Abstract
Introduction
Stress can affect the ability to acquire technical skills. Simulation-based training (SBT) courses allow surgical trainees to train their technical skills away from stressful clinical environments. Trainees’ subjective experiences of stress during SBT courses on laparoscopic surgery remains understudied. Here, we explored the subjective stress experiences of surgical trainees during mandatory laparoscopic SBT courses. We aimed to obtain a broader understanding of which factors of the simulation training the trainees perceived as eliciting stress.
Methods
A qualitative study with semistructured individual interviews was undertaken to explore trainees’ subjective experiences of stress. Twenty surgical trainees participated while attending courses at a national training center for advanced laparoscopic surgery. Questions explored trainees’ stress experiences during the SBT courses with a focus on perceived stressors related to laparoscopic simulation training on two box-trainers and one virtual reality simulator. Interview data were analyzed using inductive, qualitative content analysis methods to identify codes, categories, and themes.
Results
Findings indicated that trainees have a variety of stress experiences during laparoscopic SBT. Three main themes were identified to be related to stress experiences: simulation task requirements, psychomotor skill levels and internal pressures, with subcategories such as task difficulty and time requirements, unrealistic haptic feedback and realism of graphics, inconsistent and poor technical performance, and self-imposed pressures and socio-evaluative threats.
Conclusions
Insights into surgical trainees’ experience of stress during laparoscopic SBT courses showed that some stress experiences were directly related to simulation training, while others were of psychological nature. The technical and efficiency requirements of simulation tasks elicited stress experiences among trainees with less laparoscopic experience and lower levels of psychomotor skills. Self-imposed pressures played an integral part in how trainees mobilized and performed during the courses, suggesting that levels of stress might enhance laparoscopic simulation performance. For course facilitators aiming at optimizing future laparoscopic SBT courses, attending to the realism, providing clarity about learning objectives, and having awareness of individual differences among trainees’ technical level when designing the simulation tasks, would be beneficial. Equally important to the laparoscopic SBT is to create a psychological safe learning space in order to reduce the internal pressures of trainees.
Similar content being viewed by others
Introduction
Surgical simulation-based training (SBT) allows surgical trainees to practice in an environment free of operating room specific stressors and without putting patients at risk [1]. In the field of laparoscopic surgery, simulators have long been utilized for practicing as adjuncts to the traditional master–apprentice model [2]. Simulators are used for training basic laparoscopic skills, as well as complex laparoscopic procedures [3,4,5]. Basic laparoscopic SBT typically involves the use of box-trainers and virtual reality (VR) simulators [6, 7]. To master laparoscopic techniques, trainees face a steep learning curve because of the intricate handling of stiff laparoscopic instruments, hand-eye coordination, bimanual efficiency, reduced sensation of touch, overcoming the Fulcrum effect (the tip of the surgical instrument moves in the opposite direction to the hand movement), and depth perception of three-dimensional (3D) surgical scene on two-dimensional (2D) images [8, 9]. With such demands on the learner’s psychomotor abilities, training in laparoscopic skills using simulators can induce both physiological and psychological stress responses [10,11,12].
Within the Lazarus and Folkman theoretical concept, the stress response is interpreted as a result of the person–environment interaction and arises when the demands of the person are not in balance with their perceived resources [13]. These demands can be of physical, cognitive, and social characteristics, and are often referred to as stressors [14,15,16]. How a person experiences and responds to stressors is dependent on their resources such as coping strategies, prior experience, personality traits, and their appraisal of socio-evaluative threats [17,18,19,20]. Therefore, they might differ from another person’s experience and response, even if the stressors or the situational settings are similar. Previous studies have shown that stress influences the acquisition of surgical skills, because excessive amount of stress can impair such performance, whereas low and moderate levels of stress might facilitate surgical performance [10,11,12, 21]. Despite substantial research on physiological stress responses related to laparoscopic skill acquisition in laboratory studies and the operating room [11, 22, 23], few studies have focused on trainees’ subjective experiences of stress during laparoscopic SBT courses. Studies using an interview-based approach, questionnaires, and self-reporting of stress have given some insights into the subjective stress experiences in simulation-based laboratory and interventional studies [12, 24, 25]. However, much remains unclear about which factors of laparoscopic SBT the trainees experience as stressful, in particular when performing simulation tasks in SBT course-based settings. An exploration into trainees’ subjective experiences would increase the understanding of how stress can influence simulation training and performance. Therefore, the aim of this study was to explore surgical trainees’ stress experiences associated with SBT of laparoscopic skills and performance.
Our research question was: “What subjective stress experiences do surgical trainees have related to simulation-based laparoscopic skills training and performance in an SBT course setting?”
Methods
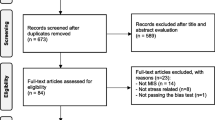
A qualitative research approach was employed to explore surgical trainees’ subjective experiences of stress during laparoscopic SBT courses [26]. This method allowed us to explore trainees’ perspectives and thought processes, as well as nuances and variables underlying their stress experience when training on three different laparoscopy simulators. We used an interview-based method and conducted semistructured individual interviews with surgical trainees attending SBT courses [27, 28]. The study design and timeline are illustrated in Fig. 1. The interview data were analyzed using inductive qualitative content analysis, an approach that allows for systematic and reliable analysis of codes, categories, and themes [27, 29]. The main themes presented are the authors’ subjective interpretation of the information yielded from the categorization and abstraction process of the interview data [30]. The study was approved by the Regional Committees for Medical and Health Research Ethics of Norway (Reference number: 2018/2414) and followed the Consolidated Criteria for Reporting Qualitative Research (COREQ) reporting guideline (Additional file 1).
The interview guide
The interview guide (Additional file 2) was developed based on the literature on the topic, and on information from former trainees and surgeon instructors. A pilot study with four trainees was carried out to test and revise the interview guide. We anticipated the trainees’ variations in the perception and interpretation of the term stress; however, to encourage trainees to talk without constraints about the topic, we decided not to present a specific concept of stress ahead of the interviews.
Sampling
Participants were included through purposive sampling. We recruited surgical trainees who were enrolled in courses at a national training center for advanced laparoscopic surgery. The trainees were in their first, second, or third year of their surgical specialization, and from different hospitals across Norway. The trainees were invited by e-mail to join the study and additional recruitments were made during the courses.
Demographics
Participants’ demographics were collected in the introduction part of the semistructured interviews. Information about gender, age, prior work experience, laparoscopic surgery experience, and simulation experience were collected.
Setting and context
The laparoscopic SBT was performed as part of a mandatory course on basic laparoscopic skills for surgical trainees in Norway. The course program consisted of several lectures followed by standardized laparoscopic SBT sessions (Fig. 1; Table 1). Each course lasted for three consecutive days and was rounded off with a written exam. These courses are normally taken early in the surgical specialist’s education (on average 5 years of education in Norway), and no previous formal laparoscopic training was required of the trainees. The trainees admitted to the courses had never taken them previously. The courses are mandatory once during the education.
Description of the laparoscopic SBT
Before the SBT sessions, the trainees were given orientation to each simulator, simulation tasks, and task requirements by instructors (detailed descriptions are provided in Table 1). Three different simulator modalities were used, two box-trainers (D-box, Covidien Surgical Box, Mansfield, MA, USA, and P.O.P-trainer, Optimist, Innsbruck, Austria) and one VR simulator (LapMentor™, 3D Systems, Littleton, CO, USA). The trainees trained for 1 h on each simulator before rotating to the next simulator, and the simulation sessions lasted for 3 h on the first day, 5 h on the second day, and 3 h on the last day. Trainees operated alone on one of the box-trainers and the VR simulator, while the trainees were paired on the other box-trainer. The instructors provided guidance and feedback on performance and technique throughout all training sessions.
Data collection
Data were collected from March 2019 to September 2021. The trainees were interviewed at the course facilities shortly after completion of the simulation training sessions. The primary author (MST) conducted all interviews. MST, an experienced interviewer, had training in conducting semistructured interviews with clinical personnel. MST was not involved as an instructor during the courses, and did not have any influence on trainees’ training or performances. The interviews lasted for 20–60 min. The interviews included follow-up questions to clarify statements and explorations into relatable themes. To ensure the validity of the data, each interview was summarized and validated orally by trainees regarding the content, accuracy, and meaning of statements. Interviews were consecutively transcribed and when preliminary analysis of the interviews showed that no new themes relating to the main topic were provided by new interviews, it was consensus that sufficient data had been obtained to answer the research question [32], and the data collection ended. All interviews were audio recorded using the dictation machine (Olympus WS-852) and transcribed verbatim by MST. Management and storing of audio recordings were in accordance with the regulations of the Regional Committees for Medical and Health Research Ethics of Norway.
Analysis
In the inductive, qualitative contents analysis process adapted from Graneheim and Lundman [27], all transcripts were reviewed, and the meaning units (all statements and sentences related to trainees’ stress experiences associated with training, performance, and course settings) were identified, condensed, and inductively coded by author MST in collaboration with author SOO. The coded interviews were read and discussed by the authors, and a consensus on codes was reached eventually. The codes were sorted into categories and further subjected to an abstraction process for the identification of main themes. In this study we identified main themes as the general stress experiences of the study group, leaving out the stress experiences only reported by one participant. The identification of main themes required an interpretation process of data involving repeated sessions of discussions involving reflection, comparison, and recategorization of themes. Table 2 lists the main themes, sub-categories, and meaning units (with example excerpts). The interpretation process yielded three main themes with associated sub-categories. Themes were validated by rechecking the transcripts to ensure they were derived from the original data. The method described by Ose [33] was employed to manage the data.
Results
Three main themes of stress experiences were identified through analysis. These related to (1) simulation task requirements such as task difficulty and time requirements, in addition, themes related to haptic feedback and realism of graphics; (2) psychomotor skill levels including inconsistent and poor technical performance; and (3) internal and self-imposed pressures, and socio-evaluative threats. These are listed in Table 2.
Participants
This study contained 20 surgical trainees. Their ages ranged from 28 to 42 years (median 34) and were of both genders with 55% identifying as female. The study participants were heterogeneous regarding prior laparoscopic experience as surgical trainees and in terms of simulation training experience as shown in Table 3. Two trainees had prior experience with the VR simulator, another two had substantial experience with the box-trainer (D-box); otherwise, the trainees had little experience with the simulators.
Stress experiences related to the complexity of simulation tasks
Trainees reported feeling stressed by the time requirements set by the box-trainers because they felt these were too rigid, and the fear of not meeting these requirements triggered stress and caused impaired performances in the early stages of training. In particular, trainees with less laparoscopic experience and those using unfamiliar laparoscopic equipment reported that the time requirements added an extra layer of stress to the simulation training, which led to poor performances. Conversely, some trainees reported that the stress triggered by the time requirements motivated them to intensify their training during the course and helped them to achieve better performance results. On the other hand, trainees with previous experience with box-trainers reported experiencing minimal stress related to training on these simulators, which was reflected in the faster accomplishment of task requirements and higher procedural efficiency. Overall, trainees reported that the stress they experienced early in the simulation course heavily affected their motivation and performance results during the course. However, all study participants passed the task requirements eventually, regardless of their initial stress levels. In contrast to the simulation training on the box-trainers, trainees reported experiencing minimal stress when training on the VR simulator. Trainees explained that they did not perceive the VR simulation tasks as “real enough” to make them feel stressed. Trainees repeatedly stated that they found the haptic feedback of the VR simulator to be too unrealistic and left them unable to differentiate between the different tissues represented in the VR operating scene, which was claimed as a major source of their demotivation toward further practice with this modality. Illustrative excerpts are listed in Table 2.
Stress experiences related to motor skills level
Trainees reported experiencing stress from their perception of poor technical performance. They expressed stress and frustration at not performing to the technical level that was required, describing stress levels as especially high when not being able to perform consistently or at technically high levels on every session on the simulators. The trainees with little previous experience with laparoscopic simulators or techniques expressed how this was reflected in their performance. The combination of handling unfamiliar laparoscopic instruments and performing demanding simulation tasks was described to have had a negative additive effect on performance and increased trainees’ stress experiences. Illustrative excerpts are listed in Table 2.
Stress experiences related to internal pressures
Trainees described how they felt stressed by the internal pressures of performing well on the simulators. On reflection, the trainees admitted that these internal pressures were their own self-imposed need to perform at high levels. This manifested as the constant need to improve upon their performance results, even if they already had accomplished the task requirements. The pressure was described as most prominent when training on the box-trainers, in particular the D-box. Several trainees reported experiencing stress when they found themselves comparing their results with those of other course participants. For other trainees, the comparison was seen as beneficial for their motivation toward performance objectives because it prompted them to engage in more intensive training, and ultimately resulting in improved performance. Illustrative excerpts are listed in Table 2.
Discussion
Our aim was to explore surgical trainees’ stress experiences during laparoscopic SBT courses to obtain a broader understanding of which factors of the SBT the trainees perceived as eliciting stress. The trainees experienced a variety of stressors, including some that are directly related to simulation training, such as the simulation task requirements and trainees’ psychomotor skills, alongside those of a psychological nature, such as internal pressures. The specific themes identified included task difficulty, time requirements, unrealistic haptic feedback and realism of graphics, inconsistent and low technical performance, self-imposed pressures, and socio-evaluative threats. The study also revealed that trainees have minimal stress experiences related to training on VR simulation tasks.
Threats, challenges, and previous experience
The trainees viewed the time pressure of the simulation tasks as a major stressor, eliciting stress experiences that they reported as leading to an impaired or poor technical performance in the early stages of the simulation training. In surgical training, it is crucial for trainees to acquire high degrees of technical as well as procedural efficiency [8]. The simulation task requirements of the SBT course were designed to measure both technical performance and procedural efficiency, where efficiency was measured through time requirements (time to complete a given task). The findings suggest that with the pressure of specific time requirements, the technical performance suffered. Research has shown that novice surgeons, when faced with competing cognitively demanding tasks, may attend to one of the tasks at the expense of others [34]. Moorthy et al. showed an adverse effect of multiple stressors, including time pressure, on the performance of a simple laparoscopic transfer task. In particular, skill-based errors appear to increase under the effect of the stressors [35]. When not being able to complete the simulation tasks as required, the trainees expressed how they perceived the simulation tasks as threats. When an individual is faced with a task that is cognitively appraised as a threat, and the demands of the threat outweigh the individual’s perceived available resources to meet the situation, the result is distress, which can impair technical performance [13, 36, 37]. Our findings are consistent with the literature, where task difficulty and time pressure are described as major stress factors impacting the technical performance of trainees in the laboratory and in clinical settings [10, 38, 39]. Likewise, in other medical simulation fields, similar findings have been reported of the impact of stress on simulation training performances [21]. In a study by LeBlanc et al. using patient simulators, impairments in technical skill performance were observed in participants following stressful simulated scenarios [40]. However, for some of the trainees, the same simulation task stressors helped to improve their performance results by prompting them to intensify their training during the course. When an individual appraises a task as a challenge, as opposed to a threat, and the demand of the task is perceived to be within their capability of handling, the stress experience can induce motivation and focus their attention on improved performance [36, 37]. Previous studies have demonstrated that participants improved their technical performance when stressors were added to the simulation session [41]. In a study by Moawad et al., gynecology residents performed with higher efficiency when tested for laparoscopic skills under stressful conditions compared with the same conditions without stressors [42]. A couple of trainees in our study had substantial prior experience with box-trainers and reported experiencing minimal stress related to the task requirements. This suggests that previous experience with similar stressful situations might have modified their stress experience. This is supported by previous research finding that a person’s prior experience with similar stressful situations or stressors can modulate their stress response [19, 43]. In a study by Crewther et al., it was demonstrated that a 3-week simulation-based laparoscopic skills training program promoted stress adaptations, which supported the acquisition of performance skills in novice surgeons [44], suggesting that repeated exposure to stressors can even have beneficial effects on the acquisition of skills.
Haptic feedback, realism of graphics, and motivation
Unlike training on the box-trainers, the trainees reported experiencing minimal stress during training on VR simulation tasks. The participants found the haptic feedback and the VR simulated tissue to be too unrealistic to stimulate a stress response during the simulation training, and some trainees expressed their demotivation toward further training on the VR simulator because of these limitations. This suggests that with the unrealistic haptic feedback and lack of realism in the graphics, the challenge of the surgical task failed, and thus diminished trainees’ stress experience and learner engagement [45, 46]. The role of haptic feedback and tissue realism of VR simulators have been discussed previously, showing that these are important features of the total simulation experience [47, 48]. However, the impacts of haptic feedback and realism on training and performance outcomes are variable. When the level of realism in a simulation task does not match the training objectives, apprehensions about the simulation modality as a training tool can develop, leading to resistance to training on these models [49,50,51]. Our findings are in line with the review by Gostlow et al. about voluntary participation in SBT of laparoscopic skills. The review showed that realistic haptic feedback and realism were important motivators for trainees to engage in repeated training activities on VR simulators [52].
Inconsistent performance and low psychomotor skills
Here, the trainees emphasized how they felt stressed by not performing consistently at high technical levels on the simulators. As novice surgeons, the trainees might have been unaware of how technically complex and steep is the learning curve for mastering laparoscopic skills. To master these skills demands high psychomotor abilities that are improved by extended and repetitive training [8]. Fitts and Posner’s model of the acquisition of motor skills describes three successive phases (cognitive, associative, and autonomous) that learners need to go through when developing new motor skills [53]. To reach the autonomous phase—where skills become automatic—requires repetitive practice over a period [54]. Without the requisite extensive training to master this surgical technique, inexperienced trainees will not be able to perform at a high level or consistently on laparoscopy simulators [55]. Depending on the trainees’ previous laparoscopic training, the simulation task difficulty levels might not have been aligned with the level of their psychomotor skills, subsequently eliciting stress experiences in those trainees with lower psychomotor skill levels or little laparoscopic training, suggesting that the demands of the simulation tasks outweighed trainees’ resources in psychomotor skills [13]. In a simulation study by Wetzel et al., junior surgeons reported that technical challenges and the lack of competence acted as sources of stress during simulated surgical procedures. In the same study, it was demonstrated that experienced surgeons, despite having high stress levels during the simulated procedures, did not show deterioration in performance. Thus, experience and surgical competence can compensate for the undesirable effects of stress on technical performance [18].
Self-imposed pressures
Trainees emphasized how important it was to perform well on the box-trainers because it was seen as basic to the SBT, and the self-imposed pressure to master these simulation tasks caused them to experience stress. The tasks performed on these simulators were designed to train basic bimanual dexterity, hand-eye coordination, and depth interpretation of 2D images, three essential skills surgeons need to master when performing laparoscopic procedures [8, 56]. In a practical simulation course setting, demonstration of technical skills is needed, with the risk of revealing weaknesses and proficiency gaps to peers and instructors, and consequently eliciting stress in trainees. Our findings suggest that trainees were worried that their performance results on the box-trainers could have been viewed as an indication of their skills, which could then be further interpreted as a reflection of their limited surgical competence [57]. Previous studies have shown that, when acting as a surgical trainee, mastering, and demonstrating basic technical skills is an important part of the process of developing surgical competence [2, 57, 58]. Trainees’ worries about acquiring sufficient surgical competence appear to be a concern that starts early in their surgical training and persist through to graduation [57].
Socio-evaluative threats
Trainees described how they felt stressed when they compared themselves with other course participants during the training, prompting them to intensify their training to improve the results, even though they had already accomplished the requirements. Many of the trainees already had some experience in training on box-trainer simulators before the course. This created a large range in skills between those familiar or unfamiliar with the simulator before the course. Previous research has shown that variations in laparoscopic skills among trainees are dependent on their access to laparoscopic procedures, equipment, and practice time [59]. Our findings suggest that when the trainees performed in a course setting among peers and instructor observers, they might have perceived the social-evaluative threat of not performing on the same level as their peers to be high, causing them to experience stress [60]. However, in contrast to the time requirements and task difficulty, socio-evaluative threats provided positive motivation for training during the course, and subsequently an increase in performance. The findings suggest that the stress experience elicited by the social setting of the SBT courses may be beneficial to training and enhance trainees’ performance results. Our findings are in line with the study by LeBlanc et al. who showed that junior surgery residents—while experiencing moderate stress levels from the examination—improved their technical performance during simulation [61].
Implications and future work
For trainees, the awareness of their stress response and how it influences their training process and performance during laparoscopic SBT courses might give them an indication as to what they might find stressful when performing laparoscopic techniques in real-life settings. By recognizing their stress-related limitations, trainees could use this as a signpost to initiate conversations with instructors or mentors about recognizing and managing stress in surgical training. Educators could encourage trainees to seek stress management training proactively in addition to extended psychomotor skills training, and trainees could start developing the coping strategies required for their professional role as surgeons [25, 62]. A broader understanding of trainees’ subjective stress experiences can aid in the development of SBT courses aimed at the acquisition of surgical skills. Educators could attain a clearer understanding of what aspects of different simulation tasks and simulator modalities are perceived as stressful, and how this influences trainees’ training process, and use this insight to adapt the simulation training. Adaptations such as adjusting the level of task difficulty to the proficiency of the trainees by considering the trainees’ level of experience and psychomotor skill, and their ability to cope with the challenges of the simulation tasks. Furthermore, reducing the simulation task into manageable steps, such as allowing the trainees to practice until they feel comfortable with the tasks before introducing the added pressure of time and other technical requirements, could improve trainees’ training process. To reduce the psychological stress pressures, instructors could clarify the learning objectives of the SBT tasks, and addressing the role of instructors and other observers attending the courses, which will set a psychological safe space for trainees to train in [63]. The relationship between the level of realism (i.e., fidelity) of the simulators, stress response, and learning outcomes is unclear [64,65,66]. Our findings indicate that higher levels of both structural and functional fidelity in VR simulation tasks might be beneficial. In particular, realistic haptic feedback appears essential to elicit stress experiences and thereby increase learner engagement and motivation [49]. Innovations within VR technology (i.e., immersive VR and augmented reality), might provide an optimal level of realism conducive to eliciting stress and facilitating the SBT experience [67]. Future studies exploring these themes would be useful for the development of VR simulation as a laparoscopic training tool.
Limitations
This study had several limitations. Major parts of this study was conducted during the global COVID-19 pandemic which involved several challenges. The pandemic involved increased clinical demands in hospital units across the country, multiple quarantines, travel ban for clinicians and therefore cancellation of planned SBT courses, and comprehensive COVID-testing pre-course admission. However, several aspects of the SBT remained as before: The SBT course settings, the learning objectives, the instructors and procedures. This preserved the integrity of the SBT course. For the study, it involved an extended time period for data collection; however, we do not consider that the extended time span had impact on the study findings. COVID-related adjustments during the data collection included the requirement to keep distance (1.5–2 m) and the need to wear facemasks during the interviews. This made it more challenging for the interviewer to identify non-verbal facial expressions, which may give cues for the interviewer in understanding if and when it is appropriate to go forward with more probing question. Considering the semi-structured form of the interviews, we do not think that this influenced the topics discussed and the findings as thus. At the risk of being interpreted as weak, or vulnerable to stress, trainees might have been guarded in their answers regarding stress-related themes. We ensured anonymity (de-identified audio recordings of interviews and transcripts) and chose to conduct one-on-one interviews as opposed to group interviews, but we do not know whether the trainees felt safe enough to disclose all their stress experiences to us. Therefore, more time to establish adequate levels of trust would be required for trainees to feel safe enough to be able to speak freely [28]. Trainees’ individual laparoscopic experience before the SBT course might have influenced their decision to join the study, with the risk of self-selecting bias. However, we sought a broad understanding of how stress is experienced by trainees during the SBT courses, which also included trainees with extensive prior laparoscopic experience. Despite the risk of self-selecting bias, the trainees represented a realistic sample. In this article, we did not include instructor’s perspectives on how stressful experiences might impact simulation training because we consider it to be outside the overall aims. However, the instructor’s role in a simulation training setting might have an impact on participants’ performance, so further research should elaborate on this topic [22, 68]. The generalizability of findings in qualitative studies is limited because of the nature of the findings being the subjective experience of the trainees; however, we believe our findings provide valuable insights into plausible perceptions and reactions from trainees attending laparoscopic SBT courses.
Conclusion
Insights into trainees’ stress experiences during laparoscopic SBT courses revealed how stress can both enhance and diminish performance, and influence trainees’ motivation for training during the course. This illustrates the powerful impact of stress experiences on the acquisition of surgical skills. In this study, the difficulty of simulation tasks, psychomotor skill levels, and trainees’ self-imposed pressures were identified as key factors in their subjective stress experiences. Overall, trainees had varied stress experiences depending on the perceived difficulty level and the realism of the simulation task, with previous simulator experiences modifying the stress experience. Efficiency requirements and technical difficulties of the simulation tasks elicited stress experiences among trainees with less laparoscopic experience and lower psychomotor skill levels. Self-imposed pressures and socio-evaluative threats appear to have an integral part in how trainees mobilized and performed during the courses, with levels of stress enhancing their performance. For course facilitators aiming at optimizing future laparoscopic SBT courses, attending to the realism of the simulation tasks, providing clarity about learning objectives of the simulation tasks, and having awareness of individual differences among trainees’ technical level when designing the simulation tasks, would be beneficial for the training process. Equally important to laparoscopic SBT is to create a psychological safe learning space for trainees in order to reduce their internal pressures.
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request. The data set is in Norwegian.
Abbreviations
- COREQ:
-
Consolidated Criteria for Reporting Qualitative Research
- P.O.P-trainer:
-
Pulsatile organ perfusion trainer
- SBT:
-
Simulation-based training
- VR:
-
Virtual reality
References
Aggarwal R, Mytton OT, Derbrew M, Hananel D, Heydenburg M, Issenberg B, et al. Training and simulation for patient safety. Qual Saf Health Care. 2010;19(Suppl 2):i34–43.
Prentice R. Bodies in formation. Durham and London: Duke University Press; 2012.
Childs BS, Manganiello MD, Korets R. Novel education and simulation tools in urologic training. Curr Urol Rep. 2019;20(12):81.
McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003-2009. Med Educ. 2010;44(1):50–63.
Beyer-Berjot L, Aggarwal R. Toward technology-supported surgical training: the potential of virtual simulators in laparoscopic surgery. Scand J Surg. 2013;102(4):221–6.
Aggarwal R, Grantcharov TP, Eriksen JR, Blirup D, Kristiansen VB, Funch-Jensen P, et al. An evidence-based virtual reality training program for novice laparoscopic surgeons. Ann Surg. 2006;244(2):310–4.
Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, et al. Proving the value of simulation in laparoscopic surgery. Ann Surg. 2004;240(3):518.
Gallagher AG, O’Sullivan GC. Fundamentals of surgical simulation: principles and practice. London: Springer-Verlag; 2011.
Crothers IR, Gallagher AG, McClure N, James DT, McGuigan J. Experienced laparoscopic surgeons are automated to the “fulcrum effect”: an ergonomic demonstration. Endoscopy. 1999;31(5):365–9.
Arora S, Sevdalis N, Aggarwal R, Sirimanna P, Darzi A, Kneebone R. Stress impairs psychomotor performance in novice laparoscopic surgeons. Surg Endosc. 2010;24(10):2588–93.
Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R. The impact of stress on surgical performance: A systematic review of the literature. Surgery. 2010;147(3):318–30.
Wetzel CM, Kneebone RL, Woloshynowych M, Nestel D, Moorthy K, Kidd J, et al. The effects of stress on surgical performance. Am J Surg. 2006;191(1):5–10.
Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer publishing company; 1984.
Selye H. The stress of life. New York: McGraw-Hill; 1956.
Monroe SM, Slavich GM. Chapter 13 - Psychological Stressors: Overview. In: Fink G, editor. Stress: Concepts, Cognition, Emotion, and Behavior. San Diego: Academic Press; 2016. p. 109–15.
Godoy LD, Rossignoli MT, Delfino-Pereira P, Garcia-Cairasco N, de Lima Umeoka EH. A Comprehensive Overview on Stress Neurobiology: Basic concepts and clinical implications. Front Behav Neurosci. 2018;12:127.
Childs E, White TL, de Wit H. Personality traits modulate emotional and physiological responses to stress. Behav Pharmacol. 2014;25(5 and 6):493–502.
Wetzel CM, Black SA, Hanna GB, Athanasiou T, Kneebone RL, Nestel D, et al. The effects of stress and coping on surgical performance during simulations. Ann Surg. 2010;251(1):171–6.
Clemente-Suárez VJ, Robles-Pérez JJ, Herrera-Mendoza K, Herrera-Tapias B, Fernández-Lucas J. Psychophysiological response and fine motor skills in high-altitude parachute jumps. High Alt Med Biol. 2017;18(4):392–9.
Smith TW, Jordan KD. Interpersonal motives and social-evaluative threat: Effects of acceptance and status stressors on cardiovascular reactivity and salivary cortisol response. Psychophysiology. 2015;52(2):269–76.
LeBlanc VR. The effects of acute stress on performance: implications for health professions education. Acad Med. 2009;84(10 Suppl):S25–33.
Andreatta PB, Hillard M, Krain LP. The impact of stress factors in simulation-based laparoscopic training. Surgery. 2010;147(5):631–9.
Flinn JT, Miller A, Pyatka N, Brewer J, Schneider T, Cao CG. The effect of stress on learning in surgical skill acquisition. Med Teach. 2016;38(9):897–903.
Arora S, Tierney T, Sevdalis N, Aggarwal R, Nestel D, Woloshynowych M, et al. The Imperial Stress Assessment Tool (ISAT): a feasible, reliable, and valid approach to measuring stress in the operating room. World J Surg. 2010;34(8):1756–63.
Stefanidis D, Anton NE, Howley LD, Bean E, Yurco A, Pimentel ME, et al. Effectiveness of a comprehensive mental skills curriculum in enhancing surgical performance: Results of a randomized controlled trial. Am J Med. 2017;213(2):318–24.
Meena JK, Jakhetiya A, Pandey A. Qualitative research in surgical disciplines: Need and scope. Indian J Surg. 2021;83(1):3–8.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
DiCicco-Bloom B, Crabtree BF. The qualitative research interviews. Med Educ. 2006;40(4):314–21.
Haggarty L. What is content analysis? Med Teach. 1996;18(2):99–101.
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Cheng A, Kessler D, Mackinnon R, Chang TP, Nadkarni VM, Hunt EA, et al. Reporting guidelines for health care simulation research: extensions to the CONSORT and STROBE statements. Adv Simul. 2016;1(1):25.
Varpio L, Ajjawi R, Monrouxe LV, O’Brien BC, Rees CE. Shedding the cobra effect: problematising thematic emergence, triangulation, saturation and member checking. Med Educ. 2017;51(1):40–50.
Ose SO. Using Excel and Word to structure qualitative data. J Appl Soc Sci. 2016;10(2):147–62.
Hsu KE, Man FY, Gizicki RA, Feldman LS, Fried GM. Experienced surgeons can do more than one thing at a time: effect of distraction on performance of a simple laparoscopic and cognitive task by experienced and novice surgeons. Surg Endosc. 2008;22(1):196–201.
Moorthy K, Munz Y, Dosis A, Bann S, Darzi A. The effect of stress-inducing conditions on the performance of a laparoscopic task. Surg Endosc. 2003;17(9):1481–4.
Harvey A, Nathens AB, Bandiera G, LeBlanc VR. Threat and challenge: cognitive appraisal and stress responses in simulated trauma resuscitations. Med Educ. 2010;44(6):587–94.
Tomaka J, Blascovich J, Kelsey RM, Leitten CL. Subjective, physiological, and behavioral effects of threat and challenge appraisal. J Pers Soc Psychol. 1993;65(2):248–60.
Modi HN, Singh H, Darzi A, Leff DR. Multitasking and time pressure in the operating room: Impact on surgeons’ brain function. Ann Surg. 2020;272(4):648–57.
Poolton JM, Wilson MR, Malhotra N, Ngo K, Masters RSW. A comparison of evaluation, time pressure, and multitasking as stressors of psychomotor operative performance. Surgery. 2011;149(6):776–82.
LeBlanc VR, MacDonald RD, McArthur B, King K, Lepine T. Paramedic performance in calculating drug dosages following stressful scenarios in a human patient simulator. Prehosp Emerg Care. 2005;9(4):439–44.
DeMaria S Jr, Bryson EO, Mooney TJ, Silverstein JH, Reich DL, Bodian C, et al. Adding emotional stressors to training in simulated cardiopulmonary arrest enhances participant performance. Med Educ. 2010;44(10):1006–15.
Moawad GN, Tyan P, Kumar D, Krapf J, Marfori C, Abi Khalil ED, et al. Determining the effect of external stressors on laparoscopic skills and performance between obstetrics and gynecology residents. J Surg Educ. 2017;74(5):862–6.
Ng R, Chahine S, Lanting B, Howard J. Unpacking the literature on stress and resiliency: A Narrative review focused on learners in the operating room. J Surg Educ. 2019;76(2):343–53.
Crewther BT, Shetty K, Jarchi D, Selvadurai S, Cook CJ, Leff DR, et al. Skill acquisition and stress adaptations following laparoscopic surgery training and detraining in novice surgeons. Surg Endosc. 2016;30(7):2961–8.
Singapogu R, Burg T, Burg KJ, Smith DE, Eckenrode AH. A perspective on the role and utility of haptic feedback in laparoscopic skills training. Crit Rev Biomed Eng. 2014;42(3–4):293–318. https://doi.org/10.1615/critrevbiomedeng.2014011701.
Oussi N, Enochsson L, Henningsohn L, Castegren M, Georgiou E, Kjellin A. Trainee performance after laparoscopic simulator training using a blackbox versus LapMentor. J Surg Res. 2020;250:1–11.
Rangarajan K, Davis H, Pucher PH. Systematic review of virtual haptics in surgical simulation: A valid educational tool? J Surg Educ. 2020;77(2):337–47.
Lamata P, Gómez EJ, Sánchez-Margallo FM, Lamata F, del Pozo F, Usón J. Tissue consistency perception in laparoscopy to define the level of fidelity in virtual reality simulation. Surg Endosc. 2006;20(9):1368–75.
Hamstra SJ, Brydges R, Hatala R, Zendejas B, Cook DA. Reconsidering fidelity in simulation-based training. Acad Med. 2014;89(3):387–92.
Zendejas B, Brydges R, Hamstra SJ, Cook DA. State of the evidence on simulation-based training for laparoscopic surgery: a systematic review. Ann Surg. 2013;257(4):586–93. https://doi.org/10.1097/SLA.0b013e318288c40b.
Shetty S, Zevin B, Grantcharov TP, Roberts KE, Duffy AJ. Perceptions, training experiences, and preferences of surgical residents toward laparoscopic simulation training: a resident survey. J Surg Educ. 2014;71(5):727–33.
Gostlow H, Marlow N, Babidge W, Maddern G. Systematic review of voluntary participation in simulation-based laparoscopic skills training: motivators and barriers for surgical trainee attendance. J Surg Educ. 2017;74(2):306–18.
Fitts PM, Posner MI. Human performance. Belmont: Brooks/Cole Publishing Company; 1967.
Cook DA, Brydges R, Zendejas B, Hamstra SJ, Hatala R. Mastery learning for health professionals using technology-enhanced simulation: a systematic review and meta-analysis. Acad Med. 2013;88(8):1178–86.
Stefanidis D, Korndorffer JR Jr, Markley S, Sierra R, Heniford BT, Scott DJ. Closing the gap in operative performance between novices and experts: does harder mean better for laparoscopic simulator training? J Am Coll Surg. 2007;205(2):307–13.
Stefanidis D, Korndorffer JR Jr, Sweet R. Comprehensive healthcare simulation: surgery and surgical subspecialties. Cham: Springer; 2019.
Gardner AK, Willis RE, Dunkin BJ, Van Sickle KR, Brown KM, Truitt MS, et al. What do residents need to be competent laparoscopic and endoscopic surgeons? Surg Endosc. 2016;30(7):3050–9.
Faurie C, Khadra M. Technical competence in surgeons. ANZ J Surg. 2012;82(10):682–90.
Kroeze SGC, Mayer EK, Chopra S, Aggarwal R, Darzi A, Patel A. Assessment of laparoscopic suturing skills of urology residents: A pan-european study. Eur Urol. 2009;56(5):865–73.
Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychol Bull. 2004;130(3):355–91.
LeBlanc V, Woodrow SI, Sidhu R, Dubrowski A. Examination stress leads to improvements on fundamental technical skills for surgery. Am J Surg. 2008;196(1):114–9.
Anton NE, Mulji N, Howley LD, Yurco AM, Tobben D, Bean E, et al. Effects of a novel mental skills curriculum on surgical novices’ attention. J Surg Res. 2017;219:86–91.
Bong C, Fraser K, Oriot D. Cognitive Load and Stress in Simulation. In: Grant V, Cheng A, editors. Comprehensive healthcare simulation: pediatrics. Comprehensive Healthcare Simulation: Springer; 2016. p. 3–17.
Weiß S, Klassen N, Heuten W. Effects of image realism on the stress Response in virtual reality. proceedings of the 27th ACM Symposium on virtual reality software and technology; Osaka, Japan: Association for Computing Machinery; 2021;10:1–10. https://doi.org/10.1145/3489849.3489885.
Beaubien JM, Baker DP. The use of simulation for training teamwork skills in health care: how low can you go? Qual Saf Health Care. 2004;13(Suppl 1):51–6.
Miotto HC, Couto BRGM, Goulart EMA, Amaral CFS, Moreira MCV. Advanced cardiac life support courses: live actors do not improve training results compared with conventional manikins. Resuscitation. 2008;76(2):244–8.
Lungu AJ, Swinkels W, Claesen L, Tu P, Egger J, Chen X. A review on the applications of virtual reality, augmented reality and mixed reality in surgical simulation: an extension to different kinds of surgery. Expert Rev Med Devices. 2021;18(1):47–62.
Strandbygaard J, Bjerrum F, Maagaard M, Winkel P, Larsen CR, Ringsted C, et al. Instructor feedback versus no instructor feedback on performance in a laparoscopic virtual reality simulator: a randomized trial. Ann Surg. 2013;257(5):839–44. https://doi.org/10.1097/SLA.0b013e31827eee6e.
Acknowledgements
We would like to acknowledge the surgical trainees who participated in the study, the staff and surgeon instructors at the simulation training facility. Special thanks to former chief surgeon and director of the National Research Center for Minimally invasive and image-guided Diagnostics and Therapy (MiDT), St. Olavs Hospital, Trondheim, Norway, Dr. Ronald Mårvik.
Funding
Open access funding provided by Norwegian University of Science and Technology. This study was supported by a grant funded by the Research Council of Norway (grant number: 272402).
Author information
Authors and Affiliations
Contributions
MST, AD, and SOO designed the project. MST performed the interviews and transcribed these verbatim. MST and SOO analyzed the data. MST drafted the manuscript. SOO, AD, and CV revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for this study was obtained through the Regional Committees for Medical and Health Research Ethics of Norway (REK) reference number (2018/2414), which is in accordance with the Declaration of Helsinki. The participants were given oral and written information concerning the purpose of the study, its confidentiality, and the rights to withdraw their consent at any time.
Consent for publication
Written, informed consent was obtained from all study participants.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Report in accordance with the COREQ guidelines-checklist for reporting qualitative research. Description of data: Completed checklist in accordance with the COREQ guidelines.
Additional file 2.
Interview guide. Description of data: Topical questions used in the interviews for data collection.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tjønnås, M.S., Das, A., Våpenstad, C. et al. Simulation-based skills training: a qualitative interview study exploring surgical trainees’ experience of stress. Adv Simul 7, 33 (2022). https://doi.org/10.1186/s41077-022-00231-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41077-022-00231-2