Abstract
Background
Craniopharyngioma is a common intracranial tumor located in the sellar-suprasellar region. Due to the involvement of adjacent structures, it can lead to increased intracranial pressure, visual impairment, and endocrine deficiencies. Surgical resection is the primary treatment, but it is a tough challenge to achieve total resection, which will led to the frequency of recurrences and progressions. Among them, distant spread is extremely rare, but important complication, identifying and providing proper therapy, is crucial.
Methods
We report two cases of ectopic recurrence craniopharyngioma and make a literature review for the published similar case reports.
Results
Our literature review revealed 63 cases (including our patient). The onset age in children group and adult group ranges from 2–14 years old (6.70 ± 3.33) to 17–73 years old (40.63 ± 15.58), while the interval year between tumor initiation and ectopic recurrence ranges from 0.17–20 (7.28 ± 6.76) years to 0.3–34 (6.85 ± 7.29). Achieving gross total resection seems not to prevent the ectopic recurrence. The major pathology of ectopic recurrence craniopharyngioma is adamantinomatous type. The most common site of ectopic recurrence is frontal lobe. According to the pathogenesis, 35 cases were seeding along the surgical approach, and 28 cases were seeding via the CSF pathway.
Conclusion
Ectopic recurrence craniopharyngioma is rare, but it can lead to serious symptoms. Delicate surgical procedure can help to reduce the risk of ectopic recurrence, and standardized follow-up can provide valuable information for treatment.
Similar content being viewed by others
Background
Craniopharyngioma is a rare malformational tumor of low histological malignancy, and two primary subtypes have been recognized (adamantinomatous and papillary) as yet. It originates from the remnants of Rathke’s pouch and mainly occurs in sellar-suprasellar region [1]. However, some rarely distant spread had been reported. This ectopic recurrence mainly disseminates along the surgical approach or via the cerebrospinal fluid (CSF) pathway. In this study, we report two cases of ectopic recurrence craniopharyngioma and make a literature review for the published similar case reports to introduce some experience with the management of ectopic recurrence craniopharyngioma. All the patients consented to the procedure.
Case presentation
Case 1
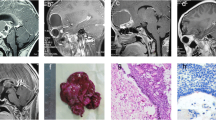
A 49-year-old female patient initially complained of vision loss and nausea in 2005. A sellar lesion had been detected and subtotally resected by craniotomy. The lesion was histologically determined to be an adamantinomatous craniopharyngioma. As supplementary therapy, the patient received gamma-knife treatment in 3 months and 12 months after operation. In 2012, the patient suffered severe nausea and vomiting again. The MR scan displayed tumor recurrence in the sellar region, with a cystic lesion extend to the right frontal lobe (Fig. 1A). These two lesions had been simultaneously resected through a transcranial surgery (Fig. 1B), and the pathology showed both were adamantinomatous craniopharyngioma (Ki-67 = 3%). However, in 2021, it had been found tumor recurrence in the sellar region; even worse, there was a new isolated lesion in the right frontal lobe (Fig. 1C). She received tumor resection therapy via the same transcranial approach (Fig. 1D), and the pathological staining confirmed the adamantinomatous craniopharyngioma with Ki-67 2% (Fig. 1E).
MRI, CT scans, and pathological features of case 1. A Preoperative MRI showed a cystic solid lesion in the sellar-suprasellar region extending to the right frontal lobe in 2012. B Postoperative CT scan showed total resection of the right frontal lesion. C MRI scan showed tumor recurrence in both the sellar-suprasellar region and the right frontal lobe in 2021. D Postoperative CT scan showed total resection of the two lesions. E The pathological features showed typical morphology of adamantinomatous craniopharyngioma
Case 2
A 63-year-old female patient suffered from bilateral vision loss for 6 months before the first diagnosis as craniopharyngioma in 2017. The patient received a subtotal resection of the tumor by craniotomy in other hospital. Her vision had partially recovered after operation. However, in 2019, the patient felt vision loss again, while the MR scan showed the tumor had recurred not only in the initial site but also in the right temporal lobe with a 1.2 × 0.9-cm lesion (Fig. 2A). Due to the small lesion volume and lack of related symptoms, this patient decided to resect the tumor in the suprasellar region by transsphenoidal surgery firstly (Fig. 2B) and did a close follow-up to the right temporal lesion. One year postoperatively in 2020, the patient suffered serious symptoms like worse vision, bluntness, and drowsiness. The MR scan displayed tumor recurrence in the suprasellar region, and the right temporal lesion had enlarged (Fig. 2C). A craniotomy surgery was performed to resect both lesions and place an Ommaya catheter in the cyst (Fig. 2D). In 2021, unfortunately, the tumor relapsed rapidly (Fig. 1E). The pathology of both lesions was adamantinomatous craniopharyngioma (Fig. 2 F–G), with a higher Ki-67 index (5%) of the ectopic recurrence compared with that (3%) in initial site.
MRI, CT scans, and pathological features of case 2. A Preoperative MRI showed a cystic and solid lesion in the sellar-suprasellar region and a small lesion in the right temporal lobe in 2019. B CT scan after endoscopic transsphenoidal surgery. C MRI scan showed tumor recurrence with cyst in the suprasellar region and enlargement of the lesion in the right temporal lobe in 2020. D CT scan after transcranial surgery and Ommaya reservoir implantation. E MRI scan showed tumor recurrence again in the suprasellar region in 2021. F The pathological features of suprasellar lesion showed adamantinomatous craniopharyngioma. G The pathological features of right temporal lobe lesion also showed adamantinomatous craniopharyngioma
Discussion
Craniopharyngioma is a benign epithelial tumor and accounts for 0.5–2.5 cases per 1 million population every year [2–4]. It originates from the sellar region, specifically the craniopharyngeal duct [1]. The main symptoms are caused by compression of adjacent tissues such as visual disturbance (optic nerve), endocrine disorder (pituitary gland), personality changes (hypothalamus), and hydrocephalus (third ventricle) [5, 6]. The primary therapy is surgical resection. However, due to the unpredictable growth pattern and involvement of critical anatomical structures, it is difficult to achieve total resection and apt to relapse.
Ectopic recurrence craniopharyngioma is rare. Up to date, only 61 patients with 63 cases had been described in the literature including our own [7–53] (Table 1). All the cases are exhibited by case reports; thus, it is difficult to make epidemiology statistics. According to previous studies listed in Table 1, the incidence of ectopic recurrence craniopharyngioma has been 0 ~ 4.7% and accounts for 7 ~ 20% of all recurrences approximately. As craniopharyngioma has a bimodal age distribution, with peak incidence rates observed in children aged 5–14 years and adult aged 50–74 years [54], the incidence of ectopic recurrence between children group and adult group has no significant difference based on our statistic. The onset age in children group and adult group ranges from 2–14 years old (6.70 ± 3.33) to 17–73 years old (40.63 ± 15.58), while the interval year between tumor initiation and ectopic recurrence ranges from 0.17–20 (7.28 ± 6.76) years to 0.3–34 (6.85 ± 7.29), respectively. There is no significant gender difference on ectopic recurrence. By reviewing the treatment history, achieving gross total resection seems not to prevent the ectopic recurrence during first operation. What’s more, 16 patients who received postoperative adjuvant radiotherapy still suffer from the ectopic recurrence. There is no accurate data about the long-term prognosis of ectopic recurrence due to the scarcity of clinical cases. According to current data, no recurrence was observed at a longest follow-up duration of 12 years [26]. But one patient died due to local recurrence in sellar region [35].
The diameter of ectopic recurrence tumor ranges from 0.5 to 6.5 (3.14 ± 1.73) cm. The pathological results of ectopic recurrence craniopharyngioma demonstrate that the adamantinomatous type constituted the majority with the number of 36, while the papillary type accounted for only 4 cases and 20 cases’ pathology was unclear. The Ki-67 index of ectopic tumor does not show a remarkable increasement than that of initial tumor. The most common site of ectopic recurrence is frontal lobe, followed by cerebellopontine angle (CPA), temporal lobe, parietal lobe, and others. Currently, there are two views on the mechanism about ectopic recurrence, along the surgical approach and the CSF pathway. Transcranial surgery for craniopharyngioma via pterion is the most frequently used approach that can achieve sufficient surgical field and better protection of nerves and vessels. But it is believed that the tumor cells would disseminate or seed during the operation, and that is the reason why frontal lobe was the most common site of ectopic recurrence, so did the recurrence in Sylvian fissure. The ectopic recurrence mechanism of case 1 in our study belonged to this type. Ectopic recurrence in CPA, temporal and parietal lobe, and lumber space, which far from the surgical route, were considered as the dissemination of tumor cells via CSF pathway. That is the mechanism of case 2; the recurrence site in temporal lobe was far away from the primary surgical area. After statistical analysis, 35 ectopic recurrence cases were due to the seeding along the surgical approach, and 28 cases were due to the seeding via the CSF pathway.
Ectopic recurrence craniopharyngioma is rare, but it can lead to serious symptoms according the location such as hearing loss, disequilibrium, epilepsy, behavioral, and personality change. Thus, some delicate surgical procedure such as strictly separating the tumor by cottonoids, carefully aspirating the cystic fluid to avoid the contamination of CSF, and adequate irrigation in surgical field can help to reduce the risk of ectopic recurrence, and standardized follow-up can provide valuable information for treatment.
Availability of data and materials
Not applicable.
References
Jane JA Jr, Laws ER. Craniopharyngioma Pituitary. 2006;9(4):323–6.
Olsson DS, Andersson E, Bryngelsson IL, Nilsson AG, Johannsson G. Excess mortality and morbidity in patients with craniopharyngioma, especially in patients with childhood onset: a population-based study in Sweden. J Clin Endocrinol Metab. 2015;100(2):467–74.
Zacharia BE, Bruce SS, Goldstein H, Malone HR, Neugut AI, Bruce JN. Incidence, treatment and survival of patients with craniopharyngioma in the surveillance, epidemiology and end results program. Neuro Oncol. 2012;14(8):1070–8.
Bunin GR, Surawicz TS, Witman PA, Preston-Martin S, Davis F, Bruner JM. The descriptive epidemiology of craniopharyngioma. J Neurosurg. 1998;89(4):547–51.
Muller HL, Merchant TE, Warmuth-Metz M, Martinez-Barbera JP, Puget S. Craniopharyngioma Nat Rev Dis Primers. 2019;5(1):75.
Pascual JM, Carrasco R, Prieto R, Gonzalez-Llanos F, Alvarez F, Roda JM. Craniopharyngioma classification. J Neurosurg. 2008;109(6):1180–2. author reply 1182-3.
Cai M, He H, Zhang B, et al. An ectopic recurrent craniopharyngioma of the temporal lobe: case report and review of the literature. World Neurosurg. 2019;126:216–22.
Renfrow JJ, Greeneway GP, Carter L, Couture DE. Intraventricular recurrence of a craniopharyngioma: case report. J Neurosurg Pediatr. 2018;22(4):393–6.
Mahdi MA, Krauss JK, Nakamura M, Brandis A, Hong B. Early ectopic recurrence of craniopharyngioma in the cerebellopontine angle. Turk Neurosurg. 2018;28(2):313–6.
Jian XD, Shrestha D, Zhuang Z. Craniopharyngioma: a case report of ectopic recurrence. Turk Neurosurg. 2017;27(1):160–2.
Carleton-Bland N, Kilday JP, Pathmanaban ON, Stivaros S, Kelsey A, Kamaly-Asl ID. Ventricular metastatic dissemination of a paediatric craniopharyngioma: case report and literature review. Br J Neurosurg. 2017;31(4):474–7.
Du C, Feng CY, Yuan J, Yuan X. Ectopic recurrence of pediatric craniopharyngiomas after gross total resection: a report of two cases and a review of the literature. Childs Nerv Syst. 2016;32(8):1523–9.
Clark SW, Kenning TJ, Evans JJ. Recurrent ectopic craniopharyngioma in the sylvian fissure thirty years after resection through a pterional approach: a case report and review of the literature. Nagoya J Med Sci. 2015;77(1–2):297–306.
Yang Y, Shrestha D, Shi XE, Zhou Z, Qi X, Qian H. Ectopic recurrence of craniopharyngioma: Reporting three new cases. Br J Neurosurg. 2015;29(2):295–7.
Goncalves CB, Lima GA, Nogueira J, do Souto AA, Chimelli L, Taboada GF. Subgaleal recurrence of craniopharyngioma of rapid growing pattern. Pituitary. 2014;17(3):214–9.
Jakobs M, Orakcioglu B. Ectopic recurrent craniopharyngioma of the frontal bone. J Neurosurg. 2012;117(3):490–7.
Elfving M, Lundgren J, Englund E, Stromblad LG, Erfurth EM. Ectopic recurrence of a craniopharyngioma in a 15-year-old girl 9 years after surgery and conventional radiotherapy: case report. Childs Nerv Syst. 2011;27(5):845–51.
Salunke P, Bhardwaj LK, Gupta K, Das K. Ectopic recurrence of craniopharyngioma along the surgical tract. Neurol India. 2011;59(1):137–9.
de Blank PM, Minturn JE. A rare case of ectopic recurrence of a craniopharyngioma diagnosed 17 years after initial presentation. J Pediatr Hematol Oncol. 2011;33(5):392–7.
Kordes U, Flitsch J, Hagel C, et al. Ectopic craniopharyngioma. Klin Padiatr. 2011;223(3):176–7.
Wang XY, Xu SJ, Li XG. Post-operative implantation metastasis of craniopharyngioma: a case report. J Int Med Res. 2010;38(5):1876–82.
Lermen O, Frank S, Hassler W. Postoperative spinal recurrence of craniopharyngioma. Acta Neurochir (Wien). 2010;152(2):309–11 . discussion 311.
Schmalisch K, Beschorner R, Psaras T, Honegger J. Postoperative intracranial seeding of craniopharyngiomas–report of three cases and review of the literature. Acta Neurochir (Wien). 2010;152(2):313–9 . discussion 319.
Romani R, Niemela M, Celik O, Isarakul P, Paetau A, Hernesniemi J. Ectopic recurrence of craniopharyngioma along the surgical route: case report and literature review. Acta Neurochir (Wien). 2010;152(2):297–302 . discussion 302.
Frangou EM, Tynan JR, Robinson CA, Ogieglo LM, Vitali AM. Metastatic craniopharyngioma: case report and literature review. Childs Nerv Syst. 2009;25(9):1143–7.
Elliott RE, Moshel YA, Wisoff JH. Surgical treatment of ectopic recurrence of craniopharyngioma. Report of 4 cases. J Neurosurg Pediatr. 2009;4(2):105–12.
Bikmaz K, Guerrero CA, Dammers R, Krisht AF, Husain MM. Ectopic recurrence of craniopharyngiomas: case report. Neurosurgery. 2009;64(2):E382-3 . discussion E383.
Novak Z, Chrastina J, Feitova V, Lzicarova E, Riha I. Minimally invasive treatment of posterior fossa craniopharyngioma by means of navigated endoscopy. Minim Invasive Neurosurg. 2008;51(3):165–8.
Jeong IH, Lee JK, Moon KS, et al. Ectopic recurrence of craniopharyngioma: a case report and review of the literature. J Neurooncol. 2006;79(2):191–5.
Yamada Y, Haraoka J, Akimoto J. Ectopic recurrence of craniopharyngioma. Neurol Med Chir (Tokyo). 2006;46(12):598–600.
Bianco Ade M, Madeira LV, Rosemberg S, Shibata MK. Cortical seeding of a craniopharyngioma after craniotomy: case report. Surg Neurol. 2006;66(4):437–40 . discussion 440.
Kawaguchi T, Fujimura M, Shirane R, Shoji T, Watanabe M, Tominaga T. Ectopic recurrence of craniopharyngioma. J Clin Neurosci. 2005;12(3):307–9.
Ishii K, Sugita K, Kobayashi H, et al. Intracranial ectopic recurrence of craniopharyngioma after Ommaya reservoir implantation. Pediatr Neurosurg. 2004;40(5):230–3.
Liu JM, Garonzik IM, Eberhart CG, Sampath P, Brem H. Ectopic recurrence of craniopharyngioma after an interhemispheric transcallosal approach: case report. Neurosurgery. 2002;50(3):639–44 . discussion 644-5.
Nomura H, Kurimoto M, Nagai S, et al. Multiple intracranial seeding of craniopharyngioma after repeated surgery–case report. Neurol Med Chir (Tokyo). 2002;42(6):268–71.
Fuentes S, Metellus P, Dufour H, Do L, Grisoli F. Postoperative intracranial seeding of craniopharyngioma Three case reports and a review of the literature. Neurochirurgie. 2002;48(4):345–50 . Dissemination postoperatoire des craniopharyngiomes.
Elmaci L, Kurtkaya-Yapicier O, Ekinci G, et al. Metastatic papillary craniopharyngioma: case study and study of tumor angiogenesis. Neuro Oncol. 2002;4(2):123–8.
Novegno F, Di Rocco F, Colosimo C Jr, Lauriola L, Caldarelli M. Ectopic recurrences of craniopharyngioma. Childs Nerv Syst. 2002;18(9–10):468–73.
Lee DK, Jung HW, Kim DG, Paek SH, Gwak HS, Choe G. Postoperative spinal seeding of craniopharyngioma. Case report J Neurosurg. 2001;94(4):617–20.
Ito M, Jamshidi J, Yamanaka K. Does craniopharyngioma metastasize? Case report and review of the literature. Neurosurgery. 2001;48(4):933–5 . discussion 935-6.
Freitag SK, Miller NR, Brem H. Recurrent ectopic craniopharyngioma. Br J Neurosurg. 2001;15(6):511–3.
Kim SK, Wang KC, Shin SH, Choe G, Chi JG, Cho BK. Radical excision of pediatric craniopharyngioma: recurrence pattern and prognostic factors. Childs Nerv Syst. 2001;17(9):531–6 . discussion 537.
Gupta K, Kuhn MJ, Shevlin DW, Wacaser LE. Metastatic craniopharyngioma. AJNR Am J Neuroradiol. 1999;20(6):1059–60.
Lee JH, Kim CY, Kim DG, Jung HW. Postoperative ectopic seeding of craniopharyngioma. Case illustration J Neurosurg. 1999;90(4):796.
Israel ZH, Pomeranz S. Intracranial craniopharyngioma seeding following radical resection. Pediatr Neurosurg. 1995;22(4):210–3.
Keohane C, Hally M, Ryder DQ, Buckley TF. Late recurrence of craniopharyngioma in the cerebellopontine angle in a fertile woman. J Neurol Neurosurg Psychiatry. 1994;57(7):873–4.
Tomita T, McLone DG. Radical resections of childhood craniopharyngiomas. Pediatr Neurosurg. 1993;19(1):6–14.
Malik JM, Cosgrove GR, VandenBerg SR. Remote recurrence of craniopharyngioma in the epidural space. Case report J Neurosurg. 1992;77(5):804–7.
Tomita S, Mendoza ND, Symon L. Recurrent craniopharyngioma in the posterior fossa. Br J Neurosurg. 1992;6(6):587–90.
Gokalp HZ, Egemen N, Ildan F, Bacaci K. Craniopharyngioma of the posterior fossa. Neurosurgery. 1991;29(3):446–8.
Ragoowansi AT, Piepgras DG. Postoperative ectopic craniopharyngioma. Case report J Neurosurg. 1991;74(4):653–5.
Barloon TJ, Yuh WT, Sato Y, Sickels WJ. Frontal lobe implantation of craniopharyngioma by repeated needle aspirations. AJNR Am J Neuroradiol. 1988;9(2):406–7.
Baba M, Iwayama S, Jimbo M, Kitamura K. Cystic craniopharyngioma extending down into the upper cervical spinal canal (author’s transl). No Shinkei Geka. 1978;6(7):687–93.
Karavitaki N, Cudlip S, Adams CB, Wass JA. Craniopharyngiomas. Endocr Rev. 2006;27(4):371–97.
Acknowledgements
Not applicable
Funding
This study was supported by the Clinical Research Plan of SHDC (SHDC2020CR2004A) and the National Project in Promoting the Diagnosis and Treatment of Major Diseases by MDT.
Author information
Authors and Affiliations
Contributions
CJ did the analysis and wrote the first draft of the manuscript. ZY, XZ, and YZ designed the study and revised the draft. HC did the pathological analysis. XC and NQ provided neurosurgical consultation of the study. CS and YZ collected the data. The final version was approved by all listed authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All the clinical materials were obtained with the written consent from all patients.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ji, C., Cheng, H., Zhou, X. et al. Ectopic recurrence craniopharyngioma: series report and literature review. Chin Neurosurg Jl 9, 13 (2023). https://doi.org/10.1186/s41016-023-00326-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41016-023-00326-3