Abstract
Background
Carbendazim (methyl 2-benzimidazolecarbamate, CASRN: 10605-21-7) exhibits spindle poisoning effects and is widely used as a fungicide. With respect to genotoxicity, carbendazim is deemed to be non-mutagenic in vitro, but it causes indicative DNA damage in vivo and chromosome aberrations in vitro and in vivo. In this study, we examined the mutagenicity of carbendazim in vivo.
Results
MutaMice were treated with carbendazim orally at doses of 0 (corn oil), 250, 500, and 1,000 mg/kg/day once a day for 28 days. A lacZ assay was used to determine the mutant frequency (MF) in the liver and glandular stomach of mice. MutaMice were administered up to the maximum dose recommended by the Organization for Economic Co-operation and Development Test Guidelines for Chemicals No. 488 (OECD TG488). The lacZ MFs in the liver and glandular stomach of carbendazim-treated animals were not significantly different from those in the negative control animals. In contrast, positive control animals exhibited a significant increase in MFs in both the liver and glandular stomach.
Conclusions
Carbendazim is non-mutagenic in the liver and glandular stomach of MutaMice following oral treatment.
Similar content being viewed by others
Introduction
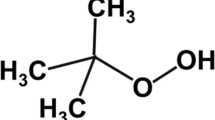
Carbendazim belongs to the benzimidazole fungicide family. Its mode of action involves binding to β-tubulin to disrupt microtubule assembly and inhibit cell division. The antimicrobial efficacy of carbendazim has industrial applications, where it is incorporated as a preservative into paints, films, plastic, concrete, and textiles. It is also sprayed foliar in a wide variety of crops as a pesticide [1, 2].
In Japan, carbendazim is used as a preservative during manufacturing and occupational workers are believed to be exposed to carbendazim. It is listed as an additive on a positive list of the food apparatus, containers, and packaging under “Food Sanitation Act” of Japan. Consumers may ingest small amounts of carbendazim that leaches from these products to food. In developing countries, benzimidazole agents have been indiscriminately used on farmland [3, 4]. A survey in Nepal concluded that on average, 1.91 kg active ingredient/ha of carbendazim is used in vegetable cultivation, although the recommended dose is 0.050–0.250 kg active ingredient/ha [3]. Concerns have been raised that long-term carbendazim exposure may cause DNA damage with insufficient risk regulations and little health protection [3, 5].
The safety of carbendazim was evaluated by the World Health Organization (WHO) in 1993 [6], the FAO/WHO Expert Committee on Pesticide Residues (JMPR) in 1995 and 2005 [2, 7], and European Food Safety Authority (EFSA) in 2010 and 2012 [8, 9]. In 2019, the EU released an assessment report [1]. Most of the data reviewed by the risk assessment bodies include unpublished studies and information could only be obtained from secondary sources.
The biological fate of carbendazim has been described in rodents and livestock. In rats, the xenobiotic profile of carbendazim following oral gavage revealed > 85% gastrointestinal absorption calculated from urinary excretion [10]. Most of the administered radioactivity was excreted within 72 h, primarily in the urine. The excretion half-life is approximately 12 h for both sexes, with residual radioactivity detected only in the liver and carcass [1, 11, 12]. In rats, the proposed biotransformation pathway of carbendazim involves oxidization of the phenyl ring, resulting in the formation of methyl (5-hydroxy-1 H-benzimidazol-2-yl)-carbamate (5-HBC) and 5,6-dihydroxy-carbendazim, which are subsequently conjugated with glucuronic acid and sulfate [10,11,12,13]. The same metabolites were found in mouse urine [11, 14]. Based on a residue analysis in livestock (lactating cow, nonlactating goat, and laying hen), radioactivity in the edible part was marginal after discontinuing the treatment [6, 15,16,17,18]. Carbendazim was extensively biotransformed through oxidation, to form the same metabolites produced in rats and mice. In addition, methyl (4-hydroxy-1 H-benzimidazol-2-yl)-carbamate was detected in livestock [15,16,17,18]. Thus, the biotransformation of carbendazim is not markedly different between species.
Under short-term oral doses of carbendazim, the liver and testis are toxicological targets [1]. Major findings include increased liver weight, decreased testis weight, and azoospermia. Subchronic toxicity studies in rats and dogs, mostly conducted between the 70s and 80s, showed similar effects [11]. Based on hepatotoxicity and testicular toxicity, the no-observed-adverse-effect level (NOAEL) was 163 and 2.7 mg/kg/day in rats and dogs, respectively [11, 19, 20].
In orally dosed long-term toxicity and carcinogenicity studies in mice, rats, and dogs, the liver is the target organ. Carbendazim induces centrilobular hypertrophy (rats and mice) and changes in hematology without histopathological findings (dogs) [1]. Based on hepatotoxicity, the derived NOAEL was 22 mg/kg/day (rat) and 2.6 mg/kg/day (dog) [21]. Neoplastic changes in the liver were observed in two sensitive mouse strains (CD-1 and Swiss), but not in NMRKf mice [11, 22,23,24]. The combined incidence of hepatocellular adenoma and carcinoma in CD-1 mice increased significantly, and the postulated NOAEL was < 81 mg/kg/day [11, 23, 24]. In Swiss mice, neoplastic liver nodules in females and hepatoblastoma in males have been reported, with a NOAEL of 22.5 mg/kg/day [11, 24, 25]. Risk assessment bodies suggest that liver tumors in susceptible mouse strains are not relevant to humans [1, 6, 8]; however, carbendazim caused hepatic aneuploidy in ddY mice [26]. Somatic tumor cells are often aneuploid with chromosome instability and the correlation between aneuploidy and tumorigenesis is still controversial [27,28,29,30,31,32]. Therefore, the risk of carcinogenesis from carbendazim exposure cannot be excluded.
Gene mutation studies in Salmonella typhimurium and Escherichia coli have reported conflicting results [11, 33–38]. Positive results were believed to be derived from the impurities 2, 3-diaminophenazine, 3-amino-2-hydroxyphenazine, and an unidentified chemical. Highly purified carbendazim (purity: > 99.50%) did not cause mutagenicity in the presence of S9 mix with Salmonella typhimurium strains TA98 and TA1538. In contrast, two different batches of technical carbendazim (purity: 97.8% and 90.11%) were positive at levels higher than 5,000 µg/plate [11, 39]. Based on these data, carbendazim was deemed to non-mutagenic in vitro [1, 6, 8]. Positive results in TA98 and TA1535 were reported for three other batches of carbendazim (purity: > 99%) in an unpublished study [11], and it did not cause gene mutations in mammalian cell cultures (HPRT test with Chinese hamster ovary cells, mouse lymphoma tests with L5178Y TK+/− cells) [11, 40,41,42]. In contrast, many studies have demonstrated that carbendazim causes chromosome aberrations in vitro and in vivo [43,44,45,46,47,48,49,50]. Numerical chromosome aberrations are well-defined by identifying kinetochore-positive micronuclei with immunofluorescent antibodies [47] and by examining chromosomes using fluorescence in situ hybridization (FISH) with centromere probes [45, 46]. In mice, carbendazim-induced micronuclei were detected in bone marrow after a single oral dose at 1,646 mg/kg [47], in hepatocytes after a single oral dosing 125–1,000 mg/kg [26], and in the gut following a single oral dose at 500 and 1,000 mg/kg [51]. In rats, micronuclei were detected in the bone marrow after one or two oral doses at 150 mg/kg [52] and in the spermatids after a single oral dose of 100 mg/kg [53]. Of note, the comet assay detected DNA damage that may be converted into a heritable mutation in the lymphocytes and hepatocytes of mice treated with 20 µM drinking water and 20 mg/kg oral carbendazim for subchronic treatment [5, 54].
Carbendazim is deemed to be non-mutagenic in vitro based on unpublished data from secondary sources [1, 6, 8]. Carbendazim primarily targets the liver and testis and induces hepatic tumors in some mouse strains; however, the correlation between aneuploidy and tumorigenicity has not been firmly established [55]. In contrast, long-term persistent genotoxic effects are of concern [4, 5]. In this study, we performed transgenic rodent gene mutation assays to determine whether carbendazim-mediated genotoxicity induces mutations in vivo. For the analysis, we selected the liver, which is a major organ to which carbendazim is distributed. It is for metabolism and associated with tumorigenesis and exhibits high sensitivity in this assay. We also evaluated the glandular stomach, which is directly exposed by a gavage route.
Results
Male MutaMice were orally treated with carbendazim at doses of 0 (corn oil), 250, 500, and 1,000 mg/kg/day once a day for 28 days. Tissues were collected three days after the final treatment. No mortality, clinical signs of toxicity, or treatment-related changes in body weight were observed in either group. In addition, no gross pathological abnormalities were evident in the liver or glandular stomach at necropsy (data not shown).
A lacZ assay was performed to estimate MFs in the liver and glandular stomach (five mice per group). Tables 1 and 2 show the lacZ MFs from the negative control, carbendazim-treated, and positive control (N-ethyl-N-nitrosourea (ENU)-treated animals) tissues. In the liver, lacZ MFs (×10− 6) were 41.2 ± 12.8, 39.2 ± 9.0, and 45.7 ± 15.7 (mean ± SD), respectively, in the 250, 500, and 1,000 mg/kg/day treatment group, which were not significantly different from that of the negative control animals (40.9 ± 11.6). In contrast, lacZ MF (×10− 6) in the positive controls (108.1 ± 23.8) was significantly increased compared with that in the negative control animals (p < 0.05, Student’s t-test).
In the glandular stomach, lacZ MFs (×10− 6) were 38.9 ± 10.5, 41.1 ± 11.9, and 37.7 ± 7.2, respectively, in the 250, 500, and 1,000 mg/kg/day treatment group, which was not significantly different from that of the negative control animals (40.6 ± 10.4). In contrast, lacZ MF (×10− 6) in the positive controls (396.1 ± 53.8) was significantly increased from that in the negative control animals (p < 0.05, Aspin–Welch’s t-test).
Discussion
In this study, we determined whether in vivo genotoxicity, such as DNA damage, micronucleus formation, and aneuploidy caused by carbendazim, result in gene mutations in vivo. We set the doses at 250, 500, and 1,000 mg/kg/day based on the results of range-finding toxicity studies, in which 1,000 mg/kg/day was the maximum dosage recommended by the guidelines. No toxicological changes in body weight, gross observations, or necropsy findings in the liver and glandular stomach were observed in the MutaMice. The xenobiotic profiles of mice and rats are comparable and gastrointestinal absorption after oral dosing is rapid and high [10, 11, 14]; therefore, carbendazim was assumed to be systemically absorbed by the gastrointestinal tract and distributed via the liver [10,11,12]. Genotoxicity studies in mice revealed colon and bone marrow micronuclei after a single oral dose of 500 and 1,646 mg/kg, respectively [47, 51]. DNA strand breaks were observed in male Swiss mouse lymphocytes after a 90-day treatment of 5.4 mmol/kg/day carbendazim in drinking water (approximately 1 mg/kg/day) [5]. The mice exhibited DNA damage, but no change in body weight, food and water consumption, or gross behavior [5]. Based on our results and other studies, we hypothesize that carbendazim reaches the glandular stomach and liver without showing visible signs of toxicity.
Conflicting results can occur in bacterial assays because of mutagenic contaminants; however, carbendazim itself did not show mutagenic potential according to several risk assessment reports [1, 2, 6, 8]. Although a risk assessment decision was publicly announced, the underlying data were not published. Therefore, we could not evaluate these studies. Here, we show that the MFs in the liver and glandular stomach tissue of carbendazim-treated animals were similar to those of the negative control animals. This confirms that carbendazim did not cause mutations in the liver and glandular stomach in vivo, and the development of liver tumors may occur through a non-mutagenic mode of action. Tumorigenic responses to carbendazim were observed in CD-1 and Swiss mice. In long-term toxicity and carcinogenicity studies, CD-1 and Swiss mice treated with carbendazim showed hepatic alterations, such as increased weight, centrilobular hepatocellular swelling or necrosis, focus/foci of eosinophilic cellular alterations, and nodular hyperplasia [11, 23, 24]. Benomyl, a benzimidazole family fungicide and carbendazim precursor, caused hepatic tumors in CD-1 and Swiss mice as well as hepatocellular toxicity followed by cell proliferation and cytochrome P450 induction in a subchronic (28-day) feeding study [56, 57]. Thus, benomyl and carbendazim induce hepatic neoplasms after hepatic alterations [56]. Oral exposure to carbendazim resulted in hepatic numerical aberrations in ddY mice bearing resected livers [26]. Carbendazim-induced chromosomal instability and hepatotoxicity may be one possible mechanism of tumorigenesis. The role of aneuploidy in carcinogenesis has not been fully established and it may not have a primary causative role [32]. Therefore, further mechanistic studies on carbendazim-mediated carcinogenesis are warranted.
Aneuploidy in germ cells results in infertility and pregnancy loss [58, 59]. Carbendazim treatment did not cause any histopathological changes in female reproductive organs and had no estrogenic or anti-estrogenic effect on uterine weight [4]. However, carbendazim reaches the oocytes and induces aneuploidy, suggesting a correlation between aneugenic oocytes and implantation loss [48, 50, 60, 61]. Numerical chromosome aberrations in the spermatids of carbendazim-treated rats suggest concomitant testicular toxicity [62, 63]. With respect to reproduction and developmental toxicity, carbendazim caused testicular toxicity, characterized by vacuolization of Sertoli cells as well as sloughing and elongation of spermatids and spermatocytes [63,64,65,66,67]. In addition, carbendazim altered serum LH, FSH, testosterone, and GnRH levels [68, 69]. This suggests that carbendazim-mediated reproductive and developmental toxicity may also have an endocrine mode of action, although contradictory results have been reported [4]. Our study was designed to examine the mutagenic potency of carbendazim in somatic cells. Meanwhile, OECD TG488 requires prolonged fixation time, such as 28 days of exposure and 28 days of fixation in germ cells [70, 71]. Further studies are needed to elucidate the overall mechanism of toxicity by carbendazim.
Our results provide convincing evidence that carbendazim is non-mutagenic and that a threshold mechanism may occur, which results in its toxicity and carcinogenicity. Because the dietary risk of carbendazim has not been evaluated in Japan, these results are meaningful for risk assessment and regulation.
Conclusions
We performed transgenic rodent gene mutation assays using MutaMice to evaluate the mutagenicity of orally administered carbendazim. Although MutaMice were administered up to the maximum dose recommended by the OECD guidelines, lacZ MFs in the liver and glandular stomach of carbendazim-treated animals were not affected. Our results indicate that carbendazim is non-mutagenic in the liver and glandular stomach of MutaMice following oral exposure.
Methods
This study was conducted by OECD TG 488 [72] at the BioSafety Research Center (BSRC; Shizuoka, Japan) in compliance with “Act on Welfare and Management of Animals” [73], “Standards relating to the Care and Keeping and Reducing Pain of Laboratory Animals” [74], “BSRC Guidelines for Animal Experimentation,” and “Act on the Conservation and Sustainable Use of Biological Diversity through Regulations on the Use of Living Modified Organisms” [75]. The study was approved by the BSRC Safety Management Regulations for Recombinant DNA Experiment.
Test chemicals and reagents
Carbendazim (CASRN: 10605-21-7, Lot no. MKCM2970, purity: 97%) was purchased from Sigma-Aldrich Japan (Tokyo, Japan). ENU (CASRN: 759-73-9), a positive control, was purchased from Toronto Research Chemicals Inc. (Ontario, Canada). Corn oil was purchased from FUJIFILM Wako Pure Chemical Corp. (Osaka, Japan). Carbendazim was suspended in corn oil. The dosing formulations were stored at room temperature until use and used within 8 days after preparation. Stability and uniformity during storage were verified. ENU was dissolved in phosphate buffer (pH 6.0) before administration.
Animals and breeding conditions
We purchased male and female CD2F1 mice as well as male MutaMice (CD2-LacZ80/HazfBR), aged 8 weeks, from Japan SLC, Inc. (Shizuoka, Japan) and Trans Genic Inc. (Fukuoka, Japan). Food (CRF-1, Oriental Yeast, Japan) and water were provided ad libitum. The animals were maintained at 20–26 °C, 35–70% relative humidity, 12-h light/dark cycle, and 12 air changes per hour. The animals were acclimatized for 8 days before beginning treatment.
Dose selection
In a range-finding toxicity study, four groups of three male and three female CD2F1 mice were administered 30, 100, 300, or 1,000 mg/kg/day of carbendazim in a volume of 10 mL/kg once daily for 14 days. The highest dose was established based on OECD TG 488, and the four levels were divided by a geometric ratio of three. Body weight was recorded on days 1, 8, and 15 (next day of the last dosing) and mortality and clinical signs were checked daily. The surviving animals were euthanized with CO2 on day 15. There were no obvious sex differences in the range-finding toxicity study; therefore, only male mice were included in the main study. Mortality, clinical signs of toxicity, or treatment-related body weight changes were not observed up to the highest tested dose. We set the main study dosage at 0, 250, 500, and 1,000 mg/kg/day, up to the maximum dosage recommended by the guidelines for 28-day repeated administration.
Treatments and tissue isolation
Four groups containing six male MutaMice each were administered 0 (vehicle: corn oil), 250, 500, and 1,000 mg/kg/day carbendazim at a constant volume of 10 mL/kg once daily for 28 days. The mice were euthanized three days after the final treatment. Body weight was recorded on days 1, 8, 15, 22, 29, and 31 (before tissue isolation), and mortality and clinical signs were checked daily. Positive controls were administered 100 mg/kg/day ENU by intraperitoneal injection on days 2 and 3 once daily. The mice were euthanized 10 days after the final treatment. Body weight was recorded on days 1 and 13 (before the tissue isolation). Mortality and clinical signs were checked daily in the positive control group.
The liver and stomach were isolated and a gross pathological examination was conducted. Two points of the left lateral lobe of the liver were hollowed out and frozen in liquid N2. The forestomach and glandular stomach were separated and the glandular stomach was frozen in liquid N2. Frozen samples were stored in an ultradeep freezer at −80 °C until further analysis.
Genomic DNA isolation
Genomic DNA was isolated from the tissues of five animals in each group in ascending order of animal ID as described previously [76]. Briefly, frozen tissue was homogenized using a pestle in Dounce buffer and the homogenized tissue was transferred to an ice-cold centrifuge tube containing 0.5 mol/L sucrose. After centrifugation at 1,750 × g for 10 min, the supernatant was removed. Precipitated nuclei/cells were resuspended in 3 mL of Dounce buffer containing 0.002% RNase (NIPPON GENE Co., Ltd.), mixed with 3 mL of 0.2% proteinase K solution (FUJIFILM Wako Pure Chemical Co., Ltd.), and incubated at 50 °C for 2 h. The suspension was mixed with an equal volume of phenol/chloroform (1:1), rotated for 10 min, and centrifuged at 1,220 × g for 10 min. The aqueous layer was collected and extracted twice with phenol: chloroform. The aqueous layer was mixed with an equal amount of chloroform: isoamyl alcohol (24:1) and extracted in the same manner. Genomic DNA was precipitated by adding ethanol to the aqueous layer. The precipitated DNA was rinsed with 70% ethanol for 10 min, placed at room temperature, air-dried overnight, and dissolved in TE buffer (NIPPON GENE Co., Ltd.). The purified DNA was stored in a refrigerator NanoDrop (AGC TECHNO GLASS Co., Ltd.) was used to determine the DNA concentration.
In vitro packaging
Lambda in vitro packaging reaction was performed for transgene rescue based on the Transpack instruction manual (Agilent Technologies, Transpack Packaging Extract Catalog #200,220, #200,221, and #200,223). Approximately 10 µL of genomic DNA (200–600 µg/mL) was gently mixed with the Transpack packaging reagent, incubated twice at 30 °C for 1.5 h, and mixed with 700 µL of SM buffer to stop the reaction.
MF determination
A lacZ mutation assay was performed as previously described [76]. Briefly, a mixture of E. coli C (lacZ−, gal E−) cell suspension and the total packaged sample were incubated for 30 min. The rescued phages were absorbed into E. coli. An aliquot of this suspension was diluted and mixed with LB top agar for titer plates. The remaining cell suspension was mixed with LB top agar containing phenyl-β-D-galactoside for selection. Both plates were incubated overnight at 37 °C. MFs were calculated by dividing the total number of mutant plaques on the selection plates by the total number of rescued phages.
Statistical analysis
Bartlett’s test was used to compare the homogeneity of variances across the groups. When homogeneity was detected, Dunnett’s test was used for analysis. Steel’s test was used for non-homogeneous data. Based on the results of an F-test, a Student’s t-test or Aspin–Welch’s t-test was used to compare MFs between negative and positive controls. The criterion for significance was set at 5% probability.
Data availability
All available data are presented in this article.
Abbreviations
- MF:
-
mutant frequency
- OECD:
-
Organization for Economic Co-operation and Development
- WHO:
-
World Health Organization
- JMPR:
-
FAO/WHO Expert Committee on Pesticide Residues
- EFSA:
-
European Food Safety Authority
- NOAEL:
-
no-observed-adverse-effect level
- ENU:
-
N-ethyl-N-nitrosourea
- LH:
-
luteinizing hormone
- FSH:
-
follicle stimulating hormone
- GnRH:
-
gonadotropin-releasing hormone
References
EU, Carbendazim. assessment report. 2019. https://echa.europa.eu/information-on-chemicals/biocidal-active-substances/-/disas/factsheet/1260/PT07. Accessed 8 Dec 2023.
JMPR, Carbendazim. (addendum). 2005. https://apps.who.int/pesticide-residues-jmpr-database/pesticide?name=CARBENDAZIM. Accessed 8 Dec 2023.
Bhandari G, Atreya K, Yang X, Fan L, Geissen V. Factors affecting pesticide safety behaviour: the perceptions of Nepalese farmers and retailers. Sci Total Environ. 2018;631–632:1560–71.
Rama EM, Bortolan S, Vieira ML, Gerardin DCC, Moreira EG. Reproductive and possible hormonal effects of carbendazim. Regul Toxicol Pharmacol. 2014;69:476–86.
Rai B, Mercurio SD. Environmentally relevant exposures of male mice to carbendazim and thiram cause persistent genotoxicity in male mice. Environ Sci Pollut Res Int. 2020;27:10629–41.
WHO. Environmental Health Criteria (EHC) 149 Carbendazim. 1993. https://apps.who.int/iris/bitstream/handle/10665/37443/9241571497-eng.pdf?sequence=1. Accessed 8 Dec 2023.
JMPR. Pesticide residues in food Part II Toxicology and environmental. 1995. https://www.inchem.org/documents/jmpr/jmpmono/v95pr04.htm. Accessed Dec 8 2023.
EFSA. Conclusion on the peer review of the pesticide risk assessment of the active substance carbendazim. EFSA J. 2010;8.
EFSA. Reasoned opinion on the modification of the existing MRLs for thiophanate-methyl and carbendazim in apples and pears. EFSA J. 2012;10.
Krechniak J, Kłosowska B. The fate of 14C-carbendazim in rat. Xenobiotica. 1986;16:809–15.
EU. Draft re-assessment report carbendazim. B-6: Toxicology and metabolism. 2009. https://www.efsa.europa.eu/en/consultations/call/public-consultation-active-substance-carbendazim. Accessed 8 Dec 2023.
Monson KD. Metabolism of [phenyl(U)-14C]carbendazim in rats (1990). Wilmington, Delaware, E.I. Du Pont de Nemours and Co., Inc. (unpublished data) cited in EHC (1993).
Monson KD. Release and characterization of bound benomyl and carbendazim metabolites in animal tissues via Raney nickel desulfurization and acid dehydration. J Agric Food Chem. 1991;39:1808–11.
Dorn E, Schmidt E, Kellner HM, Leist KH. HOE 017411-14C (carbendazim-14C) metabolic fate in rats and mice, a comparison (1983). Frankfurt, Germany, Hoechst AG. (unpublished data) cited in EHC (1993).
Monson KD. Metabolism of [2-14C]-carbendazim in the lactating dairy cow (1985). Wilmington, Delaware, E.I. Du Pont de Nemours and Co., Inc. (Unpublished data) cited in EHC (1993).
Johnson JD. Determination of the plateau level of bound [phenyl(U)-14C]carbendazim residues in goat liver (1988). Columbus, Ohio, Battelle Columbus Division (Unpublished data) cited in EHC (1993).
Monson KD. Metabolism of [2-14C]-carbendazim in laying hens (1986). Wilmington, Delaware, E.I. Du Pont de Nemours and Co., Inc. (unpublished data) cited in EHC (1993).
Eckert J, Stauffer R, Hoppman D. Determination of MBC, 4-OH MBC, and 5-OH MBC in chicken eggs, tissues and feces (1985). Bernville, Pennsylvania, Enviro-Bio-Tech Ltd. (unpublished data) cited in EHC (1993).
Scholz S. Report on a subchronic feeding experiment (93 days) with technical active substance Hoe 17 411OF (1973). (unpublished data) cited in EFSA (2010) and EU assessment report (2019).
Sherman H, Barnes JR, Aftosmis JG, Zapp JA. Three-month feeding study on dogs with benzimidazole, 2-amino (INB-572) (1970). (unpublished data) cited in EFSA (2010) and EU assessment report (2019).
Sherman H. Long-term feeding studies in rats and dogs with 2-benzimadazole carbamic acid, methyl ester (INE-965) (50% and 70% MBC wettable powder formulations). Parts I and II (1972). Newark, Delaware, E.I. Du Pont de Nemours and Co., Inc., Haskell Laboratory (Unpublished data) cited in EHC (1993), EFSA (2010), and EU assessment report (2019).
Donaubauer HH, Schuetz E, Weigand W, Kramer M. Repeated dose (24 month) feeding study for determination of the carcinogenic effect of HOE 17411 OFAT204 (carbendazim) in mice (1982). Frankfurt, Germany, Hoechst AG, Pharmaceuticals Research, Toxicology Section (Unpublished data) cited in EHC (1993), EFSA (2010), and EU assessment report (2019).
Wood CK. Long-term feeding study with 2-benzimidazolecarbamate, methyl ester (< 99% MBC, INE-965) in mice. Parts I and II (1982). Newark, Delaware, E.I. Du Pont de Nemours and Co., Inc., Haskell Laboratory. (Unpublished data) cited in EHC (1993), EFSA (2010), and EU assessment report (2019).
Beems RB, Til HP, van der Heijden CA. Carcinogenicity study with carbendazim (99% MBC) in mice (1976). The Hague, Central Institute for Nutrition and Food Research (TNO) (unpublished data) cited in EHC (1993), EFSA (2010), and EU assessment report (2019).
Mohr U. Review of liver sections from mice and rats fed with carbendazim (1977). (Unpublished data) cited in EHC (1993).
Igarashi M, Setoguchi M, Takada S, Itoh S, Furuhama K. Optimum conditions for detecting hepatic micronuclei caused by numerical chromosome aberration inducers in mice. Mutat Res. 2007;632:89–98.
Naylor RM, van Deursen JM. Aneuploidy in cancer and aging. Annu Rev Genet. 2016;50:45–66.
Orr B, Compton DA. A double-edged sword: how oncogenes and tumor suppressor genes can contribute to chromosomal instability. Front Oncol. 2013;3:164.
Weaver BA, Silk AD, Montagna C, Verdier-Pinard P, Cleveland DW. Aneuploidy acts both oncogenically and as a tumor suppressor. Cancer Cell. 2007;11:25–36.
Pfau SJ, Amon A. Chromosomal instability and aneuploidy in cancer: from yeast to man. EMBO Rep. 2012;13:515–27.
Ricke RM, van Ree JH, van Deursen JM. Whole chromosome instability and cancer: a complex relationship. Trends Genet. 2008;24:457–66.
Tweats D, Eastmond DA, Lynch AM, Elhajouji A, Froetschl R, Kirsch-Volders M, et al. Role of aneuploidy in the carcinogenic process: part 3 of the report of the 2017 IWGT workgroup on assessing the risk of aneugens for carcinogenesis and hereditary diseases. Mutat Res Genet Toxicol Environ Mutagen. 2019;847:403032.
Pandita TK. Assessment of the mutagenic potential of a fungicide bavistin using multiple assays. Mutat Res. 1988;204:627–43.
Albertini S. Influence of different factors on the induction of chromosome malsegregation in Saccharomyces cerevisiae D6l.M by Avistan and assessment of its genotoxic property in the Ames test and in Saccharomyces cerevisiae D7. Mutat Res. 1989; 216 327– 40.
Ficsor G, Bordas S, Stewart SJ. Mutagenicity testing of benomyl, methyl-2-benzimidazole carbamate, streptozotocin and N-methyl-N’-nitro-N-nitrosoguanidine in Salmonella typhimurium in vitro and in rodent host-mediated assays. Mutat Res. 1978;51:151–64.
Gericke D. Test for mutagenicity in bacteria strains in the absence and presence of a liver preparation (1977). Frankfurt, Germany, Hoechst AG, Laboratory for Cancer Research (unpublished data) cited in EHC (1993).
Arce GT. Mutagenicity evaluation in Salmonella typhimurium (1984). Newark, Delaware, E.I. Du Pont de Nemours and Co., Inc., Haskell Laboratory (Unpublished data) cited in EHC (1993).
Donovan SD. Mutagenicity evaluation in Salmonella typhimurium (1982). Newark, Delaware, E.I. Du Pont de Nemours and Co.,Inc., Haskell Laboratory (Unpublished data) cited in EHC (1993).
Reynolds VL, Sarrif AM. Evaluation of carbendazim for gene mutations in the salmonella/Ames plate incorporation assay: The role of aminophenazine impurities (1993). (unpublidhed data) cited in EFSA (2010) and EU assessment report (2019).
Waterer JC. Chinese hamster ovary cell assay for mutagenicity (1980). Newark, Delaware, E.I. Du Pont de Nemours and Co., Inc., Haskell Laboratory (Unpublished data) cited in EHC (1983).
Adams K, Scammell R. Carbendazim - Mammalian cell mutation assay (1996). (unpublished data) cited in EU assessment report (2019).
McCooey KT, Arce GT, Sarrif AM. L5178Y mouse lymphoma cell assay for mutagenicity (1983). (unpublished data) cited in EU assessment report (2019).
Kirsch-Volders M, Vanhauwaert A, Eichenlaub-Ritter U, Decordier I. Indirect mechanisms of genotoxicity. Toxicol Lett. 2003;140–141:63–74.
Bentley KS, Kirkland D, Murphy M, Marshall R. Evaluation of thresholds for benomyl- and carbendazim-induced aneuploidy in cultured human lymphocytes using fluorescence in situ hybridization. Mutat Res. 2000;464:41–51.
Elhajouji A, Van Hummelen P, Kirsch-Volders M. Indications for a threshold of chemically-induced aneuploidy in vitro in human lymphocytes. Environ Mol Mutagen. 1995;26:292–304.
Elhajouji A, Tibaldi F, Kirsch-Volders M. Indication for thresholds of chromosome non-disjunction versus chromosome lagging induced by spindle inhibitors in vitro in human lymphocytes. Mutagenesis. 1997;12:133–40.
Sarrif AM, Bentley KS, Fu LJ, O’Neil RM, Reynolds VL, Stahl RG. Evaluation of benomyl and carbendazim in the in vivo aneuploidy/micronucleus assay in BDF1 mouse bone marrow. Mutat Res. 1994;310:143–9.
Jeffay SC, Libbus BL, Barbee RR, Perreault SD. Acute exposure of female hamsters to carbendazim (MBC) during meiosis results in aneuploid oocytes with subsequent arrest of embryonic cleavage and implantation. Reprod Toxicol. 1996;10:183–9.
Seiler JP. The mutagenicity of benzimidazole and benzimidazole derivatives. VI. Cytogenetic effects of benzimidazole derivatives in the bone marrow of the mouse and the Chinese hamster. Mutat Res. 1976;40:339–47.
Zuelke KA, Perreault SD. Carbendazim (MBC) disrupts oocyte spindle function and induces aneuploidy in hamsters exposed during fertilization (meiosis II). Mol Reprod Dev. 1995;42:200–9.
Vanhauwaert A, Vanparys P, Kirsch-Volders M. The in vivo gut micronucleus test detects clastogens and aneugens given by gavage. Mutagenesis. 2001;16:39–50.
Ashby J, Tinwell H. Continuing ability of the rodent bone marrow micronucleus assay to act as a predictor of the possible germ cell mutagenicity of chemicals. Mutat Res. 2001;478:211–3.
Matsuo F, Nakai M, Nasu T. The fungicide carbendazim induces meiotic micronuclei in the spermatids of the rat testis. J Vet Med Sci. 1999;61(5):573–6.
Ðikić D, Mojsović-Cuić A, Cupor I, Benković V, Horvat-Knezević A, Lisicić D, et al. Carbendazim combined with imazalil or cypermethrin potentiate DNA damage in hepatocytes of mice. Hum Exp Toxicol. 2012;31:492–505.
Lynch AM, Eastmond D, Elhajouji A, Froetschl R, Kirsch-Volders R, Marchetti F, et al. Targets and mechanisms of chemically induced aneuploidy. Part 1 of the report of the 2017 IWGT workgroup on assessing the risk of aneugens for carcinogenesis and hereditary diseases. Mutat Res Genet Toxicol Environ Mutagen. 2019:403025.
McCarroll NE, Protzel A, Ioannou Y, Frank Stack H, Jackson M, Waters M, et al. A survey of EPA/OPP and open literature on selected pesticide chemicals III. Mutagenicity and carcinogenicity of benomyl and carbendazim. Mutat Res. 2002;512:1–35.
Van Pelt CS. Twenty-eight-day feeding study with benomyl in mice, final report; study no. 324– 90, (1990) Haskell Laboratory (unpublished data) cited in McCarroll et al. Mutat Res. 2002;512:1–35.
More SJ, Bampidis V, Bragard C, Halldorsson TI, Hernandez-Jerez AF, Bennekou SH, et al. Guidance on aneugenicity assessment. EFSA Scientific Committee (SC). EFSA J. 2021;19:6770.
Pacchierotti F, Masumura K, Eastmond DA, Elhajouji A, Froetschl R, Kirsch-Volders M, et al. Chemically induced aneuploidy in germ cells. Part II of the report of the 2017 IWGT workgroup on assessing the risk of aneugens for carcinogenesis and hereditary diseases. Mutat Res Genet Toxicol Environ Mutagen. 2019;848:403023.
Hummler E, Hansmann I. Pattern and frequency of nondisjunction in oocytes from the djungarian hamster are determined by the stage of first meiotic spindle inhibition. Chromosoma. 1988;97:224–30.
Perreault SD, Jeffay S, Poss P, Laskey JW. Use of the fungicide carbendazim as a model compound to determine the impact of acute chemical exposure during oocyte maturation and fertilization on pregnancy outcome in the hamster. Toxicol Appl Pharmacol. 1992;114:225–31.
de Stoppelaar JM, van de Kuil T, Bedaf M, Verharen HW, Slob W, Mohn GR, et al. Increased frequencies of diploid sperm detected by multicolour FISH after treatment of rats with carbendazim without micronucleus induction in peripheral blood erythrocytes. Mutagenesis. 1999;14:621–31.
Nakai M, Hess RA. Effects of carbendazim (methyl 2-benzimidazole carbamate; MBC) on meiotic spermatocytes and subsequent spermiogenesis in the rat testis. Anat Rec. 1997;247:379–87.
Correa LM, Nakai M, Strandgaard CS, Hess RA, Miller MG. Microtubules of the mouse testis exhibit differential sensitivity to the microtubule disruptors carbendazim and colchicine. Toxicol Sci. 2002;69:175–82.
Hess RA, Nakai M. Histopathology of the male reproductive system induced by the fungicide benomyl. Histol Histopathol. 2000;15:207–24.
Nakai M, Hess RA. Morphological changes in the rat sertoli cell induced by the microtubule poison carbendazim. Tissue Cell. 1994;26:917–27.
Nakai M, Hess RA, Moore BJ, Guttroff RF, Strader LF, Linder RE. Acute and long-term effects of a single dose of the fungicide carbendazim (methyl 2-benzimidazole carbamate) on the male reproductive system in the rat. J Androl. 1992;13:507–18.
Goldman JM, Rehnberg GL, Cooper RL, Gray LE, Hein JF, McElroy WK. Effects of the benomyl metabolite, carbendazim, on the hypothalamic-pituitary reproductive axis in the male rat. Toxicology. 1989;57:173–82.
Rehnberg GL, Cooper RL, Goldman JM, Gray LE, Hein JF, McElroy WK. Serum and testicular testosterone and androgen binding protein profiles following subchronic treatment with carbendazim. Toxicol Appl Pharmacol. 1989;101:55–61.
Marchetti F, Aardema M, Beevers C, van Benthem J, Douglas GR, Godschalk R, et al. Simulation of mouse and rat spermatogenesis to inform genotoxicity testing using OECD test guideline 488. Mutat Res Genet Toxicol Environ Mutagen. 2018;832–833:19–28.
Marchetti F, Aardema MJ, Beevers C, van Benthem J, Godschalk R, Williams A, et al. Identifying germ cell mutagens using OECD test guideline 488 (transgenic rodent somatic and germ cell gene mutation assays) and integration with somatic cell testing. Mutat Res Genet Toxicol Environ Mutagen. 2018;832–833:7–18.
OECD. Test No. 488: Transgenic rodent somatic and germ cell gene mutation assays. https://www.oecd-ilibrary.org/environment/test-no-488-transgenic-rodent-somatic-and-germ-cell-gene-mutation-assays_9789264203907-en. Accessed 8 Dec 2023.
Act on Welfare and Management of Animals (Act No. 105 of 1973). https://www.japaneselawtranslation.go.jp/en/laws/view/3798. Accessed 8 Dec 2023.
Standards relating to the Care and Keeping and Reducing Pain of Laboratory Animals. (Notice of the Ministry of the Environment (No. 88 of 2006). https://www.env.go.jp/nature/dobutsu/aigo/2_data/laws/nt_h25_84_en.pdf. Accessed 8 Dec 2023.
Act on the conservation. and sustainable use of biological diversity through regulations on the use of living modified organisms (Act No. 97 of 2003). https://www.japaneselawtranslation.go.jp/en/laws/view/3252. Accessed 8 Dec 2023.
Murata Y, Natsume M, Iso T, Shigeta Y, Hirose N, Umano T, et al.In vivo mutagenicity assessment of styrene in MutaMouse liver and lung. Genes Environ. 2023;45:12.
Acknowledgements
The Ministry of Health, Labour and Welfare, Japan, provided funding for this research.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
TI wrote the manuscript, K.Suzuki conducted the experiments, KH, K.Sugiyama and KM administered the experiments, MM administered the project, and AH conceptualized the project. All authors have reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional animal care and use committee approved the animal experiments in this study, which followed the recommendations for animal handling, maintenance, treatment, and sacrifice.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Authors’ information
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Iso, T., Suzuki, K., Murata, Y. et al. Lack of in vivo mutagenicity of carbendazim in the liver and glandular stomach of MutaMice. Genes and Environ 46, 7 (2024). https://doi.org/10.1186/s41021-024-00299-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41021-024-00299-4