Abstract
Background
In continuous renal replacement therapy (CRRT), administration of anticoagulants is necessary for achieving a certain level of filter lifetime. Generally, anticoagulant doses are controlled to keep activated partial thromboplastin time and other indicators within a certain target range, regardless of the membrane materials used for the filter. However, in actual clinical practice, the filter lifetime varies significantly depending on the membrane material used. The objective of this study was to demonstrate that the minimum anticoagulant dose necessary for prolonging the filter lifetime while reducing the risk of hemorrhagic complications varies depending on the type of membrane.
Methods
In three beagles, hemodiafiltration was performed with hemofilters using polysulfone (PS), polymethylmethacrylate (PMMA), and AN69ST membranes separately. The minimum dose of nafamostat mesylate (NM) that would allow for 6 h of hemodiafiltration (required dose) was investigated for each membrane material.
Results
The NM doses required for 6 h of hemodiafiltration were 2 mg/kg/h for the PS membrane, 6 mg/kg/h for the PMMA membrane, and 6 mg/kg/h for the AN69ST membrane.
Conclusion
For hemodiafiltration performed in beagles, the required NM dose varied for each filter membrane material. Using the optimal anticoagulant dose for each membrane material would allow for safer CRRT performance.
Similar content being viewed by others
Background
Renal replacement therapy (RRT) has been an essential therapeutic strategy in the intensive care unit (ICU), such as mechanical ventilation [1, 2]. The incidence of acute kidney injury (AKI) requiring RRT has been increasing by 10% each year for the past 20 years [3]. Continuous renal replacement therapy (CRRT) is recommended, especially for critically ill patients with unstable hemodynamics [4, 5]. Of the available modalities for CRRT, continuous hemodiafiltration (CHDF) is frequently used in Japan [2].
When CRRT is performed, administration of anticoagulants is necessary for achieving certain levels of circuit and filter lifetimes. As for anticoagulants, nafamostat mesylate (NM), which is considered less likely to cause hemorrhagic complications, has been covered by the National Health Insurance scheme and is widely used in Japan [6]. The dose of this anticoagulant is predefined and fixed or it is determined to maintain activated partial thromboplastin time (APTT) or activated clotting time (ACT), etc. within a target range. Because the onset of hemorrhagic complications can be lethal for critically ill patients with unstable hemodynamics, controlling the anticoagulant dose is extremely important. To perform CRRT more safely, anticoagulant doses should be kept as low as possible while still prolonging the circuit and filter lifetimes to clinically acceptable levels.
While anticoagulants are administered at doses predefined and fixed or keep APTT or ACT constant in clinical practice, we have found that the circuit and filter lifetimes vary significantly depending on the membrane type selected for the filter. We assume that the optimal dose, which is the minimum necessary to reduce the risk of hemorrhagic complications and to safely perform hemodiafiltration, differs depending on the type of membrane used. A number of studies on filter lifetime using animals have been conducted in the past [7, 8], and we presumed this would be useful for clinical applications in humans. We presumed that an animal study on filter lifetime according to membrane type would be useful for developing clinical applications in humans Therefore, in this study using beagles, we investigated the minimal NM dose necessary to achieve a certain level of filter lifetime for each membrane type, aiming to show that the doses vary depending on the membrane used.
Methods
Objectives
The minimal NM dose necessary to perform hemodiafiltration (HDF) for a certain period was compared between filters using three different types of membrane materials: polysulfone (PS), polymethylmethacrylate (PMMA), and AN69ST membranes. By revealing differences between these doses, we aimed to demonstrate that the optimal NM doses varied depending on the type of membrane used.
Experimental animals
Three male adult beagles with a mean body weight of 10.3 kg were used (No. 1–3). After they were delivered, the beagles were immediately quarantined and acclimated for at least 1 week. HDF was to be performed once a week. Up to three times HDF were to be performed to each beagle.
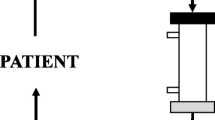
HDF devices used
HDF was performed using TR55X (JUNKEN MEDICAL Co., Ltd.). For the filters, EXCELFLO AEF-07® 0.7 m2 was used for the PS membrane (hereinafter referred to as PS; Asahi Kasei Medical CO., Ltd.), Hemofeel CH® 0.6 m2 was used for the PMMA membrane (hereinafter referred to as PMMA; Toray Medical Co., Ltd.), SepXiris® 0.6 m2 was used for the AN69ST membrane (hereinafter referred to as AN69ST; Baxter Limited), and these three types of filters were compared. The UK-catheter kit 6Fr (UB-0610-W; Unitika) was used for venous access.
HDF preparation
The beagles were pretreated with a single intramuscular injection of ketamine hydrochloride (100 mg/2 mL/body). After general anesthesia was induced with inhalation anesthesia using a mask (isoflurane and nitrous oxide), they underwent tracheal intubation and mechanical ventilation was initiated. Anesthesia was maintained using inhalation anesthesia (isoflurane and nitrous oxide). A venous access catheter (filled with physiological saline containing approximately 10 IU of heparin sodium in the blood removal-side circuit and physiological saline in the reinfusion-side circuit) was inserted and placed in the right internal jugular vein.
The circuit was primed by flushing with heparinized physiological saline (approximately 5000 U/L of heparin) and refilled with physiological saline. The substitution fluid was administered in the post-dilution mode. After the preparation was complete, the venous access catheter was connected to the HDF device. The blood pump and syringe pump for the anticoagulant were activated to extracorporeally circulate the blood. The blood flow rate was started at 10 mL/min and raised by 2 mL/min every 30 s to the target rate of 30 mL/min. Immediately after the blood flow rate reached 30 mL/min, the pumps for dialysate, filtrate, and substitution fluid were activated to start HDF.
HDF procedure
HDF was performed at a blood flow rate of 30 mL/min, a dialysate flow rate of 10 mL/kg/h, a substitution fluid flow rate of 6 mL/kg/h, and a filtrate flow rate of 6 mL/kg/h. For anticoagulation, NM was administered at prespecified doses before the hemofilter.
Evaluation items and methods
The target duration of HDF was set at 6 h. Achievement of the target duration was defined as HDF for 6 h after initiation without any interruption. During HDF, the inlet chamber, the outlet chamber, and filtration pressures were monitored and recorded every hour. When the module inlet or outlet chamber pressure was 250 mmHg or higher, clotting was determined to have occurred in the blood circuit or the filter. The duration of HDF was recorded, and HDF was discontinued.
For each filter, of the NM doses that could be achieved in the target duration in three courses, the lowest dose was defined as the required dose. NM dosage was determined according to the following protocol:
Protocol
In each HDF course, if the target duration of 6 h was achieved, we set up the next course with the NM dosage reduced by 2 mg/kg/h. If the target duration was not achieved, we set up two courses with the same dosage and with the dosage increased by 2 mg/kg/h.
Precondition
-
1)
For each filter, NM 6 mg/kg/h was administered in the first course.
-
2)
Minimum dose was 2 mg/kg/h; maximum dose was 8 mg/kg/h.
-
3)
If the target duration was not achieved even once, HDF was not performed with a lower NM dose.
-
4)
Experimental HDF was performed with the same NM dose for up to three courses.
-
5)
To determine the required dose, a course was added to confirm the achievement of a total of three courses with a dose that was 2 mg/kg/h higher than the dose that was interrupted.
-
6)
If there was no interruption even at a dose of 2 mg/kg/h, a course was added to confirm the achievement of a total of three courses at 2 mg/kg/h.
As the number of experimental HDF courses performed with each membrane was not the same for all beagles, we performed the following validations to decrease the bias related to individual animal characteristics. We calculated the mean of each least dose, which was determined for each beagle with each filter membrane when the target duration was achieved, and defined it as the minimal NM dose in each filter. The minimal NM dose was compared using one-way analysis of variance (ANOVA). When a significant difference was observed, the Bonferroni multiple comparison test was performed.
In addition to anticoagulants, other factors that may affect filter lifetime include poor blood removal from the catheter and the degree of hemoconcentration. Therefore, vital signs were recorded before the experiment and every hour after starting the experiment. An additional 0.5 mL of blood was collected from the blood removal side at the start of HDF and at 1, 3, and 6 h after initiation, and blood counts were measured to identify any undetectable hemorrhagic complications and abnormal values of red blood cell (RBC) and platelet counts.
This study was approved by the Institutional Animal Care and Use Committee of Tokyo Women's Medical University (Permission number.: AE16-155) and conducted according to the Animal Experimentation Regulations of Tokyo Women's Medical University.
Results
Results of the experimental HDF are shown in Table 1. The experimental HDF was performed for a total of six courses with PMMA and AN69ST and a total of five courses with PS. With PMMA and AN69ST, experimental HDF was performed for two courses each in animals Nos. 1 to 3. However, with PS, it was performed for two courses each in animals Nos. 1 and 2 and for one course in animal No. 3. Vital signs were stable throughout the experiment, and there were no interruptions due to poor blood removal from the catheter in all experiments. ACT at the start of the experiment did not differ significantly; furthermore, no significant differences in RBC count and platelet count were observed throughout the experiment.
Comparison of required doses
With PS, experimental HDF was performed without interruption while NM was administered at 6 and 4 mg/kg/h and the target duration was achieved for three courses with an NM dose of 2 mg/kg/h. With PMMA, the target duration was achieved for three courses with an NM dose of 6 mg/kg/h. When NM was administered at 4 mg/kg/h, however, experimental HDF was performed without interruption for two courses but interrupted for one course. The cause of interruption was the gradual increase in the module inlet chamber pressure to more than 250 mmHg, 4 h 16 min after starting CHDF. On visual confirmation of coagulation, in addition to membrane clogging, only one hole on the blood removing side was blocked. Therefore, we determined that the main cause of the blockage was membrane clogging.
Similarly, with AN69ST, the target duration was achieved with an NM dose of 6 mg/kg/h. However, when NM was administered at 4 mg/kg/h, experimental HDF was performed without interruption for one course but interrupted for two courses. Module inlet chamber pressure of more than 250 mmHg was the cause of interruption in both courses. In one course, 3 h 47 min after starting HDF, we observed clotting at the side holes of the catheter, pillow, sampling port, and venous blood chamber. This was speculated to be a result of membrane clogging and blood circuit blockage. In another course, the interruption occurred 0 h 27 min after starting HDF. There was occlusion due to blood clots at two points in the side holes of the blood-removing part and at four points in the blood-returning part in the double-lumen catheter; there was no clogging in other parts of the blood circuit or membrane. In this case, clogging of the catheter was the main cause of interruption.
The required NM doses, therefore, were 2 mg/kg/h for PS, 6 mg/kg/h for PMMA, and 6 mg/kg/h for AN69ST (Table 1).
Comparison of minimal NM doses
The minimal NM doses were 2.00 mg/kg/h for PS, 4.67 mg/kg/h for PMMA, and 5.33 mg/kg/h for AN69ST. Because one-way ANOVA revealed significant differences between the three filters (P = 0.011), the Bonferroni multiple comparison test was performed. The results showed that the minimal NM dose was significantly lower for PS than for either PMMA or AN69ST (PS-PMMA, P = 0.040; PS-AN69ST, P = 0.015) (Fig. 1).
Comparison of minimal doses of nafamostat mesylate for different hemofilter membrane materials. Data represent the mean (SD) of each least dose, which was determined for each beagle in each filter membrane. Legend: after comparing the minimal doses of nafamostat mesylate (NM) for the three types of hemofilter membrane materials using one-way ANOVA, the membrane materials were found to be different in their effects (P = 0.011). Furthermore, the Bonferroni multiple comparison test of the minimal NM doses showed significant differences between **the polymethylmethacrylate (PMMA) and polysulfone (PS) membranes (P = 0.040) and between the *the AN69ST and PS membranes (P = 0.015)
Presence or absence of adverse events
In this study, no gross external bleeding occurred, and the measured red blood cell counts did not change. No apparent hemorrhagic complications were observed. Furthermore, during experimental HDF, neither skin eruption nor redness suggestive of anaphylaxis was observed, nor was there any change in vital signs or granulocyte counts.
Discussion
According to previous reviews, acute renal failure occurs in 30–60% of ICU patients [9], of whom 5–10% reportedly require RRT [3]. AKI alone is considered a risk factor for death [10], and mortality in patients with AKI who require RRT is estimated to be 30–70% [3]. This indicates that those requiring RRT are in an extremely vulnerable state. In addition, critically ill patients often have unstable hemodynamics. For these patients, CRRT is a commonly selected modality [9, 11] that is used especially in Japan [2].
However, because CRRT is performed over a long period of time, it is naturally more likely to cause clotting in the filter and circuit. Administration of anticoagulants at a certain dose is necessary to reduce blood loss due to clotting in the filter and circuit, to achieve a certain level of filter and circuit lifetimes, and to maintain stable CRRT performance. However, because the administration of anticoagulants increases the risk of bleeding, anticoagulant doses cannot be increased haphazardly. If dose reduction increases the incidence of clotting in the filter and circuit, blood transfusion may be required due to blood loss. Thus, it is necessary to balance these two conflicting risks. For this reason, selection of anticoagulants and control of their doses are important in CRRT and even more so in critically ill patients with coagulopathy [12,13,14]. The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines also recommend that for patients without coagulopathy or those not receiving systemic administration of anticoagulants for prevention of venous thromboembolism, anticoagulants should be selected with due consideration of the risk of blood loss, economic aspects, and staff workload while the risk of bleeding is recognized [4].
In general, unfractionated heparin is a widely used anticoagulant. Other anticoagulants selected to more safely perform CRRT include low-molecular-weight heparins (LMWHs), heparinoids (danaparoid and fondaparinux), direct thrombin inhibitors (lepirudin and argatroban), and regional anticoagulants such as citrate, serine protease inhibitors, and prostanoids [15]. However, there is no clear evidence of their usefulness at present [4]. Uchino et al. aggregated data on anticoagulants used in CRRT performed on 1006 patients with acute renal failure in 23 countries and reported that some patients did not receive anticoagulants (33.1%) and others received unfractionated heparin (42.9%), citrate (9.9%), NM (6.1%), or LMWH (4.4%) [16]. Citrate, which can contain the anticoagulant effect within the circuit, is recognized as useful [3] and recommended as the first-choice drug for patients at a high risk of bleeding with CRRT as per the KDIGO guidelines [4]. However, citrate is not widely used in Japan because it is not covered under the National Health Insurance scheme. Instead, NM is widely used in Japan as mentioned above. NM is suitable for dialysis because of its short half-life of 5–8 min and small molecular weight of 539.6 [14, 17]. Due to these properties, NM has been widely used as an anticoagulant with a low risk of causing hemorrhagic complications for CRRT in Japan [6]. According to the 2013 surveillance by the Japan Society for Blood Purification in Critical Care (JSBPCC), anticoagulants used for HDF in ICUs at 43 institutions in Japan were NM (84.3%), heparin (11.5%), LMWH (2.4%), and others (1.8%) [2], which indicates that NM is the predominantly used anticoagulant in Japan. However, it is not used in other countries because of concerns over adverse reactions, such as anaphylaxis [18] and agranulocytosis [19]. In this experiment on dogs, no such adverse reactions were observed.
Ohtake et al. evaluated the incidence of bleeding episodes in 43 critically ill patients who underwent CHDF and reported that the incidence was 67% in the heparin group, 29% in the LMWH group, and 4% in the NM group [20]. Although NM is less likely to cause hemorrhagic complications, increased doses naturally make blood less likely to coagulate. Consequently, the filter and circuit lifetimes are prolonged, but hemorrhagic complications can be lethal, as with heparin, if they occur. Thus, when CRRT is selected for critically ill patients with unstable hemodynamics, regardless of which anticoagulant is used, the doses must be reduced as much as possible while keeping the circuit and filter lifetimes within an acceptable range.
To date, studies have been conducted to reduce the risk of hemorrhagic complications and to achieve a certain filter lifetime. As mentioned above, many studies have been conducted on unfractionated heparin, citrate, LMWH, etc. [12, 14, 15, 20,21,22]. Although some of these studies mention the blood flow rate, etc., no study has mentioned the membrane materials used for hemofiltration. In many studies, anticoagulant doses were predefined and fixed or they were determined to maintain APTT, ACT, etc. within a target range [3, 22, 23]. Oudemans et al. presented doses of multiple anticoagulants, including NM, and values of monitoring indicators; however, membrane materials were also not mentioned in their study [12]. In other reported studies, NM doses were controlled based on ACT and APTT, regardless of membrane materials [14, 15, 21]. In their report, Oudemans et al. recommended administering NM at 0.1–0.5 mg/kg/h and adjusting the dose to keep APTT within 2–2.5 times the reference value as a target range [12]. Additionally, Ohtake et al. demonstrated a good correlation between ACT and NM doses and suggested that the use of NM in combination with monitoring ACT might allow for safer CRRT performance. They recommended an ACT of approximately 150 s as a target [20]. They also, however, did not mention the membrane material used.
In clinical practice, we found that filter lifetimes vary significantly depending on the membrane type used when anticoagulant doses are controlled to keep APTT and ACT within a certain range, regardless of membrane materials. For this reason, we performed this experiment on dogs to reveal the impact of membrane materials. The circuit and filter lifetimes are affected by various factors, including venous access and blood flow rate, in addition to the types and doses of anticoagulants [24]. Furthermore, when in vivo studies are conducted, there are additional biological factors, such as differences in blood coagulability among cases. We used dogs for the experiment and kept factors, except for anticoagulant doses, as consistent as possible. As a result, experiments were conducted without major changes to vital signs or platelet.
In addition to the PS and PMMA membranes, which are frequently used in Japan [2], the filter using the AN69ST membrane, which was recently covered by the National Health Insurance scheme in Japan, was selected for this experiment [25]. When the NM doses were controlled to keep APTT and ACT within a certain range, the lowest NM dose required to achieve a certain level of filter lifetime was observed in CRRT performed with the PS membrane in this experiment with dogs. This result is consistent with actual clinical practice, where the PS membrane has appeared to be associated with the longest filter lifetime. If the clinical efficacy of the three filters is similar, the conclusion that can be drawn from this experiment with dogs is that the filter using the PS membrane should be used to maximize the safety of performing RRT with NM anticoagulation in critically ill patients.
According to various guidelines, the clinical efficacy of HDF on cytokine removal in adults is under investigation. The usefulness of HDF has not yet been demonstrated, and RRT is not recommended for this purpose [4, 5]. Nevertheless, in Japan, the PMMA membrane, as well as the AN69ST membrane, which has recently been added, has still actively been used as a cytokine-absorbing membrane to treat sepsis primarily caused by hypercytokinemia. Thus, to safely perform CRRT in actual clinical practice at present, NM doses and other indicators should be set for each membrane material to minimize hemorrhagic complications without causing clotting in the circuit and to optimally control anticoagulant doses for each membrane. These approaches should allow for safer CRRT performance. Moreover, this concept may be applicable to not only NM but also to heparin used in CRRT. For safer CRRT performance in the future, it is presumably necessary to set APTT and ACT at levels that allow the optimal control of anticoagulant doses for each membrane.
This study has several limitations. First, it was conducted in dogs. Because their body weight is small, the blood flow rate set in this study was much lower than that for human adults. In consequence, this study provides reference values useful for studies on how to set anticoagulant doses for each filter but cannot present any target doses applicable to actual clinical practice. Second, NM, which is a widely used anticoagulant in Japan, was used in this study. Its use in dogs is limited, and whether NM acts in dogs in the same manner as in humans has not been investigated. However, the results of this study show a three-fold difference in the minimal NM dose between PS and PMMA, which is almost consistent with empirical data in humans. However, as mentioned above, evaluation of filter lifetime is complicated because of the effects of several factors, such as venous access, blood circuit, blood purification dose, and patient factors. It is necessary to fully recognize that even if the optimal anticoagulant dose is set for each membrane, this is only one of the factors that affect filter lifetime in actual clinical practice. Third, it was unfeasible to conduct a statistical analysis due to the small sample size. In addition, in normal situations, two-way ANOVA with repeated measures should have been performed to evaluate each NM dose for each filter. However, if the NM dose was reduced after clotting occurred in the circuit or the filter, it would be easy to expect that clotting would occur in the circuit or the filter again. Thus, in this study, from the perspective of animal welfare, priority was given to reducing the number of experimental sessions to be performed, and the protocol was designed to minimize the administration of NM at low doses that were expected to result in an interruption of the experiment. According to this protocol, therefore, experimental CRRT with NM administered at 2 mg/kg/h was performed only with the PS membrane. Likewise, to reduce unnecessary experimentation, only one course of CRRT using the PS membrane was performed each for NM administered at 6 and 4 mg/kg/h; as a result, animal No. 3 underwent only one course of this procedure. Although the results were self-evident, the conditions for each filter were inconsistent.
Conclusions
For RRT with the administration of NM, the required NM doses varied depending on the membrane material used. Thus, it seems necessary to set optimal anticoagulant doses according to membrane types instead of uniformly controlling the doses based only on ACT and APTT regardless of membrane types, as is currently done in many institutions. This approach should allow for safer CRRT performance.
Availability of data and materials
Please contact the corresponding author for any data requests.
Abbreviations
- ACT:
-
Activated clotting time
- APTT:
-
Activated partial thromboplastin time
- CHDF:
-
Continuous hemodiafiltration
- CRRT:
-
Continuous renal replacement therapy
- HDF:
-
Hemodiafiltration
- LMWH:
-
Low-molecular-weight heparin
- JSBPCC:
-
the Japan Society for Blood Purification in Critical Care
- NM:
-
Nafamostat mesylate
- One-way ANOVA:
-
One-way analysis of variance
- PMMA:
-
Polymethylmetacrylate
- PS:
-
Polysulfone
- RBC:
-
Red blood cell
- RRT:
-
Renal replacement therapy
References
Schetz M, Lauwers PM, Ferdinande P. Extracorporeal treatment of acute renal failure in the intensive care unit: a critical view. Intensive Care Med. 1989;15:349–57.
Arimura T, Abe M, Shiga H, Katayama H, Kaizu K, Oda S. Clinical study of blood purification therapy in critical care in Japan: results from the survey research of the Japan Society for Blood Purification in Critical Care in 2013. J Artif Organs. 2017;20:244–51.
Tandukar S, Palevsky PM. Continuous renal replacement therapy: who, when, why, and how. Chest. 2019;155:626–38.
Association of the Estimated Glomerular Filtration Rate With vs Without a Coefficient for Race With Time to Eligibility for Kidney Transplant. JAMA Netw Open. 2021;4(1):e2034004. https://doi.org/10.1001/jamanetworkopen.2020.34004. (PMID:33443583)
Doi K, Nishida O, Shigematsu T, Sadahiro T, Itami N, Iseki K, et al. The Japanese clinical practice guideline for acute kidney injury 2016. J Intensive Care. 2018;6:48.
Sadahiro T, Yuzawa H, Kimura T, Oguchi M, Morito T, Mizushima S, et al. Current practices in acute blood purification therapy in Japan and topics for further study. Contrib Nephrol. 2018;196:209–14.
Francey T, Schweighauser A. Regional citrate anticoagulation for intermittent hemodialysis in dogs. J Vet Intern Med. 2018;32:147–56.
Lavaud S, Canivet E, Wuillai A, Maheut H, Randoux C, Bonnet JM, et al. Optimal anticoagulation strategy in haemodialysis with heparin-coated polyacrylonitrile membrane. Nephrol Dial Transplant. 2003;18:2097–104.
Heung M, Yessayan L. Renal replacement therapy in acute kidney injury: controversies and consensus. Crit Care Clin. 2017;33:365–78.
Bellomo R, Ronco C, Mehta RL, Asfar P, Boisramé-Helms J, Darmon M, et al. Acute kidney injury in the ICU: from injury to recovery: reports from the 5th Paris International Conference. Ann Intensive Care. 2017;7:49.
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–8.
Oudemans-van Straaten HM, Wester JPJ, ACJM dP, MRC S. Anticoagulation strategies in continuous renal replace- ment therapy: can the choice be evidence based? Intensive Care Med. 2006;32:188–202.
Monchi M, Berghmans D, Ledoux D, Canivet JL, Dubois B, Damas P. Citrate vs. heparin for anticoagulation in continuous venovenous hemofiltration: a prospective randomized study. Intensive Care Med. 2004;30:260–5.
Choi JY, Kang YJ, Jang HM, Jung HY, Cho JH, Park SH, et al. Nafamostat mesilate as an anticoagulant during continuous renal replacement therapy in patients with high bleeding risk: a randomized clinical trial. Medicine (Baltimore). 2015;94:e2392.
Nongnuch A, Tangsujaritvijit V, Davenport A. Anticoagulation for renal replacement therapy for patients with acute kidney injury. Minerva Urol Nefrol. 2016;68:87–104.
Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, et al. Continuous renal re-placement therapy: a worldwide practice survey. The beginning and ending supportive therapy for the kidney (B.E.S.T. kidney) investigators. Intensive Care Med. 2007;33:1563–70.
Maruyama H, Miyakawa Y, Gejyo F, Arakawa M. Anaphylactoid reaction induced by nafamostat mesilate in a hemodialysis patient. Nephron. 1996;74:468–9.
Okada H, Suzuki H, Deguchi N, Saruta T. Agranulocytosis in a haemodialysed patient induced by a proteinase inhibitor, nafamostate mesilate. Nephrol Dial Transplant. 1992;7:980.
Nakae H, Tajimi K. Pharmacokinetics of nafamostat mesilate during continuous hemodiafiltration with a polyacrylonitrile membrane. Ther Apher Dial. 2003;7:483–5.
Ohtake Y, Hirasawa H, Sugai T, Oda S, Shiga H, Matsuda K, et al. Nafamostat mesylate as anticoagulant in continuous hemofiltration and continuous hemodiafiltration. Contrib Nephrol. 1991;93:215–7.
Schetz M. Anticoagulation for continuous renal replacement therapy. Curr Opin Anaesthesiol. 2001;14:143–9.
Hirsh J, Warkentin TE, Shaughnessy SG, Anand SS, Halperin JL, Raschke R, et al. Heparin and low-molecular-weight heparin: mechanisms of action, pharmacokinetics. dosing, monitoring, efficacy, and safety. Chest. 2001;119:64S–94S.
Vinsonneau C, Allain-Launay E, Blayau C, Darmon M, Ducheyron D, Gaillot T, et al. Renal replacement therapy in adult and pediatric intensive care : recommendations by an expert panel from the French Intensive Care Society (SRLF) with the French Society of Anesthesia Intensive Care (SFAR) French Group for Pediatric Intensive Care Emergencies (GFRUP) the French Dialysis Society (SFD). Ann Intensive Care. 2015;5:58.
Brain M, Winson E, Roodenburg O, McNeil J. Non anti-coagulant factors associated with filter life in continuous renal replacement therapy (CRRT): a systematic review and meta-analysis. BMC Nephrol. 2017;18:69.
Doi K, Iwagami M, Yoshida E, Marshall MR. Associations of polyethylenimine-coated AN69ST membrane in continuous renal replacement therapy with the intensive care outcomes: observations from a claims database from Japan. Blood Purif. 2017;44:184–92.
Acknowledgements
We would like to thank Dr. Yuichiro Yamada (Department of Cardiology, Tokyo Women’s Medical University) for his technical support in statistical analysis.
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
HY made the substantial contributions to the study conception and design, acquisition analysis, and interpretation of the data. TS helped to draft of the manuscript. YY analyzed the patient data. All authors read and approved of the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study conformed to the provisions of the Declaration of Helsinki. The study was approved by the Tokyo Women’s Medical University Animal Care and Use Committee (No. AE16-155).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yuzawa, H., Hirose, Y., Kimura, T. et al. Filter lifetimes of different hemodiafiltration membrane materials in dogs: reevaluation of the optimal anticoagulant dosage. Ren Replace Ther 7, 7 (2021). https://doi.org/10.1186/s41100-021-00323-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-021-00323-1