Abstract
Background
rhBMP-2 is regarded as the most potent osteoinductive growth factor, and it has been used in the oral cavity with different carriers. The purpose of this study is to evaluate the bone-regenerative effect of rhBMP-2 delivered with different carrier systems through three-dimensional cone beam computed tomography analysis.
Method
A total of 112 patients underwent oral surgery with rhBMP-2 application (Group 1, n = 53) or without rhBMP-2 application (Group 2, n = 59). Group 1 was divided into 3 groups according to carriers, rhBMP-2 with allograft (Group 1–1, n = 34), rhBMP-2 with xenograft (Group 1–2, n = 5), and rhBMP-2 with absorbable collagen sponge (Group 1–3, n = 14). Cone beam computed tomography scans were taken before surgery (T0) 6 months after surgery (T1). The volume of defects was measured through the three-dimensional image analysis tool.
Results
The average bone regeneration rate of Group 1 was significantly greater than that of Group 2. Within Group 1, the group that used allograft as a carrier (Group 1–1) showed significantly higher bone regeneration rates than the group that used absorbable collagen sponge as a carrier (Group 1–3).
Conclusion
The use of rhBMP-2 after oral surgery results in a superior bone regeneration rate compared to not using rhBMP-2, and its efficacy depends on the carriers it is used with. Allograft affects bone regeneration more than absorbable collagen sponge when it is carried with rhBMP-2. Therefore, the appropriate use of rhBMP-2 with suitable bone grafting materials is useful for promoting postoperative bone regeneration in oral surgery.
Similar content being viewed by others
Background
Bone morphogenetic proteins (BMPs) regulate cellular processes such as differentiation, proliferation, and morphogenesis [1]. They are present within the bone and play a crucial role as inducers of bone formation in cases of bone fractures and bone defects caused by trauma or diseases [2]. The BMP family comprises approximately 40 known members, among which BMP-2 has been identified as the most potent stimulator of bone healing and bone formation [3, 4].
BMPs are present in small amounts within bone and do not exhibit species-specific characteristics. Therefore, extraction of BMPs from both homologous and heterologous sources has been extensively attempted to harness their osteogenic abilities. These proteins have been isolated from the mammalian bone, osteosarcoma, and dental pulp, among other sources [5, 6]. However, the extraction and purification of BMPs are complex and provide a limited yield [7]. Recent advancements in genetic engineering have made it possible to produce large quantities of BMPs through genetic manipulation.
More than 20 different types of recombinant human BMPs (rhBMPs) have been synthesized through genetic manipulation [8, 9]. These proteins can induce cartilage and bone formation and create a foundational environment for functional bone marrow formation during bone formation [10]. BMP-2 directly promotes nerve cell growth and induces chondrocyte and osteoblast differentiation. The differentiation of surrounding immature mesenchymal cells into osteogenic cells enables stimulation and regulation of bone formation [11,12,13].
Although BMPs have been commercialized and applied in clinical settings, they are currently available in liquid form. This poses challenges as BMPs alone are difficult to manipulate, have low stability, and tend to quickly diffuse and be absorbed and degraded in the body, making it difficult to induce bone formation effectively [14]. Therefore, the use of delivery systems is essential to overcome these limitations.
Carriers have been designed to control or slow down the release of BMPs while maintaining their biological activity, allowing for a sustained release at the desired time for bone formation and mitigating the initial burst release effect [15].
BMP carriers should be biocompatible, easily manipulated, and biodegradable in the body, without causing adverse tissue reactions. They should allow easy replacement with newly formed bone, maintain space for a specific period, and gradually release BMPs [16]. Through this, carriers should provide maximum opportunities for BMPs to come into contact with the surrounding cells [17, 18]. Various materials with these characteristics are being researched, and the most commonly used carriers include absorbable collagen sponge (ACS) and synthetic bone materials, such as hydroxyapatite or β-tricalcium phosphate, which may be used either alone or in combination.
Superior bone regeneration has been observed on applying BMPs with various carriers than that achieved without BMPs. However, the carrier demonstrating the most effective bone regeneration has not yet been conclusively identified [19, 20].
Therefore, we aimed to assess the effect of applying rhBMP-2 with different carriers, such as allografts, xenografts, and ACS, on bone regeneration by measuring the preoperative and postoperative volumes of maxillofacial bone defects through cone beam computed tomography (CBCT).
Methods
Patients
We included 112 patients diagnosed with cysts, benign tumors, or osteomyelitis of the jaw who underwent oral surgery at Ajou University Dental Hospital between 2019 and 2022. All patients were followed up for more than 6 months. Patients with uncontrolled systemic disease, infection, or lesion recurrence after surgery were excluded.
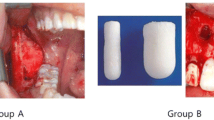
The patients who received rhBMP-2 (Novosis®, Dae-woong Bio, Korea) with different carriers at the defect site were assigned to the experimental group (Group 1, n = 53). Group 1 was divided into three sub-group according to the carrier used: allograft (Allomix®, CGBIO, Korea) (Group 1–1, n = 34), xenograft (The Graft®, PurgoBiologics, Korea) (Group 1–2, n = 5), and ACS (Ateloplug®, Hyundae Bioland, Korea) (Group 1–3, n = 14). Patients who did not receive rhBMP-2 were included in the control group (Group 2, n = 59). Group 2 included patients who received bone grafts (3 patients with allograft, 40 patients with xenograft) or ACS (13 patients) as well as those who received no material (3 patients).
This study was conducted with the approval of the Institutional Review Board of Ajou University Hospital (IRB No: AJOUIRB-DB-2023–201).
CBCT examination and measurements
CBCT (Dinnova3, HDX, Korea) was performed preoperatively (T0) and at 6 months postoperatively (T1) at Ajou University Dental Hospital using the following imaging condition: 80kVp, 7.0 mA, and scan time for 20 s. The slice thickness was 0.3 mm, and the distance between slices was 1.0 mm. The digital CBCT scans were exported as Digital Imaging and Communications in Medicine (DICOM) format files to InVivo Dental Application version 5 (Anatomage, San Jose, CA).
Bone regeneration rate analysis
InVivo Dental Application version 5 was used to measure the volume (Fig. 1). After determining the regions of each defect, the functionality selects only the pixels within the range of the hounsfield unit (HU) specified by the user. This enabled the calculation of volume for the selected pixels (Fig. 2). Lesions with a density of -1000–200 HU were considered defects [21].
To minimize visual errors during volumetric measurements, the position of the patient’s head on the CBCT image was reoriented before measurement. Reorientation was performed in the coronal plane, and a line connecting both orbitales was used. In the horizontal plane, a line connecting the Frankfort horizontal plane passing through the orbitale and porion was used. In the sagittal plane, a line connecting the anterior and posterior nasal spines (PNS) was used.
The bone regeneration rate was calculated based on the preoperative and postoperative defect volumes as follows:
The measurements were performed twice with a 2-week washout period.
Statistical analysis
A single investigator performed the measurements twice to minimize methodological errors. The Kolmogorov-Smirnova test was performed to test the normality of data. The Kruskal–Wallis, Mann–Whitney tests, and Bonferroni correction were performed to evaluate the bone regenerative rate in each group. Statistical significance was set at p < 0.05. SPSS Statistics version 25.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
Result
The average age of all patients was 42.24 years, with 52 males and 60 females. In the experimental group where rhBMP-2 was used, there were a total of 53 patients with an average age of 46.47 years, including 28 males and 25 females. In the control group without the use of rhBMP-2, there were a total of 59 patients with an average age of 38.29 years, including 24 males and 35 females.
All patients showed a decrease in the volume of the defect after surgery compared to before surgery. The bone regeneration rate in the experimental group, where rhBMP-2 was used, ranged from a minimum of 30.82% to a maximum of 89.38%, with an average of 66.28%. In the control group without the use of rhBMP-2, the bone regeneration rate ranged from a minimum of 16.72% to a maximum of 88.14%, with an average of 57.79%. The bone regeneration rate in the experimental group using rhBMP-2 was significantly higher compared to the control group without rhBMP-2 (Table 1, Fig. 3).
In the experimental group, the bone regeneration rate of Group 1–1 (using allograft as a carrier) ranged from a minimum of 60.22% to a maximum of 89.38%, with an average of 70.53%. The bone regeneration rate of Group 1–2 (using xenograft as a carrier) ranged from a minimum of 60.43% to a maximum of 70.43%, with an average of 65.13%. The bone regeneration rate of Group 1–3 (using ACS as a carrier) ranged from a minimum of 30.82% to a maximum of 85.92%, with an average of 56.36% (Table 2).
Group 1–1 which used allograft as a carrier showed a significantly higher bone regeneration rate compared to Group 1–3, which used ACS as a carrier (p = 0.003). However, there was no statistically significant difference in the bone regeneration rate between Group 1–2, which used xenograft as a carrier, and Group 1–3 (p = 0.803). Additionally, there was no statistically significant difference in the bone regeneration rate between Group 1–2 and Group 1–3 (p = 0.997) (Table 3, Fig. 4).
Discussion
rhBMP-2 is a growth factor with excellent osteoinductive properties. It has therefore been actively studied [22, 23] and has received attention as a treatment method for bone defects. rhBMP-2 should be used with a carrier for maximum effectiveness, and the choice of carrier can influence the effects of rhBMP-2 [24].
The ideal carrier for rhBMP-2 should be biocompatible and capable of degrading at an appropriate rate while being replaced by newly formed bone. It should have porosity to allow the ingrowth of new blood vessels and cells. Most importantly, it should maintain BMP activity and enable controlled release at an appropriate rate [25, 26].
Although several studies have been conducted to identify ideal carriers, most have focused on animal models or histological analyses [27,28,29]. Therefore, in this study, we aimed to investigate the bone regeneration rate when rhBMP-2 is applied with various carriers through a three-dimensional analysis with CBCT. This approach allowed the identification of the most effective carrier for bone regeneration among allograft, xenograft, and ACS.
The present results revealed a significantly higher average bone regeneration rate when rhBMP-2 was applied to the site of bone defect after surgery than when rhBMP-2 was not applied. This finding aligns with those of previous studies demonstrating the osteogenic potential of rhBMP-2 [30, 31]. Furthermore, the choice of carrier material for rhBMP-2 also influenced the bone regeneration rate, which was significantly higher on using allograft bone as the carrier as compared with that on using ACS.
However, it is important to note that this was a retrospective analysis of patients who underwent surgery. The decision to use rhBMP-2 or the choice of carrier material was based on factors, such as the number of remaining walls in the bone defect, diagnosis, and patient age. In this study, in all patients with osteomyelitis, ACS with rhBMP-2 and carrier was applied to the area of the defect after surgery. In the case of osteomyelitis, rhBMP-2 was used for bone regeneration after removal of the sequestrum, and ACS was used together to reduce the risk of infection. For all other patients, there was no preference for a specific repair method. The number of compromised walls in patients with osteomyelitis was higher than that of patients with other diagnoses, and the existing defect volume of group 1–3 was also higher than that of other groups. These factors are potentially contributing to the lower bone regeneration rates in Group 1–3 compared to Group 1–1 and Group 1–2. Therefore, this study could not be conducted in a completely randomized manner, which may have influenced the bone regeneration rate findings (Tables 4 and 5).
Furthermore, there was a significant disparity in the sample size of the sub-group that received allografts as carriers (n = 34) and sub-group that received xenografts (n = 5). The small sample size of the xenograft group may have prevented a meaningful comparison of the two groups. Further studies with a larger sample are necessary to enable appropriate comparisons between these groups and obtain a comprehensive understanding.
However, this study has significant value because the CBCT scans of actual patients were evaluated preoperatively and at the 6-month follow-up postoperatively. This study provides meaningful insights into the effectiveness of rhBMP-2 in the clinical setting.
Conclusion
This study aimed to investigate the impact of using rhBMP-2 with various carriers on bone regeneration in maxillofacial defects. The bone regeneration rate was calculated through a CBCT analysis computed to evaluate the effects of rhBMP-2. The use of rhBMP-2 after oral surgery resulted in a superior bone regeneration rate compared to that achieved without rhBMP-2, and its efficacy depended on the carrier used. Allograft carriers affected bone regeneration more than the ACS carrier. Therefore, the appropriate use of rhBMP-2 with suitable bone-grafting materials on CBCT analysis is useful to promote postoperative bone regeneration in oral surgery.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMPs:
-
Bone morphogenetic proteins
- rhBMPs:
-
Recombinant human bone morphogenetic proteins
- ACS:
-
Absorbable collagen sponge
- CBCT:
-
Cone beam computed tomography
- HU:
-
Hounsfield unit
- PNS:
-
Posterior nasal spine
References
Urist MR, DeLange RJ, Finerman GA (1983) Bone cell differentiation and growth factors. Science 220:680–686. https://doi.org/10.1126/science.6403986
Wang EA, Rosen V, D’Alessandro JS, Bauduy M, Cordes P, Harada T, Israel DI, Hewick RM, Kerns KM, LaPan P et al (1990) Recombinant human bone morphogenetic protein induces bone formation. Proc Natl Acad Sci U S A 87:2220–2224. https://doi.org/10.1073/pnas.87.6.2220
Deschaseaux F, Sensébé L, Heymann D (2009) Mechanisms of bone repair and regeneration. Trends Mol Med 15:417–429. https://doi.org/10.1016/j.molmed.2009.07.002
Triplett RG, Nevins M, Marx RE, Spagnoli DB, Oates TW, Moy PK, Boyne PJ (2009) Pivotal, randomized, parallel evaluation of recombinant human bone morphogenetic protein-2/absorbable collagen sponge and autogenous bone graft for maxillary sinus floor augmentation. J Oral Maxillofac Surg 67:1947–1960. https://doi.org/10.1016/j.joms.2009.04.085
Reddi AH (1997) Bone morphogenetic proteins: an unconventional approach to isolation of first mammalian morphogens. Cytokine Growth Factor Rev 8:11–20. https://doi.org/10.1016/s1359-6101(96)00049-4
Rosen V, Thies RS (1992) The BMP proteins in bone formation and repair. Trends Genet 8:97–102. https://doi.org/10.1016/0168-9525(92)90197-c
Langer R, Vacanti JP (1993) Tissue engineering. Science 260:920–926. https://doi.org/10.1126/science.8493529
Wozney JM, Rosen V, Celeste AJ, Mitsock LM, Whitters MJ, Kriz RW, Hewick RM, Wang EA (1988) Novel regulators of bone formation: molecular clones and activities. Science 242:1528–1534. https://doi.org/10.1126/science.3201241
Toriumi DM, Kotler HS, Luxenberg DP, Holtrop ME, Wang EA (1991) Mandibular reconstruction with a recombinant bone-inducing factor. Functional, histologic, and biomechanical evaluation. Arch Otolaryngol Head Neck Surg 117:1101–1112. https://doi.org/10.1001/archotol.1991.01870220049009
Wozney JM (2002) Overview of bone morphogenetic proteins. Spine (Phila Pa 1976) 27:S2–S8. https://doi.org/10.1097/00007632-200208151-00002
Sampath TK, Maliakal JC, Hauschka PV, Jones WK, Sasak H, Tucker RF, White KH, Coughlin JE, Tucker MM, Pang RH et al (1992) Recombinant human osteogenic protein-1 (hOP-1) induces new bone formation in vivo with a specific activity comparable with natural bovine osteogenic protein and stimulates osteoblast proliferation and differentiation in vitro. J Biol Chem 267:20352–20362. https://doi.org/10.1016/S0021-9258(19)88709-4
Yasko AW, Lane J, Fellinger E, Rosen V, Wozney J, Wang E (1992) The healing of segmental bone defects, induced by recombinant human bone morphogenetic protein (rhBMP-2). A radiographic, histological, and biomechanical study in rats. J Bone Joint Surg Am 74:659–670
Miyamoto S, Takaoka K, Ono K (1993) Bone induction in monkeys by bone morphogenetic protein. A trans-filter technique. J Bone Joint Surg Br 75:107–110. https://doi.org/10.1302/0301-620x.75b1.8421005
Hong SJ, Kim CS, Han DK, Cho IH, Jung UW, Choi SH, Kim CK, Cho KS (2006) The effect of a fibrin-fibronectin/beta-tricalcium phosphate/recombinant human bone morphogenetic protein-2 system on bone formation in rat calvarial defects. Biomaterials 27:3810–3816. https://doi.org/10.1016/j.biomaterials.2006.02.045
Carreira AC, Lojudice FH, Halcsik E, Navarro RD, Sogayar MC, Granjeiro JM (2014) Bone morphogenetic proteins: facts, challenges, and future perspectives. J Dent Res 93:335–345. https://doi.org/10.1177/0022034513518561
Sigurdsson TJ, Nygaard L, Tatakis DN, Fu E, Turek TJ, Jin L, Wozney JM, Wikesjö UM (1996) Periodontal repair in dogs: evaluation of rhBMP-2 carriers. Int J Periodontics Restorative Dent 16:524–537
Burg KJ, Porter S, Kellam JF (2000) Biomaterial developments for bone tissue engineering. Biomaterials 21:2347–2359. https://doi.org/10.1016/s0142-9612(00)00102-2
Friess W (2000) Drug delivery systems based on collagen. Shaker Verlag GmbH, Aachen
Ahn SH, Kim CS, Suk HJ, Lee YJ, Choi SH, Chai JK, Kim CK, Han SB, Cho KS (2003) Effect of recombinant human bone morphogenetic protein-4 with carriers in rat calvarial defects. J Periodontol 74:787–797. https://doi.org/10.1902/jop.2003.74.6.787
Kim CS, Choi SH, Choi BK, Chai JK, Park JB, Kim CK, Cho KS (2002) The effect of recombinant human bone morphogenetic protein-4 on the osteoblastic differentiation of mouse calvarial cells affected by Porphyromonas gingivalis. J Periodontol 73:1126–1132. https://doi.org/10.1902/jop.2002.73.10.1126
Lamba R, McGahan JP, Corwin MT, Li CS, Tran T, Seibert JA, Boone JM (2014) CT Hounsfield numbers of soft tissues on unenhanced abdominal CT scans: variability between two different manufacturers’ MDCT scanners. AJR Am J Roentgenol 203:1013–1020. https://doi.org/10.2214/ajr.12.10037
Carragee EJ, Hurwitz EL, Weiner BK (2011) A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. Spine J 11:471–491. https://doi.org/10.1016/j.spinee.2011.04.023
Gutwald R, Haberstroh J, Stricker A, Rüther E, Otto F, Xavier SP, Oshima T, Marukawa E, Seto I, Enomoto S, Hoogendijk CF, Schmelzeisen R, Sauerbier S (2010) Influence of rhBMP-2 on bone formation and osseointegration in different implant systems after sinus-floor elevation. An in vivo study on sheep. J Craniomaxillofac Surg 38:571–579. https://doi.org/10.1016/j.jcms.2010.02.010
Dimitriou R, Giannoudis PV (2005) Discovery and development of BMPs. Injury 36(Suppl 3):S28–S33. https://doi.org/10.1016/j.injury.2005.07.031
Kirker-Head CA (2000) Potential applications and delivery strategies for bone morphogenetic proteins. Adv Drug Deliv Rev 43:65–92. https://doi.org/10.1016/s0169-409x(00)00078-8
Brekke JH, Toth JM (1998) Principles of tissue engineering applied to programmable osteogenesis. J Biomed Mater Res 43:380–398. https://doi.org/10.1002/(SICI)1097-4636(199824)43:4<380::AID-JBM6>3.0.CO;2-D
Han DK, Kim CS, Jung UW, Chai JK, Choi SH, Kim CK, Cho KS (2005) Effect of a fibrin-fibronectin sealing system as a carrier for recombinant human bone morphogenetic protein-4 on bone formation in rat calvarial defects. J Periodontol 76:2216–2222. https://doi.org/10.1902/jop.2005.76.12.2216
Hyun SJ, Han DK, Choi SH, Chai JK, Cho KS, Kim CK, Kim CS (2005) Effect of recombinant human bone morphogenetic protein-2, -4, and -7 on bone formation in rat calvarial defects. J Periodontol 76:1667–1674. https://doi.org/10.1902/jop.2005.76.10.1667
Kim CS, Kim JI, Kim J, Choi SH, Chai JK, Kim CK, Cho KS (2005) Ectopic bone formation associated with recombinant human bone morphogenetic proteins-2 using absorbable collagen sponge and beta tricalcium phosphate as carriers. Biomaterials 26:2501–2507. https://doi.org/10.1016/j.biomaterials.2004.07.015
Sigurdsson TJ, Fu E, Tatakis DN, Rohrer MD, Wikesjö UM (1997) Bone morphogenetic protein-2 for peri-implant bone regeneration and osseointegration. Clin Oral Implants Res 8:367–374. https://doi.org/10.1034/j.1600-0501.1997.080503.x
Barboza EP, Duarte ME, Geolás L, Sorensen RG, Riedel GE, Wikesjö UM (2000) Ridge augmentation following implantation of recombinant human bone morphogenetic protein-2 in the dog. J Periodontol 71:488–496. https://doi.org/10.1902/jop.2000.71.3.488
Acknowledgements
None.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SIS carried out the surgical treatment of the patient and contributed to the conception of the report and critical revising. JIS and JHL participated in the treatment, collection of the data, and drafting of the manuscript. JIS and WMJ performed the statistical analysis. SIS and JKL contributed to the critical revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ajou University School of Medicine Institutional Review Board (IRB No: AJOUIRB-DB-2023–201) approved the study protocol.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seo, J.I., Lim, J.H., Jo, W.M. et al. Effects of rhBMP-2 with various carriers on maxillofacial bone regeneration through computed tomography evaluation. Maxillofac Plast Reconstr Surg 45, 40 (2023). https://doi.org/10.1186/s40902-023-00405-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40902-023-00405-6