Abstract
Background
Dengue remains a major public health problem in the Philippines, particularly in urban areas of the National Capital Region. Thematic mapping using geographic information systems complemented by spatial analysis such as cluster analysis and hot spot detection can provide useful information to guide preventive measures and control strategies against dengue. Hence, this study was aimed to describe the spatiotemporal distribution of dengue incidence and identify dengue hot spots by barangay using reported cases from Quezon City, the Philippines from 2010 to 2017.
Methods
Reported dengue case data at barangay level from January 1, 2010 to December 31, 2017 were obtained from the Quezon City Epidemiology and Surveillance Unit. The annual incidence rate of dengue from 2010 to 2017, expressed as the total number of dengue cases per 10,000 population in each year, was calculated for each barangay. Thematic mapping, global cluster analysis, and hot spot analysis were performed using ArcGIS 10.3.1.
Results
The number of reported dengue cases and their spatial distribution varied highly between years. Local clusters were evident during the study period. Eighteen barangays were identified as hot spots.
Conclusions
Considering the spatial heterogeneity and instability of hot spots in Quezon City across years, efforts towards the containment of dengue can be made more targeted, and efficient with the application of hot spot analysis in routine surveillance. This may be useful not only for the control of dengue but also for other diseases, and for public health planning, monitoring, and evaluation.
Similar content being viewed by others
Introduction
With an active transmission in at least 128 countries and four billion people at risk, dengue is recognized as the most common mosquito-borne viral disease [1]. There have been at least 50 million apparent cases every year; the majority of which were reported in the Western Pacific region [2,3,4]. About 10,000 deaths per annum have been attributed to symptomatic dengue infection; most which were reported from the Southeast Asian region [3]. Since the epidemic of hemorrhagic fever in 1954, dengue remains a major public health concern in the Philippines [5]. The country was identified as one of the member states of the Association of Southeast Asian Nations (ASEAN) with the highest burden of dengue [6]. In 2022, more than two hundred thousand dengue cases were documented in the country, which was more than double the documented cumulative number of cases in the past 2 years [7]. Central Luzon (Region II), the National Capital Region (NCR), and the Cagayan Valley (Region II) were the regions with the highest magnitudes of reported cases in 2022 [8].
The Philippines is implementing its National Dengue Prevention and Control Program (NDPCP), aiming to reduce dengue morbidity through its six component strategies—surveillance, case management and diagnosis, integrated vector management, outbreak response, health promotion and advocacy, and research [9]. By offering timely detection of outbreaks and better collection of data on disease burden, a strong case surveillance system can offer supplementary yet vital contributions to achieve the aim of the NDPCP.
The utility of geographic information system (GIS) technology and spatial analytical techniques in dengue epidemiology and surveillance have already been demonstrated in several studies [10]. Global clustering analysis and local cluster detection of diseases are common spatial statistical methods that assess if the geographically bounded aggregation of a disease is of sufficient size and concentration that it is unlikely to be attributable to chance [11, 12]. In a study done in two cities and one county in Taiwan, global clustering analysis and local cluster detection showed that the dengue outbreaks in 2014 and 2015 were highly aggregated and the dengue hot spots were located in the urban, metropolitan districts [13]. Hot spot analysis of dengue in Singapore from 2013 to 2015 showed that the incidence was higher in blocks of low-rise houses, which paved the way for the recommendation of incorporating control of vector borne diseases in public housing plans [14]. The utility of GIS and spatial analysis in surveillance were further underscored during the pandemic when several web-based dashboards were developed to map the spatial distribution of COVID-19 cases globally and across subnational areas [15]. The COVID-19 pandemic in 2020 made it difficult for public health decision makers and managers to allocate human and financial resources and to render health care services against diseases with competing interests, e.g., COVID-19 and dengue. Hot spot identification became useful for identifying priority areas that need immediate attention.
There have been only few studies on mapping and detecting dengue hot spots in the Philippines. In the study of Garcia and de las Llagas in 2011, dengue incidence from 2005 to 2008 across the villages of Quezon City (QC) were mapped using ArcGIS and the maps were analyzed by overlaying with maps of population density, river networks, and land use [16]. The findings of the study provided useful insights into the relationship of dengue incidence with these factors; however, the conclusions were based on visual inspection that may be subjective. A later study, which covered the entire NCR including QC, mapped dengue incidence from 2010 to 2013 across the cities and municipality, and also compared the performance of local Moran’s I and Kulldorf’s spatial scan statistics for detecting dengue hot spots [17]. However, the analysis could have been achieved at a finer spatial scale, i.e., at the level of villages (called barangay).
In consideration of the abovementioned studies on dengue and the persistence of dengue as a public health problem in QC, a collaboration was established between the authors and the Quezon City Epidemiology and Surveillance Unit (QCESU) to demonstrate how GIS and hot spot detection can be used to study the local spatial epidemiology of the disease [18]. Specifically, the spatiotemporal distribution of dengue incidence from 2010 to 2017 was described and dengue hot spots were identified at the barangay level. Findings of this study could be useful for informing public health decision making in QC.
Methods
Study area
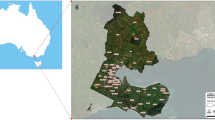
Covering almost one-fourth of the northern part of the NCR, QC rests on the Guadalupe plateau (Fig. 1). Lowlands and rolling ridges characterize the city terrain. The elevation increases towards the north. QC has a total land area of 171.1 km2, the majority of which are residential areas. Since it is a highly urbanized area, much of the land area is used for industrial, commercial, institutional, and recreational purposes. In terms of political administration, QC is divided into six legislative districts and 142 barangays (Fig. 2). The barangay is the smallest administrative unit in the Philippines. The city has a population of 2,936,116, growing at a rate of 1.17% per annum. The population density in the city is 17,099 persons per km2 [19]. The city government is implementing a local dengue control program, which is complemented by a GIS-enabled epidemiology and surveillance unit.
Six legislative districts and barangays of Quezon City, National Capital Region, Philippines. Quezon City is subdivided into 142 barangays, which are grouped into six legislative districts (Additional file 1)
Data collection
Individual level deidentified data on reported dengue cases from January 1, 2010 to December 31, 2017 was provided by the QCESU. The data included the date of consultation, barangay of residence, and name of the disease reporting unit (DRU). Under the Philippine Integrated Disease Surveillance and Response, all units of health service delivery rendered as DRUs in the city, i.e., barangay health stations, hospitals, and clinics, are mandated to routinely submit weekly reports of all dengue cases to QCESU [20]. The population data from each barangay for the national census years 2010 and 2015 were obtained directly from the Civil Registry Department of the Local Government of Quezon City. Population estimation and projection were done for the years 2011 to 2014 and 2016 to 2017 based on the data from 2010 and 2015, respectively.
Data analysis
The annual incidence rate of dengue from 2010 to 2017, expressed as the total number of dengue cases per 10,000 population in each year, was calculated for each barangay. Thematic mapping, global cluster analysis, and hot spot analysis were performed using ArcGIS 10.3.1 (Environmental Systems Research institute, Inc., Redlands, CA, USA). Global cluster analysis was performed using the Getis-Ord General G statistic, while hot spot analysis was done using Getis-Ord Local Gi* statistic. Both tests were performed at the 95% confidence level. Global clustering and identification of dengue hot spots were both indicated by a statistically significant, positive Gi* index [21].
Ethical considerations
Since this study utilized secondary data that did not include any personally identifiable information, an exemption from review and subsequent approval for implementation was granted by the Far Eastern University—Nicanor Reyes Medical Foundation Institutional Ethics Review Committee (FEU-IERC Code: 2018-0011) and the Ethical Committee of University of the Ryukyus (Approval Number: 1391).
Results
Dengue cases and incidence rate
From 2010 to 2017, a total of 41,045 reported dengue cases were recorded by the QCESU. The 8-year average of the annual dengue incidence rates in QC was 16.7 per 10,000. There was large variation in the magnitude of reported cases across the years. The highest number of cases and incidence rate were reported in 2012, while the lowest were in 2011 (Table 1).
Spatial distribution
The spatial distribution of reported dengue cases in QC varied highly across years, as presented in incidence rate maps (Fig. 3). In 2010, dengue was present in almost the entire study area. Only four barangays (barangay 32, 40, 61, and 92) had no reported cases of dengue. The highest incidence rate at 67.44 cases per 10,000 people was documented in barangay 17.
In 2011, dengue appeared to concentrate in the South and near the boundaries of the central area of QC. In the same year, almost 10% of all the barangays had no reported cases of dengue. The highest incidence rate at 39.93 cases per 10,000 people was documented in barangay 62.
The highest number of dengue cases from 2010 to 2017 was reported in 2012 with more than 9000 cases. Dengue was reported in almost all of the barangays in that year. Only barangay 18, 26, and 42 had no reported cases of dengue. The highest incidence rate at 106.84 per 10,000 was documented in barangay 76.
Although the total number of reported dengue cases decreased in 2013, some barangays had higher incidence when compared to others. Barangay 74 had the highest incidence at 185.79 per 10,000. Only barangay 16 had no reported dengue cases.
In 2014, 20% of barangays had an incidence rate of reported dengue cases less than 5 per 10,000. About 8.5% of all the barangays had no reported dengue cases. The highest incidence rate was reported from barangay 93 with 60.94 per 10,000.
An increase in the magnitude of disease was observed in 2015. Only Barangay 61 and 78 had no reported dengue cases. Barangay 76 had the highest incidence rate at 176.17 per 10,000.
In 2016 and 2017, the spatial distributions of reported dengue cases were almost comparable. In both years, barangays 48 and 76 had the highest incidence rate. Barangays 32 and 61 had no reported dengue cases in 2016. However, in 2017, all barangays had reported dengue cases.
Cluster analysis
Statistically significant global clustering of reported dengue cases was observed from 2011 to 2015 (Table 2). Local clusters were evident from 2010 to 2017 (Fig. 4). The highest count of identified hot spots was in 2012 with nine hot spots, while the lowest was in 2016 with only three hot spots. From 2010 to 2017, 18 barangays were identified as hot spots. Barangay 76 was identified annually as a hot spot, except in 2011. Barangay 74 was identified as a hot spot consecutively from 2011 to 2013 and then in 2015. Barangay 93 was identified as a dengue hot spot in the years 2014, 2015 and 2017. Other barangays that were identified in consecutive years were Barangays 56 (2010 to 2011), 86 (2012 to 2013), 91 (2012 to 2013), 123 (2014 to 2015), and 49 (2016 to 2017).
Discussion
In the current study, the annual spatial and temporal variations in the distribution of reported dengue cases in QC from 2010 to 2017 were investigated through mapping, cluster analysis, and hot spot identification. The results revealed that the incidence rates of dengue across barangays were spatially heterogeneous and the dengue hot spots were unstable and varied over the years.
Significant clustering of dengue incidence was observed in QC from 2011 to 2015 based on the results of the global clustering analysis using the Getis-Ord General G statistic. The observed patterns in 2010, 2016, and 2017 were attributable to random processes. However, local cluster detection using Getis and Ord Local Gi* statistic identified hot spots or clusters of areas with high incidence rates throughout the study period. The discrepancy can be explained by the limitation of global measures of spatial autocorrelation, such as the General G statistic. Those measures observe the assumption that spatial processes are stationary, thereby local spatial processes are obscured [11].
To the best of the authors’ knowledge, this is the first study in QC that mapped the incidence of dengue and detected hot spots over time. The presence of time varying hot spots is evidence of spatial heterogeneity, which indicates the non-uniform distribution of any attribute value in a geographic area, i.e., dengue incidence across barangays of QC [11, 22]. Across the years, different hot spots were identified except for a minority of barangays that remained consistently as hot spots, e.g., barangay 76. Mapping the stability of hot spots proved to be useful, because stable hot spots can predict the occurrence of future hot spots and can identify areas that are highly susceptible for a targeted implementation of interventions [23]. In the current study, most of the identified hot spots were unstable. Having hot spot instability has implications for the public health response towards controlling and preventing dengue. Since new hot spots were identified across the years, data collection and analysis need to be done quickly each year to guide targeting of control activities. Ideally, near real-time data collection and analysis are required to rapidly identify new hotspots in a particular year as part of an early warning system to give the public health authorities enough time to respond. This could be operationalized on a weekly or monthly basis. The response should be designed dynamically and contextualized to the situation of the identified hot spot. Aside from depending on the proactive approach of dengue control and prevention, the reactive arm should be strengthened.
Another implication of observing hot spot instability is the identification of the causes of the variability across years. The current study was not designed to determine the factors driving the spatial heterogeneity and instability of hot spots. However, cautious observations can be made. Throughout the study period, the dengue hot spots were frequently situated in the southern half of the city, particularly those barangays in Districts 3 and 4. Having an elevation of 50 m at most, these areas are the city’s lowlands. The predilection of Aedes aegypti to thrive in urban lowlands can explain the observed clustering of dengue in the south [24]. Specifically, the consistent clusters were situated in residential areas that are near commercial areas, which was also noted in a previous study done by Garcia and de las Llagas [16]. Other factors that had been suggested by their study that may explain the distribution of dengue incidence in QC were the presence of informal settlements, poor sanitation, and soil organic carbon content in the area [16]. However, the association of these factors with the observed spatial pattern of dengue in this study was not examined. Spatial regression could be done, provided suitable covariate data could be obtained; i.e., data with the same spatial and temporal scales [22].
During the first 2 years of the COVID-19 pandemic, an apparent decline in reported dengue cases was observed in several countries including the Philippines [25, 26]. This could be the consequence of implementing public health and social measures that restricted human mobility, such as community quarantine, school closures, and lockdowns [27]. However, essential health services were substantially disrupted as countries focused on strengthening their COVID-19 responses [28, 29]. Diagnostic and surveillance capacities of countries could have been limited by the pandemic, which may have resulted in the underreporting of other diseases including dengue [26]. The decline in reported dengue cases may have also been due to reporting hesitancy due to people’s fear of acquiring COVID-19 upon visiting a health facility [30]. Anticipated stigma associated with COVID-19 could have also led people to avoid being tested, which could hamper case detection of both COVID-19 and dengue [31]. As the Philippines moves towards the relaxation of countermeasures against COVID-19, outbreaks of dengue may occur [32, 33]. Spikes in the number of reported dengue cases had already been documented in certain regions of the Philippines, such as the Zamboanga Peninsula, Cagayan Valley, Western Visayas, and Davao Region [34].
While COVID-19 continues to be a priority, resources may remain unevenly allocated for the control and prevention of other diseases including dengue. To address this, hot spot analysis can be used to identify high priority areas and inform public health decision making. However, the instability of hot spots indicates that the analysis needs to be updated more often. This opens an opportunity for integrating hot spot analysis as an innovation in routine dengue surveillance, which can be institutionalized in every municipality or city in the country though a national policy.
Conclusions
The current study demonstrated the utility of GIS, global cluster analysis and hot spot identification in assessing the dengue situation in QC. Findings revealed that dengue remains a challenge to the health situation in QC considering the spatial heterogeneity and the instability of dengue hot spots. Through the identification of hot spots, efforts towards the containment of dengue can be made more targeted and efficient.
Availability of data and materials
The data that support the findings of this study are available from the QCESU, but restrictions apply to the availability of these data, which were used under permission for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the QCESU.
Abbreviations
- ASEAN:
-
Association of Southeast Asian Nations
- COVID-19:
-
Coronavirus disease 2019
- DOH:
-
The Department of Health, the Philippines
- DRU:
-
Disease Reporting Unit
- GIS:
-
Geographic information system
- NDPCP:
-
National Dengue Prevention and Control Program
- QC:
-
Quezon City
- QCESU:
-
The Quezon City Epidemiology and Surveillance Unit
- WHO:
-
World Health Organization
References
Zheng C, Fu J, Li Z, Lin G, Jiang D, Zhou XN. Spatiotemporal variation and hot spot detection of visceral leishmaniasis disease in Kashi Prefecture, China. Int J Environ Res Public Health. 2018;15(12):2784. https://doi.org/10.3390/ijerph15122784.
Pakzad R, Pakzad I, Safiri S, Shirzadi MR, Mohammadpour M, Behroozi A, et al. Spatiotemporal analysis of brucellosis incidence in Iran from 2011 to 2014 using GIS. Int J Infect Dis. 2018;67:129–36. https://doi.org/10.1016/j.ijid.2017.10.017. (Epub 2017 Nov 6).
Chang BA, Pearson WS, Owusu-Edusei K Jr. Correlates of county-level nonviral sexually transmitted infection hot spots in the US: application of hot spot analysis and spatial logistic regression. Ann Epidemiol. 2017;27(4):231–7. https://doi.org/10.1016/j.annepidem.2017.02.004. (Epub 2017 Feb 21).
Hao Y, Zhang N, Wu J, Su B, Gong L, Ma W, et al. Identifying infectious diarrhea hot spots and associated socioeconomic factors in Anhui Province, China. Am J Trop Med Hyg. 2019;101(3):549–54. https://doi.org/10.4269/ajtmh.19-0161.
Bravo L, Roque VG, Brett J, Dizon R. Epidemiology of dengue disease in the Philippines (2000–2011): a systematic literature review. PLOS Negl Trop Dis. 2014;8(11): e3027. https://doi.org/10.1371/journal.pntd.0003027.
Edillo FE, Halasa YA, Largo FM, et al. Economic cost and burden of dengue in the Philippines. Am J Trop Med Hyg. 2015;92(2):360–6. https://doi.org/10.4269/ajtmh.14-0139.
World Health Organization Regional Office for the Western Pacific. Dengue situation updates 664, 2 February 2023. https://www.who.int/docs/default-source/wpro---documents/emergency/surveillance/dengue/dengue-20230202.pdf?sfvrsn=5160e027_111.
Department of Health—Epidemiology Bureau Public Health Surveillance Division. Epidemic-prone disease case surveillance (EDCS): morbidity week no. 52. https://doh.gov.ph/sites/default/files/statistics/2022-EDCS-Weekly-Surveillance-Report-No-52.pdf.
Department of Health, Government of the Philippines. Dengue. https://doh.gov.ph/Health-Advisory/Dengue. Accessed 18 Apr 2022.
Duncombe J, Clements A, Hu W, Weinstein P, Ritchie S, Espino FE. Geographical information systems for dengue surveillance. Am J Trop Med Hyg. 2012;86(5):753–5. https://doi.org/10.4269/ajtmh.2012.11-0650.
Pfeiffer D, Robinson T, Stevenson M, Stevens K, Rogers D, Clements A. Spatial analysis in epidemiology. Oxford: Oxford University Press; 2008.
Lawson AB, Banerjee S, Haining RP, Ugarte MD, editors. Handbook of spatial epidemiology. Boca Raton: CRC Press Taylor & Francis Group; 2016.
Huang CC, Tam TYT, Chern YR, Lung SC, Chen NT, Wu CD. Spatial clustering of dengue fever incidence and its association with surrounding greenness. Int J Environ Res Public Health. 2018;15(9):1869. https://doi.org/10.3390/ijerph15091869.
Seidahmed OME, Lu D, Chong CS, Ng LC, Eltahir EAB. Patterns of urban housing shape dengue distribution in Singapore at neighborhood and country scales. Geohealth. 2018;2(1):54–67. https://doi.org/10.1002/2017GH000080.
Kamel Boulos MN, Geraghty EM. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int J Health Geogr. 2020;19(1):8. https://doi.org/10.1186/s12942-020-00202-8.
Garcia FB Jr, De Las Llagas LA. An examination of the spatial factors of dengue cases in Quezon City, Philippines: a geographic information system (GIS)-based approach, 2005–2008. Acta Med Philipp. 2011;45(1):53–62.
Pangilinan MAP, Gonzales DPG, Leong RNF, Co FF. Spatial analysis of the distribution of reported dengue incidence in the national capital region, Philippines. Acta Med Philipp. 2017;51(2):126–32. https://doi.org/10.47895/amp.v51i2.610.
Hicap J. NCR tallies 11,390 dengue cases; QC, Malabon with highest cases, attack rate. https://mb.com.ph/2022/08/30/ncr-tallies-11390-dengue-cases-qc-malabon-with-highest-cases-attack-rate/. Accessed 31 Jan 2023.
Philippines Statistics Authority. Population, land area, population density, and percent change in population density of the Philippines by region, province/highly urbanized city, and city/municipality; 2015. https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Fpsa.gov.ph%2Fsites%2Fdefault%2Ffiles%2Fattachments%2Fhsd%2Fpressrelease%2F2015%2520Population%2520Density_web.xlsx&wdOrigin=BROWSELINK. Accessed 26 Apr 2022.
Department of Health National Epidemiology Center. Manual of procedure for the Philippine integrated disease surveillance and response, 3rd edition. (Tayag EG, Roque V, Elfa DC, et al., editors). Manila; 2014.
Environmental Systems Research Institute Inc. How hot spot analysis (Getis-Ord Gi*) works. 2018. https://pro.arcgis.com/en/pro-app/tool-reference/spatial-statistics/h-how-hot-spot-analysis-getis-ord-gi-spatial-stati.htm. Accessed 31 Jan 2023.
Lawson A. Statistical methods in spatial epidemiology. Chichester: Wiley; 2006.
Noé A, Zaman SI, Rahman M, Saha AK, Aktaruzzaman MM, Maude RJ. Mapping the stability of malaria hotspots in Bangladesh from 2013 to 2016. Malar J. 2018;17(1):259. https://doi.org/10.1186/s12936-018-2405-3.
Tuladhar R, Singh A, Banjara MR, Gautam I, Dhimal M, Varma A, et al. Effect of meteorological factors on the seasonal prevalence of dengue vectors in upland hilly and lowland Terai regions of Nepal. Parasites Vectors. 2019;12:42. https://doi.org/10.1186/s13071-019-3304-3.
Khan S, Akbar SMF, Yahiro T, Mahtab MA, Kimitsuki K, Hashimoto T, Nishizono A. Dengue infections during COVID-19 period: reflection of reality or elusive data due to effect of pandemic. Int J Environ Res Public Health. 2022;19(17):10768. https://doi.org/10.3390/ijerph191710768.
European Centre for Disease Prevention and Control. Dengue annual epidemiological report for 2020. https://www.ecdc.europa.eu/sites/default/files/documents/DENGUE_AER_2020_Report%20-%20final.pdf. Accessed 9 May 2022.
Chen Y, Li N, Lourenço J, Wang L, Cazelles B, Dong L, et al. Measuring the effects of COVID-19-related disruption on dengue transmission in Southeast Asia and Latin America: a statistical modelling study. Lancet Infect Dis. 2022;22(5):657–67. https://doi.org/10.1016/S1473-3099(22)00025-1. (Epub 2022 Mar 2).
World Health Organization. COVID-19 continues to disrupt essential health services in 90% of countries. https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries. Accessed 13 May 2022.
Downey LE, Gadsden T, Del Rio VV, Peiris D, Jan S. The impact of COVID-19 on essential health service provision for endemic infectious diseases in the South-East Asia Region: a systematic review. Lancet Reg Health Southeast Asia. 2022. https://doi.org/10.1016/j.lansea.2022.04.007.
Seposo XT. Dengue at the time of COVID-19 in the Philippines. WPSAR. 2021;12(2):38–9. https://doi.org/10.5365/wpsar.2020.11.2.015.
Sotgiu G, Dobler CC. Social stigma in the time of coronavirus disease 2019. Eur Respir J. 2020;56(2):2002461. https://doi.org/10.1183/13993003.02461-2020.
Montemayor MT. DOH notes huge drop in dengue cases, deaths. In: GOV.PH. 2021. https://www.pna.gov.ph/articles/1144030?msclkid=f4d46c53d0f011ecb15b22a13d68bd84; https://manilanews.ph/philippines-dengue-pangasinan-reports-doubling-of-cases-in-2021/?msclkid=2a748d89d0f111ec9f8c26975fbafe33. Accessed 13 May 2022.
Fernandez D, Orejas T. DepEd prods all schools to resume 100% face-to-face classes for SY 2022–23. In: Inquirer.net. https://newsinfo.inquirer.net/1604264/fwd-deped-urges-all-schools-to-open-for-faceface-classes-in-next-academic-year. Accessed 2 June 2022.
Casas W. DOH: dengue cases rising in Zambo, CAR, BARMM. In: Manila Standard.net. https://manilastandard.net/news/314222403/doh-dengue-cases-rising-in-zambo-car-barmm.html. Accessed 6 May 2022.
Acknowledgements
The authors would like to extend their deepest gratitude to Mr. Kim Ian Tiu and Mr. Mark Joseph Catayong for liaising on behalf of JCM in public agencies in the Philippines during data acquisition; to Mr. Johnedel Mendoza and Mr. Edmund Basalio of the Quezon City Epidemiology and Surveillance Unit for their support in extracting the data from the database; and to Mrs. Margherita Lotti, Mr. Charbel Makhlouf, Ms. Marie Françoise-Thérèse Martin and Mr. Fernando Martins de Bulhões for their assistance that led to the accomplishment of this study.
Funding
The sponsors did not play any role in this study. This work was primarily supported by JSPS KAKENHI Grant Number JP20KK0223. This research was also funded in part by the Wellcome Trust (grant number 220211). For the purpose of open access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission.
Author information
Authors and Affiliations
Contributions
JCM and JK were involved in the conceptualization of the study. JCM, JK, RJM, CEGM, PMRH, FBG, DN, RVC, and MDA contributed in designing of the study. JRCM, FBG, RVC, and MDA were involved in the data acquisition. FBG, CSR, MS, and ERG coordinated the field work. JCM, SK, KEH, and MK developed the maps. JCM, JK, CEGM, RJM, FBG, PMRH, RVC, MDA, and DN were involved in the data analysis and interpretation of the results. JRCM, RT, and CSR drafted the manuscript. All authors critically reviewed the final manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethical Committee of University of the Ryukyus (approval number: 1391), and by the Far Eastern University—Nicanor Reyes Medical Foundation Institutional Ethics Review Committee (IERC Code: 2018-0011). This study used secondary data, which did not include any personally identifiable information.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Barangays in Quezon City, the Philippines.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Medina, J.R.C., Takeuchi, R., Mercado, C.E.G. et al. Spatial and temporal distribution of reported dengue cases and hot spot identification in Quezon City, Philippines, 2010–2017. Trop Med Health 51, 31 (2023). https://doi.org/10.1186/s41182-023-00523-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41182-023-00523-x