Abstract
Background
We aim to present an unique case of inflammatory myofibroblastic tumor (IMT) of the brain parenchyma and study the clinical presentation, imagine characteristic, intraoperative findings, and histopathology features of IMT in the brain parenchyma.
Case Presentation
A 36-year-old female with IMT come to see doctor presented with a 3-month history of progressively worsening weakness in the left upper limb along with alalia. Serial magnetic resonance imaging studies revealed a lesion within the right frontal lobe. The lesions were locally clear boundary with peripheral tissues. A right frontotemporal craniotomy was performed and the specimens were detected by immunohistochemical staining and light microscopy. Through the microscope, the tumor was composed of large number of chronic inflammatory cells and spindle cells. From immunohistochemical stains, it demonstrated CD34 (+), SMA (+), Vimentin (+), and actin (+) were positive meanwhile S-100(-) was negative.
Conclusion
IMT of the right frontal lobe is a rare lesions. Surgical resection is the best and the most effective treatment.
Similar content being viewed by others
Background
Inflammatory myofibroblastic tumor (IMT) is a disease characterized by tumorous lesions formed by inflammatory cells and myofibroblastic spindle cells that occur primarily in the viscera and soft tissues of children and young adults [1]. IMT is most commonly seen in the lungs, omentum and mesentery. IMT of the brain is rare. We herein present a case of IMT located in the frontal lobe.
Case presentation
Clinical data
Patient data
A 36-year-old man was admitted in December 2013 with progressively worsening weakness in the left upper limb along with alalia. Two months before admission, she had undergone a history of mild head injury. Physical examination is in good condition.
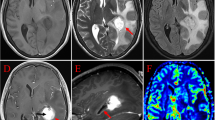
CT of the brain showed (Fig. 1a): a lesion located in the right frontal lobe, slightly more mixed density, size 3 cm, peripheral edema; T1 and T2-weighted Magnetic resonance imaging (MRI) showed: a low or iso-intensity area at the same site in T1-weighted MRI (Fig. 1c), a high and low mixed signal at the same site in T2-weighted MRI (Fig. 1d–f), with homogeneous enhancement by Gd-DTPA (Fig. 1g–i); MRS (Fig. 1b) showed no peak of Cho and NAA.
A 36-year-old man was admitted in December 2013 and diagnosed as IMT after surgery. a CT of the brain showed a mass located in the right frontal lobe, slightly more mixed density, size 3 cm, peripheral edema; b MRS showed no peak of Cho and NAA; c T1-weighted Magnetic resonance imaging (MRI) showed a low or iso-intensity area at the same site; d-f T2-weighted Magnetic resonance imaging (MRI) showed a high and low mixed signal at the same site; g-i MR image showing an homogeneous enhancement by gadolinium diethylenetriaminepenta-acetic acid (Gd DTPA) in the right frontal lobe
A right frontotemporal craniotomy was performed. The tumor located in a right frontal lobe with a clear boundary, and partly adhered to the dura. Tumor mass is toughening and had to be block excised.
Pathological examination
Histologically, the tumor specimen predominantly consisted of mature myofibroblast cells, with a large number of inflammatory cells infiltration, and distribution of collagen fibers. Myofibroblast cells are spindle, of red dye cytoplasm and round or oval nuclei. Most of inflammatory cells are plasma cells and lymphocytes, which are in diffused distribution or gather into oven. Spindle tumor cell is rare nuclear division, no obvious heteromorphism which accord with inflammatory myofibroblast cells.
Immunohistochemical analysis: Immunostaining demonstrated that the spindle cells reacted with vimentin and smooth muscle actin. CD34+, vimentin (+), actin (+), SMA+, Ki-67 positive rate < 5%, desmin (+), GFAP-, S-100(-), EMA-, ALK-1-, CD117-.
According to these findings, a histopathological diagnosis of IMT was made.
Result
Postoperative CT: the tumor was total resected, with no residual tumor, and swelling is improving than before. In the one year of follow-up after the patient’s discharge, there has been no any tumor progression or recurrence.
Discussion
Inflammatory myofibroblastic tumor (IMT) is a disease characterized by spindle cell neoplasm composed of lymphocytes, plasma cells, and so on. IMT is rare in clinical, which mainly located in the lungs. IMT has been defined by many different names, including inflammatory pseudotumor (IPT) and plasma cell granuloma, highlighting the complexity and variable histological characteristics of these tumors. Pettinato and colleagues in 1990 first put forward the concept of inflammatory myofibroblastic tumor (IMT) [2]. In the 2002, World Health Organization (WHO) classification of soft tissue tumors, these lesions were renamed [3].
The etiology of these ‘tumors’ is not certain and the current acquaintance of the pathophysiology of this disease is based on an abnormal response by the myofibroblast to trauma, tissue injury, surgery, inflammation and so on. Our patient admitted to hospital with a history of head injury in before two month age, which may be the inducing factors of this disease. Some cases have been associated with tuberculosis or malignancy as satellite lesions, and some suggested to be associated to cocaine consumption [4–6] and even by viral infection such as Epstein–Barr virus [4, 7]. There have been reported IMT in the spleen may be associated with EBV infection [8]. In addition, there are scholars believe that abnormal autoimmune mechanism may be related to the occurrence of a muscle fiber mother cell tumor. Plasma cell granuloma might be responsible for the immunological abnormalities because symptom of plasma cell granuloma was resolved as soon as the tumor was removed [9, 10]. Recent studies have confirmed that the chromosome 2p23 of IMT case is rearrangement, which hints the of the monoclonal hyperplasia characteristics of IMT and supports this lesion as true tumor rather than inflammatory pseudotumor [11, 12]. However, the lack of p53 detection in IMT gone with the low proliferation index (Ki67 < 10%) hints that IMT may be a low-grade tumor, if at all [13].
Making a diagnosis of IMT requires a histopathological examination because the radiological and clinical findings are generally nonspecific [1]. Research suggests electron microscopic observation is special. Under the electron microscope, this tumor cells are of ultra microstructure characteristics of fibroblast and myofibroblast cell, show the bipolar or irregular cellular processes, well-differentiated rough endoplasmic reticulum, and filament bundle of the surrounding cytoplasm, discontinuous base board structures and pinocytosis vesicles surrounding cells. Immunohistochemical can assist the diagnosis to this disease. Spindle cells of IMT is performance for different degrees of positive reaction to the following antibody: vimentin, SMA, MSA (muscle-specific actin). Positive reaction of vimentin is usually very strong, but its specificity is not high, because the vimentin can be found in all normal mesenchymal tissue and most sarcoma. Specificity of SMA is good, whose positive reaction is thought to be important marker to IMT. A small part of IMT is of positive reactions to epithelial membrane antigen, CK, CD68, CD30, α-antitrypsin, α-anticoagulant protease or melting bacteria enzymes, and so on, but no specificity to diagnosis [14]. This case was proved as IMT by immunohistochemical staining with Vim+, SMA+, actin+, desmin (partly cells +).
Steroids have been used to treat unresectable lesions and got some success. Other medical treatment choice, however, are less effective, including radiotherapy and/or adjuvant chemotherapy and treatment with immunosuppressive and anti-inflammatory drugs. Treated with high-dose corticosteroid anti-inflammatory drug, some patients symptoms can subside, but withdrawal symptoms once drug discontinuance. Methotrexate, azathioprine, vinca alkaloids, cyclophosphamide and cyclosporine have been used; however, the response is variable and often poor [15–18]. Fumiko et al. report a successful treatment case of an unresectable inflammatory myofibroblastic tumor of the frontal bone by methotrexate and cyclooxygenase-2 inhibitor [1]. In summary to the existing literature, there is a consensus that total surgical excision is the most effective therapeutic option in cases in which the tumors are surgically accessible.
Our patient received only surgical excision therapy. This patient got a good postoperative outcome with no recurrent signs according to follow-up MR imaging for about one year. However, it must be carefully observed especially for recurrent signs of the tumor.
Conclusion
IMT of the right frontal lobe is a rare lesions. Surgical resection is the best and the most effective treatment.
Abbreviations
- CT:
-
Computed Tomography
- IMT:
-
Inflammatory myofibroblastic tumor
- IPT:
-
Inflammatory pseudotumor
- MRI:
-
Magnetic resonance imaging
References
Kusunoki-Nakamoto F, Matsukawa T, Tanaka M, Miyagawa T, Yamamoto T, Shimizu J, Ikemura M, Shibahara J, Tsuji S. Successful treatment of an unresectable inflammatory myofibroblastic tumor of the frontal bone using a cyclooxygenase-2 inhibitor and methotrexate. Intern Med. 2013;52(5):623–8.
Pettinato G, Manivel JC, De Rosa N, Dehner LP. Inflammatory myofibroblastic tumor (plasma cell granuloma). Clinicopathologic study of 20 cases with immunohistochemical and ultrastructural observations. Am J Clin Pathol. 1990;94(5):538–46.
Jeon YK, Chang KH, Suh YL, Jung HW, Park SH. Inflammatory myofibroblastic tumor of the central nervous system: clinicopathologic analysis of 10 cases. J Neuropathol Exp Neurol. 2005;64(3):254–9.
Boutarbouch M, Arkha Y, Rifi L, Derraz S, El Ouahabi A, El Khamlichi A. Intradural cervical inflammatory pseudotumor mimicking epidural hematoma in a pregnant woman: case report and review of the literature. Surg Neurol. 2008;69(3):302–5.
Hytiroglou P, Brandwein MS, Strauchen JA, Mirante JP, Urken ML, Biller HF. Inflammatory pseudotumor of the parapharyngeal space: case report and review of the literature. Head Neck. 1992;14(3):230–4.
Karatsis P, Wyman A, Sweetland HM, Bull AD, Rogers K. Inflammatory pseudotumour of the liver. Eur J Surg Oncol. 1993;19(4):384–7.
Arber DA, Kamel OW, van de Rijn M, Davis RE, Medeiros LJ, Jaffe ES, Weiss LM. Frequent presence of the Epstein-Barr virus in inflammatory pseudotumor. Hum Pathol. 1995;26(10):1093–8.
Oz Puyan F, Bilgi S, Unlu E, Yalcin O, Altaner S, Demir M, Cakir B. Inflammatory pseudotumor of the spleen with EBV positivity: report of a case. Eur J Haematol. 2004;72(4):285–91.
Coffin CM, Humphrey PA, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor: a clinical and pathological survey. Semin Diagn Pathol. 1998;15(2):85–101.
Figarella-Branger D, Gambarelli D, Perez-Castillo M, Garbe L, Grisoli F. Primary intracerebral plasma cell granuloma: a light, immunocytochemical, and ultrastructural study of one case. Neurosurgery. 1990;27(1):142–7.
Coffin CM, Patel A, Perkins S, Elenitoba-Johnson KS, Perlman E, Griffin CA. ALK1 and p80 expression and chromosomal rearrangements involving 2p23 in inflammatory myofibroblastic tumor. Mod Pathol. 2001;14(6):569–76.
Rabban JT, Zaloudek CJ, Shekitka KM, Tavassoli FA. Inflammatory myofibroblastic tumor of the uterus: a clinicopathologic study of 6 cases emphasizing distinction from aggressive mesenchymal tumors. Am J Surg Pathol. 2005;29(10):1348–55.
Meis-Kindblom JM, Kjellström C, Kindblom LG. Inflammatory fibrosarcoma: update, reappraisal, and perspective on its place in the spectrum of inflammatory myofibroblastic tumors. Semin Diagn Pathol. 1998;15(2):133–43.
Coffin CM, Watterson J, Priest JR, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol. 1995;19(8):859–72.
Dishop MK, Warner BW, Dehner LP, Kriss VM, Greenwood MF, Geil JD, Moscow JA. Successful treatment of inflammatory myofibroblastic tumor with malignant transformation by surgical resection and chemotherapy. J Pediatr Hematol Oncol. 2003;25(2):153–8.
Favini F, Resti AG, Collini P, Casanova M, Meazza C, Trecate G, Ferrari A. Inflammatory myofibroblastic tumor of the conjunctiva: response to chemotherapy with low-dose methotrexate and vinorelbine. Pediatr Blood Cancer. 2010;54(3):483–5.
Sacco O, Gambini C, Gardella C, Tomà P, Rossi UG, Jasonni V, Bush A, Rossi GA. “Atypical steroid response” in a pulmonary inflammatory myofibroblastic tumor. Pediatr Pulmonol. 2010;45(7):721–6.
Trojan A, Stallmach T, Kollias S, Pestalozzi BC. Inflammatory myofibroblastic tumor with CNS involvement. Onkologie. 2001;24(4):368–72.
Acknowledgements
We didn’t receive any financial support to analyze this data and we didn’t have any financial interest in any materials or devices described.
Funding
This research supported by: (1) Young Medical Project of Nantong City Health Bureau (WQ2014016); (2) Traditional Chinese medicine science and technology project in Jiangsu province (No. YB2015113); (3) the science and technology program of Nantong city (no. : MS12015016).
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Authors’ contributions
Conceived and designed: Xuejian Wang, Yang Chen. Performed: Zhifeng Wang, Ming Qian. Analyzed the data: Xuejian Wang. Wrote the paper: Xuejian Wang. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Ethics approval and consent to participate
This research has been approved by the ethics committee of the Second Hospital affiliated to Nantong University(2016002). Informed consent has been obtained and this report was processed according to the principles expressed in the Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wang, X., Wang, Z., Chen, Y. et al. Inflammatory myofibroblastic tumor of the right frontal lobe. Chin Neurosurg Jl 3, 12 (2017). https://doi.org/10.1186/s41016-017-0076-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41016-017-0076-5