Abstract
Background
To compare the functional and anatomical outcomes of primary surgery in patients with giant retinal tear (GRT)-associated retinal detachment (GRT-RD) to patients with simple rhegmatogenous RD (RRD).
Methods
This is a retrospective study at the CHU de Québec - Université Laval. Medical records of all consecutive patients operated for RD between 2014 and 2018 were reviewed. Patients with GRT-RD and RRD were included. Preoperative, intraoperative, and postoperative data were compared between both groups, including extension of giant tears, number of RD quadrants, preoperative macula and lens status, type of surgery, best corrected visual acuity (BCVA) in logarithm of the minimum angle of resolution (logMAR) preoperatively and at follow-up, and single surgery anatomical success (SASS).
Results
There were 39 patients (1.7%) with GRT-RD and 1661 patients (74%) with RRD. Median [Q1, Q3] ages were 59 [52, 62] years and 62 [56, 69] years (p = 0.003), while number of affected quadrants were 2 [2, 3] and 2 [2, 3] (p = 0.96) in GRT-RD and RRD patients, respectively. In GRT-RD patients, GRT size was 120 [90, 150] degrees. Final BCVA was 0.30 [0.10, 0.30] and 0.30 [0.10, 0.40] (p = 0.76) in GRT and RRD patients, respectively. SSAS was 82% (32/39) in the GRT-associated-RD group and 90% (1495/1661) in the RRD group (p = 0.10). After correcting for other preoperative factors, GRT was a risk factor for worse SSAS (odds ratio: 0.422, p = 0.047).
Conclusions
GRT-RD is still challenging to treat, and our results suggest that it is a risk factor for poorer SSAS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Giant retinal tears (GRTs) are defined as full thickness neurosensory retinal breaks extending circumferentially for 90° (3 clock hours) or more in the presence of posterior vitreous detachment (PVD) [1]. Different risk factors have been identified for GRT such as high myopia, trauma, pseudophakia and aphakia, and connective tissue diseases (e.g., Marfan syndrome, Stickler syndrome). The majority of GRTs are idiopathic and occur spontaneously [2].
GRTs can lead to the development of retinal detachment (RD), causing rapid and important loss of vision in most patients. It is estimated that GRTs are responsible for 0.5 to 8.3% of all RD [3,4,5,6]. In such cases, surgery is required to reattach the retina and optimize final functional outcomes. Like in simple rhegmatogenous RD (RRD), both pars plana vitrectomy (PPV) and PPV with scleral buckle (SB) (PPV-SB) are commonly used for management of GRT-associated-RD (GRT-RD). However, an increased tendency for proliferative vitreoretinopathy (PVR) development and greater technical requirements contribute to poorer outcomes in these patients [7, 8]. GRT-RD treatment remains a challenge for retinal surgeons and anatomical success of primary surgery tends to be lower than for RRD.
Few studies from a single center directly compared the qualitative and quantitative characteristics between GRT-associated-RD and simple RRD patients. The aim of this study is to analyze the anatomical and functional outcomes in GRT-RD and simple RRD patients, including rate of primary surgery success and final visual acuity. The secondary objective is to identify any factors predictive of a successful surgical outcome and better visual outcome.
Methods
This is a retrospective study of all patients operated for GRT-RD (n = 39) or RRD (n = 1661) at the Centre hospitalier universitaire de Québec - Université Laval between 2014 and 2018. It adhered to the tenets of Declaration of Helsinki and the Institutional Review Board of the CHU de Québec (Reference number 2020:4798). Individual patient consent was waived given the retrospective nature of the study. All patients were operated for RD by one of five fellowship certified attending vitreoretinal surgeons. Surgery choice and tamponade agent used were at the discretion of the treating surgeon and were comparable between all surgeons. Patients with secondary causes of RD, including traumatic RD (including traumatic GRT), tractional diabetic RD, RD with preoperative PVR ≥ C2, retinoschisis, retinal dialysis, and macular holes were excluded. Patients treated with pneumatic retinopexy as primary surgery were also excluded (shown in Fig. 1). All ophthalmology follow-ups until March 2020 were reviewed and included for analysis. Patients needed to have a minimum follow-up of 3 months to be included.
We collected complete preoperative, intraoperative, and postoperative data for all included patients from baseline evaluations including visual acuity, ophthalmic history, complete slit lamp exam, and dilated fundus examination, intraoperative surgeon observations, and follow-up visits. Preoperative data included age, sex, laterality, best-corrected visual acuity (BCVA) at baseline, lens status (i.e., phakic, pseudophakic, or aphakic), macula status (i.e., on, off, or split), myopia ≥ 4 diopters, the number of RD quadrants, the size of the giant retinal tear for the GRT group, and the duration of symptoms before first surgery. Macula status was determined through clinical examination, but in cases which were unclear, optical coherence tomography (OCT) were reviewed to confirm macula status. RD not involving the fovea were defined as “macula on”, RD fully involving the fovea were considered “macula off”, and RD partially involving the fovea were considered “macula split.”
The presence of a GRT or an RD was evaluated based on clinical assessment by a surgical retina specialist. Classification of patients as having GRT-RD or RRD, as well as classification of the size of GRT are based on the preoperative and intraoperative assessment of the RD. All retinal specialist used the standard definition of GRT (i.e., 90° or more) to make the diagnosis. In this study, we defined all full-thickness retinal defects as retinal breaks. The number of retinal breaks was noted in preoperative evaluations and confirmed by direct observation intraoperatively. The presence of PVR was also confirmed by notation on surgery protocol. Operative data included the type of surgery and tamponade agent used for the primary surgery. Postoperative data included BCVA at 3 months and at the final follow-up, the development of visually significant cataracts requiring surgery, and the total duration of follow-up. Primary outcome was single surgery anatomical success (SSAS) defined as the absence of RD recurrence requiring an additional surgical intervention at any time during follow-up. Laser procedures performed in the outpatient clinic were not considered reoperations and patients needed to be followed for a minimum of 3 months to confirm SSAS.
Surgical data were further analyzed to determine the influence of initial surgery choice on SSAS. To compare the surgical anatomical and functional success, we focused on the two main surgeries performed for the treatment of RD: PPV alone and PPV-SB. We also compared the SSAS for patients with GRT-RD against patients with RRD.
Statistical analysis
Data are presented as mean ± standard deviation for continuous, normally distributed variables, as median [first quartile, third quartile] for continuous, non-normally distributed variables, and as frequencies (percentages) for categorical variables. Characteristics and variables were compared between the two groups (i.e., PPV and PPV-SB) using independent Student’s t-test or Mann–Whitney U test for continuous variables and Chi-square analysis or Fisher’s exact test for categorical variables, as appropriate. Shapiro–Wilk test and Q–Q plots with 95% confidence intervals were used to test for normal distribution of continuous variables.
Vision was converted from metric Snellen notation to logarithm of the minimum angle of resolution (logMAR) for analysis purpose [9]. Vision levels of counting fingers, hand motion, light perception, and no light perception were assigned Snellen visual acuity values of 1.0/200, 0.5/200, 0.25/200, and 0.125/200 (logMAR equivalent 2.3, 2.6, 2.9, and 3.2, respectively) [10, 11].
A multiple logistic regression model was built for SSAS. All relevant preoperative and intraoperative characteristics were considered for inclusion. These include age, sex, pseudophakia, myopia greater than 4 diopters, presence of GRT, baseline VA, duration of symptoms at presentation, RD quadrants involved, preoperative macula status, type of surgery, type of gas tamponade. Variables were included in the model while respecting a minimum of 5–9 events per predictor variable [12]. A backwards elimination strategy was used to manually select variables for the final model, with variables p > 0.2 removed. Odds ratios (OR) with 95% confidence intervals (CI) were produced for each variable included. Number of RD quadrants, macula status, and visual acuity at presentation were not added in the final model because of collinearity with the presence of inferior tears in inferior RD variable which was more closely associated with the outcome. Aphakia was also not considered given that no patient in the GRT group was aphakic and only 11 patients in the RRD group were aphakic.
Statistical analyses were performed using R for Windows (version 3.6.3; R Foundation for Statistical Computing) and IBM SPSS Statistics for Windows (version 27.0; IBM Corp., Armonk, NY). Analyses were conducted at the 0.05 significance level.
Results
Patient baseline characteristics
During the study period, among 2247 patients operated for RD, 39 eyes (1.7%) were operated for GRT-RD and 1661 eyes (74%) for simple RRD. Baseline characteristics by group are presented in Table 1. Median [Q1, Q3] age at the time of primary surgery was significantly greater among the RRD group compared to the GRT-RD group (62 [56, 69] years vs. 59 [52, 62] years; p = 0.003). There was no significant difference in macular status at presentation between the GRT-RD group compared to the RRD group preoperatively (p = 0.07). There were no other differences among baseline characteristics, including number of RD quadrants, baseline BCVA, or duration of symptoms. In the GRT-RD group, the median size of the GRT at baseline was 120 [90, 150] degrees. In RRD patients, the median [Q1, Q3] number of retinal tears within the retinal detachment was 2 [1, 3].
Intraoperative management
The primary surgery type performed and choice of tamponade agent by group are presented in Table 1. Principal surgery performed in the entire cohort was PPV (n = 843, 50%) and PPV-SB (n = 744, 43%) and there was no statistically significant difference between the GRT-RD and the RRD groups regarding procedure choice (p = 0.07). None of the patients in the GRT-RD group were treated with SB alone, and 7% of RRD group had SB alone. A significantly greater number of patients in the GRT-RD group received C3F8 as primary tamponade agent compared to the RRD group (n = 28, 72% vs. n = 291, 18%) (p < 0.001).
Postoperative outcomes
The median total duration of follow-up was 17 [4, 28] months and 11 [3, 25] months in the GRT-RD and RRD groups, respectively (p = 0.05). At 3 months and at final follow-up, BCVA was not significantly different between RRD patients compared to GRT-RD patients.
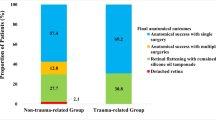
SSAS was achieved in 32 (82%) GRT-RD patients, while SSAS was achieved in 1495 (90%) RRD patients (p = 0.10). PVR was the cause of surgery failure for all 7 patients who had RD recurrences in the GRT-RD group and among them, two patients underwent PPV alone as primary surgery (n = 2/16, 13%) and five patients underwent PPV-SB (n = 5/23, 22%) (p = 0.68). For the RRD patients, the success rate of PPV alone and PPV-SB was also similar. Among those with RD recurrences, 76 patients were treated with PPV alone (76/827, 9%) and 80 patients were treated with PPV-SB (80/721, 11%) (p = 0.21). Among patients who had recurrences in the RRD group, 133 (8%) required a second surgery, while 31 (2%) required three and 2 (0.1%) required four surgeries. This was similar to patients in the GRT-RD group who required two surgeries in 4 patients (10%), three surgeries in 2 (5%) and four surgeries in 1 (2.6%) (p = 0.09). Final retina status was “on” for 39 (100%) of GRT-RD patients compared to 1655 (99.6%) of RRD patients (p = 1.00).
Multiple regression analysis for SSAS
The final multiple logistic regression model for SSAS is presented in Table 2. The variables included in the model were: age, sex, duration of symptoms, presence of myopia, presence of GRT, macula status and pseudophakia. Number of RD quadrants, and visual acuity at presentation were not added in the final model because of collinearity. Aphakia was also not considered given that no patient in the GRT group was aphakic and only 11 patients in the RRD group were aphakic. After correction for other preoperative factors, GRT was associated with a significantly decreased rate of SSAS (OR 0.422, 95% CI 0.190–1.071; p = 0.047).
Discussion
In this study, we compared the anatomical and functional outcomes of 39 eyes with GRT-RD to 1661 eyes with simple RRD. The prevalence of GRT-RD of 1.7% in our cohort is comparable with previous studies reporting a prevalence of 0.5 to 8.3% [3,4,5,6]. A Scottish study reported a GRT-RD prevalence of 1.3% among 1130 patients with RD [13].
The baseline characteristics between both groups differed significantly for age. In our study, GRT-RD patients were significantly younger than RRD patients at presentation. It is known that giant retinal tears affect younger patients, with a mean age of 30 to 53 years old in previous reports [14,15,16,17,18,19,20,21]. While the median age of GRT-RD patients in our study is greater than that reported in the literature, this discrepancy can be explained by the fact that we did not include traumatic GRT. Trauma is an important risk factor for developing a GRT and younger patients are more susceptible to experiencing a trauma. There is also a known preponderance of GRT in men than in women [2]. In our study, 29 patients (74%) in the GRT-RD group were men, which is consistent with a male prevalence between 65 and 91% previously reported [22]. Meanwhile, there was no significant difference between the BCVA and the macular status of patients with GRT-RD or RRD at baseline. The median BCVA at presentation was 20/40 for GRT-RD group, which is within the expected range observed in GRT [23]. While traumatic GRT and PVR grade C2 or greater may be expected to have a higher prevalence of detached macula, these cases had been excluded.
The BCVA at 3 months of follow-up and at final follow-up were similar between both groups. The high proportion of patients being macula “on’’ at baseline in the GRT-RD group and the fact that traumatic GRT were excluded could have contributed to better visual outcomes.
In our study, the primary reattachment rate was not significantly different between GRT-RD and RRD patients (82% vs 90%, p = 0.10). Previously published studies have stated a primary anatomical success rate between 68 and 96% in GRT-RD patients, which is concordant with our results [22]. The British Giant Retinal Tear Epidemiology Eye Study (BGEES) prospectively analyzed 60 patients (62 eyes) with GRT-RD. They had a primary anatomical success rate of 87.7%, which is also compatible with our analysis [23]. Our multiple regression analysis however suggests that GRT might be associated with poorer anatomical outcomes in the primary repair of RD. The bigger size of the retinal tears and increased propensity for PVR development in GRT-RD patients may be plausible explanation. The final anatomical success rate in our study was 100% (39/39) and 99.6% (1655/1661), which is consistent with previous reports (81% to 100%) [22].
Different types of surgery exist for the repair of GRT-RD but PPV alone and PPV combined with a SB (PPV-SB) remain the most frequently performed. In our study, the primary anatomical success rate was not significantly different between PPV and PPV-SB in GRT-RD patients (88% vs. 78%; p = 0.68). In 2018, Rodriguez et al. analyzed 80 eyes treated with SB, PPV or PPV-SB for GRT-RD and found no differences in the primary anatomical success rate between the three groups [24]. Another study of 94 Indian patients with GRT-RD also stated no differences in the anatomical outcomes of primary surgery between PPV and PPV-SB [25]. The addition of a scleral buckle is particularly recommended if the edge of the GRT is not inverted and in cases of PVR [2]. In other circumstances, the role of scleral buckle is still controversial.
To our knowledge, our study is the only large population study that directly compares the anatomical and functional outcomes of retinal detachment associated with a giant retinal tear with simple RRD.
Limitations
This is a retrospective, single center study. We describe 39 patients with GRT in this cohort, which was insufficient to build a multivariable model examining rates of SSAS within this group only. Given the small number of patients with GRT, the effect of GRT on SSAS yields a wide confidence interval encompassing the threshold of OR = 1, even though the p-value is deemed statistically significant (OR 0.422, 95% CI 0.190–1.071; p = 0.047). We also could not study specific interventions to improve success rates in GRT-RD including using multiple linear regression for final VA given the small sample size of GRT.
Outcome data was collected until final follow-up. Rates of outcomes such as cataract development and recurrence of detachment could however be affected by total length of follow-up, which was restricted to 3 months in several patients.
Conclusion
In conclusion, our retrospective cohort study highlights that the initial presentation and clinical course of RD patients with GRT may differ from simple RRD patients. Management of GRT-RD also remains more challenging with potentially less favorable anatomical and functional outcomes compared to RRD. When adjusting for other preoperative risk factors, GRT remained significantly associated with reduced SSAS compared to simple RRD. Standard PPV and combined PPV-SB showed similar surgical outcomes in repairing the RD associated with a giant retinal tear. More studies are needed to optimize surgical outcomes in GRT-RD.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BCVA:
-
Best-corrected visual acuity
- C3F8 :
-
Perfluoropropane
- CI:
-
Confidence intervals
- GRT:
-
Giant retinal tear
- GRT-RD:
-
Giant retinal tear-associated retinal detachment
- logMAR:
-
Logarithm of the minimum angle of resolution
- OCT:
-
Optical coherence tomography
- OR:
-
Odds ratio
- PPV:
-
Pars plana vitrectomy
- PPV-SB:
-
Pars plana vitrectomy with scleral buckle
- PVD:
-
Posterior vitreous detachment
- PVR:
-
Proliferative vitreoretinopathy
- RD:
-
Retinal detachment
- RRD:
-
Rhegmatogenous retinal detachment
- SB:
-
Scleral buckle
- SD:
-
Standard deviation
- SF6:
-
Sulfur hexafluoride
- SSAS:
-
Single surgery anatomical success
- VA:
-
Visual acuity
References
Schepens CL, Dobble JG, McMeel JW. Retinal detachments with giant breaks: preliminary report. Trans Am Acad Ophthalmol Otolaryngol. 1962;66:471–9.
Berrocal MH, Chenworth ML, Acaba LA. Management of giant retinal tear detachments. J Ophthalmic Vis Res. 2017;12(1):93–7.
Chou SC, Yang CH, Lee CH, Yang CM, Ho TC, Huang JS, et al. Characteristics of primary rhegmatogenous retinal detachment in Taiwan. Eye. 2007;21(8):1056–61.
Freeman HM. Fellow eyes of giant retinal breaks. Trans Am Ophthalmol Soc. 1978;76:343–82.
Malbran E, Dodds RA, Hulsbus R, Charles DE, Buonsanti JL, Adrogué E. Retinal break type and proliferative vitreoretinopathy in nontraumatic retinal detachment. Graefes Arch Clin Exp Ophthalmol. 1990;228(5):423–5.
Yorston DB, Wood ML, Gilbert C. Retinal detachment in East Africa. Ophthalmology. 2002;109(12):2279–83.
Ting DSW, Foo VHX, Tan TE, Sie NM, Wong CW, Tsai ASH, et al. 25-years trends and risk factors related to surgical outcomes of giant retinal tear-rhegmatogenous retinal detachments. Sci Rep. 2020;10(1):5474.
Hocaoglu M, Karacorlu M, Ersoz MG, Muslubas IS, Arf S. Vitrectomy with silicone oil tamponade for retinal detachment associated with giant retinal tears: favourable outcomes without adjuvant scleral buckling. Acta Ophthtalmol. 2019;97(2):e271–6.
Tiew S, Lim C, Sivagnanasithiyar T. Using an excel spreadsheet to convert Snellen visual acuity to LogMAR visual acuity. Eye. 2020;34(11):2148–9.
Scott IU, Schein OD, West S, Bandeen-Roche K, Enger C, Folstein MF. Functional status and quality of life measurement among ophthalmic patients. Arch Ophthalmol. 1994;112(3):329.
Gregori NZ, Feuer W, Rosenfeld PJ. Novel method for analyzing snellen visual acuity measurements. Retina. 2010;30(7):1046–50.
Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and cox regression. Am J Epidemiol. 2007;165(6):710–8.
Mitry D, Singh J, Yorston D, Siddiqui MAR, Wright A, Fleck BW, et al. The predisposing pathology and clinical characteristics in the Scottish retinal detachment study. Ophthalmology. 2011;118(7):1429–34.
Ambresin A, Wolfensberger TJ, Bovey EH. Management of giant retinal tears with vitrectomy, internal tamponade, and peripheral 360 degrees retinal photocoagulation. Retina. 2003;23(5):622–8.
Freeman HM, Castillejos ME. Current management of giant retinal breaks: results with vitrectomy and total air fluid exchange in 95 cases. Trans Am Ophthalmol Soc. 1981;79:89–102.
Ghosh YK, Banerjee S, Savant V, Kotamarthi V, Benson MT, Tyagi AK. Surgical treatment and outcome of patients with giant retinal tears. Eye. 2004;18(10):996–1000.
Goezinne F, Heij ECL, Berendschot TTJM, Gast STJM, Liem ATA, Lundqvist IL, et al. Low redetachment rate due to encircling scleral buckle in giant retinal tears treated with vitrectomy and silicone oil. Retina. 2008;28(3):485–92.
Lee SY, Ong SG, Wong DW, Ang CL. Giant retinal tear management: an Asian experience. Eye. 2009;23(3):601–5.
Norton EW, Aaberg T, Fung W, Curtin VT. Giant retinal tears. I. Clinical management with intravitreal air. Am J Ophthalmol. 1969;68(6):1011–21.
Sirimaharaj M, Balachandran C, Chan WC, Hunyor AP, Chang AA, Gregory-Roberts J, et al. Vitrectomy with short term postoperative tamponade using perfluorocarbon liquid for giant retinal tears. Br J Ophthalmol. 2005;89(9):1176–9.
Wolfensberger TJ, Aylward GW, Leaver PK. Prophylactic 360 degrees cryotherapy in fellow eyes of patients with spontaneous giant retinal tears. Ophthalmology. 2003;110(6):1175–7.
Shunmugam M, Ang GS, Lois N. Giant retina tears. Surv Ophthalmol. 2014;59(2):192–216.
Ang GS, Townend J, Lois N. Epidemiology of giant retinal tears in the United Kingdom: the British Giant Retinal Tear Epidemiology Eye Study (BGEES). Invest Ophthalmol Vis Sci. 2010;51(9):4781–7.
Rodriguez M, Lin J, Townsend JH, Smiddy WE, Albini TA, Berrocal AM, et al. Giant retinal tears: clinical features and outcomes of vitreoretinal surgery at a university teaching hospital (2011–2017). Clin Ophthalmol. 2018;12(12):2053–8.
Taleb EA, Nagpal MP, Mehrotra NS, Bhatt K, Goswami S, Noman A. Giant retinal tear retinal detachment etiologies, surgical outcome, and incidence of recurrent retinal detachment after silicone oil removal. Oman J Ophthalmol. 2020;13(3):117–22.
Acknowledgements
Not applicable.
Funding
The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by JG, MH, EY and AD. The first draft of the manuscript was written by JG, MH and EY and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study adheres to the tenets of the Declaration of Helsinki. The study was examined by the Institutional Review Board of the Centre hospitalier universitaire de Québec - Université Laval which waived the necessity to review the study, (Reference number: 2020-4798) and individual patient consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Garneau, J., Hébert, M., You, E. et al. Anatomical and functional outcomes of retinal detachment associated with nontraumatic giant retinal tears compared to simple rhegmatogenous retinal detachment. Int J Retin Vitr 8, 65 (2022). https://doi.org/10.1186/s40942-022-00407-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40942-022-00407-y