Abstract
Background
Recognizing and identifying latent safety threats (LSTs) before patient care commences is crucial, aiding leaders in ensuring hospital readiness and extending its impact beyond patient safety alone. This study evaluated the effectiveness of a combination of Simulation-based Clinical Systems Testing (SbCST) with Healthcare Failure Mode and Effect Analysis (HFMEA) with regard to mitigating LSTs within a newly constructed hospital.
Methods
Three phases of the combined SbCST and HFMEA approach were implemented across all hospital settings. The scenarios tested system functionalities, team responses, and resource availability. The threats thus identified were categorized into system-related issues, human issues, and resource issues, after which they were prioritized and addressed using mitigation strategies. Reassessment confirmed the effectiveness of these strategies before hospital commissioning.
Results
More than 76% of the LSTs were mitigated through the combined approach. System-related issues, such as nonfunctional communication devices and faulty elevators, were addressed by leadership. Human issues such as miscommunication and nonadherence to hospital policy led to improvements in interprofessional communication and teamwork. Resource issues, including missing equipment and risks of oxygen explosion, were addressed through procurement, maintenance, and staff training for equipment preparation.
Conclusion
The SbCST and HFMEA were highly effective with regard to proactively identifying and mitigating LSTs across all aspects of hospital preparedness. This systematic and comprehensive approach offers a valuable tool for enhancing patient safety in new healthcare facilities, thereby potentially setting a new standard for proactive hazard identification and risk management in the context of healthcare construction and commissioning.
Similar content being viewed by others
Introduction
Healthcare simulation-based training has been widely recognized for its effectiveness with regard to enhancing the knowledge, skills, and attitudes of healthcare providers across a variety of disciplines [1]. Simulation-based training has a positive impact on the ability of staff to manage high-stress situations, leading to improved confidence, skills, and knowledge among participants [2,3,4]. Beyond the level of individual development, simulation-based approaches have also been identified as invaluable tools for assessing and optimizing the operational readiness of healthcare facilities. In the design and construction phases of modern healthcare facilities, relevant leaders are increasingly incorporating features that support safe and efficient patient and staff care, such as controlled indoor environments, optimized interior designs, and well-planned area layouts, into the infrastructure [5, 6]. However, poorly conceived layouts or architectural decisions can inadvertently compromise patient safety by introducing systemic flaws and inefficiencies that ultimately elevate the risk of latent safety threats (LSTs) [7,8,9]. While human factors and ergonomics (HFE) has gained recognition for its importance in healthcare quality and patient safety, existing evidence underscores its potential to enhance the quality of care and patient safety through healthcare system redesign. Numerous models exist that can provide a deeper understanding of HFE conditions and contribute to the development of frameworks aimed at addressing ongoing design challenges to improve patient safety, human factors, and work environment solutions [10, 11].
Accordingly, in situ simulation-based approaches are now being utilized postconstruction to assess and mitigate the risk of LSTs in newly built healthcare facilities before they receive patients [5, 8, 9, 12,13,14]. This approach has proven to be instrumental with regard to evaluating the healthcare system’s preparedness for diverse scenarios, including disasters. Studies have further demonstrated how simulation can inform the development of new disaster response protocols that are critical for managing patient triage, resource allocation, and public communication [3, 15]. In conjunction with simulation testing, Healthcare Failure Mode and Effect Analysis (HFMEA) can be employed as a systematic tool to identify, categorize, prioritize, and mitigate the risk of LSTs. Within this framework, the notion of failure modes represents the inability of hospital-based systems to perform their intended functions, while the concept of effects refers to the potential consequences of these failures [16,17,18]. The HFMEA assigns numerical hazard values based on a two-pronged analysis: (1) the severity of the potential impact on patients and clinical staff and (2) the probability of the failure mode occurring [19].
Despite the increasingly widespread use of in situ simulation testing, there may be a need for further attention to its applicability and specific use in evaluating hospital readiness prior to patient admission [3, 13,14,15,16,17,18, 20,21,22,23,24,25].
This research gap limits our understanding of how preopening evaluations can inform the development of solutions and optimize hospital preparedness. Therefore, this paper aims to critically evaluate the efficacy of in situ simulation testing with regard to establishing a new hospital by assessing its effectiveness with respect to recognizing, mitigating, and addressing LSTs related to demands imposed on hospital systems, patient transportation pathways, equipment and team readiness, and overall operational efficiency.
Setting
This prospective study was conducted at Women’s Health Hospital (WHH), a leading women’s health facility located in King Abdulaziz Medical City, the largest medical complex in Saudi Arabia. WHH is the largest hospital specializing in women’s health in the Gulf area. It boasts a total capacity of 349 beds catering to adult female inpatients, along with a 96-bed neonatal intensive care unit (NICU) and intermediate care nursery (ICN). Additionally, WHH houses day treatment facilities, a 27-bed labor and delivery unit (L&D), four operating rooms (OR), and a 27-bed gynecology obstetric triage assessment and management unit (GOTAMU).
Methods
The study spanned 14 months, from July 2022 to September 2023, and followed a two-stage approach.
Stage 1: Development and planning. This initial stage focused on establishing a multidisciplinary team, identifying testing objectives related to high-stress situations and healthcare system readiness, and designing relevant scenarios.
Stage 2: Implementation. This subsequent stage encompassed three distinct phases: testing hospital infrastructure and patient transfer pathways under simulated crisis situations, evaluating equipment and team readiness through simulated crisis scenarios, and retesting the LSTs identified, along with corresponding mitigation strategies, in response to crisis situations (Fig. 1).
Development and planning
The establishment of a multidisciplinary collaborative workgroup
Our simulation-based clinical systems testing (SbCST) program aimed to uncover and address LSTs that emerge before and during patient transfer to the new Women’s Health Hospital (WHH). These LSTs could pertain to the following issues:
-
System and patient transportation pathways both within WHH and from the old hospital.
-
Equipment readiness and functionality.
-
Team preparedness and responses in high-stress situations.
To achieve this goal, we established a multidisciplinary team comprising clinical leaders, simulation experts, and frontline staff. The team collectively decided to employ the HFMA testing as an effective strategy for detecting and evaluating LSTs, aiming to enhance systems and ultimately improve patient safety [17, 26, 27].
Based on brainstorming sessions and interviews, we identified high-frequency/low-acuity (e.g., routine admissions) and low-frequency/high-acuity events that could inform subsequent steps of the process:
-
Needs assessment: This step established key objectives such as identifying testing priorities, developing process maps, designing scenarios, and defining roles within the collaborative workgroup.
-
Shared mental model: The cultivation of a clear understanding of the purpose and goals of the scenarios among all participants (including stakeholders unfamiliar with SbCST) was crucial for ensuring accurate analysis and open communication.
-
Testing objectives: Clear communication and repetition were emphasized when conveying objectives and roles to stakeholders, clinical leaders, and participants, thus maximizing understanding and engagement. This process involved leveraging routine patient movements to assess adherence to safe design principles, such as minimizing interruptions, reducing excessive walking, and optimizing equipment placement [11].
Execution team
The Paediatric Simulation Training & Education Program (PediSTEP) team, working alongside clinical leaders from the obstetrics and gynecology (Ob-Gyn) department, NICU, and nursing services, formed the execution team. These participants planned and executed the program collaboratively; reviewed the proposed scenarios for feasibility, validity, and reliability, and assigned team members from relevant medical and allied services.
Process mapping
Detailed process maps outlining each event sequence were constructed through collaboration between team members and frontline staff. Every activity, decision point, set of personnel, supply source, set of equipment, and participant role was clearly identified for each clinical situation, process, or workflow scheduled for testing (Fig. 1).
Comprehensive in situ testing
The simulations encompassed both clinical and nonclinical areas (patient care, public spaces, support services, administration) to ensure a comprehensive and realistic evaluation before patient arrival. This holistic approach facilitated the functional assessment, system process evaluation, and early identification of potential patient safety concerns, thus offering more benefits than testing focused on limited hospital settings.
Scenario development
In collaboration with clinicians from each area, the execution team developed in situ simulation sessions focusing on routine clinical practice and crisis situations that were relevant to specific patient populations. This partnership ensured both clinical fidelity and alignment with the SbCST objectives. Simulationists anchored each task to a safe design principle, thus facilitating the robust testing of multiple elements within each scenario. The process of prioritization focused on frequent, urgent, challenging, new, or high-risk situations. Clinical complexity and complex medical decision-making were minimized to maintain a focus on system- and process-related aspects. The number and length of the scenarios depended on the scope of the evaluation, the new areas under investigation, and the distinct clinical departments involved. Individual scenario complexity influenced the duration, participant numbers, observer requirements, and debriefing length of the process.
Simulation preparation
During the week prior to each SbCST, simulationists meticulously assembled event materials (rosters, scripts, checklists, guides, etc.). Clinical leaders ensured that team members who were going to participate in the scenarios were notified and received confirmation, thereby extending communication to relevant services and operational units to guarantee comprehensive awareness and coordination.
Implementation phases
The implementation stage involved three distinct phases, each of which had a specific goal:
-
Phase I: Infrastructure and transfer pathways: This phase involved testing the functionality of hospital infrastructure and the effectiveness of patient transfer pathways both within WHH and between the old hospital and WHH.
-
Phase II: Equipment and team readiness: This phase focused on evaluating the preparedness of equipment and team responses under simulated high-stress situations.
-
Phase III: LST retesting and mitigation: This phase involved retesting previous LSTs and evaluating the effectiveness of the implementation of mitigation strategies drawn from phases I and II.
Simulation pre-briefing and orientation
Before each simulation session, a pre-briefing was used to establish the scenario objectives and ensure the overall flow of the process. Notably, this pre-briefing focused on the task of ensuring a psychologically safe environment in which individual performance evaluation was not the main area of focus. This approach aimed to encourage open and honest discussion, which is particularly valuable for stakeholders and leaders. Following the prebriefing, participants familiarized themselves with the space, while observers strategically positioned themselves in designated locations. The observers comprised the nursing manager, simulationists, project management office members, department managers, and clinical department chairpersons from the relevant units. They actively engaged in the debriefing session, bringing their notes and comments for discussion.
Data collection through debriefing
Multidisciplinary teams of frontline staff implemented care scenarios in each clinical area under examination. Structured and facilitated debriefing sessions were used to identify latent conditions and potential active failures related to the architectural design. Simulation team members meticulously transcribed these sessions into a predefined template (Additional file 1) [17]. The simulationist participated actively in this process, inputting information into a preformatted reporting template to facilitate the comprehensive documentation of the identified issues. Detailed notes were kept to outline each potential safety threat or system inefficiency alongside the corresponding potential impact on patient safety, workflow, or process efficiency. For each scenario, one or two simulationists independently completed checklists to ensure a thorough evaluation. In the event of any disagreement among simulationists, the matter would undergo further review by the simulation program chair before finalizing the report.
Debriefing techniques
Immediate debriefing sessions followed each simulation; these sessions were based on a standardized approach that involved scoring checklists (Additional files 1 and 2). Importantly, SbCST debriefing techniques differ significantly from traditional, education-based debriefing techniques. The SbCST approach is facilitator-focused; the facilitator from the simulation team of PediSTEP prompts reactions for each scenario step [28]. This approach guides the group in identifying safety threats and their potential impacts on patient/staff safety, workflow, process efficiency, and equipment/technology functionality [17, 28, 29]. This focused exploration ensures an in-depth evaluation of aspects that are crucial for assessing clinical scenarios in the context of hospital design.
Data analysis
Hazard analysis and HFMEA scoring
Following each simulation event, a dedicated scoring group is convened to conduct HFMEA. This group comprises departmental and service line leaders, institutional operational leaders, and executive leaders, thereby representing a multidisciplinary perspective that can be used to evaluate potential risks. The HFMEA serves as a proactive risk assessment tool, guiding the team in analyzing healthcare processes. High-risk LSTs refer to incidents for which the risk priority number (RPN) exceeds 32 (Additional file 2) [17].
The simulationists utilized the HFMEA to facilitate the scoring process. They reviewed, evaluated, and scored each potential LST identified during the debriefing sessions. Each LST underwent a meticulous assessment, in which it was assigned scores for occurrence, detection, and severity. These scores then informed categorization based on system-, human-, and resource-related issues.
Following the scoring process, a comprehensive report was generated, which detailed each LST alongside its corresponding score and RPN categorization. This report was distributed to stakeholders, clinical leaders, and the quality team, thus ensuring transparent communication and proactive mitigation of potential risks identified during the simulation events.
Ethical statement
Ethics approval for the study was obtained from our local Institutional Review Board (IRB) prior to data collection (RO/WE/WS/008/2024).
Scenario scope and risk analysis of the SbCST
The SbCST spanned three phases, including 34 scenarios extending across various hospital services, including neonatal intensive care units, GOTAMU, operating rooms, wards, and outpatient clinics (Table 1).
-
Phase I: Infrastructure and transfer pathways (16 scenarios): This phase involved assessing hospital infrastructure functionality and coordination with a focus on patient transfers both within WHH and between old and new facilities.
-
Phase II: Equipment and team readiness (12 scenarios): This phase focused on evaluating the preparedness of equipment and team responses under simulated high-stress situations.
-
Phase III: LST retesting and mitigation (6 scenarios): This phase entailed reassessing scenarios drawn from phases 1 and 2 for safety and readiness before hospital commissioning.
The scenarios involved the participation of multidisciplinary teams such as military and nursing staff, obstetrics and gynecology teams, neonatal intensive care units, anesthesia units, laboratories, and social care units (Table 1).
Outcomes of the SbCST/HFMEA testing
Identified LSTs
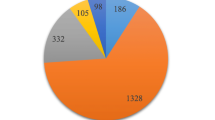
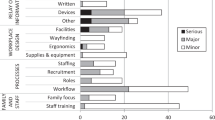
A total of 136 LSTs were identified through HFMEA risk analysis, in which context phases I and II revealed more LSTs (94) than did phase III (24). Of these LSTs, 97 were considered to be high risk (RPN > 32), and 39 were considered to be low risk (RPN < 32). The number of high-risk threats per scenario varied from 0 to 7, with scenarios 7 and 10 in phase 1 and scenario 11 in phase 2 representing the extremes (Table 2). The highest threats thus detected occurred in phase I and phase II rather than in phase III. Following the application of phase I and II testing, action plans were derived for the mitigation of the risks thus detected (Table 3). These action plans, which contained recommended actions and changes, were submitted to a leadership panel to allow the recommended changes to be implemented.
LST categorization and action plans
Based on the risk analysis, action plans were developed to address potential LSTs (Table 3). LSTs were further categorized into three groups:
-
System-related issues: Unclear/low-tone code announcements, malfunctioning equipment (critical care response team (CCRT), pager, phones, computers, Health Information System (HIS)), inaccessible elevators, and lack of policy adherence and understanding of responsibilities, which is a major human factor, led to system-related failures such as improper code announcement. These failures significantly impacted the response sequence system.
-
Human issues: Delays in code activation (2–25 min), incorrect/incomplete information from code agents, unavailable teams (such as anesthesia or imaging teams), the lack of prepared operating rooms, and miscommunication among responders contributed to human factor-related failures.
-
Resource issues: The lack of available resources such as cardiotocography (CTG) machines, ultrasound machines, portable Doppler devices, oxygen tanks, personal protective equipment (PPEs), medications, operating room equipment, and emergency transport boxes containing essential emergency equipment required during patient transfer, alongside inadequate oxygen holder design, were categorized as resource-related failures. To differentiate between issues related to availability and those due to the hospital not yet being operational, we considered the timing of the simulations. As phases II and III were conducted before the hospital’s opening, any unavailable resources during this period were attributed to resource-related failures rather than issues arising from the hospital not being operational.
Discussion
The combination of SbCST along with HFMEA assessment effectively identifies and categorizes LSTs. This approach aids in exploring potential risks and prioritizing their resolution before they impact patients negatively. Detection of hazards and risks facilitates the prioritization of the process of addressing and retesting before patients are negatively impacted [30]. This study aimed to use in situ simulation testing processes alongside HFMEA tools to recognize, mitigate, and address LST-imposed demands on hospital systems, transportation processes, equipment, and team readiness. The outcomes of the three phases involved in the SbCST and HFMEA approaches enabled threats to be categorized into three areas: (1) system-related issues, (2) human issues, and (3) resource issues. The findings concerning phase III showed that the LSTs decreased by 76%, thus suggesting two conclusions: (1) the risk mitigation solutions were effective in some cases, and (2) the actions taken did not solve each problem; thus, additional modifications were needed. Leadership was able to correct 100% of the LSTs thus identified before the commencement of patient admissions to the hospital.
All system-related risks identified, including delays in code announcements, elevator failures, errors in the paging system, malfunctions in phones and computers, and errors in the HIS, were addressed by leadership (Table 3). These system-related issues can lead to various negative consequences, underscoring the urgency of action. For instance, the malfunctioning code activation system was noted in multiple clinical areas, prompting a special meeting and discussion with the communication department to address this issue.
Similarly, all human-related LSTs that were included in this study were addressed by leaders (Table 3). The LSTs thus identified included delayed and/or absent code activation and team response for two reasons. First, miscommunication between healthcare individuals may have occurred, such as situations in which incomplete or incorrect pink code (missing baby) information was provided. Such failure modes could result in a delay in the location of missing infants by military police. A link between ineffective interprofessional communication and poor patient outcomes has previously been documented [31, 32]. Foronda et al. reported that interprofessional miscommunication can lead to delayed patient treatment, patient dissatisfaction, medical errors, and death [33].
All LSTs pertaining to resources were also addressed by leadership. Between 39 and 85% of documented cases of patient safety hazards were related to equipment and supplies [13, 34]. In this study, some required equipment and supplies were not available. For example, a lack of operating room equipment could prevent care teams from performing surgery or securing patients’ airways in the operating room. Additionally, unavailable emergency transport boxes could result in a failure to manage the risks associated with patient transfers.
Our findings underscored the importance of HFMEA testing in identifying and addressing LSTs, ultimately improving patient safety. Further research and reporting into the success of SbCST is essential to understand its effectiveness and promote its wider adoption, fostering a healthcare environment where patient safety is integral to care delivery. Additionally, it aids leaders in ensuring hospital readiness, extending its impact beyond patient safety alone.
Strengths and limitations
This study has three major strengths. First, conducting the work prior to hospital commissioning, thereby avoiding the bustling patient environment, is a noteworthy advantage. Second, the study employed a rigorous methodology to identify, categorize, prioritize, and mitigate the included LSTs by using in situ simulation in conjunction with the HFMEA tool and group debriefings. This approach may facilitate the reporting of credible findings and ensure that trustworthiness, validity, and reliability are maintained. Third, the reassessment phase allowed us to retest and determine the effectiveness of the mitigation strategies before hospital commissioning. However, it is important to acknowledge the limited generalizability of simulation findings to other institutions due to the inherent differences between healthcare facilities.
This study is subject to several limitations. First, the simulation program was conducted after the completion of the hospital infrastructure, thereby limiting its impact on major design changes in the hospital. Early engagement of the hospital architectural team is crucial in the schematic design evaluation process to address this limitation effectively. Second, while the simulation program focused on hospital readiness, team response, equipment, and patient transfer, it did not encompass other crucial components of healthcare safety such as medication safety, fall prevention, and prevention of hospital-acquired infections. Although these components may have established programs from the old hospital, they remain important safety measures to be considered in a new clinical environment. Third, the project has a large scope, and more than one year of concerted effort was required for its implementation. This process required coordination with all hospital departments, stakeholders, healthcare providers, and simulation experts, which would be challenging in other hospital settings due to the need to free the scheduled participants from their clinical duties for the duration of hospital readiness testing. Fourth, all scenarios and debriefings included in this research were aimed at testing hospital readiness rather than staff competence. This research may thus not be relevant for researchers aiming to evaluate and improve health team competencies. Thus, further healthcare simulation research is needed to investigate training with regard to assessing and improving team readiness prior to the provision of patient services. Fifth, the presence of senior observers may have induced stress among participants and influenced their behavior. However, during the pre-briefing sessions, we emphasized to participants that the primary goal of these simulations was to assess system functionality and ensure safety measures, rather than to evaluate individual skills or knowledge. We believe that by emphasizing this point, we minimized any potential impact on participants’ performance due to the observers’ presence. To mitigate this effect further, the use of video cameras for remote observation could be considered.
Conclusion
SbCST and HFMEA represent powerful and proactive approaches to patient safety, as demonstrated by this study and supporting research on this topic. They facilitate the detection and resolution of LSTs before the hospital’s actual commissioning. By addressing the limitations of traditional methods and embracing continuous improvement, this approach offers immense potential to establish safer healthcare environments for both patients and providers.
Availability of data and materials
The data underlying this article will be shared on reasonable request to the corresponding author.
Abbreviations
- LSTs:
-
Latent szafety threats
- SbCST:
-
Simulation-based Clinical Systems Testing
- HFMEA:
-
Healthcare Failure Mode and Effect Analysis
- WHH:
-
Women’s Health Hospital
- NICU:
-
Neonatal intensive care unit
- ICN:
-
Intermediate care nursery
- L&D:
-
Labor and delivery
- OR:
-
Operating room
- GOTAMO:
-
Gynecology Obstetric Triage Assessment and Management Unit
- PediSTEP:
-
Pediatric Simulation Training & Education Program
- Ob-Gyn:
-
Obstetrics and gynecology
- RPN:
-
Risk priority number
- CCRT:
-
Critical care response team
- HIS:
-
Health information system
- CTG:
-
Cardiotocography
References
Thornton E, Brook OR, Mendiratta-Lala M, Hallett DT, Kruskal JB. Application of failure mode and effect analysis in a radiology department. Radiographics a Rev Publ Radiol Soc North Am Inc. 2011;31(1):281–93.
Dubé M, Kaba A, Cronin T, Barnes S, Fuselli T, Grant V. COVID-19 pandemic preparation: using simulation for systems-based learning to prepare the largest healthcare workforce and system in Canada. Adv Simul (London, England). 2020;5:22.
Arboleda CA, Abraham DM, Lubitz R. Simulation as a tool to assess the vulnerability of the operation of a health care facility. J Perform Constr Facil. 2007;21(4):302–12.
Donohue A, Lamdark T, Lavin J, Hupalo N, Wullschleger M. Implementation of periop disaster response exercise program at gold coast health. Prehosp Disaster Med. 2019;34(s1):s81–s81.
Liu HC, Zhang LJ, Ping YJ, Wang L. Failure mode and effects analysis for proactive healthcare risk evaluation: a systematic literature review. J Eval Clin Pract. 2020;26(4):1320–37.
Register S, Brown M, White ML. Using healthcare simulation in space planning to improve efficiency and effectiveness within the healthcare system. Heal Syst. 2019;8(3):184–9. https://doi.org/10.1080/20476965.2019.1569482.
Reason J. Human error: Models and management. Br Med J. 2000;320(7237):768–70.
Adler MD, Mobley BL, Eppich WJ, Lappe M, Green M, Mangold K. Use of simulation to test systems and prepare staff for a new hospital transition. J Patient Saf. 2018;14(3):143–7.
Levi L, Bregman D, Geva H, Revach M. Hospital disaster management simulation system. Prehosp Disaster Med. 1998;13(1):22–7.
Xie A, Carayon P. A systematic review of human factors and ergonomics (HFE)-based healthcare system redesign for quality of care and patient safety. Ergonomics. 2015;58(1):33–49.
Taylor E, Hignett S. DEEP SCOPE: A Framework for Safe Healthcare Design. Int J Environ Res Public Health. 2021;18(15):7780.
Ulrich RS, Zimring C, Zhu X, DuBose J, Seo HB, Choi YS, Quan X, Joseph A. A review of the research literature on evidence-based healthcare design. HERD. 2008;1(3):61–125.
Ventre KM, Barry JS, Davis D, Baiamontea VL, Wentworth AC, Pietras M, et al. Using in situ simulation to evaluate operational readiness of a children’s hospital-based obstetrics unit. Simul Healthc. 2014;9(2):102–11.
Kaji AH, Bair A, Okuda Y, Kobayashi L, Khare R, Vozenilek J. Defining systems expertise: effective simulation at the organizational level - implications for patient safety, disaster surge capacity, and facilitating the systems interface. Acad Emerg Med. 2008;15(11):1098–103.
Thornton E, Brook OR, Mendiratta-Lala M, Hallett DT, Kruskal JB. Application of failure mode and effect analysis in a radiology department. Radiographics. 2011;31(1):281–93.
Holmes J, Chipman M, Barbour T, DiLisio C, Morejon O, Graydon-Baker E, et al. A simulation systems testing program using HFMEA methodology can effectively identify and mitigate latent safety threats for a new on-site helipad. Jt Comm J Qual patient Saf. 2022;48(1):12–24.
Colman N, Doughty C, Arnold J, Stone K, Reid J, Dalpiaz A, et al. Simulation-based clinical systems testing for healthcare spaces: from intake through implementation. Adv Simul. 2019;4(1):1–9.
Colman N, Edmond MB, Dalpiaz A, Walter S, Miller DC, Hebbar K. Designing for patient safety and efficiency: simulation-based hospital design testing. Heal Environ Res Des J. 2020;13(4):68–80.
DeRosier J, Stalhandske E, Bagian JP, Nudell T. Using health care failure mode and effect analysis: the VA National Center for Patient Safety’s prospective risk analysis system. Jt Comm J Qual Improv. 2002;28(5):248-67,209.
Kaba A, Barnes S. Commissioning simulations to test new healthcare facilities: a proactive and innovative approach to healthcare system safety. Adv Simul. 2019;4(1):1–9.
Patterson MD, Geis GL, Falcone RA, LeMaster T, Wears RL. In situ simulation: Detection of safety threats and teamwork training in a high risk emergency department. BMJ Qual Saf. 2013;22(6):468–77.
Brokalaki HJ, Brokalakis JD, Digenis GE, Baltopoulos G, Anthopoulos L, Karvountzis G. Intrahospital transportation: monitoring and risks. Intensive Crit Care Nurs. 1996;12(3):183–6.
Carson KJ, Drew BJ. Electrocardiographic changes in critically ill adults during intrahospital transport. Prog Cardiovasc Nurs. 1994;9(4):4–12.
Caruana M, Culp K. Intrahospital transport of the critically ill adult: a research review and implications. Dimens Crit Care Nurs. 1998;17(3):146–56.
De Cosmo G, Primieri P, Mascia A, Gualtieri E, Bonomo V, Villani A. Intra-hospital transport of the anaesthetized patient. Eur J Anaesthesiol. 1993;10(3):231–4.
Passarella C. Failure modes and effects analysis. Control. 2018;31(10):72–3.
Nielsen DS, Dieckmann P, Mohr M, Mitchell AU, Østergaard D. Augmenting health care failure modes and effects analysis with simulation. Simul Healthc. 2014;9(1):48–55.
Colman N, Dalpiaz A, Walter S, Chambers MS, Hebbar KB. SAFEE: a debriefing tool to identify latent conditions in simulation-based hospital design testing. Adv Simul. 2020;5(1):1–12.
Dubé MM, Reid J, Kaba A, Cheng A, Eppich W, Grant V, et al. PEARLS for systems integration: a modified PEARLS framework for debriefing systems-focused simulations. Simul Healthc. 2019;14(5):333–42.
Geis GL, Pio B, Pendergrass TL, Moyer MR, Patterson MD. Simulation to assess the safety of new healthcare teams and new facilities. Simul Healthc. 2011;6(3):125–33.
Vermeir P, Vandijck D, Degroote S, Peleman R, Verhaeghe R, Mortier E, et al. Communication in healthcare: a narrative review of the literature and practical recommendations. Int J Clin Pract. 2015;69(11):1257–67.
Stewart MA. Stuck in the middle: the impact of collaborative interprofessional communication on patient expectations. Shoulder Elb. 2018;10(1):66–72.
Foronda C, MacWilliams B, McArthur E. Interprofessional communication in healthcare: an integrative review. Nurse Educ Pract. 2016;19:36–40. https://doi.org/10.1016/j.nepr.2016.04.005.
Beckmann U, Gillies DM, Berenholtz SM, Wu AW, Pronovost P. Incidents relating to the intra-hospital transfer of critically ill patients. Intensive Care Med. 2004;30(8):1579–85.
Acknowledgements
We would like to thank Dr. Abdulaleem Alatassi from the Department of Quality and Patient Safety for his valuable support of this project.
Funding
None.
Author information
Authors and Affiliations
Contributions
Tarek Hazwani: conceptualization, methodology, investigation, data curation, supervision, and writing—original draft.
Heba Hamam and Angela Caswell: conceptualization, investigation, data curation, and writing—original draft.
Azza Madkhaly and Saif Al Saif: conceptualization and investigation.
Zahra Al Hassan and Reem Al Sweilem: methodology, data curation, and formal analysis.
Asma Arabi: data curation, formal analysis, and writing—original draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for the study was obtained from our local Institutional Review Board (IRB) prior to data collection (RO/WE/WS/008/2024). As there are no identifiers were collected, the IRB considered the study exempt from the need for informed consent.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hazwani, T., Hamam, H., Caswell, A. et al. Proactive patient safety: enhancing hospital readiness through simulation-based clinical systems testing and healthcare failure mode and effect analysis. Adv Simul 9, 26 (2024). https://doi.org/10.1186/s41077-024-00298-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41077-024-00298-z