulin-HLA-G fusion gene protects mesenchymal stromal cells from allogeneic rejection and potentiates the use for off-the-shelf cell therapy. Regen Ther. 2022;21:442–52.
Kazimirsky G, Jiang W, Slavin S, Ziv-Av A, Brodie C. Mesenchymal stem cells enhance the oncolytic effect of Newcastle disease virus in glioma cells and glioma stem cells via the secretion of TRAIL. Stem Cell Res Ther. 2016;7(1):149.
Wang X, Yang Y, Wang N, Wu X, Xu J, Zhou Y, et al. Mesenchymal stem cell carriers enhance antitumor efficacy induced by oncolytic reovirus in acute myeloid leukemia. Int Immunopharmacol. 2021;94:107437.
Zhang J, Chen H, Chen C, Liu H, He Y, Zhao J, et al. Systemic administration of mesenchymal stem cells loaded with a novel oncolytic adenovirus carrying IL-24/endostatin enhances glioma therapy. Cancer Lett. 2021;509:26–38.
Chartouni A, Mouawad A, Boutros M, Attieh F, Medawar N, Kourie HR. Mesenchymal stem cells: a trojan horse to treat glioblastoma. Invest New Drugs. 2023;41(2):240–50.
Acknowledgements
We thank the IMSUT CORD staff for working on CB and UC banking. We thank Sugita M. and the staff at NTT Medical Center Hospital (Tokyo, Japan) and Yamaguchi S. and the staff at Yamaguchi Hospital for performing UC tissue and CB collection after obtaining informed consent.
Funding
This work was supported by the Japan Agency for Medical Research and Development (AMED) (Project Numbers: 21be0804004h0001, 22be0804004h0002,23be0804004h0003).
Author information
Authors and Affiliations
Contributions
TNI and FN wrote the review collecting the papers and references. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The collection, storage, and release, including safety and quality management, of CB and UC samples were approved by the Ethics Committee of the Institute of Medical Science, University of Tokyo (IMSUT) Hospital (IRB#35–2).
Consent for publication
This manuscript has not been published previously or is not under consideration for publication elsewhere. The authors have read the review manuscript and approved its submission.
Competing interests
This study was partially supported by a joint research study by the University of Tokyo and Human Life Cord Japan Inc. in the development of banking and clinical applications (September 2017). Nagamura-Inoue is a senior medical advisor at Human Life Cord Japan Inc.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nagamura-Inoue, T., Nagamura, F. Umbilical cord blood and cord tissue banking as somatic stem cell resources to support medical cell modalities. Inflamm Regener 43, 59 (2023). https://doi.org/10.1186/s41232-023-00311-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41232-023-00311-4