Abstract
Aortobronchial fistula (ABF) is a rare and potentially lethal complication of thoracic aortic replacement surgery. Currently, thoracic endovascular aortic repair (TEVAR) has emerged as a less invasive alternative to open surgery for ABF to facilitate prompt hemostasis. However, there are no published reports of TEVAR for ABF, particularly for presentation with life-threatening respiratory failure from massive hemoptysis.
A 48-year-old male patient, who had recently undergone aortic root and arch replacement due to aortic dissection, was transferred to the emergency department with massive hemoptysis and severe dyspnea. A single-lumen endotracheal tube was immediately placed in the right main bronchus to protect the nonbleeding lung from spillage of blood. Chest computed tomography (CT) showed leakage of contrast material from the distal anastomosis of the aortic graft and consolidated lung tissue adjacent to the leakage. He was diagnosed with an ABF following aortic arch replacement, and an emergency TEVAR was performed. After adequate hemostasis, severe hypercapnia remained uncorrected despite the maximum ventilatory support. Thus, venovenous extracorporeal membrane oxygenation (VV ECMO) was immediately initiated, and severe respiratory acidosis improved dramatically. Furthermore, VV ECMO facilitated prompt bronchoscopic washout of the remaining blood clot without any danger of respiratory collapse and was weaned off successfully after 5 days as ventilation improved.
This case demonstrates that emergency TEVAR in combination with VV ECMO can be a rescue strategy for massive hemoptysis from an ABF.
Similar content being viewed by others
Background
Aortobronchial fistula (ABF) is a rare and potentially lethal complication of thoracic aortic replacement surgery [1]. Thoracic endovascular aortic repair (TEVAR) is a less invasive alternative to open surgery for ABF to facilitate prompt hemostasis [2]. However, there are no published reports of TEVAR for ABF, particularly for presentation with life-threatening respiratory failure from massive hemoptysis. We describe a successful combination of venovenous extracorporeal membrane oxygenation (VV ECMO) with emergency TEVAR for a patient with ABF and life-threatening hemoptysis.
Case presentation
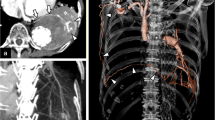
The patient was a 48-year-old male, who had undergone aortic root and arch replacement due to aortic dissection 10 months prior to the admission. He had cough and hemoptysis 1 month prior to the admission, but he had not come to the hospital. He was transferred to the emergency department with massive hemoptysis and severe dyspnea. Even after initial resuscitation of hemorrhagic shock, respiratory failure continued because of uncontrolled massive hemoptysis; thus, a single-lumen endotracheal tube was immediately placed in the right main bronchus to protect the nonbleeding lung from blood spillage. Arterial blood gas analysis showed severe respiratory acidosis (pH, 7.13; pCO2 76.2 mmHg, pO2 92.8 mmHg; HCO3 − 25.2 mEq/L; BE −4.0 mmol/L). Chest computed tomography showed leakage of contrast material from the distal anastomosis of the aortic arch, and chest X-ray showed consolidated lung tissue adjacent to the leakage (Fig. 1). He was diagnosed with ABF following aortic arch replacement, and emergency TEVAR was scheduled. At this time, massive hemothorax and lung bleeding from the ABF had led to not only potentially lethal hypercapnic respiratory failure but also hemodynamic instability. Therefore, endovascular treatment was preferred to achieve hemostasis and avoid prolonged operative time, because extensive pleural adhesions were anticipated from a history of repeat thoracotomy.
Emergency TEVAR under general anesthesia was successfully completed within 30 min and provided both adequate hemostasis and hemodynamic stability. He was transfused with 22 units of packed red blood cells, 20 units of platelet concentrate, and 18 units of fresh frozen plasma until adequate hemostasis was achieved. Despite the maximum manual ventilatory support and administration of tromethamine, severe hypercapnia and life-threatening acidosis remained uncorrected. Worse still, peak airway pressure higher than 60 mmH2O was required to achieve tidal volume of 5 ml/kg. Arterial blood gas analysis showed the following: pH, 6.88; pCO2, 199.9 mmHg; pO2, 129.0 mmHg; HCO3 −, 37.3 mEq/L; and BE, 3.3 mmol/L. Thus, VV ECMO was immediately initiated as a bridge therapy for respiratory recovery. Drainage cannula was inserted from the left femoral vein and placed in the inferior vena cava. Return cannula was inserted into the right internal jugular vein. Intravenous heparin (2000 units) was administered before cannula insertion to maintain activated clotting time (ACT) values lower than 200 s. Additional heparin was not required to maintain adequate anticoagulation during the surgery.
Soon after the initiation of ECMO, the severe respiratory acidosis dramatically improved to a pH of 7.34, a pCO2 of 39.3 mmHg, and a bicarbonate level of 21.0 mEq/L. Sufficient oxygenation was provided without ventilation during maintenance with ECMO; therefore, fiber-optic bronchoscopy was performed to clear the airways of the remaining blood clots without any danger of respiratory collapse. Additionally, endotracheal tube in the right main bronchus was replaced to the trachea in the operation room. Intravenous heparin was continued after ICU admission because there were no signs of hemoptysis. The aim of ACT was 180 to 200 s, and there was no obvious bleeding from the bronchus during ECMO therapy. For the purpose of preventing rebleeding, positive end-expiratory pressure (PEEP) was maintained above 10 cmH20. Propofol and dexmedetomidine were administered to provide adequate sedation. The dose of these drugs were adjusted aiming to achieve a Richmond Agitation Sedation Scale of 0 to −2. Despite the additional blood, components were required for few days to correct for anemia and coagulation disorder, and he was hemodynamically stable without vasopressors. Although hypercapnia was corrected after removing blood clots, subsequent oxygenation failure emerged after the ICU admission impeded weaning from VV ECMO for 5 days. Fluid removal by continuous renal replacement therapy improved oxygenation, and VV ECMO was weaned off uneventfully on postoperative day 5 (see Table 1).
However, on postoperative day 12, he developed fever and distributive shock. Contrast CT indicated mesenteric artery embolism and multiple cerebral infarctions. From these findings, intestinal necrosis and sepsis due to bacterial translocation were suspected. Despite the intensive therapy including resection of the necrotic intestine, his infection was difficult to treat and the patient died on postoperative day 56.
Discussion
Hemoptysis is the first and often only symptom of ABF, a rare complication of thoracic aortic replacement surgery [1]. Once a massive hemoptysis occurs from ABF, patients require urgent medical treatment because of a double risk of death from hypovolemic shock by uncontrolled bleeding and bronchial tree obstruction by blood clots. Therefore, prompt diagnosis and hemostasis are essential to decrease mortality [3, 4]. TEVAR is a less invasive alternative to open surgery for ABF to facilitate prompt hemostysis [2]. Although there are several reports of successful management with VV ECMO in patients with pulmonary hemorrhage or hemoptysis [5,6,7,8], to our knowledge, this is the first case of ABF with life-threatening hemoptysis treated successfully under VV ECMO after emergency TEVAR.
Although ECMO was successfully applied in some reported cases of thoracic aortic rupture [9] and lung bleeding [5,6,7,8], it remains unclear whether ECMO can be safely applied in massive hemoptysis; in other words, systemic anticoagulation and thrombocytopenia during ECMO are debatable. However, we focused on immediate correction of life-threatening acidosis, consequently leading to recovery of hemostatic function, on the assumption that severe acidosis could probably induce coagulopathy by fibrinogen degeneration [10] and platelet functional impairment [11]. Moreover, it was of utmost importance that ECMO support could allow the patient to undergo prompt bronchoscopic washout of the remaining blood clots from the lower airway without any danger of respiratory collapse. Emergency physicians must be aware of these potential benefits of VV ECMO as a bridge for life-threatening hemoptysis.
Ventilator management for ABF is a clinical challenge. According to the Extracorporeal Life Support Organization (ELSO) guideline [12], a lung rest setting is recommended after initiation of ECMO. Low plateau inspiratory pressure (under 25 cm H2O) is desirable and PEEP is usually set between 5–15 cmH2O. However, low inspiratory pressure could predispose to bleeding for patients with hemoptysis. Similar to our case, a lung bleeding patient was successfully managed with higher airway pressure (max plateau pressure 35 cmH2O for a day) in a previous report [8]. In terms of hemostasis, transient high airway pressure may be permitted until bleeding stops.
A balance between preventing thrombosis (anticoagulation) and bleeding risk has been a difficult clinical dilemma. In our case, heparin was continuously administered during ECMO therapy. Nevertheless, there was an embolic event after weaning of ECMO. In addition to the use of ECMO, aortic dissection could predispose to systemic hypercoagulation and thromboembolism. Although antithrombin III (AT) was not examined, AT deficiency was also suspected because of increasing needs of heparin dose during ECMO therapy. In consideration of avoiding hemorrhage, we aimed ACT below 200 s according to the previous reports [5,6,7]. However, there was a case of successful VV ECMO for alveolar hemorrhage under a mean ACT of 274 s [8]. Heparin administration aiming for higher ACT levels and/or AT replacement might have prevented the fatal mesenteric artery embolism, provided that there were no signs of bleeding complications. Anticoagulation therapy should be carefully titrated with observing clinical presentations.
On the other hand, the emergency endovascular approach is a promising treatment option for ABF and acute massive hemoptysis, assuming that surgical repair through a left thoracotomy approach may be technically difficult due to extensive pleural adhesions or vascular abnormalities.
Conclusions
This case demonstrates that emergency TEVAR in combination with VV ECMO can be an attractive rescue strategy for massive hemoptysis in a patient with an ABF.
Abbreviations
- ABF:
-
Aortobronchial fistula
- CT:
-
Computed tomography
- TEVAR:
-
Thoracic endovascular aortic repair
- VV ECMO:
-
Venovenous extracorporeal membrane oxygenation
References
MacIntosh EL, Parrott JC, Unruh HW. Fistulas between the aorta and tracheobronchial tree. Ann Thorac Surg. 1991;51:515–9.
Bailey CJ, Force S, Milner R, Kasirajan K, Veeraswamy RK. Thoracic endovascular repair as a safe management strategy for aortobronchial fistulas. J Vasc Surg. 2011;53:1202–9.
Liu SF, Chen YC, Lin MC, Kao CL. Thoracic aortic aneurysm with aortobronchial fistula: a thirteen-year experience. Heart Lung. 2004;33:119–23.
Picichè M, De Paulis R, Fabbri A, Chiariello L. Postoperative aortic fistulas into the airways: etiology, pathogenesis, presentation, diagnosis, and management. Ann Thorac Surg. 2003;75:1998–2006.
Ahmed SH, Aziz T, Cochran J, Highland K. Use of extracorporeal membrane oxygenation in a patient with diffuse alveolar hemorrhage. Chest. 2004;126:305–9.
Hohenforst-Schmidt W, Petermann A, Visouli A, Zarogoulidis P, Darwiche K, Kougioumtzi I, Tsakiridis K, Machairiotis N, Ketteler M, Zarogoulidis K, Brachmann J. Successful application of extracorporeal membrane oxygenation due to pulmonary hemorrhage secondary to granulomatosis with polyangiitis. Drug Des Devel Ther. 2013;7:627–33.
Mongero LB, Brodie D, Cunningham J, Ventetuolo C, Kim H, Sylvan E, Bacchetta MD. Extracorporeal membrane oxygenation for diffuse alveolar hemorrhage and severe hypoxemic respiratory failure from silicone embolism. Perfusion. 2010;25:249–52.
Patel JJ, Lipchik RJ. Systemic lupus-induced diffuse alveolar hemorrhage treated with extracorporeal membrane oxygenation: a case report and review of the literature. J Intensive Care Med. 2014;29:104–9.
Masroor S, Tehrani H, Pham S, Neijman T, Martinez-Ruiz R, McKenney M, et al. Extracorporeal life support in pulmonary failure after traumatic rupture of the thoracic aorta: a case report. J Trauma. 2004;57:389–91.
Martini WZ, Holcomb JB. Acidosis and coagulopathy: the differential effects on fibrinogen synthesis and breakdown in pigs. Ann Surg. 2007;246:831–5.
Hanke AA, Dellweg C, Kienbaum P, Weber CF, Görlinger K, Rahe-Meyer N. Effects of desmopressin on platelet function under conditions of hypothermia and acidosis: an in vitro study using multiple electrode aggregometry. Anaesthesia. 2010;65:688–91.
ELSO Guidelines for Cardiopulmonary Extracorporeal Life Support Extracorporeal Life Support Organization, Version 1.3. Ann Arbor; 2013. https://www.elso.org/Portals/0/IGD/Archive/FileManager/929122ae88cusersshyerdocumentselsoguidelinesgeneralalleclsversion1.3.pdf. Accessed 8 June 2017.
Authors’ contributions
KT wrote the case report. MK and WT conducted anesthetic management to the patient. TK, WT, and YK helped to draft the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
This case report was approved by the Institutional Review Board and Hospital Research Ethics Committee of Kawasaki Saiwai Hospital.
Consent for publication
Written informed consent was obtained from the patient’s family because the patient died.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Takahashi, K., Kajitani, M., Kamada, T. et al. Endovascular repair with extracorporeal membrane oxygenation as a rescue strategy for aortobronchial fistula: a case report. JA Clin Rep 3, 34 (2017). https://doi.org/10.1186/s40981-017-0103-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40981-017-0103-8