Abstract
Background
Chronic kidney disease (CKD) is frequently associated with renal anemia. Erythropoiesis-stimulating agent-hyporesponsive anemia is often caused by iron deficiency in patients with CKD. We hypothesized that high accumulation of indoxyl sulfate, a uremic toxin, accelerates iron deficiency in patients with CKD. The aim of this study was to clarify whether the accumulation of indoxyl sulfate is a cause of iron deficiency in patients with CKD. Therefore, we investigated the association between serum indoxyl sulfate concentration and iron dynamics in patients with end-stage kidney disease (ESKD).
Methods
We performed a cross-sectional study on 37 non-dialyzed patients with ESKD, who were hospitalized to undergo maintenance hemodialysis treatment at Shirasagi Hospital. Serum indoxyl sulfate concentration, iron dynamics parameters and other laboratory data were measured immediately before the initiation of hemodialysis treatment. Clinical characteristics were obtained from electronic medical records.
Results
The estimated glomerular filtration rate (eGFR) of 37 patients with ESKD was 5.08 (3.78–7.97) mL/min/1.73 m2 (median [range]). Serum ferritin and transferrin saturation (TSAT) were 90 (10–419) ng/mL and 20 (8–59)% (median [range]), respectively. Serum indoxyl sulfate concentration was 62 (11–182) μM (median [range]). Serum indoxyl sulfate concentration was inversely correlated with serum ferritin level (ρ = − 0.422, p = 0.011), but not with TSAT, age, gender, eGFR and c-reactive protein (CRP) in 37 patients. In eight patients taking iron-containing agents, serum indoxyl sulfate concentration was strongly correlated with serum ferritin level (ρ = − 0.796, p = 0.037); however, in 29 patients not taking an iron-containing agent, this correlation was not observed (ρ = − 0.336, p = 0.076). In the multivariate analysis including age, gender, eGFR and CRP, the correlation between serum indoxyl sulfate concentration tended to be, but not significantly correlated with serum ferritin level in 37 patients (regression coefficient = − 54.343, p = 0.137).
Conclusion
Our study suggests that serum accumulation of indoxyl sulfate is one of causes not to increase serum ferritin level in patients with ESKD taking an iron-containing agent. Further clinical study is needed to reveal the appreciable relationship between serum ferritin and serum indoxyl sulfate.
Similar content being viewed by others
Background
The production of erythropoietin, a hematopoietic hormone produced in the kidney, is decreased in patients with chronic kidney disease (CKD) [1]; therefore, CKD is frequently complicated by renal anemia. It is well known that renal anemia is a risk factor for all-cause mortality [2], cardiovascular disease [3] and CKD progression [4]. Congestive heart failure, CKD and anemia are known to exacerbate each other, and the triangular relationship is called cardio-renal anemia (CRA) syndrome [5]. In addition, Malyszko et al. reported that severe CRA syndrome was an independent predictor of death in patients with peritoneal dialysis [6]. Therefore, the therapeutic management of anemia is one of the important factors for avoiding the poor outcome in CKD patients. However, recently, it has been pointed out that erythropoiesis-stimulating agent (ESA)-hyporesponsive anemia is a frequent complication in patients with CKD. Several studies have reported that hyporesponsiveness to ESA leads to increased all-cause mortality in hemodialysis patients [7] and subsequent risk of death or cardiovascular events in patients with CKD with type 2 diabetes mellitus not undergoing dialysis [8]. Therefore, it is likely that clarifying the therapeutic approach toward ESA-hyporesponsive anemia leads patients with CKD to have a good prognosis.
Renal anemia is induced not only by a decrease in the production of erythropoietin, but also by iron deficiency in patients with CKD. It has been reported that the expression of hepcidin, an iron regulatory peptide, increases with the progression of CKD [9]. Hepcidin decreases the expression of ferroportin, suppresses intestinal absorption of iron and its release from various tissues [10] and induces functional iron deficiency. Iron deficiency causes hyporesponsiveness of ESA in patients with CKD; therefore, elucidating the mechanism of iron deficiency in patients with CKD can improve medication for renal anemia.
In patients with CKD, various uremic toxins accumulate with the progression of CKD. Because indoxyl sulfate, a metabolite of tryptophan derived from dietary protein, has a high plasma protein-binding affinity, indoxyl sulfate accumulates as kidney function deteriorates and remains accumulated after the initiation of dialysis [11]. The accumulation of indoxyl sulfate causes further progression of CKD [12], cardiovascular events [13] and microvascular damage [14] in patients with CKD. In addition, it has been reported that indoxyl sulfate stimulates cellular inflammation and increases the expression of inflammatory cytokines, such as interleukin-6 (IL-6) [15]; IL-6 induces hepcidin expression [16]. However, the effects of indoxyl sulfate accumulation on iron dynamics remain unclear in clinical settings.
The aim of this study was to clarify whether the accumulation of indoxyl sulfate induces iron deficiency in patients with CKD, and to investigate the relationship between serum indoxyl sulfate concentration and iron dynamics index in patients with end-stage kidney disease (ESKD).
Methods
Patients and study design
This study was a single-center, cross-sectional study. We enrolled 37 non-dialyzed patients with ESKD, who were hospitalized for maintenance hemodialysis at Shirasagi Hospital (Osaka, Japan) and have obtained written informed consent for participation in this study between February 1, 2015, and May 31, 2016. The exclusion criteria were active malignancy, infection and urgent initiation of hemodialysis for treatment of unstable conditions, such as acute kidney injury and acute fluid retention.
Data collection
Demographic and clinical characteristics including age, sex, body mass index, cause of ESKD, incidence of complications, laboratory data and drug prescriptions were obtained from electronic medical records maintained at Shirasagi Hospital. The estimated glomerular filtration rate (eGFR) was calculated using the formula proposed by Matsuo et al.: eGFR = 194 × (serum creatinine)−1.094 × age−0.287 × 0.739 (if female) [17].
Measurement of serum indoxyl sulfate concentrations
The blood sample was obtained from the blood removal side of the dialysis fluid circuit prior to the start of the first hemodialysis session. The sample was immediately centrifuged at 1500 × g for 5 min, and the serum obtained was stored at − 70 °C until analysis.
Serum indoxyl sulfate concentrations were quantified using high-performance liquid chromatography (HPLC)-fluorescence methods. The standard curve for HPLC analysis of serum indoxyl sulfate was prepared by using potassium indoxyl sulfate purchased from Nacalai Tesque Inc. (Kyoto, Japan). Methanol (150 µL) was added to a 30-µL serum sample and mixed at 300 strokes per minute for 10 min. The mixture was centrifuged at 1630 × g for 30 min, and the resulting supernatant was evaporated to dryness under a stream of nitrogen gas (N2) at 50 °C. The dried residue was then dissolved in the mobile phase (20 mM phosphate buffer [pH 4.0] containing 10 mM tetra-butyl-ammonium iodide:acetonitrile, 78:22 [v/v]) and injected into the HPLC system (LC-10-AS series; Shimadzu, Kyoto, Japan) utilizing an Inertsil C-8 column (dimensions, 4.6 mm × 250 mm; particle size, 5 µm; column temperature, 35 °C; GL Sciences, Tokyo, Japan) to quantify indoxyl sulfate. The analytical conditions for indoxyl sulfate were as follows: flow rate, 1.5 mL/min; column temperature, 35 °C; excitation, 280 nm; and emission, 330 nm. The limit of quantification for serum indoxyl sulfate was 0.3 µM in this study.
Statistical analyses
The normality of distribution was examined using a Shapiro–Wilk test. Data with normal distributions are presented as mean ± standard deviation, while those with non-normal distributions are presented as medians with ranges. The Student’s t test, Chi-square test or nonparametric Mann–Whitney's U test was used to compare differences between groups of lower and higher serum indoxyl sulfate concentrations. Correlations between single variables were examined using a Spearman rank correlation test. Univariate and stepwise multiple linear regression analysis was used to examine the association between serum ferritin level and serum indoxyl sulfate concentration. Data with non-normal distributions were log-transformed in multiple linear regression analysis. All the statistical analyses were performed with EZR, which is a modified version of R commander, equipped with statistical functions for medical statistics [18].
Results
Patient demographics and clinical characteristics
The demographics and clinical characteristics of all the 37 patients with ESKD are shown in Table 1. Male of the patients accounted for 76% (M/F, 28/9) of the patients. The average age of the patients was 69 ± 12 years. The average serum creatinine level and eGFR of all the patients were 8.62 ± 1.47 mg/dL and 5.08 (3.78–7.97) mL/min/1.73 m2, respectively. Eight patients had received an iron-containing agent treatment. Thirty-three patients received an ESA treatment.
To analyze the effect of indoxyl sulfate, we divided the patients into two groups based on the median serum concentration of indoxyl sulfate (62 μM)—the high concentration group (indoxyl sulfate > 62 μM) and the low concentration group (indoxyl sulfate ≤ 62 μM). The details of demographics and clinical characteristics of each group are listed in Table 1. Serum creatinine was significantly higher in the high concentration group than in the low concentration group; however, there was no statistically significant difference in the eGFR between the two groups. Serum ferritin level was significantly lower in the high concentration group than in the low concentration group.
Correlation between serum ferritin level and serum indoxyl sulfate concentration in patients with ESKD
The correlation between serum ferritin level and serum indoxyl sulfate concentration is shown in Fig. 1. In all the 37 patients, serum ferritin level was significantly negatively correlated with serum indoxyl sulfate concentration (ρ = − 0.422, p = 0.011, Fig. 1A). In 29 patients not taking an iron-containing agent, serum ferritin level was not correlated with serum indoxyl sulfate concentration (ρ = − 0.336, p = 0.076, Fig. 1B). However, in the eight patients taking iron-containing agents, serum ferritin level was strongly negatively correlated with serum indoxyl sulfate concentration (ρ = − 0.786, p = 0.037, Fig. 1C).
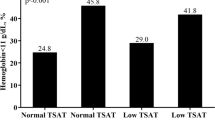
Correlation between TSAT level and serum indoxyl sulfate concentration in patients with ESKD
The correlation between TSAT level and serum indoxyl sulfate concentration is shown in Fig. 2. TSAT level was not significantly correlated with serum indoxyl sulfate concentration in all the 37 patients (ρ = − 0.177, p = 0.289, Fig. 2A). In the subgroup analysis, TSAT level was not correlated with serum indoxyl sulfate concentration in 29 patients not taking iron-containing agent (ρ = − 0.092, p = 0.617, Fig. 2B) and in 8 patients taking iron-containing agents ((ρ = − 0.476, p = 0.208, Fig. 2C).
Linear regression analysis between serum ferritin level and serum indoxyl sulfate concentration
The result of univariate and multivariate linear regression analysis between serum ferritin level and some factors is shown in Table 2. Multivariate linear regression analysis showed that serum ferritin level tended to be, but not significant correlated with serum indoxyl sulfate concentration (regression coefficient = − 54.343, p = 0.137), after adjustment for age, gender, eGFR, albumin, alanine aminotransferase and CRP.
Discussion
In this clinical study, we found the possibility that serum indoxyl sulfate concentration was negatively correlated with serum ferritin level in patients with ESKD, particularly in patients taking iron-containing agent (Fig. 1). Unfortunately, the association between serum ferritin and serum indoxyl sulfate proven in a nonparametric correlation analysis disappeared after adjusting for other confounding factors in multivariate analysis (Table 2). Iron dynamics and accumulation of indoxyl sulfate may be associated with various factors such as residual kidney function and inflammation; therefore, it is thought that our study had a small sample size to explain multiple factors. Further clinical study can reveal the appreciable relationship between serum ferritin and serum indoxyl sulfate.
Our study indicated serum indoxyl sulfate concentration was not associated with CRP (Table 2). However, Kaminski et al. have reported that serum indoxyl sulfate concentration is correlated with inflammatory markers, such as high sensitive CRP and TNF-α in patients with various chronic kidney disease stage [19]. We excluded patients complicated active malignancy and infection and included patients with ESKD only in this study. That is, it is thought that the difference in these results is based on the difference in the patients’ population. Therefore, there may be no correlation between serum indoxyl sulfate concentration and CRP in ESKD patients.
It has been reported previously that ESA treatment decreases serum ferritin level via inhibition of hepcidin synthesis [20]. In this study, 89% of the patients received ESA treatment (Table 1). Therefore, it is thought that the correlation between serum ferritin level and serum indoxyl sulfate concentration, which we observed in our study, may be not related to the ESA treatment. However, a plausible explanation for our results could be that indoxyl sulfate increases the expression of hepcidin, a key negative regulator of iron [21], which in turn inhibits the transportation of iron from intestinal epithelial cells to blood and iron release from various macrophages via ferroportin [22]. Therefore, it is likely that the accumulation of indoxyl sulfate induces iron deficiency in patients with ESKD.
In a subgroup analysis of patients taking an iron-containing agent, the serum concentration of indoxyl sulfate was strongly negatively correlated with serum ferritin level (Fig. 1C). Therefore, it is likely that the intestinal absorption of iron is strongly suppressed in patients with CKD and high serum indoxyl sulfate concentrations. Duodenal cytochrome b (Dcytb), ferric reductase and divalent metal transporter (DMT1), an uptake transporter of iron on the apical surface of duodenal enterocytes, play an important role in intestinal iron absorption. It has been reported that the expression of both DMT1 and Dcytb is induced by hypoxia-inducible factor (HIF), a transcription factor stabilized under hypoxic conditions [23, 24]. Interestingly, Asai et al. reported that indoxyl sulfate decreases HIF activity [25]. Therefore, it is likely that the accumulation of indoxyl sulfate suppresses the absorption of iron in the intestine of patients with ESKD.
Iron deficiency with low TSAT and normal or high serum ferritin level is called functional iron deficiency. Patients with CKD frequently suffer from functional iron deficiency. Maryszko et al. reported that 23% of patients with chronic hemodialysis was complicated by functional iron deficiency, and patients with functional iron deficiency had high levels of IL-6, CRP, hepcidin and N-terminal pro-B-type natriuretic peptide levels and low levels of TSAT in comparison with patients with non-functional iron deficiency [26]. Awan et al. reported that among non-dialysis-dependent patients with CKD and anemia, 30% had absolute iron deficiency (TSAT ≦ 20%, ferritin < 100 ng/mL) and 19% had functional iron deficiency (TSAT ≦ 20%, ferritin 100–500 ng/mL) [27]. Our study is shown that high concentration of indoxyl sulfate does not always induce functional iron deficiency represented by high ferritin (Fig. 1) and low TSAT (Fig. 2). On the other hand, various reports show that some inflammatory markers such as IL-6 and CRP are elevated in hemodialysis patients with functional iron deficiency [26], and serum indoxyl sulfate concentration is also associated with elevated inflammatory markers [15, 19]. That is to say, these reports indicate that high concentration of indoxyl sulfate may induce functional iron deficiency via chronic inflammation. The discrepancy between this hypothesis and our results may be explained by the fact that our study included small number of only ESKD patients just prior to the introduction of hemodialysis. Because maintenance hemodialysis patients are assumed to have higher serum indoxyl sulfate concentration [11] and chronic inflammation [26], larger studies including maintenance hemodialysis patients would clarify the relationship between indoxyl sulfate and functional iron deficiency.
Our study suggests that the accumulation of indoxyl sulfate is at least partially associated with the iron deficiency in patients with CKD. Wu et al. [28] reported that continuous administration of the oral adsorbent AST-120 can decrease serum indoxyl sulfate concentration and increase the ratio of achieving hemoglobin level > 11 g/dL by continuous administration of erythropoietin receptor activator. In addition, Hamano et al. [21] reported that AST-120 ameliorated the increase in serum hepcidin levels in adenine-induced CKD mice. On the other hand, it has been reported that AST-120 adsorbs various uremic toxins other than indoxyl sulfate, such as p-cresyl sulfate [29]. Therefore, it is possible that the measurement of serum concentrations of these uremic toxins, such as indoxyl sulfate, and the administration of AST-120 could be a new strategy for intractable iron deficiency in patients with CKD.
Our study has some limitations. First, the sample size was small, and we could not show the exact association between serum indoxyl sulfate concentration and serum ferritin level with multiple regression analysis. In addition, we could not control the amount and quality of diet of the patients before enrollment, which could have influenced the serum indoxyl sulfate concentration in each patient as indoxyl sulfate is derived from protein (tryptophan) in the diet [30].
Conclusion
Our study suggests that serum accumulation of indoxyl sulfate is one of causes decreasing serum ferritin level in patients with ESKD taking an iron-containing agent. Further clinical study is needed to reveal the appreciable relationship between indoxyl sulfate serum ferritin and serum indoxyl sulfate.
Availability of data and materials
All datasets analyzed in this study are referenced in the manuscript.
Abbreviations
- AST:
-
Aspartate aminotransferase
- CKD:
-
Chronic kidney disease
- CRA:
-
Cardio-renal anemia
- CRP:
-
C-reactive protein
- Dcytb:
-
Duodenal cytochrome b
- DMT1:
-
Divalent metal transporter
- eGFR:
-
Estimated glomerular filtration rate
- ESA:
-
Erythropoiesis-stimulating agent
- ESKD:
-
End-stage kidney disease
- HIF:
-
Hypoxia-inducible factor
- HPLC:
-
High-performance liquid chromatography
- IL-6:
-
Interleukin-6
- TSAT:
-
Transferrin saturation
References
Astor BC, Muntner P, Levin A, Eustace JA, Coresh J. Association of kidney function with anemia: the Third National Health and Nutrition Examination Survey (1988–1994). Arch Intern Med. 2002;162(12):1401–8.
Vlagopoulos PT, Tighiouart H, Weiner DE, Griffith J, Pettitt D, Salem DN, et al. Anemia as a risk factor for cardiovascular disease and all-cause mortality in diabetes: the impact of chronic kidney disease. J Am Soc Nephrol. 2005;16(11):3403–10.
Ahmad AA, Rand WM, Manjunath G, Konstam MA, Salem DN, Levey AS, et al. Reduced kidney function and anemia as risk factors for mortality in patients with left ventricular dysfunction. J Am Coll Cardiol. 2001;38(4):955–62.
Yi SW, Moon SJ, Yi JJ. Low-normal hemoglobin levels and anemia are associated with increased risk of end-stage renal disease in general populations: a prospective cohort study. PLoS ONE. 2019;14(4):e0215920.
Silverberg DS, Wexler D, Blum B, Iaina A. Anemia in chronic kidney disease and congestive heart failure. Blood Purif. 2003;21(1):124–30.
Malyszko J, Zbroch E, Malyszko J, Mysliwiec M, Iaina A. The cardio-renal-anaemia syndrome predicts survival in peritoneally dialyzed patients. Arch Med Sci. 2010;6(4):539–44.
Kilpatrick RD, Critchlow CW, Fishbane S, Besarab A, Stehman-Breen C, Krishnan M, et al. Greater epoetin alfa responsiveness is associated with improved survival in hemodialysis patients. Clin J Am Soc Nephrol. 2008;3(4):1077–83.
Solomon SD, Uno H, Lewis EF, Eckardt KU, Lin J, Burdmann ESA, Trial to Reduce Cardiovascular Events with Aranesp Therapy (TREAT) Investigators, et al. Erythropoietic response and outcomes in kidney disease and type 2 diabetes. N Engl J Med. 2010;363(12):1146–55.
Zaritsky J, Young B, Wang HJ, Westerman M, Olbina G, Nemeth E, et al. Hepcidin—a potential novel biomarker for iron status in chronic kidney disease. Clin J Am Soc Nephrol. 2009;4(6):1051–6.
Yeh K, Yeh M, Glass J. Hepcidin regulation of ferroportin 1 expression in the liver and intestine of the rat. Am J Physiol Gastrointest Liver Physiol. 2004;286(3):G385–94.
Barreto FC, Barreto DV, Liabeuf S, Meert N, Glorieux G, Temmar M, European Uremic Toxin Work Group (EUTox), et al. Serum indoxyl sulfate is associated with vascular disease and mortality in chronic kidney disease patients. Clin J Am Soc Nephrol. 2009;4(10):1551–8.
Niwa T, Ise M. Indoxyl sulfate, a circulating uremic toxin, stimulates the progression of glomerular sclerosis. J Lab Clin Med. 1994;124(1):96–104.
Cao X, Chen J, Zou J, Zhong Y, Teng J, Ji J, et al. Association of indoxyl sulfate with heart failure among patients on hemodialysis. Clin J Am Soc Nephrol. 2015;10(1):111–9.
Ryu JW, Yu M, Lee S, Ryu DR, Kim SJ, Kang DH, et al. AST-120 improves microvascular endothelial dysfunction in end-stage renal disease patients receiving hemodialysis. Yonsei Med J. 2016;57(4):942–9.
Sun C, Hsu H, Wu M. p-Cresol sulfate and indoxyl sulfate induce similar cellular inflammatory gene expressions in cultured proximal renal tubular cells. Nephrol Dial Transplant. 2013;28(1):70–8.
Zhang S, Chen Y, Guo W, Yuan L, Zhang D, Xu Y, et al. Disordered hepcidin-ferroportin signaling promotes breast cancer growth. Cell Signal. 2014;26(11):2539–50.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53(6):982–92.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Kaminski TW, Pawlak K, Karbowska M, Znorko B, Mor AL, et al. The impact of antihypertensive pharmacotherapy on interplay between protein-bound uremic toxin (indoxyl sulfate) and markers of inflammation in patients with chronic kidney disease. Int Urol Nephrol. 2019;51(3):491–502.
Akizawa T, Nangaku M, Yonekawa T, Okuda N, Kawamatsu S, et al. Efficacy and safety of daprodustat compared with darbepoetin alfa in japanese hemodialysis patients with anemia: a randomized, double-blind, phase 3 trial. Clin J Am Soc Nephrol. 2020;15(8):1155–65.
Hamano H, Ikeda Y, Watanabe H, Horinouchi Y, Izawa-Ishizawa Y, Imanishi M, et al. The uremic toxin indoxyl sulfate interferes with iron metabolism by regulating hepcidin in chronic kidney disease. Nephrol Dial Transplant. 2018;33(4):586–97.
Nemeth E, Tuttle MS, Powelson J, Vaughn MB, Donovan A, Ward DM, et al. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science. 2004;306(5704):2090–3.
Luo X, Hill M, Johnson A, Latunde-Dada GO. Modulation of Dcytb (Cybrd 1) expression and function by iron, dehydroascorbate and Hif-2α in cultured cells. Biochim Biophys Acta. 2014;1840(1):106–12.
Wang D, Wang L, Zhao Y, Lu Y, Zhu L. Hypoxia regulates the ferrous iron uptake and reactive oxygen species level via divalent metal transporter 1 (DMT1) Exon1B by hypoxia-inducible factor-1. IUBMB Life. 2010;62(8):629–36.
Asai H, Hirata J, Hirano A, Hirai K, Seki S, Watanabe-Akanuma M. Activation of aryl hydrocarbon receptor mediates suppression of hypoxia-inducible factor-dependent erythropoietin expression by indoxyl sulfate. Am J Physiol Cell Physiol. 2016;310(2):C142–50.
Małyszko J, Koc-Żórawska E, Levin-Iaina N, Małyszko J, Koźmiński P, Kobus G, et al. New parameters in iron metabolism and functional iron deficiency in patients on maintenance hemodialysis. Pol Arch Med Wewn. 2012;122(11):537–42.
Awan AA, Walther CP, Richardson PA, Shah M, Winkelmayer WC, Navaneethan SD. Prevalence, correlates and outcomes of absolute and functional iron deficiency anemia in nondialysis-dependent chronic kidney disease. Nephrol Dial Transplant. 2021;36(1):129–36.
Wu IW, Hsu KH, Sun CY, Tsai CJ, Wu MS, Lee CC. Oral adsorbent AST-120 potentiates the effect of erythropoietin-stimulating agents on Stage 5 chronic kidney disease patients: a randomized crossover study. Nephrol Dial Transplant. 2014;29(9):1719–27.
Yamamoto S, Kazama J, Omori K, Matsuo K, Takahashi Y, et al. Continuous reduction of protein-bound uraemic toxins with improved oxidative stress by using the oral charcoal adsorbent AST-120 in haemodialysis patients. Sci Rep. 2015;5:14381. https://doi.org/10.1038/srep14381.
Niwa T. Uremic toxicity of indoxyl sulfate. Nagoya J Med Sci. 2010;72(1–2):1–11.
Acknowledgements
We would like to thank nurses, medical clerks and clinical engineering technologists at Shirasagi hospital for introducing patients into this study and blood sampling from patients.
Funding
This work was supported financially in part by a grant from the Ministry of Education, Culture, Sports, Science and Technology of Japan (MEXT)-supported program for the Strategic Research Foundation at Private Universities, 2012-2016 (S1201008), and by a Grant-in-Aid for Scientific Research (C) (No. 15K08601) from the Japan Society for the Promotion of Science (JSPS) KAKENHI. The funding bodies had no role in the study design, data collection and analysis, interpretation of results, manuscript preparation or decision to publish.
Author information
Authors and Affiliations
Contributions
TY was responsible for patient enrollment, sample collection, data interpretation, statistical analyses and writing of the manuscript. MT was responsible for data interpretation, statistical analyses and writing of the manuscript. HF, YI, SK, SN, AI and AS were responsible for the measurement of indoxyl sulfate in patients with ESKD. MM, KH, RT, TO and TF were responsible for patient enrollment and sample collection. SI and TY helped draft the study design. TM and KN were responsible for writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki and was approved by the Shirasagi Hospital Ethics Committee (approval number 27-1) and Kyoto Pharmaceutical University Ethics Committee (approval number 15-1). All patients provided written informed consent prior to undergoing the necessary procedures.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yoshida, T., Tsujimoto, M., Kawakami, S. et al. Research on the relationship between serum indoxyl sulfate concentration and iron dynamics index in patients with end-stage kidney disease: a cross-sectional study. Ren Replace Ther 8, 59 (2022). https://doi.org/10.1186/s41100-022-00444-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-022-00444-1