Abstract
Background
Food frequency questionnaires (FFQ) are a useful dietary assessment tool to determine relationships between diet and non-communicable diseases (NCDs). Our purpose was to validate a semiquantitative FFQ (semi-FFQ) for Thais at risk of metabolic syndrome (MS).
Methods
The researchers identified 345 men and women aged 30–65 years who were eligible for the study. Ninety-four participants were finally enrolled (54 in a “urine-collection not-required” group and 40 in a “urine collection” group). They were asked to maintain a 4-day food record for 4 weeks and partook in a semi-FFQ interview during week 4. Urine samples and biochemical results related to MS were collected. Validation results were associated with three primary nutrients for MS (sugar, fat, and sodium) and biochemical results (blood glucose, lipid profiles, blood pressure, and 24-h urine sodium).
Results
The biomarker level of each key MS nutrient significantly increased commensurate with rises in semi-FFQ estimated intakes. Correlation coefficients (r) were as follows: fasting blood glucose, r = 0.221 (fruits) and r = 0.229 (desserts); triglycerides, r = 0.112 (a la carte-dishes); low-density lipoprotein cholesterol, r = 0.205 (rice-with-topping dishes); systolic blood pressure, r = 0.272 (snacks) and r = 0.190 (a la carte dishes). Fasting blood glucose was a significant biomarker associated with the development of metabolic syndrome (OR 1.42, 95% CI 1.12–1.81). We also found that fat (OR 1.28, 95% CI 1.09–1.89), sodium (OR 1.98, 95% CI 1.05–1.95) and energy (OR 1.09, 95% CI 1.01–1.17) from an a la carte meal were significantly associated with the development of metabolic syndrome.
Conclusions
Thai food has a unique characteristic since it often pairs various ingredients and seasoning in one menu. This semi-FFQ is a tool that offers relatively valid ranking for intake of energy, nutrients, single foods, and mixed dishes based on Thai menus associated with a risk for developing metabolic syndrome and NCDs. Using this tool could help identify unhealthy dietary patterns and help develop recommendations for people at risk with the goal of preventing NCDs.
Similar content being viewed by others
Background
Metabolic syndrome is associated with an increased risk in the development of non-communicable diseases such as diabetes mellitus, hypertension, cancer, and cardiovascular diseases [1,2,3]. In Thailand, non-communicable diseases account for an estimated 74% of deaths [4]. Diet is a main lifestyle-related risk factor of these metabolic diseases. Nevertheless, metabolic syndrome can be prevented by changing eating behavior and lifestyle habits. And dietary assessment has been useful in NCD risk prediction while consuming a healthy nutrient-dense was correlated with a lower risk of death [5]. Due to the uniqueness of Thai food, it is challenging to estimate the usual intake of a single food type or the ingredients of mixed dishes. The amount and the types of food and ingredients consumed is also various among subjects [6]. To improve our understanding of the eating behavior of Thais, we previously developed a 91-item Thai semiquantitative food frequency questionnaire (semi-FFQ) that encompassed single food items and mixed dishes [7]. However, inaccurate dietary assessment may be a serious barrier of understanding the impact of dietary factors on NCDs. Therefore, the validity of the questionnaire needed to be established.
Epidemiological studies have used various reference methods to validate semi-FFQs, such as dietary records or 24-h recall. For example, Kobayashi et al. developed a semi-FFQ for Japanese children in 2011. Four weighted dietary records were conducted once a week, and the research focused on the correlation between the records and the semi-FFQ [8]. Another cohort study carried out in 2009 validated a semi-FFQ using 24-h dietary recalls. The investigators found correlation coefficients between 2 of 3 sets of 24-h dietary recalls and a 204-item semi-FFQ [9]. Rachmah et al. developed a semi-FFQ for sugar intake for Indonesian children. They used food records for six nonconsecutive days as their intake references [10]. In 2020, Mumu et al. in Bangladesh validated a semi-FFQ using a 24-h dietary recall method and the corresponding biological nutritional markers. Their study was the first to validate a semi-FFQ in Bangladesh using multiple measures, and there was acceptable agreement on ranking the dietary intake of the semi-FFQ with some biomarkers [11].
Nevertheless, each of the above methods has limitations. Dietary records and 24-h recall face the problems of respondent burden, self-report bias, and incorrect recall of information from memory [12, 13]. On the other hand, investigators using biomarkers as an alternative need to be aware of the problems presented by improper collection, transportation methods, and confounders [14]. Therefore, researchers should consider the limitations of each method before deciding on one for their studies. The present investigation aimed to validate the semi-FFQ that had been previously developed for Thais at risk of metabolic syndrome by analyzing the relationship between nutrients-derived from the semi-FFQ and biochemical markers.
Methods
Study setting and sample selection
The validation study was conducted at the Faculty of Medicine Siriraj Hospital, Bangkok, Thailand. The sample population was Siriraj personnel aged 30–65 years who were at risk of metabolic syndrome and had participated in the SIRIRAJ-Health (SI-Health) study. The SI-Health study is a prospective cohort study on non-communicable diseases that began in mid-2017. As of February 2019, its cohort had 4496 Siriraj staff members. The sample selection drew upon data previously obtained for SI-Health. Participants were divided into two main groups according to urine collection requirements: “urine-collection not-required” (a sugar and fat study group) and “urine collection” (a sodium study group). They were then divided into seven minor groups according to the most recent metabolic syndrome criteria of the International Diabetes Federation [3]. They were as follows: (1) dyslipidemia group qualified (DLP); (2) diabetes mellitus group qualified (DM); (3) hypertension group qualified (HT); (4) dyslipidemia and diabetes mellitus group qualified (DM-DLP); (5) hypertension and diabetes mellitus group qualified (HT-DLP); (6) hypertension and diabetes mellitus group qualified (HT-DM); and (7) hypertension, diabetes mellitus, dyslipidemia group qualified (HT-DM-DLP). Figure 1 illustrates the categorization of the subjects.
Study design and data collection
The validity of the Thai semi-FFQ was assessed by analyzing the relationship between the nutrients derived from the Thai semi-FFQ and the biochemical results. The biochemical results of each participant were sourced from SI-Health, which records data on annual health checks.
The duration of data collection was 4 weeks. Participants were required to attend two interviews conducted in weeks 1 and 4 at Siriraj Medical Research Center, Siriraj Hospital, Thailand. Between these interview sessions, participants could use the social networking application LINE (Line Corporation, Tokyo, Japan) to ask for more information or make an appointment for a face-to-face consultation.
In the first interview session, prospective subjects were provided with documents that described the objectives and procedures of the study. The subjects were asked to sign a consent form if they agreed to participate, and they were informed that they could withdraw at any time during the study. The investigator then explained the data collection process. Subjects in the HT, HT-DLP, HT-DM, and HT-DM-DLP subgroups were asked to undergo a 24-h urine collection. In the second interview session, the participants partook in the Thai semi-FFQ interview carried out by a dietitian.
24-h urine collection
Participants in the urine collection group were asked to record the date and time of their first urination in the morning but were instructed not to collect a sample. However, during the following 24 h, all urine was collected. To this end, an investigator provided participants with a plastic jug and a 5-L container, each using 10 g of boric acid as a preservative. The sodium in the urine was later analyzed using an indirect ion-selective electrode (Fig. 2).
Thai semi-FFQ
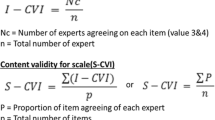
A semi-FFQ was administered in week 4. The Thai semi-FFQ was initially designed for use in the SI-Health study to obtain data on the frequency of food consumption and the amount consumed in 1 month. Methods for development of semi-FFQ were previously described [7]. Briefly, food types and amounts consumed from dietary recall and our observation in a pilot study was ranked by registered nutritionists in gram/unit intake. For food groups, itemized single foods, mixed dishes, sweets, and desserts were classified. We focused on a la carte, noodles, or rice with topping-dish. Each menu was three randomly selected sampling to measure each ingredient. The major ingredients of rice or noodle dishes, as well as meat and vegetable groups of each Thai mixed dish were separated and weighted by a digital kitchen scale (TANITA digital kitchen scale; KD-192, Japan). Nutritive values of all the foods along with their condiments were calculated by Thai food composition software (INMUCAL-v3.2) of the Institute of Nutrition, Mahidol University, Thailand. The nutritive values of food items consisted of energy, total fat, protein, sodium, sugar, dietary fiber, cholesterol, and saturated fat. Nutrient profiling (NP) was used to classify foods and snacks based on their nutritional composition. There were three levels of grading: ‘grade A’ (a suitable nutrient profile with no or low risk for NCDs), ‘grade B’ (unsuitable nutrient profile with medium risk for NCDs), and ‘grade C’ (unsuitable nutrient profile with high risk for NCDs). Mean values of each nutrient in every food items were calculated before using the NP criteria. The eating behavior questionnaires were also included for supporting dietary patterns. Finally, three patterns of FFQ that emphasized on the amounts of sugar, sodium and fat was identified since these nutrients were strongly related to MS. The food menus and serving sizes were added in the FFQ. The content validity index (CVI) was evaluated by qualified experts and nutritionists. The CVI consists of a 4-point rating scale (1 = not relevant, 4 = very relevant). An acceptable level of content validity should be greater than 0.8. After the FFQ development, three experts from Institute of Nutrition, Mahidol University, were asked for reviewing the FFQ. The Thai semi-FFQ has 97 food items: 18 tropical fruits, ten beverages, 29 snacks and desserts, 23 mixed dishes (a la carte and noodles), and 17 rice-with-topping dishes. A 5-level scale is used for serving size; the serving size unit is the “household unit” of the Thai food-based dietary guideline [15]. The frequency response options are open-ended, and the choices are “never,” “x times per month,” “x times per week,” and “x times per day” (Fig. 3). The questionnaire was completed during the interview conducted by a dietitian.
Data preparation
The Thai food composition software INMUCAL-Nutrients V.4.0, Database NB.4 (Institute of Nutrition, Mahidol University, Nakhon Pathom, Thailand), was used to calculate the nutrient intake from the Thai semi-FFQ. Nine nutrients were analyzed: energy (kcal), carbohydrate (g), total fat (g), protein (g), sodium (mg), sugar (g), dietary fiber (g), cholesterol (mg), and saturated fat (g).
Biochemical results related to metabolic syndrome criteria were obtained from the SI-Health cohort study. They were fasting blood glucose (FBG), glycated hemoglobin (HbA1c), cholesterol level, triglyceride level (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), systolic blood pressure (SBP), and diastolic blood pressure (DBP). These results were collected and analyzed in the same day as the subjects participated in annual health checkup between 2019 and 2020, which was the same time as we conducted the semi-FFQ.
To overcome the limitation of correlation analysis, reducing the variation between data points was considered. Consequently, “popular foods” were selected from the items in the Thai semi-FFQ; the resulting list consisted of foods consumed by at least one-third of the participants.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics for Windows, version 22.0 (IBM Corp., Armonk, NY, USA). General data and health information are presented as mean, median, standard deviation, frequency, and percentage. The correlations between the focus nutrients of the Thai semi-FFQ and biochemical results (both blood and urine) were measured using Spearman’s rank correlation or Pearson’s correlation for the normally distributed data (Table 1). Two-tailed statistical analyses were conducted at a probability (P) value of 0.05 to determine statistical significance. To decrease the variations between data, bootstrap resampling was used. Risk factors for the development of metabolic syndrome were analyzed using a multivariable logistic regression.
Results
Participants in this study
Of the 4496 people in the SI-Health study cohort, 345 were eligible for enrollment in the current investigation. The eligible participants were divided into two main groups based on their SI-Health results: a sugar and fat study group (the urine-collection not-required group) and a sodium study group (the urine collection group). Phone recruitment was conducted; 117 people declined to participate, and 133 could not be contacted. Eventually, 95 participants were enrolled. During the study, one person in the DLP group was lost to follow-up. Therefore, the number of participants analyzed in this study was 94 (Fig. 4). Ninety-four participants were classified into seven subgroups: DLP (n = 27), DM (n = 14), HT (n = 10), DM-DLP (n = 13), HT-DLP (n = 16), HT-DM (n = 5), and HT-DM-DLP (n = 9). The mean age of the validity study participants was 40.13 ± 7.13 years. Women predominated in all subgroups except the HT-DM-DLP group, which had an equal number of men and women. Almost 80% of the participants had a BMI greater than 25 kg/m2 (Table 2).
Data preparation
Before analysis, we reviewed the data to establish the best validation model that would provide appropriate correlation coefficient values between food items and reference indicators. We focused on the frequency of consumption of each food item and determined its popularity by multiplying that frequency by the portion size. We set distinct levels of popularity, signified by 30%, 33%, 35%, 40%, 45%, and 50% of participants consuming a food item. For example, 57% of DM subjects consumed pasteurized milk, which meant that pasteurized milk was selected for the 50% popularity level but not the 45% popularity level (Fig. 5). After performing statistical analyses, the value of 33% gave the highest number of “popular” food items compared with other procedures. Consequently, we used the 33% cutoff for popularity to analyze the correlation coefficient values.
Statistical analysis
The bootstrap method was conducted to find a correlation between crucial nutrients for metabolic syndrome (sugar, fat, and sodium) of each food group and biochemical results (FBG, HbA1c, TG, cholesterol, HDL-C, LDL-C, SBP, DBP, and urine sodium). Spearman’s correlation was selected. The popular food items of each food group were calculated by frequency multiplied by portion size. The popular items in each food group are listed in Table 3.
The validity results for sugar, fat, and sodium among the food groups and the biochemical results are presented in Table 4. Spearman’s rank correlation coefficient found the following ranges: sugar, 0.04 to 0.265; fat, 0.03 to 0.260; and sodium, 0.01 to 0.272. The correlation coefficient with/without bootstrap resampling was not different. The highest correlations were obtained for the sugars in tropical fruits and FBG, with 0.265. The lowest correlations were found for the sodium in the dessert and DBP, with a value of 0.01.
Spearman’s correlation coefficient produced significant values for the sugars in tropical fruits, sugar in desserts, FBG, and HbA1c. The sugars in tropical fruits and desserts compared with FBG ranged from 0.235 to 0.265; when compared with HbA1c, they ranged from 0.180 to 0.223. The bootstrapping correlation coefficient values for resampling the data were 0.221 for the sugars in tropical fruits (FBG), 0.229 for sugar in desserts (FBG), 0.180 for the sugars in tropical fruits (HbA1c), and 0.223 for sugar in desserts (HbA1c). There were no significant correlations between the sugar content of beverages or snacks and FBG and HbA1c.
Spearman’s correlation coefficient produced significant values for fat in a la carte dishes, fat in rice-with-topping dishes and TG, cholesterol, HDL-C, and LDL-C. The fat in a la carte dishes and rice-with-topping dishes compared with TG ranged from 0.060 to 0.214; compared with LDL-C, they ranged from 0.030 to 0.260. The bootstrapping correlation coefficient values for resampling the data were 0.112 (TG and fat in a la carte dishes), 0.242 (TG and fat in rice-with-topping dishes), 0.020 (LDL-C and fat in a la carte dishes), and 0.205 (LDL-C and fat in rice-with-topping dishes). There were no significant correlations between the fat content of snacks, desserts, and noodles and TG, cholesterol, HDL-C, or LDL-C.
Spearman’s correlation coefficient produced statistically significant values for the sodium in snacks and a la carte dishes and SBP. The sodium in snacks and a la carte dishes compared with SBP ranged from 0.206 to 0.272. The bootstrapping correlation coefficient values for resampling the data were 0.190 for sodium in snacks (LDL-C) and 0.272 for sodium in a la carte dishes (LDL-C). There were no significant correlations between the sodium content of snacks or a la carte dishes and DBP and urinary sodium. Table 5 shows the correlation between the energy intake (kcal) from semi-FFQ and the biochemical results. The correlation coefficients of energy intake from desserts, TG, and cholesterol were significantly correlated. The bootstrapping correlation values were − 0.239 (desserts and TG) and 0.235 (desserts and cholesterol). The Thai semi-FFQ consists of 54 items with significant biochemical results, as summarized in Table 5.
Risk factors for the development of metabolic syndrome were analyzed using a multivariable logistic regression (Table 6). Fasting blood glucose was the significant biomarker associated with the development of metabolic syndrome (OR 1.42, 95% CI 1.12–1.81). We also found that fat (OR 1.28, 95% CI 1.09–1.89), sodium (OR 1.98, 95% CI 1.05–1.95) and energy (OR 1.09, 95% CI 1.01–1.17) from a la carte meal were significantly associated with the development of metabolic syndrome.
Discussion
In this study, the correlations between three critical nutrients for metabolic syndrome, sugar, fat, sodium, and biochemical results were crucial for Thai semi-FFQ validation. We found that some biochemical results increased significantly with an increase in the major nutrients estimated by our semi-FFQ.
Based on the semi-FFQ estimate of sugar intake, most fruits and desserts were significantly correlated with FBG and HbA1c. In 2005, the ATTICA study in Greece set out to find the relationship between diet consumption and blood glucose among people without cardiovascular disease and diabetes. Unfortunately, Panagiotakos et al. did not find a significant association between fruit consumption and FBG, and the correlation coefficient was 0.01 [16]. The correlation coefficient of the ATTICA study was lower than that of our study, which may be due to self-administration. In addition, the nutrient composition of fruit in Greece is different from that of Southeast Asia and Thailand due to climatic and geographical differences.
Another cross-sectional study conducted in East England in 2018 examined the association between dietary sugar from different sources and metabolic markers. The researchers used a semi-FFQ for dietary assessment. They found that sugar from liquids (r = 0.16) and free sugar (r = 0.07) correlated with plasma glucose [17]. In 2019, the Japan Public Health Center-Based Prospective Study (JPHC) compared two standard methods for validating sugar intake from semi-FFQs: urinary sugar and food records. The study found that sugar intake from a semi-FFQ was positively correlated with dietary records (r = 0.34) and urinary sugar concentration (r = 0.40). Moreover, the researchers suggested that multiple measurements of urinary sugars lead to a high correlation and are more valuable than single or double measurements [18].
The natural sugars in fruits increase blood glucose nearly as much as sucrose [19]. Tropical fruits, which contain high levels of natural sugar, are widely consumed by Thais because of their digestive assistance and intestinal cleansing properties. It is common practice for Thais to finish their meals with fruits [20]. Moreover, processed foods, snacks, and desserts frequently use high-fructose corn syrup as a sweetener. This processed sugar helps improve the texture of desserts. Some studies did not find a significant difference between the effects of high-fructose corn syrup and sucrose on blood glucose [21, 22]. Other research found that consuming fructose with glucose from starch worsened insulin resistance [23].
As for the relationship between the source of fat intake and biochemical lipid profiles, 8 of the 11 a la carte dishes were correlated with an increase in triglyceride levels and a decrease in HDL-C levels. These a la carte dishes generally contained high amounts of saturated fats, tropical oils and carbohydrates (> 60% of total energy intake). Excessive consumption of both fats and carbohydrates in the Thai a la carte dishes can therefore negative affect triglycerides and HDL cholesterol [24, 25]. According to two previous studies’ findings on the nutritive values and nutrient profiles of mixed dishes [7, 26], the nutrient profiling score for fat in the a la carte group was low. Moreover, almost 50% of the rice-with-topping dishes were related to increased levels of cholesterol and LDL-C.
In 1993, a study in the Netherlands compared three methods: semi-FFQ, diet history, and biomarkers of fat intake. The investigators reported some statistically significant correlation coefficients between fatty acids in erythrocyte membranes and fatty acids from diet. The range of correlation coefficients was 0.15–0.27, which is close to our results. Another study by the ALSPAC (Avon Longitudinal Study of Parents and Children) team in 2001 reported an association between blood lipid levels and dietary intake. Correlation levels ranged between 0.178 and 0.209. The ALSPAC team also reported a correlation between total cholesterol and total fat intake (r = 0.209) [27].
Avoiding excess fat became essential for people with MS, particularly, in fat contained in fried dishes in the a la carte and rice-with-topping groups. Typical examples were rice with stir-fried crispy pork and kale, rice with stir-fried pork and hot basil, spicy shrimp paste fried rice, stir-fried crispy catfish with chili paste, stir-fried mixed vegetables with oyster sauce, and stir-fried pumpkin with eggs.
Regarding the correlation between sodium intake and biological results, we found that snacks and dishes from the a la carte group were correlated with blood pressure but not sodium in urine. Some studies found that the correlation between semi-FFQ and 24-h urine sodium was low. Day et al. [28] reported a correlation between semi-FFQ and 24-h urine sodium (r = 0.13). This value was similar to those of our study, which found correlations between semi-FFQ and 24-h urine sodium of r = 0.12 for snacks, r = 0.11 for a la carte dishes, and r = 0.08 for noodles. However, research in Brazil reported no correlation between urinary sodium excretion and its semi-FFQ (r = 0.18) [29]. Although urinary sodium collection is one of the gold-standard methods to measure the sensitivity of salt intake, a high instability of urinary sodium has been demonstrated [30, 31]. Several factors affect urinary sodium excretion. They include sodium transport mechanisms, sodium absorption, salt sensitivity, micronutrient interactions, and hormones (such as aldosterone and vasopressin) [32]. As for energy intake and biological results, we did not find significant correlations except for desserts with TG (r = − 0.262) and cholesterol (r = 0.288). The correlation between energy intake and lipid profiles should be positive due to fat consumption. However, supporting data were unavailable.
There were some limitations in our study that affect our results. First, the study did not account for any variations in individual body metabolism and physical activity levels that might have occurred during that period. Second, our study did not find any correlation between the 24-h urine sodium and sodium intake levels, despite this being the gold standard. A review article suggested that at least two to seven 24-h urine collections be performed to increase accuracy [33]. However, because our subjects were medical personnel with typically unpredictable lifestyles, 24-h urine collection tended to be challenging to execute. Third, the investigators realized during their participant interviews that the semi-FFQ was missing some food items that might be important to biochemical results (e.g., alcoholic beverages). Fourth, seasonal fruits and food festivals (such as vegetarian festivals for Thai-Chinese) can affect food availability and hence Thais’ eating behaviors. Therefore, some tropical fruits eliminated from the draft semi-FFQ might have later been available during the investigator interviews with the study participants.
On the other hand, there are some strengths of our study. First, the Thai semi-FFQ used five portion sizes that were based on the standard portion size: − 25%, − 50%, 100%, + 150%, and + 200%. Using several portion sizes helped decrease the effects of variations introduced by individuals’ different portion sizes. Second, food photography clearly illustrated the different serving sizes of mixed dishes, which facilitated the conduct of interviews in the data collection phase in week 4. Third, the inclusion of mixed-dish food items (namely, the rice-with-topping dishes) boosted the effectiveness of our questionnaire and facilitated respondents’ understanding of the food item choices.
Conclusions
Thai food has a unique characteristic since it often pairs various ingredients and seasoning in one menu. This semi-FFQ is a tool that offers relatively valid ranking for intake of energy, nutrients, single foods, and mixed dishes based on Thai menus associated with a risk for developing metabolic syndrome and NCDs. The validated Thai semi-FFQ could be a reasonable dietary assessment tool for future epidemiological studies in the country.
Availability of data and materials
Not applicable.
Abbreviations
- DBP:
-
Diastolic blood pressure
- DLP:
-
Dyslipidemia
- DM:
-
Diabetes mellitus
- FBG:
-
Fasting blood glucose
- FFQ:
-
Food frequency questionnaires
- HbA1c:
-
Glycated hemoglobin
- HDL-C:
-
High-density lipoprotein cholesterol
- HT:
-
Hypertension
- LDL-C:
-
Low-density lipoprotein cholesterol
- MS:
-
Metabolic syndrome
- NCDs:
-
Non-communicable diseases
- SBP:
-
Systolic blood pressure
- semi-FFQ:
-
Semiquantitative food frequency questionnaire
- TG:
-
Triglyceride
References
World Health Organization. Regional Office for South-East Asia. WHO country cooperation strategy, Thailand: 2017–2021. In: Regional Office for South-East Asia. New Delhi: World Health Organization; 2017. pp. 5–6.
Baxter AJ, Coyne T, McClintock C. Dietary patterns and metabolic syndrome—a review of epidemiologic evidence. Asia Pac J Clin Nutr. 2006;15(2):134–42.
Alberti KG, Zimmet P, Shaw J. Metabolic syndrome—a new world-wide definition: a consensus statement from the International Diabetes Federation. Diabetic Med. 2006;23(5):469–80.
World Health Organization. Noncommunicable diseases country profiles 2018. Geneva: World Health Organization; 2018.
Baik I, Cho NH, Kim SH, Shin C. Dietary information improves cardiovascular disease risk prediction models. Eur J Clin Nutr. 2013;67(1):25–30.
Shim JS, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health. 2014;36:e2014009.
Nirdnoy N, Sranacharoenpong K, Mayurasakorn K, Surawit A, Pinsawas B, Mongkolsucharitkul P, Pongkunakorn T, Suta S. Development of the Thai semiquantitative food frequency questionnaire (semi-FFQ) for people at risk for metabolic syndrome. J Public Health (Berl). 2021;31:1–8.
Kobayashi T, Kamimura M, Imai S, Toji C, Okamoto N, Fukui M, Date C. Reproducibility and validity of the food frequency questionnaire for estimating habitual dietary intake in children and adolescents. Nutr J. 2011;10(1):27.
Jaceldo-Siegl K, Knutsen SF, Sabaté J, Beeson WL, Chan J, Herring RP, Butler TL, Haddad E, Bennett H, Montgomery S, et al. Validation of nutrient intake using an FFQ and repeated 24 h recalls in black and white subjects of the Adventist Health Study-2 (AHS-2). Public Health Nutr. 2010;13(6):812–9.
Rachmah Q, Kriengsinyos W, Rojroongwasinkul N, Pongcharoen T. Development and validity of semi-quantitative food frequency questionnaire as a new research tool for sugar intake assessment among Indonesian adolescents. Heliyon. 2021;7(6):e07288.
Mumu SJ, Merom D, Ali L, Fahey PP, Hossain I, Rahman AKMF, Allman-Farinelli M. Validation of a food frequency questionnaire as a tool for assessing dietary intake in cardiovascular disease research and surveillance in Bangladesh. Nutr J. 2020;19(1):42.
Hebert JR, Ebbeling CB, Matthews CE, Hurley TG, Ma Y, Druker S, Clemow L. Systematic errors in middle-aged women’s estimates of energy intake: comparing three self-report measures to total energy expenditure from doubly labeled water. Ann Epidemiol. 2002;12(8):577–86.
Fries E, Green P, Bowen DJ. What did I eat yesterday? Determinants of accuracy in 24-hour food memories. Appl Cogn Psychol. 1995;9(2):143–55.
Freedman LS, Schatzkin A, Midthune D, Kipnis V. Dealing with dietary measurement error in nutritional cohort studies. J Natl Cancer Inst. 2011;103(14):1086–92.
Sirichakwal PP, Sranacharoenpong K. Practical experience in development and promotion of food-based dietary guidelines in Thailand. Asia Pac J Clin Nutr. 2008;17(S1):63–5.
Panagiotakos DB, Tzima N, Pitsavos C, Chrysohoou C, Papakonstantinou E, Zampelas A, Stefanadis C. The relationship between dietary habits, blood glucose and insulin levels among people without cardiovascular disease and type 2 diabetes; the ATTICA study. Rev Diabet Stud. 2005;2(4):208–15.
O’Connor L, Imamura F, Brage S, Griffin SJ, Wareham NJ, Forouhi NG. Intakes and sources of dietary sugars and their association with metabolic and inflammatory markers. Clin Nutr. 2018;37(4):1313–22.
Kanehara R, Goto A, Kotemori A, Mori N, Nakamura A, Sawada N, Ishihara J, Takachi R, Kawano Y, Iwasaki M, et al. Validity and reproducibility of a self-administered food frequency questionnaire for the assessment of sugar intake in middle-aged Japanese adults. Nutrients. 2019;11(3):554.
Wolever TM, Miller JB. Sugars and blood glucose control. Am J Clin Nutr. 1995;62(S1):212S-S227.
Sowattanangoon N, Kotchabhakdi N, Petrie KJ. The influence of Thai culture on diabetes perceptions and management. Diabetes Res Clin Pract. 2009;84(3):245–51.
Melanson KJ, Zukley L, Lowndes J, Nguyen V, Angelopoulos TJ, Rippe JM. Effects of high-fructose corn syrup and sucrose consumption on circulating glucose, insulin, leptin, and ghrelin and on appetite in normal-weight women. Nutrition. 2007;23(2):103–12.
Melanson KJ, Angelopoulos TJ, Nguyen V, Zukley L, Lowndes J, Rippe JM. High-fructose corn syrup, energy intake, and appetite regulation. Am J Clin Nutr. 2008;88(6):1738s-s1744.
Kolderup A, Svihus B. Fructose metabolism and relation to atherosclerosis, type 2 diabetes, and obesity. J Nutr Metab. 2015;2015:1–12.
Aekplakorn W, Satheannoppakao W, Putwatana P, Taneepanichskul S, Kessomboon P, Chongsuvivatwong V, Chariyalertsak S. Dietary pattern and metabolic syndrome in Thai adults. J Nutr Metab. 2015;2015:468759.
Shin W-K, Shin S, Lee J, Kang D, Lee JE. Carbohydrate intake and hyperlipidemia among population with high-carbohydrate diets: the Health Examinees Gem Study. Mol Nutr Food Res. 2021;65(3):2000379.
Pongutta S, Sirichakwal P, Chittchang U, Puwastien P, Rojroongwasinkul N, Sranacharoenpong K, Inthararak P, Chongviriyaphan N, Saleephan S, Moh-Suwan L, et al. Nutrient profiling: a tool to strengthen nutrition intervention in Thailand. J Health Sci. 2017;24(6):1030–40.
Cowin IS, Emmett PM. Associations between dietary intakes and blood cholesterol concentrations at 31 months. Eur J Clin Nutr. 2001;55(1):39–49.
Day N, McKeown N, Wong M, Welch A, Bingham S. Epidemiological assessment of diet: a comparison of a 7-day diary with a food frequency questionnaire using urinary markers of nitrogen, potassium and sodium. Int J Epidemiol. 2001;30(2):309–17.
Ferreira-Sae MC, Gallani MC, Nadruz W, Rodrigues RC, Franchini KG, Cabral PC, Sales ML. Reliability and validity of a semi-quantitative FFQ for sodium intake in low-income and low-literacy Brazilian hypertensive subjects. Public Health Nutr. 2009;12(11):2168–73.
Bingham SA, Williams R, Cole TJ, Price CP, Cummings JH. Reference values for analytes of 24-h urine collections known to be complete. Ann Clin Biochem. 1988;25(Pt 6):610–9.
Liu K, Stamler J. Assessment of sodium intake in epidemiological studies on blood pressure. Ann Clin Res. 1984;16(S43):49–54.
Srikan P, Callen B, Phillips K, Tavakoli A, Brockett R, Hanucharurnkul S, Beebe L. Testing a model of sodium reduction in hypertensive older Thai adults. J Nutr Gerontol Geriatr. 2017;36(1):48–62.
McLean RM, Farmer VL, Nettleton A, Cameron CM, Cook NR, Campbell NRC. Assessment of dietary sodium intake using a food frequency questionnaire and 24-hour urinary sodium excretion: a systematic literature review. J Clin Hypertens (Greenwich). 2017;19(12):1214–30.
Acknowledgements
The authors thank the staff of the Population Health and Nutrition Research Group (SPHERE) and Siriraj Health Study Group, Faculty of Medicine Siriraj Hospital for their facilities and hospitality. The authors are also indebted to Mr David Park for the English-language editing of this paper.
Members of Siriraj Health Study Group: Winai Ratanasuwan4, Mayuree Homsanit4, Keerati Charoencholvanich5, Bhoom Suktitipat6, Chalermchai Mitrpant6, Manop Pithukpakorn7, Prapat Suriyaphol8, Rungroj Krittayaphong9, Prasert Auewarakul10, Boonrat Tassaneetritap11, Naravat Poungvarin12
4Department of Preventive and Social Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Wanglang Road, Siriraj, Bangkoknoi, Bangkok, 10700, Thailand; 5Department of Orthopedic Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Wanglang Road, Siriraj, Bangkoknoi, Bangkok, 10700, Thailand; 6Department of Biochemistry, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Wanglang Road, Siriraj, Bangkoknoi, Bangkok, 10700, Thailand; 7Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Wanglang Road, Siriraj, Bangkoknoi, Bangkok, 10700, Thailand; 8Division of Bioinformatics and Data Management for Research, Research Group and Research Network Division, Research Department, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Wanglang Road, Siriraj, Bangkoknoi, Bangkok, 10700, Thailand; 9Division of Cardiology, Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Wanglang Road, Siriraj, Bangkoknoi, Bangkok, 10700, Thailand; 10Department of Microbiology, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Wanglang Road, Siriraj, Bangkoknoi, Bangkok, 10700, Thailand; 11Center of Research Excellence in Immunoregulation, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Wanglang Road, Siriraj, Bangkoknoi, Bangkok, 10700, Thailand; 12Department of Clinical Pathology, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Wanglang Road, Siriraj, Bangkoknoi, Bangkok, 10700, Thailand.
Funding
This study was funded by a research grant from the Routine to Research Unit, Siriraj Hospital, Mahidol University, Thailand (R016135033).
Author information
Authors and Affiliations
Consortia
Contributions
Siriraj Health Study Group permitted using participant data. NN, BP, PM, TP, TM, SO, SP and SS were responsible for data collection. NN, KS, and AS analyzed the data. KS and KM conceptualized the research design and obtained project funding. NN and KM produced the first draft of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Before this research began, its protocol was approved by the Siriraj Institutional Review Board, Human Research Protection Unit, Faculty of Medicine Siriraj Hospital, Mahidol University, Thailand (IRB COA. No. Si 279/2018). All the respondents signed an informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nirdnoy, N., Sranacharoenpong, K., Surawit, A. et al. Validation of a Thai semiquantitative food frequency questionnaire (semi-FFQ) for people at risk of metabolic syndrome. J Health Popul Nutr 42, 13 (2023). https://doi.org/10.1186/s41043-023-00353-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-023-00353-x