Abstract
Background
We evaluated the biocompatibility and small protein permeability of a newly developed hydrophilic-coated membrane dialyzer (NV) compared with conventional polysulfone dialyzer (APS) for hemodialysis (HD) therapy.
Methods
In a prospective crossover study, 11 maintenance HD patients (7 males; mean age 67.0 ± 10.2 years) received HD three times a week for 4 weeks with the NV membrane and then for another 4 weeks with the APS membrane. We evaluated the variation in several parameters including white blood cell (WBC) count and fibrinogen as indexes for biocompatibility. The plasma and dialysate concentrations of β2-microglobulin (β2-M), α1-microglobulin (α1-M), and albumin were measured at baseline and after 4 h of each study treatment in order to assess the removal of small proteins.
Results
Reductions in the WBC count were seen with APS compared with NV at 60 min (NV 5.65 ± 1.60, APS 5.17 ± 1.65 × 103/μL, p < 0.05) and 240 min (NV 5.28 ± 1.38, APS 4.63 ± 1.2 × 103/μL, p < 0.005) after the start of HD. With NV, we found significantly greater rates of variation of β2-M (NV 45.5 ± 1.2, APS 40.1 ± 1.2%, p < 0.0001), α1-M (NV 41.2 ± 9.9, APS 34.2 ± 18.5%, p < 0.05), and albumin (NV 31.6 ± 7.8, APS 18.1 ± 6.5%, p < 0.0001) during HD than with APS. However, there were no significant differences in the removal of β2-M between the two dialyzers.
Conclusions
The clinical characteristics of NV may reveal an improved biocompatibility and a comparable efficiency in small protein removal as compared to those of APS.
Trial registration
Clinical effects of polysulfone membrane, NV-13U UMIN000011764
Similar content being viewed by others
Background
Biocompatibility and middle molecule clearance of hemodialysis (HD) membranes affect the survival, morbidity, and quality of life of uremic patients undergoing maintenance HD therapy. In particular, malnutrition [1] and dialysis-related amyloidosis due to the reference middle molecule β2-microglobulin (β2-M) [2] are the major long-term complications. A polysulfone (PS) dialyzer is the mainstay of HD treatment because of its high performance. However, TORAYLIGHT® NV dialyzer (NV; Toray Industries, Inc., Tokyo, Japan) is expected to have different characteristics from the conventional PS due to its newly developed hydrophilic-coated membrane [3]. We therefore designed this prospective, crossover study to evaluate the biocompatibility and low-molecular-weight protein permeability (small protein permeability) of NV compared with a conventional PS (APS; ASAHIKASEI Industries, Inc., Tokyo, Japan).
Methods
Eleven maintenance HD patients (7 males; mean age 67.0 ± 10.2 years) on regular thrice-weekly HD treatment for 4 h were enrolled in the study after they had given their written informed consent. The underlying renal diseases were diabetes mellitus (N = 3), glomerulonephritis (N = 2), and unknown (N = 6). The mean duration of dialysis treatment was 48.6 ± 45.0 (range 15 to 258) months. All of the patients underwent 12 consecutive HD treatments with NV-13U (1.3 m2) and then switched with APS-13SA (1.3 m2) as a control after a 2-week wash-out period.
Laboratory measurements
The platelet (PLT) count, white blood cell (WBC) count, and hematocrit (Hct) were measured at the beginning of dialysis and after 30, 60, and 240 min. To adjust for differences in the cell counts at the beginning of dialysis, we calculated the change ratio at each point using the following formula (1):
We measured the urea nitrogen, serum creatinine, inorganic phosphorus, single-pool Kt/V [4], and hemoglobin levels; the removal rate of β2-M; and the rate of variation of β2-M, α1-microglobulin (α1-M), and albumin. We also measured the levels of platelet factor-4 (PF-4), β-thromboglobulin (β-TG), fibrinogen/fibrin degradation products (FDP), d-dimer, and fibrinogen (FIB).
Dialysate samples were collected at the final two dialysis sessions at a speed of 1.0 L/h using a fixed-quantity pump from the dialysate discharge line for 0–60, 60–180, and 180–240 min after the start of HD. On the assumption that each value measured before dialysis was 100%, the results were evaluated for variability.
This study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the ethics committees of Kamifukuoka General Hospital and National Defense Medical College Hospital.
Statistical analyses
The continuous values of variables are expressed as the mean ± standard deviation or as the median (25th, 75th percentile). The comparative p values for continuous variables were calculated by an analysis of variance (ANOVA). All of the statistical analyses were carried out using the JMP Pro Version 11.2.0 software program (SAS Institute, Cary, NC, USA), setting the significance level at a p value of less than 0.05.
Results
Biocompatibility
Reductions in the WBC count were seen with APS compared with NV at 60 min (NV 5.65 ± 1.60, APS 5.17 ± 1.65 × 103/μL, p < 0.05) and 240 min (NV 5.28 ± 1.38, APS 4.63 ± 1.20 × 103/μL, p < 0.005) after the start of HD (Fig. 1). The PLT count was not markedly different between the two dialyzers. The change ratios of the WBC count were significantly smaller with NV than with APS after 60 min (NV 96.3 ± 2.3, APS 92.5 ± 7.5%, p < 0.01) and 240 min (NV 91.3 ± 2.3, APS 84.6 ± 11.3%, p < 0.05) (Fig. 2).
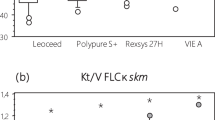
No significant differences were seen in the levels of Hct, PF-4, β-TG, FDP, or d-dimer or in the change ratio of FIB between NV and APS (Table 1). There were also no significant differences in the urea nitrogen, creatinine, inorganic phosphorus, single-pool Kt/V, or hemoglobin values between the two dialyzers (Table 2).
Small protein permeability
The intradialytic removal of α1-M was greater with NV than with APS in the first hour (NV 15.7 ± 4.0, APS 10.7 ± 3.0 mg, p < 0.001) and last hour (NV 6.47 ± 2.35, APS 3.23 ± 0.74 mg, p < 0.001) as well as over the total HD session (NV 32.0 ± 11.3, APS 17.7 ± 6.3 mg, p < 0.0001) (Fig. 3). In addition, the removal of albumin was greater with NV than with APS in the first hour (NV 340 ± 125, APS 198 ± 59 mg, p < 0.001) and last hour (NV 109 ± 46, APS 32.0 ± 3.8 mg, p < 0.001) as well as over the total HD session (NV 693 ± 283, APS 249 ± 90 mg, p < 0.001) (Fig. 4). There were no significant differences in the removal of β2-M between the two dialyzers (Fig. 5). However, the rates of variation during HD were greater with NV than with APS for β2-M (NV 45.5 ± 1.2, APS 40.1 ± 1.2%, p < 0.001), α1-M (NV 41.2 ± 9.9, APS 34.2 ± 18.5%, p < 0.05), and albumin (NV 31.6 ± 7.8, APS 18.1 ± 6.5%, p < 0.001).
Discussion
The PS membrane has shown a very good biocompatibility due to its superior removal performance for small-molecule proteins such as β2-M, high clearance of small-molecule solutes such as urea and creatinine [5], and low rate of complications such as leukopenia or disorders associated with the complement system [6]. Therefore, the PS membrane is widely used for HD treatment in Japan [7]. The NV membrane was developed as an alternative to PS. With NV, the mobility of water adjacent to the membrane surface is enhanced using a new hydrophilic polymer to reform the membrane surface. NV has antithrombotic activity and less platelet and leukocyte activation than PS, as well as the ability to sufficiently remove small solutes and low-molecular-weight proteins [3]. Further, NV induces less interleukin-6 activity, which may reduce the risk of erythropoiesis-stimulating agent hyporesponsiveness [8]. In this study, we evaluated the biocompatibility and protein permeability of NV compared with those of APS as a conventional PS.
The variation of several parameters such as the WBC, PLT, Hct and levels of PF-4, β-TG, FDP, d-dimer, and FIB were compared to evaluate the biocompatibility of NV. PF4 and β-TG are substances contained within platelet α-granules, and changes in platelet PF4 or β-TG levels are useful indicators of platelet degranulation and activation during dialysis [9]. However, there were no significant changes observed in the coagulation factor values with either dialyzer. Although acute leukopenia is known to occur in all patients during the first 30 min of HD treatment [10], our study showed no reduction in the WBC during dialysis with either dialyzer. The platelet count usually decreases 5 to 15% at 15 to 30 min from the start of HD and recovers to the normal level by the end of the dialysis session [9, 11]. Oshihara [3] reported that the numbers of platelets adhering to the membrane surface were lower with NV than with the conventional PS (CX) membrane. In our results, the variations in the platelet counts with both membranes were stable, suggesting that both may prevent HD-associated thrombocytopenia.
It is known that WBC adhesion occurs with protein adsorption, and FIB adsorption promotes PLT adhesion on the dialysis membrane surface by blood exposure in HD treatment [12]. Platelet-derived microparticles are released from activated platelets during HD [13]. Although the biocompatibility of PS is generally regarded to be good, there are some reports that the PS dialyzer caused PLT depletion [14, 15]. On the other hand, the NV membrane has been reported that it not only inhibits the adhesion of blood components such as PLT and FIB but also acts as a highly biocompatible membrane to reduce blood cell stimulation because it is developed as a new hydrophilic polymer membrane [3]. With NV, the reduction rate of the WBC count was inhibited to a greater degree than with APS. However, the change ratio of FIB showed no significant difference between NV and APS. These results suggest that NV improves the biocompatibility compared with APS.
Dialysis-related amyloidosis is a major complication with long-term HD treatment and greatly affects patients’ quality of life. The removal of β2-M is therefore important to avoid this complication. However, there have been no reports of the small protein permeability of NV. We therefore designed this prospective crossover study to evaluate whether or not NV offers any advantages over APS. We found that the intradialytic removal of α1-M and albumin but not β2-M was significantly greater with NV than with APS. The rates of variation in the β2-M and α1-M levels during HD with NV were higher than with APS, but the differences were small. These results suggest that the removal performance of β2-M with NV and APS should be almost equivalent.
In addition, since the decrease in the serum albumin may cause low muscle mass [16], malnutrition [17], and mortality risk [18], it is important to select dialyzers with consideration of the laboratory data. NV removed significantly greater albumin than APS. Therefore, we should be cautious when using the NV membrane in elderly or malnourished patients, although the amount of albumin removed was less than 1 g (NV 693 ± 283, APS 249 ± 90 mg) in either dialyzer.
Because this was a short-term, prospective, crossover study involving only a few cases, large-scale and long-term future trials are necessary to corroborate our findings.
Conclusions
We designed this crossover study of the NV and APS membranes to evaluate the biocompatibility and small protein removal ability. The clinical characteristics of NV may reveal an improved biocompatibility and a comparable efficiency in small protein removal as compared to APS.
Abbreviations
- Alb:
-
Albumin
- FDP:
-
Fibrinogen/fibrin degradation products
- FIB:
-
Fibrinogen
- Hct:
-
Hematocrit
- HD:
-
Hemodialysis
- PF-4:
-
Platelet factor-4
- PLT:
-
Platelet
- PS:
-
Polysulfone
- WBC:
-
White blood cell
- α1-M:
-
α1-Microglobulin
- β2-M:
-
β2-Microglobulin
- β-TG:
-
β-Thromboglobulin
References
Kalantar-Zadeh K, Kopple JD, Block G, Humphreys MH. A malnutrition-inflammation score is correlated with morbidity and mortality in maintenance hemodialysis patients. Am J Kidney Dis. 2001;38:1251–63.
Gejyo F, Yamada T, Odani S, Nakagawa Y, Arakawa M, Kunitomo T, et al. A new form of amyloid protein associated with chronic hemodialysis was identified as beta 2-microgulobulin. Biophys Res Commun. 1985;129:701–6.
Oshihara W, Ueno Y, Fujieda H. A new polysulfone membrane dialyzer, NV, with low-founding and antithrombotic properties. Contrib Nephrol. 2017;189:222–9.
Shinzato T, Nakai S, Fujita Y, Takai I, Morita E, Nakane K, Maeda K. Determination of Kt/V and protein catabolic rate using pre- and postdialysis blood urea nitrogen concentrations. Nephron. 1994;67:280–90.
Fukuda M, Miyazaki M, Uezumi S, Yoshida M. Design and assessment of the new APS dialyzer (APS-SA series). J Artifs Organs. 2006;9:192–8.
Yamashita S, Mochizuki A, Nakazaki T, Seita Y, Sawamoto J, Endo F, et al. A new blood compatible and permselective hollow fiber membrane for hemodialysis. ASAIO J. 1996;42(6):1019–26.
Nakai S, Suzuki K, Masakane I, et al. Overview of regular dialysis treatment in Japan (as of 31 December 2009). Ther Apher Dial. 2010;14:505–40.
Kakuta T, Komaba H, Takagi N, Takahashi Y, Suzuki H, et al. A prospective multicenter randomized controlled study on interleukin-6 removal and induction by a new hemodialyzer with improved biocompatibility in hemodialysis patients: a pilot study. Ther Apher Dial. 2016;20(6):569–78.
Daugirdas JT, Bernardo AA. Hemodialysis effect on platelet count and function and hemodialysis-associated thrombocytoperia. Kidney Int. 2012;82:147–57.
Kaplow LS, Goffinet JA. Profound neutropenia during the early phase of hemodialysis. JAMA. 1968;203:1135–7.
Amato M, Salvadori M, Bergesio F, Messeri A, Filimberti E, Morfini M. Aspects of biocompatibility of two different dialysis membranes: cuprophane and polysulfone. Int J Artif Organs. 1988;11:175–80.
Reginald G. Mason, Hanson Y.K. chuang, S. Fazal Mohammad. Extracorporeal thrombogenesis: mechanisms and prevention. replacement of renal function by dialysis. 1983: 186-200.
Daniel L, Fakhouri F, Joly D, et al. Increase of circulating neutrophil and platelet microparticles during acute vasculitis and hemodialysis. Kidney Int. 2006;69:1416–23.
Kobari E, Terawaki H, Takahashi Y, et al. Dialyzer-related thrombocytopenia due to a polysulfone membrane. Intern Med. 2016;55:965–8.
Deprada L, Lee J, Gillespie A, Benjamin J. Thrombocytopenia associated with one type of polysulfone hemodialysis membrane: a report of 5 cases. Am J Kidney Dis. 2013;61:131–3.
Yasui S, Shirai Y, Tanimura M, Matsuura S, Saito Y, Miyata K. Prevalence of protein-energy wasting (PEW) and evaluation of diagnostic criteria in Japanese maintenance hemodialysis patients. Asia Pac J Clin Nutr. 2016;25(2):292–9.
Pifer TB, McCullough K, Port FK, Goodkin DA, Maroni BJ, Held PJ, et al. Mortality risk in hemodialysis patients and changes in nutritional indicators: DOPPS. Kidney Int. 2002;62:2338–245.
Dwyer JT, Larive B, Leung J, Rocco MV, Greene T, Burrowes J, et al. Are nutritional status indicators associated with mortality in hemodialysis (HEMO) study? Kidney Int. 2005;68:1766–76.
Acknowledgements
The authors thank all the staff members working at the Division of Blood Purification Center, Kamifukuoka General Hospital and Department of Blood Purification Therapy, National Defense Medical College Hospital.
Funding
This study has received research funds from the Foundation for Promotion of Defense Medicine.
Availability of data and materials
Data sharing is not applicable to this manuscript.
Author information
Authors and Affiliations
Contributions
HK designed the study, collected the clinical data, analyzed the data, and wrote the manuscript. AT designed the study and wrote the manuscript. AF collected the clinical data. KI, KO, and TI participated in its design and coordination. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the ethics committees of Kamifukuoka General Hospital (approval number 24-01) and National Defense Medical College Hospital (approval number 939). Written informed consent was obtained from the patients.
Consent for publication
We have also obtained the consent to publish from the participant to report the individual patient data.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kodama, H., Tsuji, A., Fujinoki, A. et al. Biocompatibility and small protein permeability of hydrophilic-coated membrane dialyzer (NV) in hemodialysis patients: a pilot study. Ren Replace Ther 3, 40 (2017). https://doi.org/10.1186/s41100-017-0121-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-017-0121-z