Abstract
Background
Anaphylactic shock during pregnancy is a rare but life-threatening event for both the mother and the newborn.
Case presentation
A 42-year-old woman, who was pregnant with twins, was scheduled for cesarean delivery under combined spinal and epidural anesthesia. An epidural catheter was placed uneventfully. After spinal anesthesia, the patient exhibited skin symptoms and severe hypotension. The patient was diagnosed with anaphylaxis, and subsequently, treatment was started. Fetal heart rate monitoring revealed sustained bradycardia, and it was decided to proceed with cesarean delivery. After delivery, the mother’s vital signs recovered. Both infants were intubated due to birth asphyxia. Currently, the twins are 4 years old and exhibit no developmental problems. Clinical examination identified mepivacaine as the causative agent of anaphylaxis.
Conclusions
This case report highlights that upon occurrence of anaphylaxis during pregnancy, maternal treatment and fetal assessment should be started immediately. Indication for immediate cesarean delivery should be considered and a definite identification of the causative factor pursued.
Similar content being viewed by others
Background
Anaphylactic shock during pregnancy is a rare but life-threatening event for both the mother and the newborn. The estimated incidence is 1.6 to 3.8 cases per 100,000 maternities, which is much lower than that in other populations [1,2,3]. Since numerous drugs are contraindicated for pregnant women, the fewer opportunities for drug use may contribute to the low incidence of anaphylaxis during pregnancy. Antibiotics have been reported as the main causative agent of anaphylaxis during pregnancy, whereas local anesthetics have rarely been reported [1, 2].
Managing anaphylactic shock during pregnancy is challenging, since the fetus’ condition and how it is affected by treatment must be considered. Upon occurrence of anaphylaxis during late pregnancy, the optimal timing for delivery and anesthetic management remain controversial. Emergency cesarean delivery may benefit the newborn but poses a risk for the mother, whose condition may be unstable [4]. Each patient’s clinical treatment strategy should therefore be determined based on anaphylaxis severity, maternal condition, and fetal status.
Here, we report a case of anaphylaxis in a pregnant woman undergoing combined spinal and epidural anesthesia for cesarean delivery. Clinical examination identified mepivacaine as the causative agent.
Case presentation
A 42-year-old woman, who was pregnant with twins, was scheduled for cesarean section at 37 weeks of gestation under combined spinal and epidural anesthesia. The woman had atopic dermatitis but no past history of drug allergy. After arrival at the operating room, intravenous administration of hydroxyethylated starch was started. Combined spinal and epidural anesthesia was administered in the right lateral position, at the L3–L4 and the Th12–L1 interspaces, respectively. After local infiltration of 6 mL of preservative-free 1% mepivacaine, the epidural space was identified by loss of resistance to saline, and an epidural catheter was placed. An aspiration test was confirmed as negative, and a test dose of 1% mepivacaine (3 ml) was administered via the catheter. During spinal anesthesia, maternal blood pressure became unmeasurable with a noninvasive blood pressure monitor. Lumbar puncture was successfully performed, and 10 mg of 0.5% hyperbaric bupivacaine and 20 μg of fentanyl were intrathecally administered. After returning the patient to the supine position, her face was swollen, and she exhibited erythema all over the body. Maternal blood pressure and heart rate were 74/56 mmHg and 112 beats/min, respectively. The mother was diagnosed with anaphylaxis and immediately received infusion of Ringer’s solution with left uterine displacement. Intravenous phenylephrine was intermittently administered. Despite hemodynamic instability, the mother’s breathing remained stable at 98% of oxygen saturation on room air, and oxygen was administered via a face mask. Fetal heart rate monitoring revealed sustained fetal bradycardia of 80 beats/min. Maternal systolic blood pressure remained around 80–90 mmHg under repeated administration of phenylephrine and transfusion. Fetal bradycardia was not recovered. After confirming the sensory block level of Th4, it was decided to proceed with cesarean delivery. The infants were delivered 17 and 18 min after anaphylaxis onset, both without spontaneous respiration, and were intubated and transferred to the neonatal intensive care unit. At 1 and 5 min, the apgar scores were 2 and 4 for the first infant and 2 and 5 for the second infant, respectively. Analysis of the umbilical artery blood revealed a pH of 6.842 for the first infant and 6.775 for the second infant. After delivery, the mother’s vital signs were recovered and remained stable. A two-phase allergic reaction was prevented through administration of 500 mg of methylprednisolone. After surgery, the mother was continuously monitored in the maternity ward, and her clinical course remained uneventful, being discharged 6 days after surgery. The first infant was extubated 2 days after birth and discharged 13 days after birth, whereas the second infant required further examination and treatment after having seizures. He was discharged with an oral anticonvulsant 16 days after birth, after which he remained seizure-free. The anticonvulsant was discontinued at 6 months of age. Currently, the twins are 4 years old and exhibit no developmental problems.
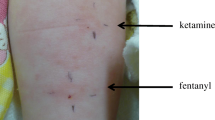
We suggested the patient to be examined to determine the causative agent of anaphylaxis. The patient agreed to be subjected to the basophil activation test (BAT), but not the skin test. The BAT was performed 9 months after the operation for mepivacaine and hydroxyethylated starch, providing a positive result to mepivacaine (Fig 1). The patient was then suggested once more to undergo the skin test to confirm the accuracy of the BAT results and to investigate cross-reactivity with other local anesthetics. The skin prick test was performed 10 months after the operation, for latex, hydroxyethylated starch, procaine, lidocaine, bupivacaine, and mepivacaine, providing a positive reaction to both lidocaine and mepivacaine (Fig 2).
Discussion
The present case describes anaphylaxis in a pregnant woman who underwent combined spinal and epidural anesthesia for cesarean delivery. The immediate diagnosis, treatment, and cesarean delivery may have led to the good outcomes achieved for both the mother and the newborns.
When treating anaphylaxis during late pregnancy, besides comprehensive treatment, care should be taken to evaluate the fetal condition and to decide the best delivery timing. Primary management of anaphylaxis includes immediate withdrawal of antigen administration, seeking help, airway maintenance, aggressive fluid resuscitation, and adrenaline administration. Examining serum tryptase and histamine levels is useful for diagnosing anaphylaxis. Additionally, obstetric management may involve left uterine displacement and fetal monitoring. Maternal hypotension immediately affects the placental circulation and fetal status. However, the American College of Obstetricians and Gynecologists indicates that, during anaphylaxis, a stable maternal hemodynamic status does not ensure adequate placental perfusion and fetal oxygenation, whereas normal fetal heart rate variability reassures fetal status [5]. Previous studies recommend that emergency cesarean delivery should be considered in cases of persistent maternal hemodynamic instability, despite resuscitation [4, 6]. In the present case, monitoring fetal heart rate was the key for the decision to perform a cesarean delivery. Although the good outcomes were achieved, fetal bradycardia was not recovered by phenylephrine. Administration of adrenaline for anaphylaxis may have increased cardiac output and systemic vascular resistance, resulting in improved uteroplacental perfusion [7].
Among previous case reports of anaphylactic labor, 46% resulted in adverse fetal neurologic outcomes [8,9,10,11,12,13]. In such cases, the anaphylactic parturients either had a delayed cesarean delivery [8, 9, 13] or did not receive sufficient adrenaline to manage severe hypotension [11]. The fetal neurologic outcome was much better in cases of anaphylaxis occurring during cesarean delivery, which can be attributed to a short duration of fetal cerebral ischemia [4]. The benefits of emergency cesarean delivery for anaphylactic patients refractory to medical treatment need to be balanced against the risks of surgery in pregnant women with an unstable general condition. If the time of gestation is less than 32 weeks, the risks of neonatal morbidity and mortality should also be considered. Anaphylaxis-related cardiovascular disturbance can be enhanced in pregnant patients by inferior vena cava compression. Moreover, neuraxial anesthesia blocks the sympathetic nerve, often causing hypotension. For anaphylaxis occurring during cesarean delivery, maternal morbidity due to severe complications was reported in 20% of cases [4]. In the present case, anaphylaxis occurred during the intrapartum period, and the immediate cesarean delivery exerted a beneficial impact both on the mother and the infants.
Identifying the causative agent of anaphylaxis is essential to prevent allergic reactions. Agents, or known as allergens, administered immediately before an event, are often determined as culprit allergens without subsequent examinations. Had we not pursued the cause of the allergic reaction, we might have mistakenly assumed that the hydroxyethylated starch was the allergen, since anesthetic allergies have rarely been reported. Therefore, it should be kept in mind that the suspected agent may not be the true causative agent, and incorrect speculation may place the patient at risk of further exposure to the true allergen or cause unnecessary avoidance of harmless effective drugs.
The skin prick test is the gold standard to determine the cause of anaphylaxis, although it carries the risk of immediate hypersensitivity reactions. On the other hand, the BAT is an in vitro examination, which poses no risk of anaphylactic reactions. The BAT is based on the upregulation of granule-derived markers expressed at the basophil membrane upon ex vivo activation by the suspected agent. It recently became widely accepted as an additional and reliable tool, with high sensitivity and specificity to identify the causative agent of immediate drug hypersensitivity [14,15,16,17]. Further studies are required to evaluate the usefulness of this tool as a diagnostic approach of anaphylaxis, although diagnostic precision can be improved by combining multiple methods, such as the skin test and the BAT. In the present case, positive reactions to mepivacaine in both the BAT and skin prick test would support the reliability of BAT as a diagnostic tool.
In summary, the present case highlights that, upon anaphylaxis during pregnancy, maternal treatment and fetal heart rate monitoring should be started immediately. If the maternal hemodynamic status does not recover or if persistent non-reassuring fetal heart rate patterns are observed, immediate cesarean delivery should be considered, especially at the intrapartum period. Moreover, pursuing a definite diagnosis of the culprit allergen is beneficial for patients to prevent allergic reactions.
Availability of data and materials
Not applicable
Abbreviations
- BAT:
-
Basophil activation test
References
McCall SJ, Bunch KJ, Brocklehurst P, D’Arcy R, Hinshaw K, Kurinczuk JJ, et al. The incidence, characteristics, management and outcomes of anaphylaxis in pregnancy: a population-based descriptive study. BJOG. 2018;125:1340–1.
Mccall SJ, Kurinczuk JJ, Knight M. Anaphylaxis in pregnancy in the United States: risk factors and temporal trends using national routinely collected data. J Allergy Clin Immunol Pract. 2019;S2213-2198(19)30455-6.
Harper NJN, Cook TM, Garcez T, Lucas DN, Thomas M, Kemp H, Kong KL, et al. Anaesthesia, surgery, and life-threatening allergic reactions: management and outcomes in the 6th National Audit Project(NAP6). Br J Anaesth. 2018;121:172–88.
Hepner DL, Castells M, Mouton-Faivre C, Dewachter P. Anaphylaxis in the clinical setting of obstetric anesthesia: a literature review. Anesth Analg. 2013;117:1357–67.
American College of Obstetricians and Gynecologists, ACOG Practice Bulletin No.106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol. 2009;114:192–202.
Adriaensens I, Vercauteren M, Soetens F, Janssen L, Leysens J, Ebo D. Allergic reactions during labour analgesia and caesarean section anaesthesia. Int J Obstet Anesth. 2013;22:231–42.
Riley ET, Editorial I. Spinal anaesthesia for caesarean delively: keep the pressure and don’t spare the vasoconstrictors. Br J Anaesth. 2004;92:459–61.
Chaudhuri K, Gonzales J, Jesurun CA, Ambat MT, Mandal-Chaudhuri S. Anaphylactic shock in pregnancy: a case study and review of the literature. Int J Obstet Anesth. 2008;17:350–7.
Shingai Y, Nakagawa K, Kato T, Fujioka T, Matsumoto T, et al. Severe allergy in a pregnant woman after vaginal examination with a latex glove. Gynecol Obstet Invest. 2002;54:183–4.
Kaneko K, Maruta H. Severe anaphylactoid reaction to ranitidine in a parturient with subsequent fetal distress. J Anesth. 2003;17:199–200.
Berardi A, Rossi K, Cavalleri F, Simoni A, Aguzzoli L, et al. Maternal anaphylaxis and fetal brain damage after intrapartum chemoprophylaxis. J Perinat Med. 2004;32:375–7.
Sheikh J. Intrapartum anaphylaxis to penicillin in a woman with rheumatoid arthritis who had no prior penicillin allergy. Ann Allergy Asthma Immunoll. 2007;99:287–9.
Khan R, Anastasakis E, Kadir RA. Anaphylactic reaction to ceftriaxone in labour. An emerging complication. J Obstet Gynaecol. 2008;28:751–3.
Horiuchi T, Yokohama A, Orihara M, Tomita Y, Tomioka A, et al. Usefulness of basophil activation tests for diagnosis of sugammadex-induced anaphylaxis. Anesth Analg. 2018;126:1509–16.
Ebo DG, Faber M, Elst J, Van Gasse AL, Birdts CH, et al. In vitro diagnosis of immediate drug hypersensitivity during anesthesia: a review of the literature. J Allergy Clin Immunol Pract. 2018;6:1176–84.
Takazawa T, Sabato V, Ebo DG. In vitro diagnostic tests for perioperative hypersensitivity, a narrative review: potential, limitations, and perspectives. Br J Anaesth. 2019;123:e117–25.
Dewachter P, Chollet-Martin S, Mouton-Faivre C, de Chaisemartin L, Nicaise-Roland P. Comparison of basophil activation test and skin testing performances in NMBA allergy. J Allergy Clin Immunol Pract. 2018;6:1681–9.
Acknowledgements
The authors would like to thank Enago (https://www.enago.jp) for the English language review.
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
MT and TI participated in the anesthetic management. SI, TT, and TH supported to make a clinical diagnosis. MK drafted the manuscript. KH and MT supervised the manuscript drafting. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Takahashi, M., Hotta, K., Inoue, S. et al. Mepivacaine-induced anaphylactic shock in a pregnant woman undergoing combined spinal and epidural anesthesia for cesarean delivery: a case report. JA Clin Rep 5, 84 (2019). https://doi.org/10.1186/s40981-019-0302-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40981-019-0302-6