Abstract
Background
To explore central nervous system (CNS) involvement in this disease, from the perspectives of diagnosis, treatment, and misdiagnosis
Methods
Twenty-eight patients with CNS echinococcosis were included in this retrospective study, including 18 males (64.3%) and 10 (35.7%) females. The average age of all the patients were 23.5 years (ranged 4–60 years). Twenty-three (23) patients (82.1%) received the first surgical resection in our hospital. Five (5) patients (17.9%) gave up surgical treatment for multiple-organ hydatidosis and previous surgery history at other hospitals, and albendazole was applied for a long-term (3–6 months) adjunct therapy for the 5 patients. The average follow-up time was 8 years.
Results
For the 28 patients, 23 cases received surgical treatments, and the diagnosis was confirmed by pathological examinations. The diagnosis of 4 cases of brain echinococcosis and 2 cases of spinal cord echinococcosis could not be confirmed, resulting in a misdiagnosis rate of 21.4% (6/28). For the pathological examination, a total of 17 cases were infected with Echinococcus granulosus (including 2 cases of spinal cord echinococcosis), and 6 cases were infected with Echinococcus alveolaris.
Conclusion
The diagnosis should be specifically considered in endemic regions. The clinical features of CNS hydatidosis were intracranial space-occupying lesions. For the treatment, the surgical removal of cysts should be necessary. In addition, the adjuvant therapy with drug and intraoperative prophylaxis is also suggested. The misdiagnosis may have resulted from atypical clinical features and radiographic manifestations, as well as the accuracy of hydatid immunologic test.
Similar content being viewed by others
Background
Echinococcosis is a zoonosis with global prevalence, which is caused by the larval stage of the Echinococcus tapeworm. There are mainly two types of hydatid disease, caused by Echinococcus granulosus and Echinococcus alveolaris. Echinococcus alveolaris-caused echinococcosis is less common but more invasive compared to Echinococcus granulosus, presented features like malignancy. Echinococcosis is prevalent in the developing countries, and it is generally observed in the great grazing regions in the world, such as Australia, New Zealand, Mongolia, Japan, and Indonesia. Echinococcosis is also prevalent in China, especially in western regions without adequate sanitation, such as Xinjiang, Ningxia, Inner Mongolia, and Qinghai.
The diagnosis and treatment of echinococcosis have been a significant issue that attracted attentions from both physicians and researchers. Echinococcosis can infect multiple organs of humans, resulting in complications during the long course of diseases. Here, a retrospective study was performed on 28 cases of CNS echinococcosis treated in our hospital during January 2000 and May 2019. These patients were analyzed from the perspectives of diagnosis, treatment, and misdiagnosis reasons. The results were further discussed with literature.
Methods
Demographic data
A total of 28 patients were admitted in our hospital for echinococcosis, including 26 cases of brain echinococcosis and 2 cases of spinal cord echinococcosis. There were 18 (18/28, 64.3%) males and 10 (10/28, 35.7%) females. The average age was 23.5 years, ranging from 4 to 60 years. The average course of disease before hospitalization was 6 months, ranging from 1 month to 3 years. For the ethnicity, there were 12 cases of Han, 5 cases of Kazak, 4 cases of Mongolian, 4 cases of Uygur, 2 cases of Tibetan, and 1 case of Hui. Liver and lung infection of hydatid cysts was concomitantly observed in 10 patients; 5 cases received the treatment of surgery in other hospital and then presented with relapse and metastasis (Table 1).
Clinical manifestations
For the clinical features, there were 21 cases of headache, 14 cases of nausea and vomiting, 7 cases of consciousness disturbance, 17 cases of papillary edema, 6 cases of vision loss, 4 cases of diplopia, 9 cases of visual field defects, 5 cases of limb paresthesia, and 7 cases of muscle weakness. Cerebral hernia was observed in 2 patients, stiff neck was observed in 3 patients, epilepsy was observed in 5 patients, and unilateral paralysis was observed in 2 patients. Pathological signs were positive in 14 patients, nystagmus was observed in 4 patients, and ataxia was observed in 4 patients.
Imaging examination
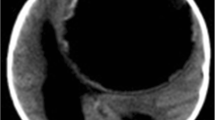
Supratentorial and subtentorial hydatidosis was observed in 22 and 4 patients, respectively. Spinal cord hydatidosis was observed in 2 patients. For the intracranial hydatidosis, multiple lesions were found in 14 patients, and single lesion was observed in 12 patients (2 cases of frontal, 3 cases of parietal lobe, 3 cases of temporal lobe, 1 case of lateral ventricle, and 3 cases of cerebellum). The diameter of hydatid cyst was from 13 to 85 mm. Computed tomography (CT) and magnetic resonance imaging (MRI) were performed for all the 28 patients (Figs. 1a–d and Fig. 2a–d).
Brain Echinococcus granulosus. a CT scan revealing a solitary cystic lesion located in the right frontotemporal lobe. The margins are well delineated. The intralesional fluid displays the same attenuation value as that of CSF. There is no obviously perilesional edema. b CT scan shows multiple cystic lesions in frontoparietal lobe, with the same density as CSF. c MRI T1-weighted images shows a homogeneous, thin-walled cystic lesion (yellow arrows). There is significant mass effect on the lateral ventricular system. Midline shift is 2 cm. Cyst signal is isointense relative to CSF. d MRI shows a cystic lesion hyperintense on T2-weighted images (similar to CSF) with a hypointense halo around the cyst capsule (yellow arrow). e Dowling’s technique. f Photomicrography (HE, original magnification, ×400) shows Echinococcus granulosus infection of the brain
Brain Echinococcus alveolaris. a CT scan shows a mixed density solid lesion located in the right temporal lobe. There is slight perilesional edema. b MRI T1W axial MR image shows multiple equal T1 signal intensity lesion located in frontoparietal lobe. There is obviously perilesional edema. c MRI T2W axial MR image shows a short T2 signal intensity multiple lesions with obviously perilesional edema located in the same place. d Contrast-enhanced MR image shows obvious enhancement of the lesion wall (yellow arrows). e Photomicrography (HE, original magnification, ×400) shows Echinococcus alveolaris infection of the brain
Laboratory tests
Hydatid immunologic test was performed for all the patients. During 2000–2005, 10 cases were tested with routine 3-item hydatid immunologic test (Casoni’s method, indirect blood coagulation method, counter immune electrophoresis), and during 2006–2019, 18 cases were tested with 8-item immunodiagnostic kit, namely, immunogold filtration assay and enzyme-linked immunosorbent assay (ELISA) for testing four hydatid antigens, including capsule liquid antigen (EgCF), head quarter antigen (EgP), sac liquid half purification antigen (EgB), and alveolar hydatid cyst antigen (Em2).
Treatment
Twenty-three patients (23/28, 82.1%) received surgery. The surgical plans (including surgical approaches, bone choice, and dural window) were designed according to the sites and size of the lesions, as well as the maximum diameter of the cyst. Dowling’s technique was applied in 17 patients to remove the cyst wall from the surrounding brain parenchyma with irrigation (Fig. 1e). The hydatid with surrounding edema was completely excised in 6 patients. Five (5/28, 17.9%) patients gave up surgery due to multiple-organ hydatidosis and history of previous surgery at other hospitals, and then, they received a long-term adjunct therapy of albendazole, with the dose of 15 mg/kg/d PO divided bid for 3 to 6 months.
Results
Preoperatively, 22 cases were diagnosed as brain echinococcosis based on the combination of clinical manifestations, hydatid immunologic test, and imaging examination. Six cases were not diagnosed as echinococcosis, including 2 cases of spinal cord echinococcosis and 4 cases of brain echinococcosis, with a misdiagnosis rate of 21.4% (6/28). For the single hydatid immunologic test, 10 cases received routine 3-item hydatid immunologic test during 2000–2005, and there were 7 positive cases, with a positive rate of 70.0%; 18 cases received hydatid 8-test immunodiagnosis during 2006–2019, and there were 15 positive cases, with a positive rate of 83.3%.
Twenty-three patients (23/28, 82.1%) received surgical resection. Postoperatively, the pathological examinations showed 17 cases of Echinococcus granulosus (Fig. 1f) (including 2 cases of spinal cord echinococcosis) and 6 cases of alveolar Echinococcus (Fig. 2e). Another 5 patients (5/28, 17.9%) gave up surgical treatment and received a long-term drug therapy of albendazole (3–6 months).
The average follow-up period was 8 years, ranging from 3 months to 11 years. For the 17 patients who received Dowling’s technique to dissect the cyst, no postoperative recurrence was reported. Four patients experienced relapse and another operation within 6 months to 1 year. Two patients died of intracranial infection and cachexia. For the 5 patients who received drug therapy, 4 patients suddenly died of cerebral hernia within 3–4 years. One patient is still alive.
Discussion
Hydatid disease has been widely prevalent in the developing countries, and it is both a medical and economic issue. Echinococcosis was generally rare in developed countries; however, it has still been a significant public health issue in endemic areas [1–3]. The prevalence of echinococcosis is also observed in western China. Echinococcosis is one of the most common zoonosis, which equally infects both genders. The younger populations were subjected to more serious infections [4]. The definite hosts of Echinococcus are a variety of carnivores, and dogs are the most common host. Sheep, cattle, and human beings can act as the intermediate host.
The transmission routes of echinococcosis are through contacting with definite host or consuming contaminated water or food. During the infection, the eggs of Echinococcus lose their enveloping layer in the stomach, and the embryos would be released. The embryos pass through the wall of the gut into the portal system, being transferred to the liver. Most larvae would be entrapped end encysted in the liver. Some larvae may occasionally reach the lungs, and some may enter the systemic circulation after passing through the capillary filter of the liver and lungs. Some of these larvae may reach the brain or spinal cord. Brain echinococcosis are often accompanied with liver and lung infections. In our study, 16 of the 28 patients showed hydatid cysts in other organs. For the cerebral hydatid cysts, most cases were supratentorial, while only a few were infratentorial lesions [5]. Brain hydatid can be rarely located in some special place, such as thalamus or ventricle [6, 7]. Intracranial hydatid cysts were generally solitary, while multiple cysts were rare [8, 9]. Intracranial hydatid cyst may also be classified as primary or secondary infection. The primary cysts resulted from direct infestation of the larvae in the brain, without significant involvement of other organs. The secondary multiple cysts resulted from spontaneous, traumatic, or surgical rupture of the primary intracranial hydatid cyst, which may lack brood capsule and scolices. In our study, the primary cyst was observed in 11 cases, and the secondary multiple cysts were found in 10 cases.
Hydatid disease of the spinal cord has been rare. The first case of spinal cord echinococcosis was reported in 1964, in Xinjiang. Notably, approximately 50% of the patients were under 30 years old [10–15]. Braithwaite and Lees [16] have classified this disease into 5 types: (1) primary intramedullary hydatid cyst, (2) intradural extramedullary hydatid cyst, (3) extradural intraspinal hydatid cyst, (4) hydatid disease of the vertebra, and (5) paraspinal hydatid disease. Based on this classification, the 2 cases of spinal cord echinococcosis in our study were classified as type 3, the extradural intraspinal hydatid cyst.
The clinical manifestations of echinococcosis are similar to those of increased intracranial pressure due to other causes. The early diagnosis of echinococcosis was difficult for those patients without apparently increased intracranial pressure [17]. Therefore, a detailed medical history record would be especially important, and it should be combined with an auxiliary examination. Attention should be paid for the following situations: (1) the patient comes from epidemic area, being exposed to patients in these regions, or reporting contact with cattle and pet; (2) the patients can be asymptomatic or show elevated intracranial pressure, epilepsy, and nervous system local functional defect; (3) imaging examinations may reveal characteristic findings of brain hydatid cysts, especially head CT and MRI [18–21]; (4) the diagnosis may be supported by positive hydatid immunological test, but cannot be excluded by negative result; (5) the exclusion of intracranial space-occupying lesions due to other causes is important; the diagnosis of intracranial cystic brain echinococcosis should be differentiated from intracranial arachnoid cysts, brain-perforating deformity, and brain abscesses. The MRI result can be enhanced for intracranial bubbly brain echinococcosis, which can be distinguished from intracranial strengthened TB tumor, glioma, brain metastases, and brain cysticercosis. In addition, spinal cord echinococcosis should be differentiated from spinal cord and arachnoid cyst, as well as hydatid vascular malformation, such as spinal cord bleeding.
The diagnosis of echinococcosis should be comprehensively made based on patient information, clinical features, imaging results, and laboratory data. The clinical features may not be obvious. The imaging results could be atypical and similar to those of other intracranial space-occupying lesions; the differential diagnosis would be difficult. The radiologists from non-epidemic area may lack experience in recognizing the characteristic echinococcosis images. The diagnosis may be missed without adequate information and laboratory data. Therefore, the good communication between radiologists and clinician is necessary. Even so, there were still false-positive results [22], and such misdiagnosis may result from cyst wall thickness, deep location, and small number of cysts. Misdiagnosis of parasites may also be observed in organs with physical barriers, like the brain. The laboratory data may be affected in immunodeficiency and immunocompromised populations, including children, people undergoing chemotherapy, patients with tumor cachexia, and AIDS patients, which may also lead to misdiagnosis.
Until now, echinococcosis could still not be cured with any drug. The early diagnosis and timely treatment are critical for controlling brain echinococcosis. The preferred therapy is surgery. The preoperative plan is important for the complete removal of hydatid lesions, such as accurate localization, proper surgical approach, and adequate bone window. The critical point for the treatment of Echinococcus granulosus was the removal of unruptured cyst. Once the cysts ruptured and entered the subarachnoid space, there would be widespread dissemination of scolices, leading to severe inflammation and anaphylactic reactions caused by the fluids containing numerous antigens. Dowling-Orlando’s technique has been widely applied in the removal of intraparenchymal cysts [23]. The cyst would be exposed by a wide incision, and saline irrigation was performed with a rubber catheter from an inclined position of the head. In our study, Dowling’s technique was conducted in 17 cases, and the cyst wall was removed from the surrounding brain parenchyma with irrigation. The cysts could be completely excised, and the prognosis was good. As an adjunct for therapy, albendazole was given to treat patients with multiple-organ involvement or gave up surgical treatment. The dose was 15 mg/kg/d PO divided into twice daily for 3–6 months.
Conclusions
Echinococcosis can infect multiple organs of humans. The diagnosis should be specifically considered in endemic regions. The clinical features of CNS hydatidosis were intracranial space-occupying lesions. For the treatment, the surgical removal of cysts should be necessary. In addition, the adjuvant therapy with drug and intraoperative prophylaxis are also suggested. The misdiagnosis may have resulted from atypical clinical features and radiographic manifestations, as well as the accuracy of hydatid immunologic test.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Altinors N, Bavbek M, Caner H, Erdogan B. Central nervous system hydatidosis in Turkey: a cooperative study and literature survey analysis of 458 cases. J Neurosurg. 2000;93(1):1–8. https://doi.org/10.3171/jns.2000.93.1.0001.
Lunardi P, Missori P, Di Lorenzo N, Fortuna A. Cerebral hydatidosis in childhood: a retrospective survey with emphasis on long-term follow-up. Neurosurgery. 1991;29(4):515–8. https://doi.org/10.1227/00006123-199110000-00005.
Nurchi G, Floris F, Montaldo C, Mastio F, Peltz T, Coraddu M. Multiple cerebral hydatid disease: case report with magnetic resonance imaging study. Neurosurgery. 1992;30(3):436–8. https://doi.org/10.1227/00006123-199203000-00023.
Khaldi M, Mohamed S, Kallel J, Khouja N. Brain hydatidosis: report on 117 cases. Child’s Nervous System. 2000;16(10-11):765–9. https://doi.org/10.1007/s003810000348.
Akdemir G, Dağlıoğlu E, Seçer M, Ergüngör F. Hydatid cysts of the internal acoustic canal and jugular foramen. J Clin Neuroscience. 2007;14:394–6.
Ersahin Y, Mutluer S, Dermirtas E. Taşkin Yurtseven: A case of thalamic hydatid cyst. Clin Neurol Neurosurg. 1995;97(4):321–3. https://doi.org/10.1016/0303-8467(95)00052-L.
Huang SP, Wang P, Luan XP, et al. The diagnosis of brain hydatid immune. Xinjiang Med J. 1993;16:182–3.
Ciurea AV, Fountas KN, Coman TC, Machinis TG, Kapsalaki EZ, Fezoulidis NI, et al. Long-term surgical outcome in patients with intracranial hydatid cyst. Acta Neurochir (Wien). 2006;148(4):421–6. https://doi.org/10.1007/s00701-005-0679-z.
Onal C, Erguvan-Onal R, Yakinci C, Karayol A, Atambay M, Daldal N. Can the requirement of a diversion procedure be predicted after an uncomplicated intracranial hydatid cyst surgery? Pediatr Neurosurg. 2006;42(6):383–6. https://doi.org/10.1159/000095570.
Karry S, Zlitni M, Fowles JV, et al. Vertebral hydatidosis and paraplegia. J Bone Joint Surg (Br). 1990;72:83–6.
Medjek L, Zenini S, Hammoum S, Martani S. Hydatidose intradurale rachidienne dorsale Apropos d’un cas. Annales de Radiologie. 1991;34(4):251–5.
Porat S, Robin GC, Wertheim G. Hydatid disease of the spine causing paraplegia. The combined treatment by surgical drainage and mebendazole: a case report. Spine. 1984;9(6):648–53. https://doi.org/10.1097/00007632-198409000-00018.
Tekkok HI, Benli K. Primary spinal extradural hydatid disease: report of a case with magnetic resonance characteristics and pathological correlation. Neurosurg. 1993;33(2):320–3. https://doi.org/10.1097/00006123-199308000-00023.
Wani MA, Taheri SA, Babu ML, Ahangar GA, Wani H. Primary spinal extradural hydatid cyst. Neurosurg. 1989;24(4):631–2. https://doi.org/10.1227/00006123-198904000-00026.
Xu MQ: Echinococcosis. Urumqi, Xinjiang People’s Publishing House 56-61, 1983
Braithwaite PA, Lees RF. Vertebral hydatid disease. Radiological assessment. Radiology. 1981;140:763–6.
Song JR, Hu GQ, Xia YC. Brain echinococcosis diagnosis and surgical treatment. Chin J Neurosurg. 1994;10:291.
Bükte Y, Kemaloglu S, Nazaroglu H, Ozkan U, Ceviz A, Simsek M. Cerebral hydatid disease: CT and MR imaging findings. Swiss Med Wkly. 2004;134(31-32):459–67 DOI: 2004/31/smw-10711.
Liu G. Brain CT imaging diagnosis of the echinococcosis. Chin Clin Med Imaging Magazine. 2008;19:359–60.
Zhang Q, Xian CM. Brain echinococcosis 12 cases of surgical report. Chin J Neurosurg. 2006;22:60.
Li ZY, Zhao ZX, Zhou J, et al. Brain echinococcus alveolaris three cases of report and literature review. Chin J Neurosurg. 2008;24:859–61.
Chen XH, Wen H, Zhang ZX, et al. Echinococcosis immune misdiagnostic reasons of analysis. Chin J Parasitology and Parasitic Diseases. 2002;20:121–2.
Altas M, Serarslan Y, Davran R, Evirgen O, Aras M, Yilmaz N. The Dowling-Orlando technique in a giant primary cerebral hydatid cyst: a case report. Neurol Neurochir Pol. 2010;44(3):304–7. https://doi.org/10.1016/S0028-3843(14)60046-3.
Acknowledgements
Not applicable.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
GD designed the study and wrote the paper. DG, PW, and XW managed the literature searches and analyses. RS, YL, and YF wrote the first draft of the manuscript. All authors contributed to and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All experimental procedures in the current study were approved by the Ethics Committee of the First Affiliated Hospital of Xinjiang Medical University (Xinjiang, China).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Du, G., Li, Y., Wu, P. et al. Diagnosis, treatment, and misdiagnosis analysis of 28 cases of central nervous system echinococcosis. Chin Neurosurg Jl 7, 30 (2021). https://doi.org/10.1186/s41016-021-00248-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41016-021-00248-y