Abstract
Background
Common B cell lymphoma locations are lymph nodes, skin, bone, mediastinum and it accounts for 2 % of NHL. Giant solitary spinal B-LBL has not yet been described.
Case presentation
A 15-years old boy was admitted for a painful swelling of the thoracolumbar spine and paraplegia. MRI showed a voluminous mass of the thoracolumbar spine. Initial treatment consisted of surgical decompression and stabilization, followed by chemotherapy and radiotherapy. Histological examination showed a B-LBL. The quality of life improved significantly.
Conclusion
To the best of our knowledge, this is the first case of giant solitary spinal B-LBL ever reported. Indication to choose a treatment method over another should weigh on individual priorities. Surgery should be considered as initial treatment option in this atypical lesion.
Similar content being viewed by others
Background
B cell lymphoblastic lymphoma (B-LBL) is a subtype of non Hodgkin’s (NHL) lymphoma with great tropism for central nervous system. It is an aggressive tumour and accounts for 2 % of all NHL [1]. Lymphoma is the term used when the process is confined as a mass lesion without evidence of blood involvement.
Common locations of B cell lymphoblastic lymphoma are lymph nodes, skin, bone, mediastinum [2] and soft tissues [3]. However, rare and uncommon sites such as gall bladder [4], nasopharynx [5], great omentum [6] and orbit [3] have been reported. As far as we know, giant spinal B-LBL as a primary location has not yet been described.
We report a case of giant spinal primary B-LBL revealed as a spinal cord compression and thoracolumbar mass syndrome. Surgical decompression and stabilization were warranted at the initial stage to improve quality of life. We present this successful management of an atypical giant lesion of this area.
Case presentation
A 15-year-old boy was reviewed by our neurosurgical team for a 9-months history of thoracolumbar back pain and intercostal neuralgia. The pain gradually exacerbated and worsening at night. One month after the onset, he complained of a painful swelling over the lower thoracic spine, rapidly increasing in size. Six months prior to admission, he experienced weakness, paresthesiae, hypoesthesia of lower limbs and urinary difficulties. Physical examination revealed paraplegia, T10 anaesthesia and a voluminous (14 cm × 8 cm), firm and painful mass of the thoracolumbar spine (Fig. 1).
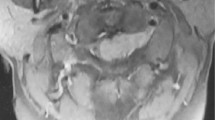
The patient couldn’t lie supine and had to be maintained permanently prone. Magnetic resonance imaging of the spine demonstrated a large hypointense expansive tissue mass on T1 weighted imaging, involving T11, T12, L1, L2 vertebral bodies. T2 weighted imaging showed a high signal change (Fig. 2). An important compression of the spinal cord and a kyphotic deformity of the thoracolumbar spine were also shown on MRI. Since the full body computed tomography scan demonstrated that the disease was limited to the spine, we concluded that the tumour was from a vertebral origin. Full blood count and biochemistry test were normal, as was CSF. A presumptive diagnosis of spinal giant solitary tumour was made. Surgical decompression and stabilization (Fig. 3) were performed to improve comfort and quality of life of the patient. The lesion was firm, encapsulated, richly vascularised and very aggressive for the vertebras. It destroyed completely the posterior arch of T12,T11 and L1 vertebras. There were left and right 11th, 12th ribs partial lysis because of the lateral extension of the tumour. During the resection we noted a cleavage plane between the dura and the tumour allowing exposure of the dura after tumour detachment without laminectomy. There was no dural invasion. Histological analysis concluded to an aggressive B-LBL (Fig. 4). The patient was then referred to our hematology and oncology team. The bone marrow biopsy examination was consistent with the diagnosis of lymphoma with less than 25 % blast in the bone marrow.
He received 4 cycles of hyperfractionned CVAD regimen as follows: cyclophosphamide administrated at the dose of 300 mg/m2 intravenously on days 1 to 3; vincristine administrated at the dose of 2 mg intravenously on days 4 and 11; doxorubicin administrated at the dose of 50 mg/m2 intravenously on day 4 and 40 mg dexamethasone administrated orally and daily on days 1 to 4 and days 11 to 14. This intensive chemotherapy was followed by 30 Gy radiotherapy in 6 fractions. Maintenance chemotherapy was then administrated for 12 months with vincristine 2 mg intravenously every month and prednisone 200 mg daily for 5 days every month orally.
There was no change in his neurological status but his general condition improved significantly, sitting pain-free and enjoying a better quality of life. Two years after surgery, chemotherapy and radiotherapy, his condition remains improved.
Discussion
B-LBL is a solid tumour without blood involvement. The accepted definition of bone lymphoma is a tumour with bone involvement without evidence of systemic involvement. [7]. When there is more than 25 % blast in the bone marrow with or without mass lesion, the lesion is defined as lymphoid leukemia [8]. Primary vertebral location of non-Hodgkin lymphomas is rare and accounts for 1.7 % of all primary bone lymphoma [9]. Spinal lymphomas are more commonly found to take origin in the epidural space and derive from normal lymphoid tissue in the epidural space [9]. Spinal giant primary solitary B-LBL has not yet been described. To our knowledge, the treatment of this atypical lymphoma is not yet codified.
For Peng et al. [10] the ideal treatment of vertebral lymphoma is chemotherapy combined with radiotherapy. Park et al. [9] however argue that treatment of spinal lymphoma must be multifactorial including surgery, radiotherapy and chemotherapy.
In this particular case, the size of the tumour was important, so much so that prone position was made impossible. Moreover, it was very aggressive for the vertebras, causing kyphosis of the spine and a serious neurological status.
Surgery was warranted as initial treatment option, for decompression, stabilization and to improve the quality of life immediately. Chemotherapy and radiotherapy followed surgery with good outcome.
We think that the management of the vertebral B-LBL must be guided by the clinical state of the patient, and particularly by the therapeutic purpose to be reached. The indications to choose a treatment with regard to another one have to depend on priorities case by case.
Conclusion
We report a unique case of giant spinal primary B-LBL lymphoma with high bone aggressivity on presentation. Decompressive surgery and stabilization can be successfully used as an initial treatment option in this rare tumour.
References
Kim HJ, Lee TJ, Choi YS. Primary B Lymphoblastic lymphoma of gallbladder involving mandibular bone. Int J of Hematol. 2014;99:790–3.
Epstein JB, Epstein JD, Le ND, Gorsky M. Characteristics of oral and paraoral malignant lymphoma : a population based review of 361 cases. Oral Surg Oral Med Oral Path Oral Radiol Endod. 2001;92:519–25.
Alford MA, Nerad JA, Conlan RM, Comito M, Giller RH. Precursor B-cell lymphoblastic lymphoma presenting as an orbital mass. Orbit. 1999;18:17–24.
Gravel J, Lallier M, Garel L, Brochu P, Champagne J, et al. Primary non hodgkin lymphoma of the extrahepatic biliary tract and gallbladder in a child. J Pediatr Gastroenterol Nutr. 2001;32:598–601.
Lopes Da Silva R, Fernandes T, Santos S, Rodrigues AS, de Sousa AB. B lymphoblastic lymphoma presenting as a tumor of the nasopharynx in an adult patient. Head Neck Pathol. 2010;4:318–23.
Kantekure K, Cossor F, Miller KB, Pilichowska ME. A unique case of relapsed B acute lymphoblastic lymphoma. Case Rep hematol. 2014; dx.doi.org/10.1155/2014/425163.
Farrès MT, Dock W, Augustin I, Windhager R, Riegler M, et al. The radiologic clinical picture of primary bone lymphoma. Rofol. 1993;58:589–93.
Roy CA, Hawkes EA, Bardy P, Woo T, Ting K, et al. Rare case of precursor B-cell acute lymphoblastic leukemia presenting as a solitary paraspinal mass. J Clin Oncol. 2013;22:e383–5.
Park DA, Park SG, Kim SW. Solitary lymphoblastic lymphoma of the thoracic spine. J Korean Neurosurg Soc. 2012;52:564–6.
Peng X, Wan Y, Chen Y, Chen I, He A, et al. Primary non hodgkin’s lymphoma of the spine with neurologic compression treated by radiotherapy and chemotherapy alone or combined with surgical decompression. Oncol Rep. 2009;21:1269–75.
Acknowledgements
Not applicable.
Funding
No funding was available in support of this study.
Availability of data and materials
All data can be found in pubmed.
Authors’ contributions
HAN has performed surgery, drafted and revised the manuscript. LKD an LD assisted HAN for surgery. SAM revised the English language. DNO and VBZ as our heads accepted the final version for publication. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
The father was informed that the case would be submitted for publication and he provided consent. The consent form is available upon request.
Ethics approval and consent participate
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
N’da, H.A., Drogba, K.L., Derou, L. et al. A rare case of giant solitary spinal B cell lymphoblastic lymphoma. Chin Neurosurg Jl 2, 37 (2016). https://doi.org/10.1186/s41016-016-0052-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41016-016-0052-5