Abstract
Background
The Geriatric Nutritional Risk Index (GNRI) is a nutritional screening method primarily developed for elderly people; it is also reported to be useful for predicting mortality in patients on maintenance dialysis. However, it is unclear whether it is useful at the time of dialysis initiation, which is accompanied by large weight fluctuations and unstable nutritional status.
Methods
The study included 1524 patients with chronic kidney disease who commenced dialysis therapy at 17 centers. Patients commenced dialysis between October 2011 and September 2013 and were followed up until March 2015.
Results
We analyzed 1489 patients whose GNRI could be calculated and whose prognosis was clear. The mean GNRI was 87.60 (median 87.86). We divided patients based on the median value into a high (H) and low (L) group. The H group included 728 patients (mean GNRI 95.2 ± 4.9, mean age 65.8 ± 13.2 years, 69.3% men), and the L group included 761 patients (mean GNRI 80.3 ± 6.1, mean age 69.1 ± 12.8 years, 66.0% men). Mortality was significantly higher in the L group (L, 22.2% vs. H, 12.6%, P < 0.001). The rates of infection-associated death in the L group was significantly higher (L, 5.5% vs. H, 1.9%, P < 0.001), although no significant difference was observed regarding cardiovascular disease-associated death (L, 7.6% vs. H, 5.2%, P = 0.059) and malignancy-associated death (L, 3.0% vs. H, 3.0%, P = 1.000). Multivariate analysis showed an association between GNRI and all-cause mortality (HR 0.9852, 95%CI 0.9707–0.9999, P = 0.049) and infection-associated death (HR 0.9484, 95%CI 0.9191–0.9786, P < 0.001).
Conclusions
GNRI is useful for predicting mortality even at the time of dialysis initiation. Among the causes of death, GNRI was strongly associated with infection-associated death.
Similar content being viewed by others
Background
The number of patients receiving dialysis therapy is increasing yearly, and these patients show high mortality from various causes, the main causes being cardiovascular and infectious diseases [1]. Therefore, to improve the prognosis of patients who commence dialysis therapy, it is important to understand the characteristics of those at a high risk of mortality.
The Geriatric Nutritional Risk Index (GNRI) is a nutritional screening method primarily developed for elderly people and is reported to be useful for ascertaining disease prognosis [2]. Its usefulness in predicting poor outcomes has also been reported for various co-morbidities such as stroke [3], heart failure [4, 5], and for hospitalized patients [6, 7]. Moreover, GNRI is useful in ascertaining disease prognosis in patients on maintenance dialysis [8,9,10]. However, it remains unclear whether this index is also beneficial at the time of dialysis initiation, where the tendency exists for weight fluctuation due to fluid retention and malnutrition because of uremia.
Therefore, we compared the prognosis of patients with high and low GNRI at the time of dialysis initiation. We also examined various causes of death with respect to GNRI.
Methods
Patients and data collection
Data from the Aichi Cohort Study of Prognosis in Patients Newly Initiated into Dialysis [11, 12] were used in this prospective multicenter study. Patients who commenced dialysis between October 2011 and September 2013 at 17 Japanese institutions were included. This study was approved by the Ethics Committee of the Institutional Review Board of Nagoya Daini Red Cross Hospital (No. IRB20110823-3), and all patients provided written informed consent. Patients who were not discharged and died in the hospital were excluded (Fig. 1). Data regarding patient background, medical history, co-morbidities, medications, and laboratory data during the period of dialysis initiation were collected. Serologic data were obtained at the first dialysis session and just before dialysis initiation. Patients were followed until the end of March 2015.
Flow chart showing the process of patient registration. Only patients who became stable and were discharged or transferred from the hospital with consent were included. Patients who were not discharged and died in the hospital were excluded. We excluded patients without GNRI data. GNRI Geriatric Nutritional Risk Index
Method for calculating GNRI
Ideal body weight (IBW) was calculated from height, and GNRI was calculated using IBW, albumin (ALB) level, and body weight (BW).
Mortality
Patients were divided into two groups—high and low levels of GNRI—and outcomes and hazard ratios (HRs) were compared between groups. The primary endpoint was mortality. Causes of death were ascertained. The incidence of death was investigated via survey slips sent to the dialysis facilities at the end of March 2015.
Statistics
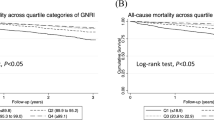
Baseline characteristics were descriptively presented and were tested using Student’s t test or chi squared test. Survival was represented graphically using the Kaplan-Meier method and analyzed using univariate and multivariate Cox regression. HRs were represented graphically using forest plots. Receiver operative characteristic (ROC) curves were used to evaluate the value of GNRI that could detect various causes of death. P values of <0.05 were considered significant.
Results
Baseline characteristics
We analyzed 1489 patients whose GNRI could be calculated and whose prognosis was clear. Table 1 shows baseline characteristics of patients based on GNRI. The mean value of GNRI was 87.60 (median 87.86). We divided patients based on the median value into a high (H) and low (L) group. The L group was older, and the percentage of ACE inhibitor, angiotensin receptor blocker, and vitamin D receptor agonist administration was lower. The L group had a higher rate of cardiovascular disease (CVD) history. Expectedly, the L group had a lower body mass index (BMI) and ALB values. Overall, the L group had significantly lower levels of electrolytes, which may have been due to a lack of intake. However, it is unknown whether the lower electrolyte levels is clinically meaningful. C-reactive protein levels were higher in the L group. All-cause death and infection-associated death were higher in the L group.
Mortality and causes of death
Figure 2 shows the Kaplan-Meier plot for survival rate in patients according to GNRI levels. Figures 3, 4, and 5 show Kaplan-Meier plots for cumulative incidence rates regarding infection-, CVD-, and malignancy-associated deaths. In the univariate analysis (Kaplan-Meier plot), the incidence of all-cause, infection-associated, and CVD-associated death was significantly higher in the L group. Multivariate analysis was then performed. Figure 6 shows the forest plot, which presents HRs of GNRI for death. In the multivariate analysis, there was no significant difference in CVD-associated death, and only all-cause and infection-associated death showed a significant association. These results indicate the usefulness of GNRI for disease prognosis, especially for infection-associated death.
Forest plot of GNRI for death. GNRI Geriatric Nutritional Risk Index, HR hazard ratio, CI confidence interval, CVD cardiovascular disease, DM diabetes mellitus, Hb hemoglobin, eGFR estimated glomerular filtration rate, ACEi, angiotensin-converting enzyme inhibitor, ARB angiotensin receptor blocker, P phosphate, CRP C-reactive protein
ROC curve of GNRI for predicting death
Because GNRI was originally synthesized from BW and ALB, we assessed whether BMI or ALB alone could sufficiently predict mortality. Figure 7 shows the ROC curve of GNRI predicting all-cause death, and Fig. 8 shows the ROC curve of GNRI predicting infection-associated death. GNRI had a superior ability to predict all-cause and infection-associated death compared to ALB alone. Although there was no significant difference in comparison with BMI, the area under the curve (AUC) of GNRI was higher for both all-cause and infection-associated death in appearance, and the predictive ability tended to be higher. Figure 9 shows stratified analysis by the ultrafiltration volume at first dialysis session for all-cause death. With high amount of ultrafiltration, the accuracy of prediction value of GNRI reduced.
Discussion
We compared the mortality of patients with high and low GNRI at the time of dialysis initiation. GNRI exhibited a good predictive ability not only during the maintenance dialysis phase but also during dialysis induction when the body weight is unstable or dietary intake may be decreasing. Further, among mortality rates, GNRI was strongly related to infection-associated death.
GNRI is a nutritional evaluation scale that was primarily developed for the elderly but is becoming increasingly used as a simple and objective indicator of prognosis in other conditions. In this study, there is novelty and clinically very meaningful in the point of usefulness of GNRI even when the items for calculating it is modified.
From our findings, patients with low GNRI exhibited a poor prognosis. In this group, there was a prevalence of factors associated with poor prognoses, such as old age, CVD history, and diabetes. Since the patient background is quite different, simple comparison with GNRI alone is difficult. It seems that the L group contains many patients with poor overall medical condition. Despite the mathematical adjustment for these factors above, complete adjustment is difficult. GNRI may comprehensively detect such “poor status.” Regarding the cause of the strong association with infection-associated death, an immunocompromised status caused by malnutrition [13, 14] may be a reason. However, a definite conclusion cannot be arrived at because leukocyte fraction or immunoglobulin was not measured. We are considering these assessments in the future.
At the time of dialysis initiation, BW and BMI increase because of body fluid retention, and ALB decreases because of dilution. These modifications impair the accuracy of GNRI as shown in Fig. 9. However, our results showed the usability of GNRI in this condition. Probably the value of GNRI would be more accurate to predict the prognosis if there are no factors to modify. However, this research is meaningful because it shows that prognosis prediction is possible to some extent even if predictive accuracy is lowered by additional modifying factors. It is already known that the stable GNRI value during maintenance dialysis period is useful for prognosis prediction. Hence, this will be a more wonderful research if we can compare the prediction accuracy of GNRI values during the introduction period and stable period. Unfortunately, values of GNRI after discharge cannot be collected and are unknown because many patients are transferring to other clinics after dialysis initiation. Although it is regrettable that there is no data during stable maintenance period, but in the sense of indicating that GNRI works effectively with the novelty of “dialysis induction period,” large number of patients, and with a tremendously high tracking rate, this report seems to be very meaningful.
Our study had some limitations. First, since this was an observational study, a selection bias is expected regarding whether physicians treated patients with end-stage kidney disease and whether poor nutritional status may have resulted in a poor prognosis. Second, regarding the reason for the strong association between GNRI and infection-associated death, we did not measure values such as fractionation of white blood cells or immunoglobulin levels. Hence, further investigation of this association could not be conducted. Third, when the amount of fluid removal was excessive, the accuracy of predictive value reduced. Therefore, in the cases with too much fluid removal compared to this study, the results of this study may not be applicable.
Conclusions
At the time of dialysis initiation, patients with low GNRI values are associated with a poor prognosis, particularly with regard to infection-associated death. The prediction accuracy of GNRI for all-cause and infection-associated death seems better than that of BMI or ALB alone.
Abbreviations
- ALB:
-
Albumin
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- BW:
-
Body weight
- CVD:
-
Cardiovascular disease
- GNRI:
-
Geriatric nutritional risk index
- HR:
-
Hazard ratio
- IBW:
-
Ideal body weight
- ROC:
-
Receiver operator characteristic
- UFV:
-
Ultrafiltration volume
References
Masakane I, Nakai S, Ogata S, Kimata N, Hanafusa N, Hamano T, et al. An overview of regular dialysis treatment in Japan (As of 31 December 2013). Ther Apher Dial. 2015;19:540–74.
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82:777–83.
Kokura Y, Maeda K, Wakabayashi H, Nishioka S, Higashi S. High nutritional-related risk on admission predicts less improvement of functional independence measure in geriatric stroke patients: a retrospective cohort study. J Stroke Cerebrovasc Dis. 2016;25:1335–41.
Kinugasa Y, Kato M, Sugihara S, Hirai M, Yamada K, Yanagihara K, et al. Geriatric nutritional risk index predicts functional dependency and mortality in patients with heart failure with preserved ejection fraction. Circ J. 2013;77:705–11.
Kalantar-Zadeh K, Anker SD, Horwich TB, Fonarow GC. Nutritional and anti-inflammatory interventions in chronic heart failure. Am J Cardiol. 2008;101(11A):89E–103E.
Abd-El-Gawad WM, Abou-Hashem RM, El Maraghy MO, Amin GE. The validity of Geriatric Nutrition Risk Index: simple tool for prediction of nutritional-related complication of hospitalized elderly patients. Comparison with mini nutritional assessment. Clin Nutr. 2014;33:1108–16.
Gamaletsou MN, Poulia KA, Karageorgou D, Yannakoulia M, Ziakas PD, Zampelas A, et al. Nutritional risk as predictor for healthcare-associated infection among hospitalized elderly patients in the acute care setting. J Hosp Infect. 2012;80:168–72.
Edalat-Nejad M, Zameni F, Qlich-Khani M, Salehi F. Geriatric Nutritional Risk Index: a mortality predictor in hemodialysis patients. Saudi J Kidney Dis Transpl. 2015;26:302–8.
Chen HY, Chiu YL, Hsu SP, Pai MF, Yang JY, Wu HY, et al. Reappraisal of effects of serum chemerin and adiponectin levels and nutritional status on cardiovascular outcomes in prevalent hemodialysis patients. Sci Rep. 2016;6:34128.
Tsai MT, Liu HC, Huang TP. The impact of malnutritional status on survival in elderly hemodialysis patients. J Chin Med Assoc. 2016;79:309–13.
Tanaka A, Inaguma D, Shinjo H, Murata M, Takeda A, Aichi Cohort Study of Prognosis in Patients Newly Initiated into Dialysis Study G. Presence of atrial fibrillation at the time of dialysis initiation is associated with mortality and cardiovascular events. Nephron. 2016;132:86–92.
Hishida M, Tamai H, Morinaga T, Maekawa M, Aoki T, Tomida H, et al. Aichi cohort study of the prognosis in patients newly initiated into dialysis (AICOPP): baseline characteristics and trends observed in diabetic nephropathy. Clin Exp Nephrol. 2016;20:795–807.
Chandra RK. Nutritional regulation of immunity and risk of infection in old age. Immunology. 1989;67:141–7.
Pifer TB, McCullough KP, Port FK, Goodkin DA, Maroni BJ, Held PJ, et al. Mortality risk in hemodialysis patients and changes in nutritional indicators: DOPPS. Kidney Int. 2002;62:2238–45.
Acknowledgements
We acknowledge the support of the following members of the Aichi Cohort Study of Prognosis in Patients Newly Initiated into Dialysis (AICOPP) who participated in this study: Hirofumi Tamai (Anjo Kosei Hospital), Tomohiko Naruse (Kasugai Municipal Hospital), Kei Kurata (Tosei General Hospital), Hideto Oishi (Komaki City Hospital), Isao Aoyama (Japan Community Healthcare Organization Chukyo Hospital), Hiroshi Ogawa (Shinseikai Daiichi Hospital), Hiroko Kushimoto (Nishichita General Hospital), Hideaki Shimizu (Chubu-Rosai Hospital), Junichiro Yamamoto (Tsushima City Hospital), Hisashi Kurata (Toyota Kosei Hospital), Taishi Yamakawa (Toyohashi Municipal Hospital), Takaaki Yaomura (Nagoya Medical Center), Hirotake Kasuga (Nagoya Kyouritsu Hospital), Shizunori Ichida (Japanese Red Cross Nagoya Daiichi Hospital), Shoichi Maruyama (Nagoya University Graduate School of Medicine), Noritoshi Kato (Nagoya University Graduate School of Medicine), Seiichi Matsuo (Nagoya University Graduate School of Medicine), Shigehisa Koide (Fujita Health University Hospital), and Yukio Yuzawa (Fujita Health University Hospital).
We would like to thank Editage (www.editage.jp) for the English language editing.
Funding
Not applicable.
Availability of data and materials
Please contact the author for data requests.
Authors’ contributions
DI designed the study. AT performed the statistical analysis and wrote the manuscript. All authors participated in the care of the patients. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Institutional Review Board of Nagoya Daini Red Cross Hospital (No. IRB20110823-3) and was conducted under the Declaration of Helsinki. Patient consent was obtained for the study.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tanaka, A., Inaguma, D., Shinjo, H. et al. Relationship between mortality and Geriatric Nutritional Risk Index (GNRI) at the time of dialysis initiation: a prospective multicenter cohort study. Ren Replace Ther 3, 27 (2017). https://doi.org/10.1186/s41100-017-0108-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-017-0108-9