Abstract
Since 2015, the Committee of International Communication for Academic Research of the Japanese Society for Dialysis Therapy has held a symposium every year at the society’s Annual Congress to discuss the current status of and demand for dialysis therapy in developing countries in Asia with the aim of identifying ways to contribute to the field of dialysis therapy in these countries. The 2018 symposium opened the door further, beyond Asian countries to include all non-Western countries. Two speakers from Cambodia and Japan contributed their manuscripts to the 2018 symposium issue. In Cambodia in 2017, a study of hemodialysis data from 5 centers in Phnom Penh was conducted for the first time. This study involving 407 patients (233 men [57.2%]; mean age 52 [SD, ± 15] years) revealed that hypertension was the main cause of end-stage renal disease (46.8%), followed by concomitant hypertension and diabetes mellitus (31%), with diabetes mellitus alone accounting for only 8.1% of cases. Mean frequency of hemodialysis was 7.5 (SD, ± 2.3) sessions per month. The duration of each session was 4 h. Patients in Cambodia are required to bear the full cost for hemodialysis because the country lacks a national health insurance system. From 2007 to 2018, several Japanese societies and organizations for dialysis therapy and technology carried out activities aimed at resolving problems in dialysis medical care in developing countries in East and Southeast Asia. The role of the academic societies and their activities in this region are discussed.
Similar content being viewed by others
Preface
The role of the Committee of International Communication for Academic Research of the Japanese Society for Dialysis Therapy in partnerships between Asian developing countries, non-Western countries, and Japan up to 2018
-
Toru Hyodo, Yusuke Tsukamoto, Nobuhito Hirawa, Yoshitaka Isaka, Hidetomo Nakamoto, Japan
Since 2015, the Committee of International Communication for Academic Research of the Japanese Society for Dialysis Therapy (JSDT) has held its first, second, and third Asian symposia at the society’s Annual Congress. The purpose is to discuss the current status of and demand for dialysis therapy in developing countries in Asia, to identify ways that JSDT can contribute to the field of dialysis therapy in these countries [1,2,3]. The symposiums revealed the substantial economic development that has occurred in these countries as well as the rapid growth in information and communications technologies. These technologies allow both physicians and the general public in developing countries to learn about the latest treatments being provided in developed countries as they occur. As a result, demand is rapidly growing for health care services of the same standard as those available in developed countries. People now know that diseases once deemed incurable can now be treated with advanced methods in use in developed countries. Dialysis therapy is a typical example. The first symposium in 2015 covered the status of dialysis therapy at the time in Myanmar, Vietnam, Thailand, China, and Japan; the second symposium in 2016 introduced issues about dialysis therapy in Cambodia, Laos, Bhutan, Mongolia, and Indonesia; and the third symposium in 2017 provided status updates for Vietnam, Myanmar, and Cambodia.
The fourth symposium, held in June 2018, opened the door beyond Asian countries to include all non-Western countries, spanning Africa, Asia, and Eastern Europe, in order to grasp the current status of dialysis therapy around the world. Two researchers from Cambodia and Japan presented their work and contributed manuscripts to this 2018 symposium issue.
We hope that this report from the 2018 symposium on the status of dialysis therapy will contribute to the continuing development of partnerships between Asian developing countries, non-Western countries, and Japan.
History and current status of hemodialysis in Cambodia: the 2017 registry study
-
Pichthida Thim, Elin Phon, Chanseila Hy, Sovandy Chan
History of dialysis in Cambodia
Cambodia is located in Southeast Asia and shares borders with Vietnam, Laos, and Thailand. It consists of 25 provinces, and the capital is Phnom Penh. The life expectancy of women nationwide is longer than that of men (67.5 years vs 62.4 years) [4]. In 1997, the first hemodialysis (HD) center in Cambodia was established at Calmette Hospital. Initially, it had only 4 HD machines. In 2007, another 3 HD centers were established. There were 2 government dialysis centers at Preah Ket Mealea Hospital and Health Science Institute Hospital. In 2014, the HD center at Health Science Institute Hospital was closed due to lack of funding. There was also a private clinic with an HD center called La Santé Medical Center. In 2010, the Cambodia Japan Friendship Blood Purification Center was established with the support of the nongovernmental organization (NGO) Ubiquitous Blood Purification International (UBPI) at Sen Sok International University Hospital. In 2012, the first provincial HD center was founded at Siem Reap Referral Hospital, supported by the Takatsuki Rotary Club of Japan and NGO UBPI. In addition, an HD center was established at Preah Kossamak Hospital. During that period, a private center, Yi Kouk Hemodialysis Center, was established in Battambang province. In 2016, the Cambodian Association of Nephrology (CAN) was founded with the support of NGO UBPI. In June 2017, CAN officially became the International Society of Nephrology (ISN) Affiliated Society. To date, there are 8 HD centers in only 3 regions: Phnom Penh, Siem Reap, and Battambang. Currently, there are 15 nephrologists in Cambodia. In 2016, the cost of a single HD session was about US$50, while the annual household income per capita was US$1228 [5]. Patients bear the full cost of treatment, as well as the cost of transportation and accommodation if they are provincial patients.
Background of the 2017 dialysis registry study in Cambodia
The number of HD patients continues to rise each year worldwide. Annually, between 2.3 and 7.1 million people in mainly low- and middle-income countries need RRT [6]. The 3 main types of renal replacement therapy (RRT) are HD, peritoneal dialysis (PD), and kidney transplantation. In Cambodia, only HD is available. The main causes of end-stage renal disease (ESRD) are hypertensive nephropathy and diabetic nephropathy. Currently, there is no national registry of Cambodian HD patients. However, the number of patients with hypertension (HTN) and diabetes mellitus (DM) continues to rise each year. Outpatients with HTN increased from 157,542 in 2014 to 255,763 in 2017. Patients with DM rose from 24,301 in 2014 to 56,152 in 2017 [7]. Accordingly, the number of patients needing HD is presumed to have also increased during that period. Therefore, the purpose of the present study was to improve current knowledge of HD patients and thus improve their outcomes and develop better approaches for this population.
Methods
This was a cross-sectional study involving patients at 5 HD centers in Phnom Penh, Cambodia, in August 2017. Data were collected by asking HD patients to complete a questionnaire that covered important variables such as age, sex, place of residence, causes of end stage renal disease, HD frequency per month, and duration of each HD session. The data were analyzed using SPSS software.
Results
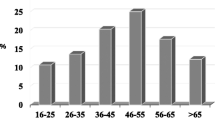
A total of 407 patients participated in the study. All patients treated at the centers responded to our questionnaire. Of these, 9.3% were incident HD patients. About half of all the patients resided in Phnom Penh, while the rest lived in provinces outside the capital. Figure 1 shows the proportion of patients by residence. Mean age was 52(standard deviation [SD], ± 15) years. Mean age of incident HD patients was 52 (SD, ± 16) years. Most were aged 51–60 years (29.2%) or 61–70 years (25.8%). No patients were aged 0–10 years. Figure 2 shows the distribution of patients according to age group. Figure 3 shows the distribution of patients by sex. There were more male patients (n = 233; 57.2%) than female patients (n = 174; 42.8%).
Many diseases can cause ESRD. In our population, HTN was the leading cause (46.8%), followed by hypertension and DM (31%), while DM alone accounted for only 8.1%. Other causes were chronic glomerulonephritis (12%), renal cystic disease (1.7%), graft rejection after kidney transplantation (0.2%), and acute kidney injury (0.2%). Detailed data on all causes are shown in Fig. 4.
Regular HD is important. Normally, dialysis frequency is reported by week. However, patients receive irregular HD doses. Therefore, only the number of HD sessions per month was analyzed in this study. Of all the patients, 56% received 8 sessions per month. Mean frequency of the sessions was 7.5 (SD, ± 2.3) per month. Figure 5 shows the frequency of HD sessions per month. The duration of each HD session was 4 h.
As mentioned above, data were collected from 5 HD centers in Phnom Penh. The top 3 centers that the patients visited were Calmette Hospital, Preah Ket Mealea Hospital, and La Santé Medical Center. Figure 6 shows the distribution of patients according to HD center. Figures 7 and 8 show the location of Cambodia in the world map and the location of HD center in the country’s capital Phnom Penh [8, 9].
Location of Cambodia in World Map [9]
Location of HD centers in Phnom Penh, Cambodia [10]
Discussion
Currently, there are insufficient physical resources such as dialysis centers and medical equipment in Cambodia. Patients must travel from provinces to access HD services, which in turn can be one of the reasons for poor adherence to HD treatment. Human resources are also limited. The number of nephrologists is insufficient in proportion to the number of patients who need HD. There are also no clinical engineers in hospitals, which means that it is difficult to fix machines that are not operating optimally. There are also no dieticians. This creates an unfavorable situation for patients because personalized meal plans are known to be crucial in helping HD patients.
Mean age of HD patients in the 1999–2003 Thai registry was 54 years, which is similar to that in our population. However, there were more male patients than female patients in our population, while the numbers were almost the same in Thailand, (male:female, 50.2%:49.8%) [10]. The Kidney Disease Outcomes Quality Initiative (KDOQI) in 2015 [11] divided HD treatment into conventional HD treatment, frequent HD treatment, and long HD treatment. Conventional HD treatment continues to be the most common treatment for ESRD worldwide, and sessions are usually 3–5 h long and delivered 3 times per week. In our population, the mean number of HD sessions per month was 7.5 (SD, ± 2.3). The mean number of HD sessions per week was approximately 1.89, and the duration of each session was 4 h. The duration of HD treatment seems to be appropriate, but most HD patients do not receive regular HD treatment. There are no insurance systems in Cambodia. Patients must bear the full cost of dialysis out of pocket, which is about US$50 per HD session. However, the average income in Cambodia is about US$1228 per capita [5]. If patients can afford treatment, then they can receive HD 3 times per week as in developed countries. The frequency of treatment depends on money, and the reality of the situation faced by HD patients in Cambodia can be summed up as “No money, no life.”
There are 2 main types of indications for initiation of HD:
-
1.
Non-emergencies, when patients begin to experience symptoms such as nausea, vomiting, and malnutrition due to uremic syndrome. In these cases, we suggest that patients start HD.
-
2.
Emergencies, where patients present with critical conditions such as severe pulmonary edema, severe hyperkalemia (K > 6.5 mmol/L), severe azotemia (manifesting as confusion or convulsions), and severe metabolic acidosis (pH < 7.2). In these cases, we explain to the patient that dialysis is immediately required.
Regardless of the indication, we always explain the process and the importance of HD to patients and then let them decide. For very poor patients who are admitted to public hospitals in critical condition, the dialysis is first done free of charge as a life-saving measure, with the government covering the cost. For chronic dialysis, on the other hand, patients must bear the cost by themselves. In fact, before 2018, only a few poor patients in critical condition were able to receive dialysis therapy for free (paid by government). However, since end of 2019 a program called the “National Social Security Fund” has helped employees and government workers pay for medical costs if they are hospitalized. This program also helps pay for poor patients who are hospitalized at public hospitals in critical condition.
In Thailand, the two most common underlying causes of kidney disease were DM (31.5%) and HT (20.9%) [10]. HTN occurred more frequently in the Cambodian patients (Fig. 4). No data are available on comorbid DM and HTN in the Thai population. Considering that the basic characteristics and lifestyles in Cambodia and Thailand are known to be similar, the difference in the causes was probably due to the small sample size. In any case, DM was revealed as the most serious cause of kidney disease in both countries.
Conclusion
Although the status of HD in Cambodia is gradually improving, it remains insufficient. There is a need for further improvement in various areas. Physical resources and human resources need to be improved in terms of quality and quantity. Solutions to poor adherence to HD treatment are important. Government and private health insurance subsidies should be implemented because they play a large role in improving adherence to HD treatment. HTN and DM are major causes of ESRD. Therefore, primary, secondary, and tertiary prevention of these chronic diseases are essential.
Current status of dialysis medical care and problems to be resolved in developing countries in East and Southeast Asia from the perspective of support activities carried out by several Japanese societies and organizations for dialysis therapy and technology
-
Kenichi Kokubo, Hirokazu Matsubara, Haruki Wakai, Akihiro C Yamashita, Hideki Kawanishi
Introduction
Recently, economic development in East and Southeast Asia has advanced remarkably, enabling improvements in medical services. In turn, these improvements have led to increased numbers of dialysis patients and dialysis facilities in the region. To assist these countries in managing these changes, support projects in Japan were initiated by NGO UBPI in 2007. Currently, support activities in the region have been seamlessly and cooperatively carried out by several organizations, including the Human Resource Development Program Committee of the JSDT, the Committee on International Affairs of the Japanese Society for Technology of Blood Purification (JSTB), the Japanese Assistance Council for Establishing Dialysis Specialists’ System in Cambodia (JAC-DSC), and NGO UBPI [12]. This study describes the activities of several Japanese societies and organizations for dialysis therapy and technology that sought to resolve problems in dialysis medical care in East and Southeast Asian developing countries in 2018, focusing on the role of academic societies in this region.
Current status of dialysis medical care and problems to be resolved
The prevalence of dialysis therapy and access to the treatment among East and Southeast Asian developing countries differ in each country. Their health insurance and social security systems also differ. Therefore, the problems these countries face are not uniform [12]. However, all the countries share the same problem of clear disparities between urban and rural areas in terms of the availability of dialysis therapy and technical problems in dialysis therapy, such as machine maintenance and management of dialysate water quality, which is essential to ensuring treatment quality and safety. One of the causes of these disparities, in addition to domestic economic disparities, is thought to be the absence of a nationwide postgraduate education system. To address this, an academic society involving nationwide medical staff is needed to provide dialysis specialists throughout all areas of these countries.
With economic development, many medical devices including dialysis machines can be purchased. However, it takes time to train personnel with expertise in providing dialysis therapy. Support from academia can assist in resolving this problem. Specifically, JSDT and JSTB can readily provide support through training programs in Japan. If counterpart societies are present in developing countries, dialysis specialists can be supported through partnerships with these two societies.
Academic societies in each country and Japanese societies’ support activities
The Myanmar Nephro-Urology Society was established with dialysis therapy included within its scope. The society has been holding an international combined nephro-urology conference every 2 years. The 1st Myanmar Nephro-Uro International Conference was held in 2013, the 2nd in 2015, and the 3rd in 2017. Dialysis specialists can be supported through partnerships with the society (Fig. 9).
In Mongolia, there is the Mongolian Association of Hemodialysis, but it has not been particularly active and has not held nationwide annual conferences or seminars. In 2017, the Mongolian and Japanese 1st Joint Seminar on Hemodialysis Technology was held in Ulaanbaatar to facilitate discussion about dialysis therapy, especially focusing on dialysis technology and daily management with the support of JSTB and NGO UBPI (Fig. 10).
In Vietnam, there are several societies in the field of nephrology, but none directly related to dialysis therapy. We have advised that a new academic society similar to the JSDT be established in Vietnam as a forum for all medical personnel, including doctors, nurses, clinical engineers, and dietitians. In 2015, the Ho Chi Minh City Society of Dialysis Therapy (HSDT) was established, and the 1st Congress of the HSDT was successfully held in Ho Chi Minh City in collaboration with Japanese members of NGO UBPI (Fig. 11).
In Cambodia, NGO UBPI and JAC-DSC supported the establishment of CAN, and the 1st Congress of the CAN was held in Phnom Penh in November 2016. CAN became an ISN Affiliated Society in June 2017 (Fig. 12).
We have also supported the establishment of the Lao Society of Nephrology (LSN). A preconference and meeting for the foundation was held in Vientiane in March 2018 in collaboration with NGO UBPI (Fig. 13).
In 2017, JSDT started a new short-term program (10 days) for the study of dialysis therapy in Japan. Trainees from developing countries in East and Southeast Asia were accepted into the program, including doctors, nurses, clinical engineers, and medical and nursing school students, who have already worked or plan to work at HD facilities in Cambodia, Myanmar, Laos, Vietnam, Indonesia, Bhutan Nepal, and Mongolia. In 2017, the trainees also participated in the “Dialysis situation in Asian countries” symposium held in Shiga, Japan. Key opinion leaders, specialists, and young clinicians were invited to the symposium and discussed the current status of dialysis therapy and problems to be resolved, with the aim of providing new insights into improving dialysis therapy in the region [13].
Future challenges
In developing countries in East and Southeast Asia, dialysis therapy is administered by doctors and nurses only. In Japan, dialysis therapy involves a team of many specialized personnel, including doctors, nurses, clinical engineers, dietitians, and physiotherapists, which ensures the quality and safety of treatment. We expect that partnerships between academic societies in Japan and East and Southeast Asian developing countries will play an important role in establishing a training system for each dialysis specialty and in developing dialysis techniques to ensure high quality and safety in the region. We hope to deepen these partnerships and further develop collaborative work.
Availability of data and material
Not applicable.
Abbreviations
- JSDT:
-
The Japanese Society for Dialysis Therapy
- HD:
-
Hemodialysis
- NGO:
-
The nongovernmental organization
- UBPI:
-
Ubiquitous Blood Purification International
- ISN:
-
The International Society of Nephrology
- CAN:
-
The Cambodian Association of Nephrology
- RRT:
-
The renal replacement therapy
- PD:
-
Peritoneal dialysis
- ESRD:
-
End-stage renal disease
- HTN:
-
Hypertension
- DM:
-
Diabetes mellitus
- KDOQI:
-
Kidney Disease Outcomes Quality Initiative
- JSTB:
-
Japanese Society for Technology of Blood Purification
- JAC-DSC:
-
The Japanese Assistance Council for Establishing Dialysis Specialists’ System in Cambodia
- HSDT:
-
The Ho Chi Minh City Society of Dialysis Therapy
References
Hyodo T, Hirawa N, Hayashi M, Than KMM, Tuyen DG, Pattanasittangkur K, Hu LW, Naramura T, Miyamoto K, Yamashita AC. Present status of renal replacement therapy at 2015 in Asian countries (Myanmar, Vietnam, Thailand, China, and Japan). Renal Replacement Ther. 2017;3:11. https://doi.org/10.1186/s41100-016-0082-7.
Hyodo T, Fukagawa M, Hirawa N, Hayashi M, Nitta K, Chan S, Souvannamethy P, Minjur Dorji M, Dorj C, Widiana IGR. Present status of renal replacement therapy in Asian countries as of 2016: Cambodia, Laos, Mongolia, Bhutan, and Indonesia. Renal Replacement Ther. 2019. https://doi.org/10.1186/s41100-019-0206-y.
Hyodo T, Fukagawa M, Hirawa N, Isaka Y, Nakamoto H, Bui PV, Thwin KH, Hy C. Present status of renal replacement therapy in Asian countries as of 2017: Vietnam, Myanmar, and Cambodia. Renal Replacement Ther. 2020;6:65. https://doi.org/10.1186/s41100-020-00312-w.
David.P. (2017). Cambodia. Retrieved from https://www.britannica.com/place/Cambodia
Census and Economic Information Center. (2017). Cambodia Household Income per Capita. Retrieved from https://www.ceicdata.com/en/indicator/cambodia/annual-household-income-per-capita
World Health Organization. (2018). The global burden of kidney disease and the sustainable development goals. Retrieved from https://www.who.int/bulletin/volumes/96/6/17-206441/en/
MOH 2017 report. http://moh.gov.kh/content/uploads/2017/05/MOH-Report-Kh-V6.pdf
On the World Map. Cambodia Location on the World Map. Retrieved October 16, 2021 from https://ontheworldmap.com/cambodia/cambodia-location-map.html
GFXKH (2020). Phnom Penh Map 2020. Retrieved October 16, 2021 from https://www.gfxkh.com/cambodia-phnom-penh-map-2020/
Udom, K., et al. Anemia and Survival in Thai hemodialysis patients: Evidence from National Registry Data. Retrieved from https://www.researchgate.net/publication/6752091_Anemia_and_survival_in_Thai_hemodialysis_patients_Evidence_from_National_Registry_Data (2006)
Update of the KDOQI Clinical Practice Guideline for Hemodialysis Adequacy. (2015). Retrieved from https://www.kidney.org/sites/default/files/KDOQI-Clinical-Practice-Guideline-Hemodialysis-Update_Public-Review-Draft-FINAL_20150204.pdf
Kokubo K, Kobayashi K, Urabe S, et al. Support for dialysis therapy in Vietnam, Cambodia, and Myanmar by Japanese societies in the field of blood purification. Blood Purif. 2017;44(Suppl 1):55–61.
Masuda T. The, “dialysis situation in Asian Countries” Symposium: providing new insights to improve dialysis in the region. Blood Purif. 2017;44(Suppl 1):3–18.
Acknowledgements
The 2017 dialysis registry data in Cambodia has been already published as the combined report of 2017 and 2018 in the Cambodian Journal of Nephrology (CJN), 2019: 4 (1): 14-21 (https://www.reiseikai-media.org/onlinelibrary/pdf/CJN_CAN_web2019_0831.pdf) because this issue was delayed and the order was upside down. The publication by using 2017 data is permitted by the publisher of CJN, Reiseikai, Media, Cambodia, Co., Ltd.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
This report is a review article by the Committee of International Communication for Academic Research of JSDT. TH, NH, and YI designed this report and are committee members. HN also designed this report and is president of JSDT. PT, KK wrote their own reports. EP, CH, and SC contributed to the Cambodian study. HM, HW, ACY, and HK contributed to the activities of the Japanese groups. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study does not report on or involve the use of any animal or human data or tissue.
Consent for publication
None of the reports contains personal data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hyodo, T., Hirawa, N., Isaka, Y. et al. Current status of renal replacement therapy in Cambodia and Japanese support activities in developing countries in East and Southeast Asia: a report as of June 2018 from the Non-Western World Countries Symposium at the 63rd Annual Meeting of the Japanese Society for Dialysis Therapy. Ren Replace Ther 8, 9 (2022). https://doi.org/10.1186/s41100-022-00398-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-022-00398-4
Keywords
- The Japanese Society for Dialysis Therapy
- The Cambodian Association of Nephrology
- Japanese Society for Technology of Blood Purification
- NGO Ubiquitous Blood Purification International
- End-stage renal disease
- Dialysis therapy
- Renal registry
- Economic development
- Chronic kidney disease
- Dialysis nurses
- Dialysis doctors
- Dialysis dietitians
- Clinical engineers
- National health insurance system