Abstract
Objective
Due to an increase in aging worldwide, assessment of the nutritional status of older people becomes an important matter. Malnutrition in older people increases the risk of infections, disease period and hospitalization rates. This study aimed to compare the different anthropometric indices for detecting malnutrition among older people and comparing these indices among males and females to explain the possible differences.
Methods
In this cross-sectional study, 2721 aged 65 years and older in Turkey were enrolled. Anthropometric measurements weight, height, hip circumference (HC), and waist circumference (WC), abdominal circumference (AC), mid-upper arm circumference (MUAC), triceps skinfold thickness (TST), calf circumference (CC)) were measured. Body mass index (BMI), abdominal volume index (AVI), body roundness index (BRI) and body adiposity index (BAI), and waist-to-hip ratio (WHR) and waist-to-height ratio (WHtR) indices were calculated using standardized formulas. The receiver operator characteristic curves (ROCs) were conducted in detecting the best anthropometric parameters. Adjusted odds ratios (OR) (stratified by sex) calculated for each anthropometric index.
Results
Participants with both BMI < 18.5 (1.1%) and BMI > 25 (80%) defined as the malnourished group and BMI of 18.5–24.99 (18.9%) defined as the normal group. In both sexes, the area under the curve (AUC) was > 0.7 for all anthropometric indices except WHR in females (AUC 0.66). BRI, WHR, WHtR, and AVI indices strongly predict the risk of malnutrition among both sexes. In males, the ORs were for BRI (6.83, 95% CI 5.39–8.66), WHR (6.43, 95% CI 5.9–6.9), AVI (2.02, 95% CI 1.86–2.12). In females, the ORs were for BRI (3.72, 95% CI 3.09–4.48), WtHR (2.63, 95% CI 1.3–3.5), and WHR (2.45, 95% CI 1.9–3.06).
Discussion
The presence of a large AUC in almost all anthropometric indices suggests that they can be used to assess the risk of malnutrition among older persons in both sexes.
Similar content being viewed by others
Introduction
Aging is increasing worldwide. The number of people aged 65 or over is projected to grow from an estimated 524 million in 2010 to nearly 1.5 billion in 2050, with most of the increase in developing countries in recent years [1, 2]. Physiological changes such as a decreased sense of taste or smell, or both in older people can related with adversely nutritional status. Ageing may also be associated with profound psychosocial and environmental changes, such as isolation, loneliness, depression, and inadequate finances, which may also have significant impacts on diet [3].
Nutritional status of older people is an important factor and it related with quality of life among them [4]. Malnutrition is common condition in older persons and it affects almost 13–78% of the older population [5, 6]. Malnutrition is as an important factor for predicting morbidity and mortality among older persons [4]. Poor nutritional status in older people increases the risk of infections, disease period, poor wound healing, hospitalization rate, postoperative complications [7,8,9,10,11].
Nutritional status of the older people has been evaluated using various tools and methods in different studies [12,13,14,15,16,17,18,19,20,21]. An available screening and assessment methods for malnutrition is anthropometric measurements [22,23,24]. Common anthropometric indices of body composition such as body mass index (BMI), waist circumference (WC), waist-to-hip ratio (WHR), waist-to height ratio (WHtR), arm circumference (AC) and calf circumference (CC) have been widely used [5, 17, 25, 26]. The anthropometric indices are simple, easily obtainable, inexpensive, noninvasive measures of assessing and early detection of malnutrition in older people [22, 26]. Among them BMI is a valid and accepted anthropometric measure indicate underweight, overweight and obesity as all forms of malnutrition [23, 27]. For adults with 20 years of age and older, BMI categories ranges are underweight (BMI<18.5 kg/m2), normal weight (18.5 to <24 kg/m2), overweight (24 to < 28 kg/m2), and obesity (≥28 kg/m2) [28]. Recently, new anthropometric indices including body roundness index (BRI), body adiposity index (BAI), abdominal volume index (AVI), and body shape index (ABSI) have been considered as a predictor of health status [27, 29,30,31]. Association between these new indices and some diseases has been evaluated [32,33,34].
Anthropometric indices are affected by several factors including gender, environmental and socioeconomic status, genetic, race, and other factors [35, 36].
Malnutrition leads to poor outcomes and poor quality of life among older persons; therefore, early detection of malnutrition and subsequent nutritional intervention can significantly benefit vulnerable populations in addition to economic benefits such as reducing medical/healthcare costs. Current study assesses the different anthropometric indices for detecting malnutrition among older people and comparing these indices between males and females to explain the possible differences in a large population-based screening in Turkey.
Methods
Study population
In this large population-based cross-sectional study, the anthropometric indices were measured in 2721 persons aged over 65 years from both sexes. Cluster sampling method was conducted for the data collection. First, research population was divided into seven geographical/political region of Turkey including Central Anatolia, Aegean, Mediterranean, Black Sea, Marmara, East Anatolia, and Southeast Anatolia. In these 7 regions, 26 provinces were included in this study. Provinces with high older population size were selected according to the population database of Turkish Statistical Institute (TSI). The percentage of participants to represent each region was estimated from the total of older population of each region based on database of TSI. Finally, participants were included in both rural and urban regions applying simple random sampling. Sample size was determined according to α = 0.01, standard deviation (σ) = 15.17, d = 0.75 and number of older persons in the + 65 years (N = 3327593) using following formula:
The number of older individuals to be included for each region was calculated as 396, 473, 274, 319, 988, 148, and 134 in Central Anatolia, Aegean, Mediterranean, Black Sea, Marmara, East Anatolia, and Southeast Anatolia, respectively.
The study protocol was approved by the Ethics Committee of Cumhuriyet University, Turkey, with 2014-03/15 number.
Anthropometry assessments
The anthropometric indices were measured according to the techniques described by the Anthropometric Standardization Reference Manual (ASRM) and the International Biological Program (IBP) [37]. The anthropometric measurements were taken by two trained staffs in each participant. The field study was carried out between December 2016 and August 2017. The measurements were taken only once for the most participants. However, a pilot study was conducted to show the invariance of the variability criterion between individual measurements by measuring 35 older adults three times within a month in Sivas Province. The body weight was measured without shoes and minimum clothing to the nearest 0.01 kg using a digital scale (AR550 Sottile Digital Glass Scale, TR). Height was measured in the standing position without shoes using strip meter with accuracy of 0.1 cm (Harpenden Anthropometer, Holtain Ltd., UK). WC was measured using the tape measure in standing with feet shoulder width apart position in the area between the hip bone and under the navel. HC is measured at the widest part of the hips. The largest circumference between the waist and the knees was considered as HC. AC is measured at the midpoint of the line between the rib or costal margin and the iliac crest in the midaxillary line. Mid-upper arm circumference (MUAC) was taken with tape measure. The participant should stand upright, the arm should be freely hanging to the side, and the biceps should be measured without applying pressure to the circumference of the most bulging (middle of the forearm). CC was measured by wrapping the tape around the widest part of the calf in a sitting position. The participant sits at the table with his feet hanging freely. The person taking the measurement stands in front of the participant and measures the maximum circumference of the calf with a tape measure. For measuring of triceps skinfold thickness (TST), the participant should be freely hanging from side to side without stretching his/her arms and the person taking the measurement should be behind the participant. The measurement is taken over the triceps muscles on the back of the upper arm and in the middle of the upper arm (between the acromion and olecranon points) with the skinfold (Skinfold Caliper, Holtain Ltd., UK). Measurements were taken between these two points with tape measure. BMI, BRI, BAI, AVI, WHtR, and WHR indices were calculated using the following standardized formulas:
-
(1).
BMI = weight (kg)/height(m2) [38]
-
(2).
\( BRI=364.2-365.5\sqrt{1-\left\{\frac{{\left( WC\left[m\right]/2\pi \right)}^2}{0.5\kern0em height\;\left[m\right]\Big){}^2}\right\}} \) [39, 40]
- (3).
-
(4).
AVI = [2WC2(cm) + 0.7(WCC − HC)2(cm)]/1000 [42]
-
(5).
WHtR = WC(cm)/Height(cm) [43]
-
(6).
WHR : WC (cm)/HC(cm) [42]
Statistical analysis
Continuous variables were presented as means ± SD and categorical variables were expressed as number and percentage. Based on BMI as common and accepted measure for assessing malnutrition, participants characterized within two groups: participants with BMI < 18.5 (underweight) and BMI > 25 (overweight and obesity) as the malnourished group and participants with BMI of 18.5–24.99 as the normal group [38, 44]. The baseline characteristics were compared between normal and malnourished groups using the Pearson’s chi-square test for categorical variables. The mean of anthropometric variables was compared by independent t test between two groups stratified by sex. The area under the receiver operating characteristic curve (AUC) was used to assess the predictive ability of anthropometric measurements for the malnutrition (stratified by sex). The odds ratios (ORs) and their 95% CIs for the risk of malnutrition for each anthropometric index were calculated by logistic regression. Logistic regression model was adjusted for age groups (65–74, 75–84, and > 85 years), marital status (single, married, and widow), and job (employer, worker, self-employment, pensionary, un-employment, and housekeeper) as categorical variables.
Results
In this cross-sectional study, 2721 aged 65 years and older in Turkey were enrolled. Of 2721 subjects, 513 (18.9%) participant had normal status and 2208 (81.1%) were malnourished. The percent of participants with BMI < 18.5, 18.5–24.99, 25–29.99, and > 30 was 29 (1.1%), 513 (18.9%), 880 (32.3%), and 299 (47.7%), respectively.
The main baseline characteristics of participants were presented in the Table 1. The sex, age groups, and marital status had statistically significant difference between normal and malnourished groups. One thousand five hundred thirty (56.23%) were females and 1193 (43.77%) were males. In the malnutrition group, 60.7% of subjects were females while 39.3% of whom were males. The prevalence of malnutrition was 62%, 31.8%, and 6.2% among 65–74, 75–84, and > 85 years, respectively. In the normal group, the frequency of single, married, and widow participants was 17.7%, 25.5%, and 56.7%, respectively, while these frequencies were 10.4%, 35.4.5%, and 54.2%, respectively, in the malnutrition group. 46.4% of malnourished participants were housekeepers while in the normal group the subjects with pensionary job status (36.3%) had the highest frequency (p < 0.05).
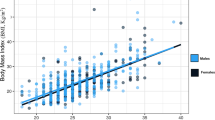
The mean of anthropometric indices was compared between normal and malnourished older persons (Table 2). All of anthropometric indices were significantly higher in malnourished group than normal group in total participants, men and women. However, most of these indices were higher in women than in men.
The area under the curve (AUC) and cut off points of anthropometric indices were presented in Table 3. In general, the most significant AUCs were > 0.8 in both males and females for all anthropometric indices except WHR and TSC in males (AUC 0.78) and WHR in females (AUC 0.66). In males, both of WC and AVI had the same largest AUC (0.94, 95% CI = 0.93–0.95), while both of WHR and TSC had the same smallest AUC (0.78, 95% CI = 0.76–0.81). In descending order, AUC was for both WHtR and BRI (0.93, 95% CI = 0.91–0.94), AC (0.92, 95% CI = 0.91–0.93), UAC (0.89, 95% CI = 0.87–0.91), HC (0.86, 95% CI = 0.0.85–0.9), both of BAI and CC (0.82, 95% CI = 0.8–0.85), and both of WHR and TST (0.78, 95% CI = 0.76–0.81), respectively.
In females, AC, WC, AVI, and MUAC had the largest AUC (AC 0.92, 95% CI = 0.9–0.93, both of WC and AVI 0.91, 95% CI = 0.9–0.93 and UAC 0.9, 95% CI = 0.088–0.93). WHR had the smallest AUC (0.66, 95% CI = 0.62–0.7). AUC was similar for HC, WHtR, and BRI (0.88, 95% CI = 0.85–0.91). AUC was for BAI (0.84, 95% CI = 0.82-0.87), for CC (0.82, 95% CI = 0.79–0.86), and TST (0.79, 95% CI = 0.76–0.83) in descending order.
Generally, there were gender differences in the cutoff point of all the anthropometric indices with approximately similar in sensitivity and specificity except for HC, WHtR, MUAC, and BRI. The cutoff point for WC was 89.95 cm and 83.75 cm in males and females, respectively. The cutoff points were for WHR, AC, TST, CC, AVI, and BAI 0.94, 95.95, 5.45, 30.75, 15.45, and 26.36 in males, respectively. While the cutoff points of these indices were in females 0.87, 97.95, 10.45, 29.45, 13.18, and 32.63, respectively.
Adjusted ORs of malnutrition risk for each anthropometric index were shown in Table 4. In both sexes, the significant OR of BRI and WHR were greater than other anthropometric indices. As the OR of BRI was OR 6.83, 95% CI 5.39–8.66 for males and OR 3.72, 95% CI 3.09–4.48 for females. For WHtR the OR was OR 6.43, 95% CI 5.9–6.9 in males and OR 2.45, 95% CI 1.9–3.06, p < 0.001 in females. In both sexes, the OR was highest following the two above indices for AVI and MUAC (OR “AVI”: 2.02 and 2.01 in males and females, respectively, and OR “MUAC”: 1.96 and 1.81 in males and females, respectively). Other anthropometric indices were positively associated with malnutrition in both sexes.
Discussion
The anthropometric indices are closely related to the nutritional status. The anthropometric assessment in older people is inexpensive, non-invasive and it can reflect the nutritional status of a population [25]. Among the anthropometric indexes, BMI was used commonly for evaluating of malnutrition [23, 27].
In current study participants were categorized into two groups: BMI < 18.5 (underweight) and BMI > 25 (overweight and obesity) as the malnourished group and participants with BMI of 18.5–24.9 as the normal group. The results showed that only 18.9% of participants had the normal status while 81.1% of them were malnourished. Sanchez-Garcia et al. showed 62.3% of Mexican older persons (> 60 years old) had BMI > 25 and 1.4% had BMI < 18.5 [25]. Setiati et al. reported that 45.01% of older people had normal nutritional status based on BMI and 54.99% of them were malnourished in Indonesia [45]. In India, Kalaiselv et al. showed that 37.6 of older adults had normal BMI (BMI 18.5–23 kg/m2) [46]. Despite the differences in eating habits around the world, the prevalence of malnutrition in the older population appears to be high in different regions of the world. Therefore, aging and the factors that lead to an increase in malnutrition in the older population should be taken in consideration.
Current study showed that the AUC of all anthropometric indices in detecting malnutrition was greater than 0.7 in both sexes except WHR in females (AUC 0.66). In both sexes, WC and AVI had the largest AUC (> 0.9). Correa et al. showed that the AUC for waist-to-height ratio (WHtR) as an anthropometric indicator of overweight according to the body mass index (BMI) classification was greater than 0.8 [26]. Consistent with our findings in a study by Jamir et al., the AUC for mid-upper-arm circumference (MUAC), triceps skinfold thickness (TST), and calf circumference (CC) was 0.93, 0.88, and 0.86 in men and 0.95, 0.9, and 0.91 in women, respectively [2].
Findings of this study revealed that there are gender differences in the cutoff points of all the anthropometric indices as nearly similar in sensitivity and specificity. The cutoff point of WC (value 93.15), WHR (value 0.94), CC (value 30.75), and AVI (value 15.45) in males was higher than females (WC value 83.75, WHR value 0.87, CC value 10.45, and AVI value 13.8). However, the cutoff point for AC (value 97.95), TST (value 10.45), and BAI (value 32.63) indices in females was higher than males (value 95.95, 5.45, 26.3 for AC, TST, and BAI, respectively). The cutoff point of HC, WHtR, MUAC, and BRI was nearly similar in both sexes. Consistent with current study, the cutoff point values reported 26.6, 7.9, and 30.7 for MUAC, TST, and CC in males and 25.9, 12, and 28.1 in females, respectively [2]. In a study, the cutoff point of WHtR and BRI was similar in both sexes (0.51 for WHtR in both sex, BRI 3.58 in males and 3.62 in females) [47]. In another study, the cut-off points of the WC, WHtR, and BRI indices for predicting metabolic syndrome (MetS) were reported 87.25, 0.51, and 3.55 in males and 77.25, 0.49, and 3.18 in females, respectively [23].
The ability of AVI, BRI, and BAI was assessed as a predictor factor of metabolic syndrome and cardiovascular diseases in several studies [48, 49]. Current study showed the BRI, WHR, WHtR, and AVI indices strongly predict the risk of malnutrition among both sexes. The odds ratio (OR) was closely for other anthropometric indices. Yang et al. showed that the OR of prediction of diabetes among older persons for BRI was greater than other anthropometric indices in both sexes [47]. Hu et al. showed that BMI, WC, and WHtR were independently associated with all-cause mortality among older persons [28]. The high prevalence of malnutrition among older persons in Turkey [19] necessitates anthropometric assessment of the older persons and this relatively can prevent and reduce the dangers of malnutrition.
In summary, although measuring BMI as common index for assessing malnutrition, the other anthropometric indices should be considered. In other words, BMI in combination with other anthropometric indices can better reflect health status.
The main strength of this study is the large sample size, and the population screening for the assessment of malnutrition status of older people. To increase accuracy, the anthropometric measurements were taken from each participants by two staffs. The limitation of this study is that the health status and illnesses among subjects were not studied.
Conclusion
Current study showed that there were differences among males and females in the cutoffs of HC, WC, WHR, WHtR, AC, MUAC, TST, CC, AVI, BRI, and BAI. Because the AUC was > 0.7 in all anthropometric measurements then these indices could be utilized to assess risk of malnutrition among older people in both sexes.
Availability of data and materials
The datasets that support the findings of this study are available on request from the first author [Özgün Başıbüyük, G.]. (As the row data are still under process of evaluation, analysis, and further publication the data are not publicly available).
Abbreviations
- HC:
-
Hip circumference
- WC:
-
Waist circumference
- AC:
-
Abdominal circumference
- MUAC:
-
Mid-upper arm circumference
- TST:
-
Triceps skinfold thickness
- CC:
-
Calf circumference
- BMI:
-
Body mass index
- AVI:
-
Abdominal volume index
- BRI:
-
Body roundness index
- BAI:
-
Body adiposity index
- WHR:
-
Waist-to-hip ratio
- WHtR:
-
Waist-to-height ratio
- ROCs:
-
Receiver operator characteristic curves
- OR:
-
Odds ratios
- AUC:
-
Area under the curve
References
Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, et al. COVID-19 in Wuhan: Immediate Psychological Impact on 5062 Health Workers. medRxiv. 2020;24:100443.
Jamir L, Kalaivani M, Nongkynrih B, Misra P, Gupta SK. Anthropometric characteristics and undernutrition among older persons in a rural area of northern India. Asia Pac J Public Health. 2015;27(2):2246–58.
Montazeri A, Harirchi AM, Shariati M, Garmaroudi G, Ebadi M, Fateh A. The 12-item General Health Questionnaire (GHQ-12): translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1(1):66–70.
Malek Mahdavi A, Mahdavi R, Lotfipour M, Asghari Jafarabadi M, Faramarzi E. Evaluation of the Iranian Mini Nutritional Assessment Short-Form in Community-dwelling Elderly. Health Promot Perspect. 2015;5(2):98–103.
Miao JP, Quan XQ, Zhang CT, Zhu H, Ye M, Shen LY, et al. Comparison of two malnutrition risk screening tools with nutritional biochemical parameters, BMI and length of stay in Chinese geriatric inpatients: a multicenter, cross-sectional study. BMJ Open. 2019;9(2):e022993.
Htun N, Ishikawa-Takata K, Kuroda A, Tanaka T, Kikutani T, Obuchi S, et al. Screening for malnutrition in community dwelling older Japanese: Preliminary development and evaluation of the Japanese Nutritional Risk Screening Tool (NRST). J Nutr Health Aging. 2016;20(2):114–20.
Yaxley A, Crotty M, Miller M. Identifying Malnutrition in an Elderly Ambulatory Rehabilitation Population: Agreement between Mini Nutritional Assessment and Validated Screening Tools. Healthcare (Basel). 2015;3(3):822–9.
Harris D, Davies C, Ward H, Haboubi N. An observational study of screening for malnutrition in elderly people living in sheltered accommodation. J Hum Nutr Diet. 2008;21(1):3–9.
Poulia KA, Klek S, Doundoulakis I, Bouras E, Karayiannis D, Baschali A, et al. The two most popular malnutrition screening tools in the light of the new ESPEN consensus definition of the diagnostic criteria for malnutrition. Clin Nutr. 2017;36(4):1130–5.
Robb L, Walsh CM, Nel M, Nel A, Odendaal H, van Aardt R. Malnutrition in the elderly residing in long-term care facilities: a cross sectional survey using the Mini Nutritional Assessment (MNA®) screening tool. S Afr J Clin Nutr. 2016;30(2):34–40.
Maeda K, Ishida Y, Nonogaki T, Mori N. Reference body mass index values and the prevalence of malnutrition according to the Global Leadership Initiative on Malnutrition criteria. Clin Nutr. 2019;39:180–4.
Baek MH, Heo YR. Evaluation of the efficacy of nutritional screening tools to predict malnutrition in the elderly at a geriatric care hospital. Nutr Res Pract. 2015;9(6):637–43.
Cascio BL, Logomarsino JV. Evaluating the effectiveness of five screening tools used to identify malnutrition risk in hospitalized elderly: A systematic review. Geriatr Nurs. 2018;39(1):95–102.
Ceolin J, Engroff P, Mattiello R, Schwanke CHA. Performance of Anthropometric Indicators in the Prediction of Metabolic Syndrome in the Elderly. Metab Syndr Relat Disord. 2019;17(4):232–9.
Chao PC, Chuang HJ, Tsao LY, Chen PY, Hsu CF, Lin HC, et al. The Malnutrition Universal Screening Tool (MUST) and a nutrition education program for high risk cancer patients: strategies to improve dietary intake in cancer patients. Biomedicine (Taipei). 2015;5(3):17.
Chourdakis M, Hecht C, Gerasimidis K, Joosten KF, Karagiozoglou-Lampoudi T, Koetse HA, et al. Malnutrition risk in hospitalized children: use of 3 screening tools in a large European population. Am J Clin Nutr. 2016;103(5):1301–10.
Engelheart S, Brummer R. Assessment of nutritional status in the elderly: a proposed function-driven model. Food Nutr Res. 2018;62:1–6.
Hailemariam H, Singh P, Fekadu T. Evaluation of mini nutrition assessment (MNA) tool among community dwelling elderly in urban community of Hawassa city, Southern Ethiopia. BMC Nutr. 2016;2(1):11–8.
Basibuyuk GO, Ayremlou P, Aeidlou SNS, Cinar Z, Ay F, Bektas Y, et al. Evaluation of Malnutrition among Elderly People Living in Nursing Homes by Mini Nutritional Assessment Short Form (MNA-SF) in Turkey. Maedica (Buchar). 2019;14(1):38–44.
Young AM, Kidston S, Banks MD, Mudge AM, Isenring EA. Malnutrition screening tools: Comparison against two validated nutrition assessment methods in older medical inpatients. Nutrition. 2013;29(1):101–6.
Slee A, Birch D, Stokoe D. A comparison of the malnutrition screening tools, MUST, MNA and bioelectrical impedance assessment in frail older hospital patients. Clin Nutr. 2015;34(2):296–301.
Gavriilidou NN, Pihlsgard M, Elmstahl S. Anthropometric reference data for elderly Swedes and its disease-related pattern. Eur J Clin Nutr. 2015;69(9):1066–75.
Zhang J, Zhu W, Qiu L, Huang L, Fang L. Sex- and Age-Specific Optimal Anthropometric Indices as Screening Tools for Metabolic Syndrome in Chinese Adults. Int J Endocrinol. 2018;2018:1067603.
Enoki H, Kuzuya M, Masuda Y, Hirakawa Y, Iwata M, Hasegawa J, et al. Anthropometric measurements of mid-upper arm as a mortality predictor for community-dwelling Japanese elderly: the Nagoya Longitudinal Study of Frail Elderly (NLS-FE). Clin Nutr. 2007;26(5):597–604.
Sanchez-Garcia S, Garcia-Pena C, Duque-Lopez MX, Juarez-Cedillo T, Cortes-Nunez AR, Reyes-Beaman S. Anthropometric measures and nutritional status in a healthy elderly population. BMC Public Health. 2007;7:1–9.
Correa MM, Tomasi E, Thume E, Oliveira ERA, Facchini LA. Waist-to-height ratio as an anthropometric marker of overweight in elderly Brazilians. Razao cintura-estatura como marcador antropometrico de excesso de peso em idosos brasileiros. Cad Saude Publica. 2017;33(5):e00195315.
Dhana K, Kavousi M, Ikram MA, Tiemeier HW, Hofman A, Franco OH. Body shape index in comparison with other anthropometric measures in prediction of total and cause-specific mortality. J Epidemiol Community Health. 2016;70(1):90–6.
Hu H, Wang J, Han X, Li Y, Wang F, Yuan J, et al. BMI, Waist Circumference and All-Cause Mortality in a Middle-Aged and Elderly Chinese Population. J Nutr Health Aging. 2018;22(8):975–81.
Krakauer NY, Krakauer JC. An Anthropometric Risk Index Based on Combining Height, Weight, Waist, and Hip Measurements. J Obes. 2016;2016:8094275.
Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, et al. A better index of body adiposity. Obesity (Silver Spring). 2011;19(5):1083–9.
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One. 2012;7(7):e39504.
Dhana K, Ikram MA, Hofman A, Franco OH, Kavousi M. Anthropometric measures in cardiovascular disease prediction: comparison of laboratory-based versus non-laboratory-based model. Heart. 2015;101(5):377–83.
Maessen MF, Eijsvogels TM, Verheggen RJ, Hopman MT, Verbeek AL, de Vegt F. Entering a new era of body indices: the feasibility of a body shape index and body roundness index to identify cardiovascular health status. PLoS One. 2014;9(9):e107212.
Gowda V, Philip K. Abdominal volume index and conicity index in predicting metabolic abnormalities in young women of different socioeconomic class. Int J Med Sci Public Health. 2016;5(7).
Perissinotto E, Pisent C, Sergi G, Grigoletto F, Enzi G, Group IW. Anthropometric measurements in the elderly: age and gender differences. Br J Nutr. 2002;87(2):177–86.
Wang Q, Xu L, Li J, Sun L, Qin W, Ding G, et al. Association of anthropometric indices of obesity with hypertension in Chinese elderly: an analysis of age and gender differences. Int J Environ Res Public Health. 2018;15(4):801–9.
Zuo M, Huang Y, Ma W, Xue Z, Zhang J, Gong Y. Expert recommendations for tracheal intubation in critically ill patients with noval coronavirus disease. Chin Med Sci J. 2020;10:105–9.
Weir CB, Jan A. BMI classification percentile and cut off points; 2019.
Chang Y, Guo X, Chen Y, Guo L, Li Z, Yu S, et al. A body shape index and body roundness index: two new body indices to identify diabetes mellitus among rural populations in northeast China. BMC Public Health. 2015;15(1):794.
Stefanescu A, Revilla L, Lopez T, Sanchez SE, Williams MA, Gelaye B. Using A Body Shape Index (ABSI) and Body Roundness Index (BRI) to predict risk of metabolic syndrome in Peruvian adults. J Int Med Res. 2020;48(1):1–12.
Bennasar-Veny M, Lopez-Gonzalez AA, Tauler P, Cespedes ML, Vicente-Herrero T, Yañez A, et al. Body adiposity index and cardiovascular health risk factors in Caucasians: a comparison with the body mass index and others. PLoS One. 2013;8(5):e63999.
Quaye L, Owiredu WKBA, Amidu N, Dapare PPM, Adams Y. Comparative Abilities of Body Mass Index, Waist Circumference, Abdominal Volume Index, Body Adiposity Index, and Conicity Index as Predictive Screening Tools for Metabolic Syndrome among Apparently Healthy Ghanaian Adults. J Obes. 2019:1–10.
Lam BCC, Koh GCH, Chen C, Wong MTK, Fallows SJ. Comparison of body mass index (BMI), body adiposity index (BAI), waist circumference (WC), waist-to-hip ratio (WHR) and waist-to-height ratio (WHtR) as predictors of cardiovascular disease risk factors in an adult population in Singapore. PLoS One. 2015;10(4):e0122985.
Control CfD, Prevention. Body mass index: Considerations for practitioners: Cdc; 2011. p. 1–4.
Setiati S, Istanti R, Andayani R, Kuswardhani R, Aryana I, Putu ID, et al. Cut-off of anthropometry measurement and nutritional status among elderly outpatient in Indonesia: multi-centre study. Acta Med Indones. 2010;42(4):224–30.
Kalaiselvi S, Arjumand Y, Jayalakshmy R, Gomathi R, Pruthu T, Palanivel C. Prevalence of under-nutrition, associated factors and perceived nutritional status among elderly in a rural area of Puducherry, South India. Arch Gerontol Geriatr. 2016;65:156–60.
Yang J, Wang F, Wang J, Han X, Hu H, Yu C, et al. Using different anthropometric indices to assess prediction ability of type 2 diabetes in elderly population: a 5 year prospective study. BMC Geriatr. 2018;18(1).
Liu PJ, Ma F, Lou HP, Zhu YN. Comparison of the ability to identify cardiometabolic risk factors between two new body indices and waist-to-height ratio among Chinese adults with normal BMI and waist circumference. Public Health Nutr. 2017;20(6):984–91.
Tian S, Zhang X, Xu Y, Dong H. Feasibility of body roundness index for identifying a clustering of cardiometabolic abnormalities compared to BMI, waist circumference and other anthropometric indices: the China Health and Nutrition Survey, 2008 to 2009. Medicine. 2016;95(34).
Acknowledgements
This study was supported within the scope of the 1001 project titled “Anthropometric Dimensions of Anatolian Older Adult” with the number of TÜBİTAK 115M548.
Funding
This study was funded by Scientific and Technological Research Council of Turkey (TÜBİTAK) via a project no. 115M548.
Author information
Authors and Affiliations
Contributions
GÖB, YB, and SNS conceived of the study, participated in its design and coordination, and helped to draft the manuscript. FA and AD planned and collected the data. PA, WS, and GAV performed the statistical analysis and drafted the manuscript. All authors read and approved the final manuscript.
Authors’ information
Gülüşan Özgün Başıbüyük is an associate professor of Gerontology in the Faculty of Health Sciences, Akdeniz University.
Parvin Ayremlou is a MSc of epidemiology in the Clinical Research Development Unit of Imam Khomeini Hospital, Urmia University of Medical Sciences.
Sakineh Nouri Saeidlou is an associate professor of nutrition sciences in the Food and Beverages
Safety Research Center, Urmia University of Medical Sciences.
Faruk Ay is a technician and MSc of anthropology in Faculty of Literature, Cumhuriyet University.
Akgul Dalkıran is a technician and MSc of Anthropology in Faculty of Literature, Cumhuriyet
University.
Wida Simzari is an assistant professor of Nutrition and Dietetics in School of Health Sciences,
Cappadocia University.
Gábor Áron Vitályos is an associate professor of Anthropology in Faculty of Primary and Pre-
School Education, Eötvös Lorand University.
Yener Bektaş is a professor of Anthropology in the Faculty of Arts and Sciences,
Nevsehir Haci Bektas Veli University.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was issued by the Ethics Committee of Cumhuriyet University, Turkey, with a number 2014-03/15. A written and oral informed consent was presented to each participant prior to participating in the study.
Consent for publication
All participants have been informed and agreed on consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Başıbüyük, G.Ö., Ayremlou, P., Saeidlou, S.N. et al. A comparison of the different anthropometric indices for assessing malnutrition among older people in Turkey: a large population-based screening. J Health Popul Nutr 40, 13 (2021). https://doi.org/10.1186/s41043-021-00228-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-021-00228-z