Abstract
Background
Tuberculosis (TB) caused by Mycobacterium tuberculosis is the 13th leading cause of death worldwide. The emergence of multidrug-resistant TB (MDR-TB) poses a major health security threat. Plants have traditionally been used as a source of medicine, since olden days and 80% of the communities in Africa still rely on herbal medicines for their healthcare. In many parts of Uganda, some plants have shown ethno-pharmacological prospects for the treatment of TB, and yet they have not been fully researched.
Aim
This study aimed to document plant species used traditionally by the herbalists and non-herbalist communities of Kitgum and Pader districts for managing symptoms of TB.
Methods
An ethnobotanical study was carried out in 42 randomly selected villages in Kitgum and Pader districts between August 2020 and January 2021. Information was obtained by administering semi-structured questionnaires to 176 respondents identified by snowball and random sampling methods. Data were analysed and presented using descriptive statistics and Informant Consensus Factor (ICF).
Results
Overall, only 27% of the respondents were knowledgeable about plants used for managing symptoms of TB. Nine plant species belonging to six families (Mimosaceae, Apiaceae, Lamiaceae, Rutaceae, Loganiaceae and Rubiaceae) were used to manage symptoms of TB. The most representative family was Rutaceae with three species, followed by Rubiaceae (two species) and the rest of the families were represented by one species each. The most frequently recorded species were Steganotaenia araliacea Hochst. (8.5%), Gardenia ternifolia Schumach. & Thonn (6.8%) and Albizia adianthifolia (Schum.) W.Wight (6.8%). Most of the medicinal plants were trees, and roots (69%) were the most frequently plant part used, followed by the bark (16%) and leaves (15%). The most common method of preparation was by pounding and mixing concoction with water. The administration of the concoctions was mostly done orally.
Conclusions
The results established the existence of few medicinal plants for managing symptoms of TB among the Acholi communities which could be used in developing new, effective plant-based antimycobacterial drugs. The few plants mentioned might face conservation threats due to exploitations of the roots. Phytochemical and toxicological studies are recommended to identify active compounds responsible for antimycobacterial activity.
Similar content being viewed by others
Background
Tuberculosis (TB) is an ancient communicable disease that has been in existence over the past millennia and remains a major global public health burden, with one-third of the world’s population currently infected and more than 1.3 million deaths per year [1, 2]. It is a contagious disease caused by Mycobacterium tuberculosis. It usually attacks the lungs, although it can also spread to other parts of the body, and is transmitted through coughing and sneezing [2]. In most Asian and some African countries, the prevalence of TB per 100,000 population peaks among those aged 35‒54 years [1]. This covers the productive age group, which consequently affects the growth of any country. Globally, an estimated 10 million people developed active TB disease in 2019, with 1.4 million TB deaths [1]. Progress in achieving the United Nations (UN) General Assembly End TB targets remains slow.
Uganda is among the 30 high TB/HIV burden countries accounting for 90% of the global TB burden [2] with an estimated TB prevalence and incidence at 253 cases per 100,000 population and 234 cases per 100,000 annually, respectively [3, 4]. Countrywide, about 7% of the health centres are reportedly providing TB treatment services but lack diagnostic services [5]. This could mean that many people within the communities go undiagnosed and continue to transmit TB among themselves. Northern Uganda with a population of about 6–7 million has a high TB prevalence up to about 8% [6]. Currently, treatment for TB is administered orally and comprises a combination of some or as single therapies of rifampicin, isoniazid, ethambutol and pyrazinamide which are taken for 6 months [7]. Even though this treatment is effective, the utilization of this regimen is challenged by either low or lack of adherence to prescribed therapies, and inefficient healthcare structures [4] which have contributed to the rise of multi-drug resistant strains (MDR) of M. tuberculosis [8, 9]. The simplicity with which TB infection spreads, for instance, by inhalation of droplets nuclei 2–5 mm in diameter containing as few as 1–3 bacilli has helped to sustain this scourge at current levels [8]. However, although millions of people are successfully getting treatment for TB each year, there are still large gaps between the number of people diagnosed and reported, and those accessing treatment [4]. The declining access to adequate TB drugs in the rural health centres calls for an extensive search for complementary, easily accessible and affordable TB drugs which could shorten treatment duration [10]. The use of plant-based drugs could be a complementary drug to treat both resistant and susceptible forms of TB. Medicinal plants have been in use for the treatment of humans and animals in many tribal cultures, and traditional knowledge related to this has been passed on from one generation to the next [11, 12]. It is estimated that nearly 80% of the world’s total population particularly in developing countries depend on traditional medicinal plants and products for their primary healthcare needs [12, 13], due to the high cost of western-style medicines. Uganda’s enormous wealth of plant resources constitute an important part of health care especially for the rural poor [14]. Several ethnobotanical studies have documented medicinal plants being used to treat several diseases [12, 14,15,16,17].
For 20 years (1986–2006), the Acholi sub-region in Northern Uganda experienced conflict as a result of fighting between the Uganda Peoples Defense Forces (UPDF) and the Lord’s Resistance Army (LRA) [18]. Among the many impacts of the war, this also devasted all social services including health systems. The displacement and overcrowding in the IDP camp, coupled with poor sanitation, poor medication and reckless social life escalated health conditions including TB and HIV/AIDS infections. When the community returned to their original homestead in 2006, they continued mixing freely with no precautionary measures hence increasing chances of infection. Inadequate functional medical facilities and poor access to healthcare in rural communities cause many people to seek herbalists who use medicinal plants as remedies for various disease conditions [19, 20]. Due to the prolonged war in the Acholi sub-region, limited research on ethnobotanical plant resources has been undertaken. Most previous studies have focused mostly on humanitarian and political aspects [21, 22] and the use and consumption of wild edible plants [23,24,25]. However, in many parts of Uganda, some plants have shown ethno-pharmacological prospects for the treatment of TB, and yet they have not been fully researched. Unfortunately, the knowledge of which medicinal plants are used in treatments of TB is not well understood. Consequently, there is a need to assess the biodiversity-based cultural knowledge in the Acholi sub-region to ascertain the available medicinal plants that could be exploited in developing new drugs for managing TB and its associated symptoms. This study aimed at documenting plant species used traditionally by herbalists and non-herbalists in Kitgum and Pader districts for managing symptoms of TB, sources of plant knowledge, parts used, habits, side-effects, methods of preparation and modes of administration.
Methods
Description of the study area
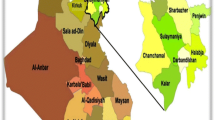
This ethnobotanical survey of plants used in the management of TB symptoms was undertaken in Kitgum and Pader districts in the Acholi sub-region of Uganda (Fig. 1). In general, the Acholi sub-region is categorized as a tropical dry climate similar to the southern part of Sudan. The land is generally well watered in the rainy season and fertile. Most of the land is covered by woody and green vegetation. The total population in Kitgum is 204,048 and that of Pader is 178,004 persons [26]. We selected Kitgum and Pader districts, because these areas are situated at the border and periodically experience an influx of refugees escaping conflicts in Southern Sudan. Moreover, these are unscreened for several diseases hence exposing the population to increasing risks of contraction of diseases including TB. High levels of poverty, poor access to modern health facilities also characterize the selected locations, causing many people to seek herbal remedies for the treatment of various disease conditions.
Population and sample size
The expected sample size of 384 respondents was calculated using the Krejcie and Morgan Table [27]. The respondents included herbalists and non-herbalists aged 15 years and above, covering both females and males of different age groups. However, due to the constraints of time and resources, we interviewed only 176 respondents including 20 herbalists and 156 non-herbalists (i.e., local people who regularly use plants for medicinal purposes) from both Kitgum and Pader districts.
Data collection and selection of study sites and participants
The field survey for this study was conducted from August 2020 to January 2021. From each district, two sub-counties were selected, from which four parishes were randomly selected, and eventually, five to six villages were selected from each parish, resulting in a total of 42 villages. In Kitgum district, Kitgum Matidi and Lagoro sub-counties were included covering Lumule and Paibony, Lukwor and Lukwir parishes, respectively. While in Pader district, Pader Town Council (within the parishes of Acoro and Luna) and Pajule Town Council (within the parishes of Ogole and Olwo) were included. Purposive and snowball sampling method was used in the identification of the herbalist respondents. The first respondent was selected by the village/community leaders from each parish and village based on their reputability and ability to portray good traditional herbal medicine knowledge, and the subsequent respondents were identified by fellow herbalists. The non-herbalists were selected by a simple random sampling technique [28] from the village household register. We selected both herbalists and non-herbalists to ensure that our sample included representatives of the whole community. For each respondent, we recorded information on the socio-demographics including location, gender, age, marital status, age, level of education and occupation and how they acquired knowledge about medicinal plants. Before the interview, the purpose of the study was explained to the respondents and voluntary written prior informed consent and assent were obtained. The respondents were assured of the confidentially of the information and that the data would be used strictly for academic purposes. Ethnobotanical data were collected using semi-structured questionnaires in Acholi, the local language of the respondents and was facilitated by local field assistants who are fluent in both Acholi and English. The questionnaire included information on the local names of the medicinal plants used in TB treatment, the plant parts used, life form, the method of preparation and mode of administration of the herbal remedy. Voucher specimens of all plant species mentioned were collected, pressed and identified by a qualified taxonomist by comparing with herbarium specimens at the Makerere University herbarium (MUH). The catalogue of life (https://www.catalogueoflife.org/), the Flora of Tropical East Africa and the Angiosperm Phylogeny Group APGIV [29] were used to confirm the botanical names, families and authorities.
Statistical analyses
The data were entered in Microsoft Excel Program, coded, and exported to SPSS software for analysis. Descriptive statistics such as frequencies and percentages in SPSS for Windows, version 26 was used to summarize ethnobotanical and respondents’ socio-demographic data. The Informant Consensus Factor, ICF [30, 31] was computed to find out the homogeneity in the ethnomedicinal information from the respondents. ICF was computed using the formula; ICF = Nur − Nt/(Nur − 1), where “Nur” refers to the total number of use reports for each disease cluster and “Nt” refers the total number of species in each use category. The ICF values range from 0 to 1; high ICF values are obtained when only one or a few plant species are reported to be used by a high proportion of informants to treat a particular category, whereas low ICF values indicate that informants disagree over which plant to use.
Results
Socio-demographic characteristics of the respondents
Out of a total of 176 respondents interviewed, the majority (65%) were females (Table 1). The majority of respondents were in the age bracket 36–45 years (34%, average age 40 years) and were mostly married (61%). The least was in the bracket 15–20 years (2.3%). Most (66%) respondents had attained primary level education and the majority were peasant farmers (82%) (Table 1).
Plant species used by the healers and resource users to treat tuberculosis
A total of nine plant species belonging to six families (Mimosaceae, Apiaceae, Lamiaceae, Rutaceae, Loganiaceae and Rubiaceae) and nine genera were reported to manage symptoms of TB in both study areas (Table 2). The most representative family was Rutaceae with three species, followed by Rubiaceae (two species) and the rest of the families were represented by one species each (Fig. 2). The most frequently recorded species were Steganotaenia araliacea Hochst. (8.5%), Gardenia ternifolia Schumach. & Thonn (6.8%) and Albizia adianthifolia (Schum.) W.Wight (6.8%) (Table 2).
The ICF value for management of TB was 0.83. Most of the medicinal plants were trees (seven species) and root was the most (69%) frequently plant part used for management of TB, followed by the bark (16%) and leaves (15%, Fig. 3).
The most common method of preparation was by pounding and mixing concoction with water. The most common method of administration of the medicinal drug was oral intake. Cups were the most used unit for measuring dosage followed by teaspoon. Overall, 27% of respondents had knowledge about plants used to treat TB. Various sources of medicinal plant knowledge exist among the Acholi community. The majority (86%) of the respondents obtained plant knowledge from their parents (Fig. 4).
Discussion
The present cross-sectional study demonstrates that indigenous knowledge and medicinal plants used in the management of TB still exist among the herbalists and non-herbalists in Kitgum and Pader districts despite the prolonged civil war that eroded the traditional culture of medicinal plants. Overall, only nine plant species were documented from a survey of 176 respondents. Although the number of species mentioned is small compared to what is recorded elsewhere in Uganda and other regions in Africa [10, 17, 32, 33], at least a database of the medicinal plants used for treating TB treatment in Kitgum and Pader district is initiated. However, the low number of plant species registered could imply that traditional knowledge for TB treatment is a closely guarded secret [34] and is likely a specialized practice, known only by few people. Knowledge of these plants may also be seen as a source of income to help lift the households out of poverty. Consequently, divulging this information would mean an infringement on their income source. Thus, to tap this knowledge, we suggest the introduction of alternative livelihoods opportunities for the target communities.
Some of the plant species documented in the present study have also been reported in other regions in Uganda and across the world for management of TB [10, 17, 35]. For example, Zanthoxylum leprieuri Guill. & Perr, Steganotaenia araliaceae Hochst and Zanthoxylum chalybeum Engl. have been documented as a remedy for managing symptoms of TB and other respiratory ailments in studies conducted in other parts of Uganda [10, 17]. This similarity in the usage of the same plant species from different places implies that these plants may be potential sources of anti-tuberculosis drugs. This calls for modern scientific validation to verify their efficacy and safety to promote their widespread use among the community.
The source of the medicinal plant knowledge from this study tally with what is reported in the literature [36], although parents were more resourceful than the grandparents. This shows that parents are still interested in passing indigenous knowledge to their children. This strengthens the model transfer of knowledge from grandparents to the parents who are now the main channel to the children according to our study. However, if adequate knowledge is not passed, to the parents then the indigenous knowledge can disappear as the older generation succumbs to death. The high ICF value (0.83) obtained indicates agreements among respondents on the different plant species used to manage TB [31]. Nonetheless, our results constitute potential plants for development of new drugs against M. tuberculosis which could be integrated into conventional medical therapies.
Rutaceae and Rubiaceae which were the dominant families in this study are in accordance with previous studies elsewhere in Uganda by Tabuti et al. [10] and Bunalema et al. [17] that have revealed these families as used in managing symptoms of TB and other respiratory infections. However, families Fabaceae and Asteraceae previously reported to house several medicinal plants for management of symptoms of TB by herbalists in other regions [10, 33] were not documented. This finding might be due to the high accessibility of these species in that region. To the best of our knowledge, plant species from the family Rubiaceae are mentioned for medicinal plant use for the first time in this region.
The finding of root bark as the most frequently mentioned plant part in managing symptoms of TB than other parts is consistent previous study conducted by Medikizela et al. [32] in O.R.Tambo district in the Eastern Cape Province, South Africa, in which roots (39%) were reported as the most frequently used plant part followed by bark (21%). On the contrary, other studies, e.g., Semenya and Maroyi, [37] in Limpopo province of South Africa; Bunalema et al. [17] in Mpigi and Bunamawa districts of Uganda and Lawal et al. [38] in Kenya have recorded leaves as the most frequently used plant part for preparing herbal remedies. The possible reasons for the preference of roots for herbal medicines are unknown but could be due to their high concentration of bioactive compounds and nutrients compared to other plant parts [39, 40]. However, the root collection is destructive and can pose serious threats to conservation of the plant species [41].
The most common form of utilization of herbal remedies was pounding and mixing concoction with cold or warm water. Similar findings have been reported in previous works conducted in other regions in East Africa [10, 17, 42] which indicated that decoction was the most prevalent mode of use of traditional ethnomedicine for TB management. The preference for decoction is probably because decoction is simple and results in more concentrations of phytochemicals and, therefore, might increase its bioactivity [43]. The use of a cup as the measure for dose administration reported in this study is in line with previous studies, e.g., Tuasha et al. [44] in Ethiopia. However, the use of cup as a measure of dosage is inappropriate and can cause overdose as cups are of different volumes. Therefore, there is a need to educate the herbalists to standardize their measurements.
Conclusions
The study demonstrates the existence of medicinal plant knowledge and plants used in the community for managing symptoms of tuberculosis. However, for most of the plants mentioned the roots and the barks were the most used plant part for therapeutic purpose and this threatens the conservation of these plant species. Decoction was the common method of preparation. However, despite the small numbers of plants mentioned, the results of the current study could form a basis for the development of a new class of drugs for treatment of TB. There is need for a systematic and comprehensive inventory of these plants in the entire Acholi subregion to tap more information on these plants. Further isolation and purification of bioactive compounds responsible for the antimycobacterial activity, safety and efficacy of the mentioned plant species are recommended. The study also recommends any possible conservation method such as the establishment of medicinal plant home gardens and in vitro plant tissue culture.
Limitations
An important limitation of this study is the small number of reported medicinal plants and this could imply that the respondents were not free to declare their acquired indigenous knowledge to the researchers for various reasons. In addition, the size of the cups which the healers referred to as used in the administration and the timing for administering the drugs in relation to the frequency were not fully captured.
Availability of data and materials
The data sets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TB:
-
Tuberculosis
- HIV/AIDS:
-
Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome
- MDR-TB:
-
Multi-drug resistant Tuberculosis
- ICF:
-
Informant Consensus Factor
- UN:
-
United Nations
- UPDF:
-
Uganda People’s Defense Forces
- LRA:
-
Lord’s Resistance Army
- IDP:
-
Internally Displaced People’s Camp
- WHO:
-
World Health Organization
- APG:
-
Angiosperm Phylogeny Group
References
Micheni LN, Kassaza K, Kinyi H, Ntulume I, Bazira J. Diversity of mycobacterium tuberculosis complex lineages associated with pulmonary tuberculosis in Southwestern. Uganda Tuberc Res Treat. 2021. https://doi.org/10.1155/2021/5588339.
World Health Organization. Global tuberculosis report 2020. https://www.who.int/publications/i/item/9789240013131. Accessed 2 Nov 2021.
NTLP. Report on the population-based survey of prevalence of tuberculosis disease in Uganda: 2014–15. 2015. https://www.health.go.ug/cause/the-uganda-national-tuberculosis-prevalence-survey-2014-2015-surveyreport/. Accessed 2 Nov 2021.
World Health Organization. Global tuberculosis report 2017. https://www.who.int/tb/publications/global_report/gtbr2017_main_text.pdf. Accessed 2 Nov 2021.
Uganda Ministry of Health. The Republic of Uganda. The Uganda National Tuberculosis Prevalence Survey, 2014–2015 Survey Report 2015. https://www.health.go.ug/cause/national-tuberculosis-and-leprosy-control-programme-revised-national-strategic-plan-2015-16-2019-20/. Accessed 2 Nov 2021.
Kitara D, Pirio P, Acullu D, Opira C. Tuberculosis (TB) Co-infection with HIV/AIDS: clinical presentation at Lacor Hospital, a post-conflict Northern Uganda. Br J Med Med Res. 2015;5(3):386–95.
Albanna AS, Smith BM, Cowan D, Menzies D. Fixed-dose combination antituberculosis therapy: a systematic review and meta-analysis. Eur Respir J. 2013;42(3):721–32.
Koul A, Arnoult E, Lounis N, Guillemont J, Andries K. The challenge of new drug discovery for tuberculosis. Nature. 2011;469(7331):483–90.
Loddenkemper R, Sotgiu G, Mitnick CD. Cost of tuberculosis in the era of multidrug resistance: will it become unaffordable? Eur Respir J. 2012;40:9–11.
Tabuti JR, Kukunda CB, Waako PJ. Medicinal plants used by traditional medicine practitioners in the treatment of tuberculosis and related ailments in Uganda. J Ethnopharmacol. 2010;127(1):130–6.
Nankaya J, Gichuki N, Lukhoba C, Balslev H. Medicinal plants of the Maasai of Kenya: a review. Plants. 2020;9(1):44.
Tugume P, Nyakoojo C. Ethno-pharmacological survey of herbal remedies used in the treatment of paediatric diseases in Buhunga parish, Rukungiri District, Uganda. BMC Complement Altern Med. 2019;19(1):1–10.
Bodeker C, Bodeker G, Ong CK, Grundy CK, Burford G, Shein K. WHO global atlas of traditional, complementary and alternative medicine. Geneva: World Health Organization; 2005.
Kamatenesi MM, Acipa A, Oryem-Origa H. Medicinal plants of Otwal and Ngai sub counties in Oyam district. Northern Uganda J Ethnobiol Ethnomed. 2011;7(1):1–4.
Nguta JM, Appiah-Opong R, Nyarko AK, Yeboah-Manu D, Addo PGA. Medicinal plants used to treat TB in Ghana. Int J Mycobacteriology. 2015;4(2):116–23.
Okello J, Ssegawa P. Medicinal plants used by communities of Ngai Subcounty, Apac District, northern Uganda. Afr J Ecol. 2007;45:76–83.
Bunalema L, Obakiro S, Tabuti JRS, Waako P. Knowledge on plants used traditionally in the treatment of tuberculosis in Uganda. J Ethnopharmacol. 2014;151(2):999–1004.
Durick H. 2013. Conflict affected development in northern Uganda: the importance of holistically addressing sexual and gender-based violence: University of Tennessee Honors Thesis Projects. http://trace.tennessee.edu/utk_chanhonoproj/1603. Accessed 03 Nov 2021.
Oryema C, Ziraba RB, Omagor N, Opio A. Medicinal plants of Erute county, Lira district, Uganda with particular reference to their conservation. Afri J Ecol. 2010;48(2):285–98.
Tugume P, Kakudidi EK, Buyinza M, Namaalwa J, Kamatenesi M, Mucunguzi P, Kalema J. Ethnobotanical survey of medicinal plant species used by communities around Mabira Central Forest Reserve. Uganda J Ethnobiol Ethnomed. 2016;12(1):1–28.
Atim T, Marshak A, Mazurana D, Farrar J. The effects of the lord’s resistance army’s violence on victims from Northern Uganda in prosecutor vs dominic ongwan. Boston: Feinstein International Center; 2018. p. 5–7.
Parker M, Fergus CA, Brown C, Atim D, Ocitti J, Atingo J, Allen T. Legacies of humanitarian neglect: long term experiences of children who returned from the Lord’s Resistance Army in Uganda. Confl Health. 2021;15(1):1–9.
Loki RB, Ndyomugyenyi EK. Diversity and nutritional values of wild fruits of Acholi Sub-region, Northern Uganda. J Environ Sci Toxicol Food Technol. 2016;10(11):79–85.
Onen CO, Oryem-Origa H. Ethno-botanical uses of Ugandan edible wild fruit species. Environ Earth Ecol. 2017. https://doi.org/10.24051/eee/80760.
Nyero A, Achaye I, Odongo W, Anywar G, Malinga GM. Wild and semi-wild edible plants used by the communities of Acholi sub-region. Northern Uganda Ethnobot Res Appl. 2021;21:1–2.
UBOS. 2014. In main report. Uganda Population and Housing Census. Kampala: The Uganda Bureau of Statistics; https://uganda.unfpa.org/en/publications/nationalpopulation-and-housing-census-2014-0. Accessed 31 Oct 2021.
Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970;30(3):607–10.
Chase MW, Christenhusz MJ, Fay MF, Byng JW, Judd WS, Soltis DE, Mabberley DJ, Sennikov AN, Soltis PS, Stevens PF. An update of the Angiosperm Phylogeny Group classification for the orders and families of flowering plants: APG IV. Bot J Linn Soc. 2016;181(1):1–20.
Cochran W. Sampling techniques. Sampling techniques, 3rd edition, vol. 3. New York: John Wiley and Sons; 1977. p. 1–500.
Heinrich M, Ankli A, Frei B, Weimann C, Sticher O. Medicinal plants in Mexico: Healers’ consensus and cultural importance. Soc Sci Med. 1998;47(11):1859–71.
Faruque MO, Uddin SB, Barlow JW, Hu S, Dong S, Cai Q, Li X, Hu X. Quantitative ethnobotany of medicinal plants used by indigenous communities in the Bandarban District of Bangladesh. Front Pharmacol. 2018;6(9):40.
Madikizela B, Kambizi L, McGaw LJ. An ethnobotanical survey of plants used traditionally to treat tuberculosis in the eastern region of OR Tambo district. South Africa S Afr J Bot. 2017;109:231–6.
Obakiro SB, Kiprop A, Kowino I, Kigondu E, Odero MP, Omara T, Bunalema L. Ethnobotany, ethnopharmacology, and phytochemistry of traditional medicinal plants used in the management of symptoms of tuberculosis in East Africa: a systematic review. Trop Med Health. 2020;48(1):1–21.
Kigen GK, Ronoh HK, Kipkore WK. Current trends of traditional herbal medicine practice in Kenya: a review. Afr J Pharmacol Ther. 2013;2(1):32–7.
Ogbole O, Ajaiyeoba E. Traditional management of tuberculosis in Ogun State of Nigeria: the practice and ethnobotanical survey. Afr J Tradit Complement Altern Med. 2010. https://doi.org/10.4314/ajtcam.v7i1.57270.
Semenya SS, Potgieter MJ. Bapedi traditional healers in the Limpopo Province, South Africa: their socio-cultural profile and traditional healing practice. J Ethnobiol Ethnomed. 2014;10(1):1–2.
Semenya SS, Maroyi A. Medicinal plants used for the treatment of tuberculosis by Bapedi traditional healers in three districts of the Limpopo Province, South Africa. Afr J Tradit Complement Altern Med. 2013;10(2):316–23.
Lawal IO, Grierson DS, Afolayan AJ. Phytotherapeutic information on plants used for the treatment of tuberculosis in Eastern Cape Province, South Africa. Evid Based Complement Alternat Med. 2014. https://doi.org/10.1155/2014/735423.
Basualdo I, Zardini EM, Ortiz M. Medicinal plants of Paraguay: underground organs. II Econ Bot. 1995;49(4):387–94.
Adnan M, Ullah I, Tariq A, Murad W, Azizullah A, Khan AL, Ali N. Ethnomedicine use in the war affected region of northwest Pakistan. J Ethnobiol Ethnomed. 2014;10(1):1–6.
Amuka O, Mbugua PK, Okemo PO. Ethnobotanical survey of selected medicinal plants used by the Ogiek communities in Kenya against microbial infections. Ethnobot Res Appl. 2014;12:627–41.
Raja RR. Medicinally potential plants of Labiatae (Lamiaceae) family: an overview. Res J Med Plant. 2012;6(3):203–13.
Barkaoui M, Katiria A, Boubaker H, Msanda F. Ethnobotanical survey of medicinal plants used in the traditional treatment of diabetes in Chtouka Ait Baha and Tiznit (Western Anti-Atlas). Morocco J Ethnopharmacol. 2017;198:338–50.
Tuasha N, Petros B, Asfaw Z. Medicinal plants used by traditional healers to treat malignancies and other human ailments in Dalle District, Sidama Zone. Ethiopia J Ethnobiol Ethnomed. 2018;14(1):1–21.
Acknowledgements
We appreciate the funding support from Training Health Researchers into Vocational Excellence in East Africa (THRiVE 2) Project, Gulu University. We are grateful to all resource users and healers from Kitgum and Pader districts who volunteered to take part in the study.
Funding
This study was funded by the Training Health Researchers into Vocational Excellence (THRiVE 2) Project of Gulu University under the Career Development Award (CDA) to CO, GMM and KR.
Author information
Authors and Affiliations
Contributions
CO, GMM and KR conceptualized and designed the study and were the principal investigators in the project. CO, GMM, KR and SWO collected field data and performed the analysis of data. SWO was a student on the project, and this contributed to his Master’s degree research. CO wrote the initial draft and GMM, KR and SWO critically revised the manuscript for its intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethical approval was obtained from the Gulu University Research Ethics Committee (GUREC) and the Uganda National Council of Science and Technology (UNCST, HS2506), office of the Ugandan President. The study participants were informed of the benefits and the risks of the study and assured of the confidentially of the information obtained. Prior to the study, written informed consent and assent were sought from respondents aged 18 years and above and from parents or guardians of children aged between 15 and 17 years, respectively.
Consent for publication
All data were anonymyized prior to analysis. Therefore, individual consent for publication was not required.
Competing interests
The authors declare that they have no any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oryema, C., Rutaro, K., Oyet, S.W. et al. Ethnobotanical plants used in the management of symptoms of tuberculosis in rural Uganda. Trop Med Health 49, 92 (2021). https://doi.org/10.1186/s41182-021-00384-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41182-021-00384-2