Abstract
Background
Renal ischemia/reperfusion injury is an unavoidable event in transplantation in which free radical-mediated injury determines release of pro-inflammatory cytokines and activation of innate immunity. In addition to their cholesterol-lowering action, statins have shown dose-dependent pleiotropic effects on inflammatory pathways and oxidative stress. We investigated the effects of high-dose atorvastatin (atorvastatin 40 mg/kg) in preventing ischemia/reperfusion injury in an animal model of kidney transplant.
Methods
Forty female rats underwent left nephrectomy and orthotopic autotransplantation. Animals were divided in four groups: A = Transplant only; B = high-dose atorvastatin + Transplant; C = right nephrectomy + Transplant; D = high-dose atorvastatin + right nephrectomy + Transplant. Bilateral nephrectomy was performed 24 h post-transplant. Oxidative stress was assessed measuring malondialdehyde (MDA), superoxide dismutase (SOD), glutathione peroxidase (GPx) and myeloperoxidase (MPO) activity on renal tissue; ischemia/reperfusion injury was also evaluated by histology. Donor pre-treatment with high-dose atorvastatin improved oxidative stress.
Results
MDA levels were lower in group B versus A (p = 0.002) and D (p = 0.004). High-dose atorvastatin pre-treated rats displayed higher GPx activity in group B versus A (p = 0.009) and D (p = 0.005). SOD scavenger activity was also higher in group B versus A (p < 0.001) D (p < 0.001) and C (p = 0.003). MPO activity was lower in group B versus A (p = 0.02), C (p = 0.007) and D (p = 0.03). Histology revealed significantly lower rate of intratubular casts and luminal congestion in Group D versus C (p = 0.02 and p = 0.008, respectively).
Conclusions
High-dose atorvastatin pre-treatment reduces oxidative stress and inflammation in a model of kidney transplant in the rat.
Similar content being viewed by others
Introduction
Ischemia/reperfusion (I/R) injury is one of the leading causes of delayed graft function and renal failure in transplanted kidneys [1, 2]. I/R injury has a multifactorial genesis in which oxidative stress, inflammation and apoptosis are the main actors, although other mechanisms which might contribute to cause cellular damage and cell death are still unclear.
During ischemia free radical-mediated injury causes the release of pro-inflammatory cytokines and activates innate immunity, but the occurrence of reperfusion leads to a rapid burst of free radicals responsible for endothelial injury and makes endothelial cells permeable to proteins and small particles, thus intensifying inflammatory edema which can increase cell death, possibly as a result of oxidative stress, inflammation and apoptosis [3]. This process is well known as the oxygen paradox [4, 5].
The relationship between ischemia and inflammation is well known and clinically relevant. Ischemia of the organ grafts can also lead to a pro-inflammatory state, which increases the immunogenicity of the graft [6].
Medical therapies based on anti-inflammatory and antiapoptotic drugs and antioxidant free radical scavengers have been attempted with the aim of preventing tissue injury and irreversible damage [3], among these the inhibitors of 3-hydroxy-3-methyl-glutaryl-coenzyme A (HMG-CoA) reductase, also known as statins, arouse particular interest.
Statins, besides their well-known cholesterol-lowering activity, have pleiotropic effects, acting on inflammatory pathways as well as on the immune system, oxidative stress and apoptosis. These effects are dose-related and independent of their lipid lowering action [7,8,9,10]. High-dose atorvastatin (HATA) in particular has shown to attenuate ischemia/reperfusion injury after cardiac percutaneous revascularization [11]. In a previous study, we have demonstrated the protective effect on oxidative stress of HATA in vivo in an ischemia–reperfusion rat model [12].
To our knowledge only few studies have analyzed the effects of statins in preventing ischemia reperfusion injury after transplantation [13, 14], none has investigated the effects of their administration before transplantation.
The aim of the present study was to evaluate the efficacy of HATA pretreatment to prevent I/R injury in a rat renal autograft model.
Materials and methods
The study was mainly focused to evaluate the protective effects of atorvastatin on ischemia reperfusion injury. Since the damage is directly connected to oxidative stress, the study was specifically designed to perform an adequate analysis of the biochemical parameters of oxidative stress and inflammation, as well as to perform the research of initial histopathological signs of cellular damage and recognize the as soon as earlier possible the effects of atorvastatin.
This preclinical, case–control, open-label study in vivo using a rat model was carried out at the Animal Care Centre of the Catholic University of Rome. Animal experiments were performed, upon approval of the Animal Care Ethical Committee in accordance with the current Italian Animals Protection Law (from the National Institute of Health) [15] and the current principles of the laboratory animal care of the European Union [16].
Experimental design
Forty female Wistar rats (weight range 300–450 gr) were randomly divided into 4 groups according to drug pre-treatment and surgical procedure. All animals underwent left nephrectomy and subsequent orthotropic kidney autotransplantation.
The choosing to include only female rats in the study depends from two reasons. The first is that several studies demonstrated that sex affects the susceptibility and pathogenesis of ischemia reperfusion injury. Some authors have demonstrated that sex and estrogen mediate the response from the normal kidney to the ischemia reperfusion injury kidney [17] In addition, both estrogen and testosterone could modulate recovery following ischemia reperfusion injury. [18]. Therefore, we choose rats of one sex to avoid some possible variability due to hormonal variation. The second reason to prefer female rats was due to the surgical technique of blood supply of left kidney and suprarenal gland. Left renal artery and vein are longer in female than male rats, as well the isolation of the left gonadal and adrenal vessels are technically easier in female specimen.
The animals were randomly allocated to 4 groups, as follows:
-
A.
Transplantation only (control): nephrectomy and renal transplantation with no drug pre-treatment.
-
B.
HATA + Transplantation: nephrectomy and renal transplantation preceded by high-dose atorvastatin treatment (40 mg/kg of atorvastatin pulverized and dissolved in 3 ml of water administered by gavage) 24 h before surgery
-
C.
Transplantation + contralateral nephrectomy + : nephrectomy and renal transplantation followed by contralateral nephrectomy, in order to reproduce a model of renal failure and eliminate the bias related to normal function of the contralateral kidney, without drug pre-treatment
-
D.
HATA + Transplantation + contralateral nephrectomy: nephrectomy and renal transplantation preceded by treatment with HATA, and followed by contralateral nephrectomy.
Dose and administration route of HATA were based on previous studies [12, 19, 20]. In the animal murine models, reported in the largest part of the studies, the dose of 40 mg/(kg day) is considered the “high dose” of atorvastatin able to warrantee the pleiotropic effects and reduce the incidence of adverse reactions in rats. We consequently applied the same dose of 40 mg/(kg day) in our murine model.
Surgical procedure
Throughout all surgery and recovery, the rat was placed on a heating pad to contrast hypothermia. Administration of antibiotics was not necessary since animals were sacrificed within 24 h from surgery, the risk of developing an infection in this period of time being considered negligible.
All animals were housed for 48 h (24 h before and 24 h after surgery), underwent general anesthesia using intramuscular ketamine 1 ml/kg, xylazine 0,7 ml/kg and were sacrificed 24 h after surgery in order to take tissue for sampling.
Transplantation technique
Kidney autotransplantation was performed with the aid of a Zeiss operator mod. OPMI PIC microscope working with 2.5 magnification. Surgical phases are described in Fig. 1.
Skin disinfection was followed by xipho-pubic incision, colic mobilization, isolation and section between ligatures of left gonadal and adrenal vessels followed by careful dissection of the left renal artery and vein from their origin (aorta and vena cava) to the renal hilum, dissection of the ureter and complete mobilization of the left kidney.
Five minutes following intracaval heparinization, the renal artery and vein were clamped and left nephrectomy performed. The procured kidney was perfused with 15 ml of heparinized solution at 4 °C and then stored for 60 min at low temperature (0–4 °C).
Arterial, venous and ureteric end to end anastomosis were performed with a 10–0 nylon suture (average anastomotic time: 45 min), at the end the kidney was re-vascularized.
For groups C and D a right nephrectomy was also performed at the end of left kidney auto-transplantation.
Tissue sampling
24 h after surgery, animals were anesthetized and underwent nephrectomy of the transplanted kidney. The kidney was then divided into 2 halves, respectively, stored at − 80 °C and in paraffin. All animals were sacrificed at the end of the procedure.
Biochemical evaluation
Half of the kidney specimen was fixed in formalin for histological essay, the remaining half was frozen at − 80 °C, until the determination of tissue levels of MPO, MDA, SOD and GPx.
Tissues were placed in 1.15% KCl solution and homogenized for 30 min at 14,000 rpm. Aliquots of homogenate were centrifuged at 10,000 rpm for 30 min, and the supernatants were analyzed for MPO, MDA, SOD and GPx activities as reported elsewhere [12, 21].
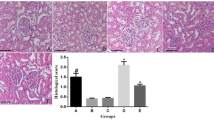
Histology
Paraffin embedding was performed using routine procedures. Paraffin sections were stained with hematoxylin/eosin, periodic acid-Schiff and trichrome and blindly revised by an experienced pathologist. Sections were scored according to the Banff classification on renal transplant biopsies [22].
The following parameters were blindly evaluated by a pathologist:
-
Convoluted proximal tubule epithelium necrosis.
-
Necrosis of the Capsular Epithelium.
-
Tubular Obstruction.
-
Hyaline casts in the convoluted distal tubule.
Statistical analysis
Rats’ identification numbers and the results of immunoenzymatically assessment of the analyzed markers were entered into a database. Statistical analysis between groups was performed using the Mann–Whitney test and Kolmogorov–Smirnov test for numeric variables with nonparametric; the analysis of variance was performed with Kruskal–Wallis one-way method (ANOVA) followed by Dunn's multiple comparison test. Categorical variables were compared using cross-tabulation and Chi-square. A p value of < 0.05 was considered statistically significant. Statistical analysis was performed with SPSS 14.0 for Windows (SPSS Statistical Software, Chicago, IL).
Results
Effect of statins on markers of oxidative stress
Table 1 reports mean and standard deviation of parameters of oxidative stress for each study group and comparison between A versus B and C versus D groups. Figure 2 reports comparison among the four groups for each parameter.
Effect on Glutathione Peroxidase (GPx) activity (Fig. 2a); Superoxide Dismutase (SOD) activity (Fig. 2b); Malondialdehyde (MDA) activity (Fig. 2c) and Myeloperoxidase (MPO) activity (Fig. 2d). A = Transplantation only (control): B = High-dose Atorvastatin + Transplant; C = Left kidney transplant + Right nephrectomy; D = High-dose Atorvastatin + Left kidney transplant + Right nephrectomy
Effect on antioxidants enzymes
We found significantly higher GPx activity in HATA treated rats versus controls group (A: 39.14 ± 27.45 vs. B 80.62 ± 49.11; p = 0.001), a positive trend was also observed in mean GPx activity in D group when compared to C group (C: 67.70 ± 49.78 vs. D 84.63 ± 49.10 nmoles/min/ml;) although without statistical significance (p = 0.28); (Fig. 2a).
A significant increase in SOD activity was observed in both treated groups versus not treated ones. B group showed significantly higher activity when compared to A group (A: 8.26 ± 3.85 vs. B 13.38 ± 1.33 UI/ml; p < 0.001) as well as D group showed higher SOD levels compared to C (C: 10.26 ± 3.31 vs. D 12.55 ± 1.88 UI/ml; p = 0.011); (Fig. 2b).
Effect on MDA
MDA concentration was significantly reduced into B group compared to A (control) (A: 25.21 ± 5.22 vs. B: 18.33 ± 6.79 nmoles/min/ml; p = 0.002), while comparison between C and D did not reach statistical significance (C: 24.81 ± 6.47 vs. D: 21.96 ± 3.02 nmoles/min/ml; p = 0.11) (Fig. 2c).
Effect on MPO
The analysis of this oxidative damage marker showed a statistically significant reduction of its concentration in B versus A group (A: 3.14 ± 2.80 vs. Controls: 1.74 ± 0.40 UI/mg: p = 0.02).
The comparison between C and D groups confirms the protective role of HATA pre-treatment in reducing the levels of MPO (C: 2.57 ± 0.13 vs. D: 1.67 ± 0.95 UI/mg: p = 0.0027); (Fig. 2d).
Histopathological changes
Histology showed the presence of ischemic parenchymal damage in all the examined sections. Incidence of histological tubular abnormalities and comparison between groups are reported in Table 2. Histology revealed a significantly lower rate of intratubular cast formation and luminal congestion in Group D versus Group C (p = 0.02 and p = 0.008).
In particular, tubular obstruction was significantly worse in non-treated rats in the non-nephrectomized groups (Group A vs. Group B p = 0.008), while there were no significant differences between treated and non-treated in the nephrectomized groups (Group C vs. Group D p = 0.71).
Finally, the rate of hyaline casts in the distal convoluted tubule was significantly higher into group D when compared to animals of Group C; (C vs. D groups p = 0.02).
There were no statistically significant differences in terms of ischemic damage between others study groups.
Discussion
Renal ischemia/reperfusion injury is an unavoidable and multifactorial event in transplantation. While cold ischemia causes serious deterioration of the balance between supply and metabolic demands, leading to tissue hypoxia, restoration of blood flow and tissue oxygenation leads to an exacerbation of cell damage and an important inflammatory response. Oxidative stress is caused by the imbalance between reactive oxygen species (ROS) and endogenous antioxidant forces: The endothelium is activated by reactive oxygen species and inflammatory cytokines, and then, adhesion molecules induce the adherence and activation of platelets to the epithelium. Finally, leukocytes, initially neutrophils then monocytes and macrophages, infiltrate into the affected tissue.
Ischemia reperfusion injury during transplantation is the major cause of renal transplant dysfunction, and it causes an oxidative burst that triggers inflammation and tubular cell injury [23, 24]. Increasing oxidative stress and inflammation may promote additional damage to the kidney, as well as additional damage to tissues, resulting in the development or progression of concomitant disease, for example, free radicals, along with inflammation, account for many of the symptoms of uremic syndrome [25]. Decreasing ROS after successful kidney transplantation results in breaking the vicious cycle of cell damage, inflammation and organ damage. Moreover, Fonseca et al. have shown how the reduction in oxidative stress markers can be used as a prognostic factor after kidney transplantation [26], similarly La Manna et al. confirmed that low levels of oxidation and apoptosis at 6 months after transplantation correlate with a better recovery of renal function in kidney allografts [27].
The discovery of the pathogenic mechanisms and of the key molecules involved in I/R injury was used to test other molecules that would act selectively on specific processes or target molecules [28]. Unfortunately, most methods that were sometimes effective in reducing oxidative stress, inflammation or apoptosis, in vivo or in vitro, have not proved to be effective in preventing or reducing functional damage; this may well get along with the hypothesis that I/R injury acts on several pathways, which is why the focus has recently been directed toward molecules with pleiotropic action such as statins.
Statins, besides their well-known cholesterol-lowering activity, have proved to have dose-dependent pleiotropic effects. These include modulation of endothelial function, reduction of oxidative stress and anti-inflammatory and immunomodulatory activities. [7,8,9,10,11,12, 29, 30]. Moreover, short-term high-dose atorvastatin pretreatment significantly improves the final thrombolysis in myocardial infarction flow grade as well as reduces the 30-day major adverse cardiac events in acute coronary syndrome patients, post-percutaneous coronary intervention regardless of cholesterol levels [11].
Previous in vivo studies, focused on ischemia reperfusion, suggested that HATA could reduce renal inflammation and apoptosis [31, 32]. Our findings support this hypothesis and the potential protective effect of high-dose statins on the pathway of I/R injury process into an isogenic transplantation rat model acting on different pathways.
Scavenger enzymes
Free radical scavengers play a determinant role in the pathogenesis of ischemia–reperfusion injury. Actually, many studies focused on the use of "scavengers” molecules, but the administration of free radical scavengers played a controversial role, as well as some sophisticated attempts to reduce I/R injury through the induction of "renoprotective" genes gave questionable results making their application in humans difficult [28].
The role of statins in the upregulation of scavenger activity is still not clear and there were substantial differences when the results of in vitro and in vivo studies were compared [30]. In a previous study Chen and coll. [33] showed that high-dose atorvastatin could upregulate the activity of glutathione peroxidase (GPx) and catalase.
Similarly, a HATA load given 24 h before induction of I/R promotes the scavenger activity of GPx [12]. In our experience, HATA, seemed to stimulate the production of endogenous scavenger enzymes, in fact, we observed an increasing activity of GPx and SOD in rats treated with high-dose atorvastatin.
Oxygen radicals
Oxygen radicals produce membrane peroxidation and MDA formation, detrimental to cellular function. Peroxidation can increase membrane permeability, whereas MDA can inactivate membrane transporters by forming intramolecular and intermolecular cross-links [34]. Actually, statins exert antioxidant effects by reducing the expression of essential NAD(P)H oxidase subunits that are the predominant source of reactive oxygen species in the vessel wall [30]. Previous studies have demonstrated the effect of statins on MDA and in reducing oxidative stress decreasing ROS [35], while some studies have shown the ability of atorvastatin, more than other statins, to reduce the levels of circulating oxidized low-density lipoprotein or of circulating MDA [36]. In our study, we observed a significant reduction in oxidative stress, also evidenced by a decrease in MDA levels in HATA-treated animals.
I/R injury can be also considered an immediate nonspecific inflammatory response and MPO levels reflect the I/R-related ROS and inflammation-mediated damage. MPO is an enzyme of the oxide-reductase group contained in polymorphonuclear leukocytes, involved in activating white blood cell response and a powerful effector of oxidative cascade exerted by the radical species production.
Some studies have shown that HATA causes a comparable significant reduction in the levels of oxidation products generated by MPO and Nitric Oxide-derived oxidants [29] and have suggested that statins could suppress MPO expression down regulating myeloperoxidase gene expression in macrophages [8].
In particular, our previous study [12] and the present results suggest that HATA decreases significantly MPO activity. This action probably has a multifactorial origin: High-dose atorvastatin could directly down-regulate MPO gene transcription but could also have indirect effects on inflammation by reducing leucocyte activation and acting on the downregulation of antigen presentation, finally causing an upstream reduction in the oxidative processes [10, 34].
Tubular abnormalities
Several studies have demonstrated that tubular damages are strongly related to kidney function, also, some of these studies have shown that hyaline casts formation occurs during the first 48 h in ischemia reperfusion model, so, hyaline casts in the convoluted distal tubules represent one of the first signs of damage [37, 38].
Histology showed a lower rate of tubular abnormalities (tubular obstruction and hyaline casts) among nephrectomized animals treated with HATA, as compared with nephrectomized controls, supporting the hypothesis that pre-treatment with high dose statins could reduce the degree of tubular necrosis and could play a more important role on inflammation as shown in our previous study [12] on MPO activity and on lymphocytes’ infiltration in ischemic tissue.
Similar results were obtained in previous studies in the setting of I/R in the myocardium [39, 40], in which short-term treatment with statins improved myocardial function by reducing the size of an infarct.
Other than these differences (Table 2), we did not find any significant histological difference among the different groups either treated or non-treated. This might be explained by too short ischemia times or too short time between transplantation and tissue sampling, or also with relatively small sample size. The same discrepancy between biochemical and histological findings were observed in our previous study [12].
Finally, one more debated issue are the possible barriers to use the atorvastatin in patients affected by chronic kidney disease regardless of dialysis status and among the human recipients of kidney transplantation. Even if, the role of statins in chronic kidney disease has been extensively evaluated, its role remains debated in specific population of patients affected by chronic kidney disease in particular dialysis-dependent. The decline in renal function of patients with chronic kidney disease is often accompanied by the increase in incidence of cardiovascular disease due to the higher prevalence of dyslipidemia and atherosclerosis and several studies have demonstrated the reduction of mortality also in patients with chronic kidney disease. Moreover, in this setting of dialysis-dependent with chronic kidney disease patients, some studies have already demonstrated [41] that statins were associated with lower mortality, regardless of dialysis status or other risk factors. Consequently, the use of statins should be encouraged in these patients over the value of cholesterol-lowering activity. Furthermore, the administration for short periods of high-dose atorvastatin among the human recipients of kidney transplantation should not be considered a true obstacle considering the potential benefic action of pleiotropic effects against the oxidative stress.
Limitation and strengths: Our study has several strengths; the main value of the study is the design itself. It is focused, for the first time, on the pleiotropic effects of statin for both oxidative stress and inflammation damage after transplantation, moreover the present study tests the efficacy of treatment by biochemical and histopathological essays, giving the more clarity to the effects of treatment. It also adds that the model is reproducible in a live animal transplant setting, and therefore, it is a step forward the application in human beings. As with strengths, the study suffers of some limitations, in particular, it lacks of data about renal function, the study was designed as acute experiment focused on oxidative stress and inflammation and the model did not provide functional outcomes. Unfortunately, changes at the molecular level of the kidney tissue occur even before nitrogenous substances, such as creatinine and urea, start to accumulate in the blood and this problem has bring us and other authors before us, to dose the markers of oxidative stress and inflammation as surrogate and early parameters of kidney damage [42]. Another point of weakness of the study is the limited duration of renal cold storage. It was brief (60 min), according with veterinary indication, but, perhaps, a longer time of cold storage of the graft should be more correct and could have amplified the effects of tests. In conclusion, a significant issue that has impacted this field of research pertains to the inconsistency between preclinical and animal studies, which have shown efficacy, and the lack of confirmation of these findings in human models and clinical trials [43,44,45]. This phenomenon has been observed across various domains of medical research, including investigations involving high doses of statins. The underlying reasons for this divergence remain elusive, possibly stemming from challenges associated with replicating animal models within the intricate human biological system, particularly when dealing with molecules like statins that exhibit pleiotropic effects.
Conclusions
Our study confirmed a protective effect of high-dose atorvastatin on oxidative stress and inflammation in a rat kidney model of isogenic transplantation. High-dose atorvastatin attenuates the ischemia/reperfusion injury reducing oxidative stress reducing both ROS production and inflammation while increasing scavenger activities.
High-dose atorvastatin pre-treatment may play a role in modulating renal impairment following transplantation surgery, allowing earlier recovery from IR injury and an overall reduction of delayed graft function.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, [GC], upon reasonable request.
Abbreviations
- HATA:
-
High-dose atorvastatin
- MDA:
-
Malondialdehyde
- SOD:
-
Superoxide dismutase
- GPx:
-
Glutathione peroxidase
- MPO:
-
Myeloperoxidase
- I/R:
-
Ischemia/reperfusion
References
Nankivell BJ, Alexander S. Rejection of the kidney allograft. N Engl J Med. 2010;363:1451–62.
Li C, Jackson RM. Reactive species mechanisms of cellular hypoxia-reoxygenation injury. Am J Physiol Cell Physiol. 2002;282:227–41.
Kosieradzki M, Rowinski W. Ischemia/reperfusion injury in kidney transplantation: mechanisms and prevention. Transplant Procee. 2008;40:3279–88.
Hearse DJ, Humphrey SM, Chain EB. Abrupt reoxygenation of the anoxic potassium-arrested perfused rat heart: a study of myocardial enzyme release. J Mol Cell Cardiol. 1973;5:395–407.
Dhillon N, et al. Donor Toll-like receptor 4 contributes to ischemia and reperfusion injury following human kidney transplantation. Proc Natl Acad Sci U S A. 2009;106:3390–5.
Yellon DM, Hausenloy DJ. Myocardial reperfusion injury. N Engl J Med. 2007;357:1121–35.
Mach F. Statins as immunomodulatory agents. Circulation. 2004;109:II15-17.
Kumar AP, Reynolds WF. Statins downregulate myeloperoxidase gene expression in macrophages. Biochem Biophys Res Comm. 2005;331:442–51.
Smaldone C, Brugaletta S, Pazzano V, et al. Immunomodulator activity of 3-hydroxy-3-methilglutaryl-CoA inhibitors. Cardiovasc Hematol Agents Med Chem. 2009;7:279–94.
Sadeghi MM, Tiglio A, Sadigh K, et al. Inhibition of interferon-gamma-mediated microvascular endothelial cell major histocompatibility complex class II gene activation by HMG-CoA reductase inhibitors. Transplantation. 2001;71:1262–8.
Liu Y, Su Q, Li L. Efficacy of short-term high-dose atorvastatin pretreatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention: a meta-analysis of nine randomized controlled trials. Clin Cardiol. 2013;36:41–8.
Cusumano G, Romagnoli J, Liuzzo G, et al. N-acetylcysteine and high-dose atorvastatin reduce oxidative stress in an ischemia-reperfusion model in the rat kidney. Transplant Proc. 2015;47:2757–62.
Raphael J, Collins SR, Wang XQ, et al. Perioperative statin use is associated with decreased incidence of primary graft dysfunction after lung transplantation. J Heart Lung Transplant. 2017;36:948–56.
Tuuminen R, Nykänen AI, Saharinen P, et al. Donor simvastatin treatment prevents ischemia-reperfusion and acute kidney injury by preserving microvascular barrier function. Am J Transplant. 2013;13:2019–34.
Italian Guidelines for Animal Research. http://www.gazzettaufficiale.it/eli/id/2014/03/14/14G00036/sg
Directive 2010/63/EU of the European Parliament and of the Council of 22 September 2010 on the protection of animals used for scientific purposes: http://eurlex.europa.eu/legalcontent/EN/TXT/?uri=CELEX:32010L0063
Aufhauser DD Jr, Wang Z, Murken DR, et al. Improved renal ischemia tolerance in females influences kidney transplantation outcomes. J Clin Invest. 2016;126(5):1968–77.
Jang HR, Rabb H. Immune cells in experimental acute kidney injury. Nat Rev Nephrol. 2015;11(2):88–101.
Jiang H, Zheng H. Efficacy and adverse reaction to different doses of atorvastatin in the treatment of type II diabetes mellitus. Biosci Rep. 2019;39(7):BSR20182371.
Nasri H, Hasanpour Z, Nematbakhsh M, et al. The effect of the various doses of atorvastatin on renal tubular cells, an experimental study. J Nephropathol. 2016;3:111–5.
Kim J, Jang HS, Park KM. Reactive oxygen species generated by renal ischemia and reperfusion trigger protection against subsequent renal ischemia and reperfusion injury in mice. Am J Physiol Renal Physiol. 2010;298:158–66.
Racusen LC, Halloran PF, Solez K. Banff 2003 meeting report: new diagnostic insights and standards. Am J Transplant. 2004;4:1562–6.
Tennankore K, Kim S, Alwayn I, et al. Prolonged warm ischemia time is associated with graft failure and mortality after kidney transplantation. Kidney Int. 2016;89:648–58.
Kumar A, Shalmanova L, Hammad A, et al. Induction of IL-8(CXCL8) and MCP-1(CCL2) with oxidative stress and its inhibition with N-acetyl cysteine (NAC) in cell culture model using HK-2 cell. Transpl Immunol. 2016;35:40–6.
Tucker PS, Scanlan AT, Dalbo VJ. Chronic kidney disease influences multiple systems: describing the relationship between oxidative stress, inflammation, kidney damage, and concomitant disease. Oxid Med Cell Longev. 2015;2015:80635.
Fonseca I, Reguengo H, Almeida M, et al. Oxidative stress in kidney transplantation: malondialdehyde is an early predictive marker of graft dysfunction. Transplantation. 2014;97:1058–65.
La Manna G, Lanci N, Della BE, et al. Reduction of oxidative damage reflects a better kidney transplantation outcome. Am J Nephrol. 2011;34:496–504.
Salvadori M, Rosso G, Bertoni E, et al. Update on ischemia-reperfusion injury in kidney transplantation: pathogenesis and treatment. World J Transplant. 2015;5:52–67.
Shishehbor MH, Brennan ML, Aviles RJ, et al. Statins promote potent systemic antioxidant effects through specific inflammatory pathways. Circulation. 2003;108:426–31.
Wassmann S, Laufs U, Müller K. Cellular antioxidant effects of atorvastatin in vitro and in vivo. Arterioscler Thromb Vasc Biol. 2002;22:300–5.
Bonnet J, McPherson R, Tedgui A, et al. CAP Investigators. Comparative effects of 10-mg versus 80-mg Atorvastatin on high-sensitivity C-reactive protein in patients with stable coronary artery disease: results of the CAP (Comparative Atorvastatin Pleiotropic effects) study. Clin Ther. 2008;12:2298–313.
Gueler F, Rong S, Park JK, et al. Postischemic acute renal failure is reduced by short-term statin treatment in a rat model. J Am Soc Nephrol. 2002;13:2288–98.
Chen J, Liu B, Yuan J, et al. Atorvastatin reduces vascular endothelial growth factor (VEGF) expression in human non-small cell lung carcinomas (NSCLCs) via inhibition of reactive oxygen species (ROS) production. Mol Oncol. 2012;1:62–72.
Kramer JH, Mak IT, Weglicki WB. Differential sensitivity of canine cardiac sarcolemmal and microsomal enzymes to inhibition by free radical-induced lipid peroxidation. Circ Res. 1984;55:120–4.
Sasaki S, Kuwahara N, Kunitomo K. Effects of atorvastatin on oxidized low-density lipoprotein, low-density lipoprotein subfraction distribution, and remnant lipoprotein in patients with mixed hyperlipoproteinemia. Am J Cardiol. 2002;89:386–9.
Jones P, Kafonek S, Laurora I, et al. Comparative dose efficacy study of atorvastatin versus simvastatin, pravastatin, lovastatin, and fluvastatin in patients with hypercholesterolemia (The CURVES study). Am J Cardiol. 1998;81:582–7.
Hassan SS, Rizk A, Thomann C, et al. Preconditioning with atorvastatin against renal ischemia-reperfusion injury in nondiabetic versus diabetic rats. Can J Physiol Pharmacol. 2019;97(1):1–14.
Bastos AP, Piontek K, Silva AM, Martini D, et al. Pkd1 haploinsufficiency increases renal damage and induces microcyst formation following ischemia/reperfusion. J Am Soc Nephrol. 2009;20(11):2389–402.
Mensah K, Mocanu MM, Yellon DM. Failure to protect the myocardium against ischemia/reperfusion injury after chronic atorvastatin treatment is recaptured by acute atorvastatin treatment: a potential role for phosphatase and tensin homolog deleted on chromosome ten? J Am Coll Cardiol. 2005;45:1287–91.
Bell RM, Yellon DM. Atorvastatin, administered at the onset of reperfusion, and independent of lipid lowering, protects the myocardium by up-regulating a pro-survival pathway. J Am Coll Cardiol. 2003;41:508–15.
Kim JE, Choi YJ, Oh SW, et al. The effect of statins on mortality of patients with chronic kidney disease based on data of the observational medical outcomes partnership common data model (OMOP-CDM) and Korea National Health Insurance Claims Database. Front Nephrol. 2022;1:821585.
Gyurászová M, Gurecká R, Bábíčková J, et al. Oxidative stress in the pathophysiology of kidney disease: implications for noninvasive monitoring and identification of biomarkers. Oxid Med Cell Longev. 2020;23(2020):5478708.
Badimon L, Mendieta G, Vilahur. Statins revisited: therapeutic applications beyond lipid lowering? Eur Heart J. 2023;44(25):2332–4.
Liakopoulos OJ, Kuhn EW, Hellmich M, et al. Statin loading before coronary artery bypass grafting: a randomized trial. Eur Heart J. 2023;44(25):2322–31.
Elgendy IY, Mahmoud AN, Bavry AA. Perioperative rosuvastatin in cardiac surgery. N Engl J Med. 2016;375(9):901.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
GC, JR designed research, performed research, collected data, analyzed data, and wrote the article. EC performed research, collected data, and analyzed data. SG designed research and wrote the paper. AS performed laboratory research. GV ES contributed to histopathological research and analyzed data. MEC supervised animal’s research. FC, FC designed research and revised article.
Corresponding author
Ethics declarations
Ethics approval and consent for publication
Animal Care Ethical Committee in accordance with the current Italian Animals Protection Law (from the National Institute of Health) [15] and the current principles of the laboratory animal care of the European Union [16]. All authors give the consent to publication.
Competing interests
The authors of this manuscript have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cusumano, G., Cola, E., Spagnoletti, G. et al. High-dose atorvastatin reduces oxidative stress of ischemia/reperfusion injury after isogeneic kidney transplantation in rats: in vivo, preclinical, case–control, open-label study. Ren Replace Ther 9, 57 (2023). https://doi.org/10.1186/s41100-023-00508-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-023-00508-w