Abstract
Background
This study evaluated the pharyngeal airway space changes up to 1 year after bilateral sagittal split osteotomy mandibular setback surgery and bimaxillary surgery with maxillary posterior impaction through three-dimensional computed tomography analysis.
Methods
A total of 37 patients diagnosed with skeletal class III malocclusion underwent bilateral sagittal split osteotomy setback surgery only (group 1, n = 23) or bimaxillary surgery with posterior impaction (group 2, n = 14). Cone-beam computed tomography scans were taken before surgery (T0), 2 months after surgery (T1), 6 months after surgery (T2), and 1 year after surgery (T3). The nasopharynx (Nph), oropharynx (Oph), hypopharynx (Hph) volume, and anteroposterior distance were measured through the InVivo Dental Application version 5.
Results
In group 1, Oph AP, Oph volume, Hph volume, and whole pharynx volume were significantly decreased after the surgery (T1) and maintained. In group 2, Oph volume and whole pharynx volume were decreased (T2) and relapsed at 1 year postoperatively (T3).
Conclusion
In class III malocclusion patients, mandibular setback surgery only showed a greater reduction in pharyngeal airway than bimaxillary surgery at 1 year postoperatively, and bimaxillary surgery was more stable in terms of airway. Therefore, it is important to evaluate the airway before surgery and include it in the surgical plan.
Similar content being viewed by others
Background
Many patients with skeletal class III malocclusion have esthetic and functional problems, and orthognathic surgery accompanying bilateral sagittal split osteotomy (BSSRO) setback surgery is administered to improve them. This surgery provides satisfactory results to patients by improving the mastication, pronunciation, esthetics, and psychological factors of the patient by changing the skeletal position of the mandible alone or both mandible and maxilla.
Orthognathic surgery affects not only hard tissue but also soft tissue and affects the stomatognathic system overall. The oropharyngeal complex is composed of the hyoid bone and the muscles connected to it, and is anatomically and functionally related to the mandible, resulting in changes after orthognathic surgery with mandible movement. When the mandible is moved backward by surgery, the tongue, hyoid bone, and muscles attached are located posterior to its original position, and as a result, the airway volume is narrowed [1,2,3,4,5,6,7,8]. Many previous studies have shown that mandible setback surgery narrows the pharyngeal airway [4, 9,10,11]. Several studies have reported that postoperative obstructive sleep apnea (OSA) occurred as a result [4, 6, 9, 11, 12]. On the other hand, in the case of BSSRO setback surgery with Le Fort I osteotomy, there are reports that the decrease in pharyngeal airway volume is less than in patients who underwent mandibular setback surgery only, and there are some studies that the anteroposterior (AP) dimension is rather increased in the upper pharyngeal airway after the surgery [13,14,15].
In the previous study, two-dimensional analysis using cephalometric radiographs was performed to investigate the change of pharyngeal airway, but there were limitations in the analysis of the three-dimensional (3D) pharyngeal airway space or volume [16, 17]. Cone-beam computed tomography (CBCT) is a 3D image that is very useful for preoperative diagnosis, operation planning, and evaluation of postoperative results. It also provides high quality while reducing scanning time and irradiation compared to conventional computed tomography (CT). In addition, a CT image is useful for evaluating pharyngeal airway including both hard tissue and soft tissue, and it is possible to visualize a 3D image to help intuitive understanding. Nowadays, as many CT scans and programs are developed, there are some studies evaluating the volumetric evaluation of the airway after surgery [12, 18,19,20,21,22]. Most of them were limited to only BSSRO setback surgery, and there were not many cases that the volume change was observed regularly until 1 year.
From our experience, airway narrowing was seen on the radiograph in some patients after mandibular setback surgery and some patients complained of airway-related symptoms such as snoring immediately after the surgery. Over time, these symptoms subsided and it was expected that there would be changes in the airway over time. In particular, in the case of bimaxillary surgery with posterior impaction, the change in the airway was expected to show a different pattern because the mandible was not simply positioned posteriorly but the maxilla was rotated clockwise. Accordingly, we hypothesized that the three-dimensional volume and anteroposterior distance of the airway would be different over time depending on the surgical methods.
The purpose of our study was to evaluate the pharyngeal airway space changes up to 1 year after BSSRO surgery with or without Le Fort I osteotomy through 3D CT analysis.
Materials and methods
Patients
From February 2014 to April 2019, 37 patients (19 men, 18 women; mean age 23.2 ± 5.47 years) diagnosed with skeletal class III malocclusion and who underwent BSSRO setback surgery or bimaxillary surgery by the same operator at the Ajou University School of Medicine (Suwon, Korea) were included in this study (Table 1). All the patients were followed for more than 1 year and pre- and postorthodontic treatments were provided. Patients who had craniofacial syndromes, such as cleft lip and palate, cranial trauma, and upper respiratory lesions, or who underwent other surgery such as genioplasty were excluded.
Patients were divided into two groups: (1) 1 jaw surgery patients (BSSRO setback surgery only), (2) 2 jaw surgery patients (Le Fort I osteotomy with posterior impaction and BSSRO setback surgery). The surgical method was different for group 1 and group 2. In the case of group 1, BSSRO setback surgery was performed, followed by rigid fixation. In group 2, after Le Fort I osteotomy, the maxilla was moved to the desired position, rigid fixation was performed, and mandible BSSRO setback surgery was performed as in group 1. After surgery, all patients had to wear wafers for 2–4 weeks to stabilize occlusion, and postorthodontic treatment was performed afterwards. Table 1 shows the amount of surgical movement in each group.
Ajou University School of Medicine Institutional Review Board approved the study protocol (Approval No. AJIRB-MED-MDB-20-078).
CBCT examination and measurements
CBCT scans were taken before surgery (T0), 2 months after surgery (T1), 6 months after surgery (T2), and 1 year after surgery (T3). During a CT scan, in order to have a reproducible posture, patients were asked to take a natural head position. Patients were asked to stand and stare at the front mirror, and the lips, chin, and masticatory muscles were relaxed to take a reproducible posture.
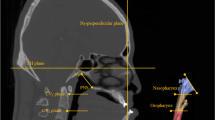
CBCT (Dinnova3; HDX, Seoul, Korea) of Ajou University Dental Hospital was used, and the imaging conditions were 80 kVp, 7.0 mA, and scan time for 20 s. The slice thickness was 0.3 mm and the distance between slices was 1.0 mm. CT digital image files were exported using the Digital Imaging and Communications in Medicine (DICOM) format and imported into the InVivo Dental Application version 5 (Anatomage, San Jose, CA, USA). The landmarks, reference planes, and measurement points used in this study are as follows (Tables 2 and 3). Since the measured value varies according to the head position, re-orientation was performed by setting the nasion as the origin point, the Frankfort horizontal plane passing through the orbitale and the porion as the horizontal reference plane, and the sella vertical plane passing through the sella and basion as the sagittal reference plane.
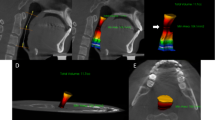
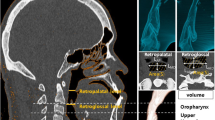
The upper airway space is surrounded by soft tissue and can be changed with surgery, dividing the upper airway space based on the plane passing through the cervical vertebra, CV1, CV2, and CV4 (Table 2). The airway space from the top of the pharynx to the CV4 plane is defined as the whole pharynx, and the nasal cavity and oral cavity are excluded. The pharynx was divided into subdivisions based on the CV1 plane and the CV2 plane, and defined as nasopharynx (Nph), oropharynx (Oph), and hypopharynx (Hph) from above (Table 3, Fig. 1). It was measured through the InVivo Dental Application version 5 (Fig. 2).
Pharyngeal airway division and measurements. a The airway space divided into three areas based on reference planes. (1) a plane parallel to the FH plane passing through CV1; (2) a plane parallel to the FH plane passing through CV2; (3) a plane parallel to the FH plane passing through CV4; A, the nasopharyngeal volume; B, oropharyngeal volume; C, hypopharyngeal volume; (a) nasopharyngeal antero-posterior distance; (b) oropharyngeal antero-posterior distance; (c) hypopharyngeal anteroposterior distance. b Measurement of SV-B. (4) sella vertical plane; (d) the distance from the sella vertical plane to the B point. PNS posterior nasal spine
Statistical analysis
Methodological errors in the measurement were minimized by double recording of the same investigator. The Shapiro-Wilk test was performed for the normalization test. A paired t-test was used to evaluate postoperative changes of pharyngeal space and relapse in each group. An independent t-test was used to determine the difference between groups. Probability values less than 0.05 were deemed statistically significant. SPSS Statistics version 23.0 software (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
Results
The measurements and volumes before surgery (T0), 2 months after surgery (T1), 6 months after surgery (T2), and 1 year after surgery (T3) in group 1 are shown in Table 4. Data for group 2 are shown in Table 5 and comparisons between groups are shown in Table 6. The mean of the mandibular setback amount was 4.85 ± 4.34 mm in group 1 and 6.81 ± 5.14 mm in group 2. The mean change of the mandibular plane angle was 3.54 ± 4.56° in group 1 and 2.17 ± 4.24° in group 2. Maxillary posterior impaction was done in group 2 with 4.23 ± 3.14 mm posterior nasal spine upward and 0.81 ± 2.11 mm advance of the anterior nasal spine (Table 1).
Nasopharyngeal airway change
In group 1, the average Nph AP was 13.35 mm preoperatively, and significantly decreased by 0.96 to 12.39 mm at 2 months after surgery (p < 0.05). It gradually increased and relapsed to 12.48 mm at 1 year after surgery (T3) without difference from T0 (p > 0.05). The mean preoperative Nph volume (Nph vol) was measured to be 6.23 cm3 and was 5.53 cm3 at 1 year postoperatively, with no difference before and after surgery (p > 0.05) (Table 4).
In group 2, the Nph AP was 13.24 mm, which was similar to the preoperative average of group 1, and 12.58 mm at 1 year after surgery (T3) without difference from T0 (p > 0.05). In group 2, the Nph vol was 7.43 cm3 before surgery (T0), and no significant change was observed until 6 months after surgery (p > 0.05). Nph vol significantly increased during the T2–T3 period (p < 0.01) and relapsed to 7.76 cm3 at 6 months postoperatively (T0–T3, p > 0.05). (Table 5).
Oropharyngeal airway change
In group 1, the average preoperative measurement of Oph AP was 12.30 mm and decreased to an average of 10.05 mm at 2 months after surgery (p < 0.01), and remained reduced to 10.20 mm at 6 months after surgery (p < 0.01). After that, it increased slightly, and after one year, it became 11.12 mm, which is 1.18 mm lower than before the operation (p < 0.05). Oph vol decreased significantly from 6.04 cm3 preoperatively to 4.24 cm3 at 2 months postoperatively (p < 0.01) and remained decreased to 4.10 cm3 at 1 year postoperatively (p < 0.01) (Table 4).
In group 2, the preoperative mean of Oph AP was 14.52 mm, and no significant change was observed after surgery (p > 0.05). Oph vol decreased from an average of 7.39 cm3 preoperatively to 5.26 cm3 at 6 months postoperatively and then returned to 7.11 cm3 at 1 year postoperatively (Table 5).
Group 1 and group 2 were significantly different in the Oph vol change at the T1–T2, T2–T3, and T0–T3 periods (Table 6).
Hypopharyngeal airway change
In group 1, the Hph AP value decreased significantly from 17.70 mm preoperatively to 15.93 mm at 2 months postoperatively and 15.30 mm at 6 months postoperatively (p < 0.05). Then Hph AP significantly increased at T2–T3 periods to 16.67mm (p < 0.05) and relapsed to preoperative value (T0–T3, p > 0.05). Hph vol significantly decreased from 7.80 cm3 preoperatively to 5.94 cm3 at 2 months postoperatively (p < 0.01) and remained decreased to 5.93 cm3 at 6 months and 6.04 cm3 at 1 year postoperatively (p < 0.01) (Table 4).
In group 2, Hph AP was 18.00 mm preoperatively and no change was observed until 1 year postoperatively (p > 0.05). The average Hph vol value was 8.32 cm3 preoperatively, and no significant change was observed until the first year (p > 0.05) (Table 5).
Group 1 and group 2 were significantly different in the Hph vol change at the T0–T1 stage (p < 0.05) (Table 6).
Whole pharynx volume change
Whole pharynx volume is the sum of the nasopharyngeal, oropharyngeal, and hypopharyngeal airway volume values. Whole pharynx volume in group 1 significantly decreased from 20.07 cm3 preoperatively to 16.07 cm3 at 2 months postoperatively by 3.99 cm3 (p < 0.01) and decreased the most to 15.67 cm3 at 1 year postoperatively (p < 0.01) (Table 4).
In group 2, whole pharynx volume decreased from 23.14 cm3 before surgery to 21.25 cm3 at 2 months after surgery, but there was no significant change in comparison (p > 0.05). In addition, when comparing whole pharynx volume at T2 with T3, the average increased significantly from 19.19 cm3 to 22.81 cm3 (p < 0.01) and relapsed to a similar value to the preoperative average of 23.14 cm3 (T0–T3, p > 0.05) (Table 5).
Group 1 and group 2 were significantly different in the T2–T3 and T0–T3 stages (p < 0.05) (Table 6)
B point change (setback amount)
SV-B is the distance from the sella vertical plane to the B point, which is measured to know the setback amount and relapse tendency. The difference between the SV-B values before and after surgery means the setback amount.
In group 1, the average preoperative SV-B was 64.97 mm, and in group 2, the average preoperative SV-B was 63.93 mm. The amount of change in SV-B value before and at 2 months after surgery was 4.85 mm in group 1 and 6.81 mm in group 2. In both groups, the SV-B value decreased significantly at T1 (p < 0.01), and the decreased value was maintained until T3 (Tables 4 and 5, Fig. 3).
Discussion
BSSRO setback surgery and bimaxillary surgery are often used to treat class III malocclusion patients. Since there is a possibility of OSA after surgery, it is necessary to evaluate the pharyngeal airway before and after surgery. Because of its relatively simple and inexpensive advantage, many studies have used lateral cephalograms for preoperative and postoperative airway evaluation.
Riley and Powell [23] said that both CT and cephalometry are quite accurate for measuring the airway volume. However, Lenza et al. [24] argued that the upper airway could not be represented accurately by linear measurements only on cephalogram. Because of its low exposure and intuitive viewing of 3D structures, CBCT is widely used in hospitals these days. Since it is taken before and after surgery, during diagnosis, planning, and follow-up, it is possible to evaluate hard tissue and soft tissue in 3D for pharyngeal airway. There have been many studies on pharyngeal airway analysis through CT after mandible setback surgery, and various reference points, planes, and measurements were used [5, 12, 25]. In this study, the changes in pharyngeal airway after two types of mandibular setback surgery were investigated. The InVivo5 program was used for CT analysis, and since the measured values for the airway may vary depending on the posture, re-orientation was performed based on the right porion and the Frankfort horizontal plane passing through the orbitalia with the nasion as the origin. The landmarks, sella (Se), PNS, P, E, B point, were indicated, and Nph AP, Oph AP, and Hph AP were measured for AP distance, and Nph vol, Oph vol, Hph vol, and whole pharyngeal volume were measured to obtain volumetric change. The SV-B distance was measured to find out the amount of mandible setback.
Holmberg and Linder-Aronson [26] found that Nph is not affected by mandibular setback surgery. Wenzel et al. [27] reported that after BSSRO setback surgery, Nph AP decreased by 2.3 mm after surgery and maintained until 1 year. In the present study, there was no significant change in Nph vol after surgery in group 1 and group 2 patients, and this was the same as that of Hatab et al. [5], Uesugi et al. [12], and Park et al. [25]. Most of the studies reported that Nph measurements were not related to surgery in both group 1 and group 2. In our study, in group 1, the direction of posterior movement of the mandible and the Nph space were anatomically far apart, so it seems that there was no difference before and after surgery. In group 2 patients, Nph AP decreased at postoperative 6 months (T0–T2, p < 0.05) and then increased at 1 year after surgery (T2–T3, p < 0.01) and relapsed (T0–T3, p > 0.05).
Enacar et al. [28] found that the volume of the oropharyngeal airway remained reduced for more than 1 year and 6 months in mandibular setback surgery patients. The hyoid bone and lower tongue point moved down, and accordingly, the hypopharyngeal airway space was significantly reduced. Tselink and Pogrel [29] and Hochban et al. [30], however, found that the oropharyngeal airway reduced postoperatively and recovered. In the present study, oropharyngeal and hypopharyngeal volume significantly decreased and maintained for up to 1 year in group 1. Park et al. [25] and Greco et al. [31] suggested that the Oph was affected more by mandibular setback because it is the close to the mandible and the tongue anatomically. In this study, in group 2, Oph vol were decreased at 6 months postoperatively (T0–T2, p < 0.05) but increased and relapsed significantly at the T2–T3 period. There was no significant change in measurement at 1 year after surgery (T0–T3, p > 0.05). This is consistent with the results of previous papers that the reduction of airway diminished after surgery [13, 14, 25].
The change of whole pharynx volume was significantly decreased and maintained in group 1, but in group 2, there was a tendency to relapse after postoperative reduction, and no significant change was observed at 1 year postoperatively (T0–T3, p > 0.05).
When comparing between group 1 and group 2, the decrease in Oph vol and whole pharynx volume was significantly greater in group 1 up to 1 year after surgery (p < 0.01). In this study, the bimaxillary surgery group was accompanied by an average 4.23 mm of posterior impaction and 0.81 mm advance of the maxilla. This movement causes upward and forward movement of the posterior nasal spine, attached muscles, and soft tissues and it could reduce the effect of narrowing upper airway space, against the posterior movement of the mandible.
In the present study, no patients complained of postoperative OSA or severe and persistent snoring at 1 year postoperatively. However, after orthognathic surgery, especially when only mandibular setback was performed, the volume and distance of the pharyngeal airway were decreased, so a long-term follow-up is required for airway-related symptoms such as snoring and OSA.
Conclusion
In class III malocclusion patients, mandibular setback surgery only showed a greater reduction in pharyngeal airway than bimaxillary surgery with posterior impaction, and bimaxillary surgery was more stable in terms of airway. Therefore, it is important to evaluate the airway before surgery and include it in the surgical plan.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BSSRO:
-
Bilateral sagittal split ramus osteotomy
- OSA:
-
Obstructive sleep apnea
- AP:
-
Anteroposterior
- 3D:
-
Three-dimensional
- CBCT:
-
Cone-beam computed tomography
- CT:
-
Computed tomography
- DICOM:
-
Digital imaging and communications in medicine
- Nph:
-
Nasopharynx
- Oph:
-
Oropharynx
- Hph:
-
Hypopharynx
- SV-B:
-
The distance from the sella vertical plane to the B point
- Se:
-
Sella
- PNS:
-
Posterior nasal spine
- Vol:
-
Volume
References
Li YM, Liu JL, Zhao JL, Dai J, Wang L, Chen JW (2014) Morphological changes in the pharyngeal airway of female skeletal class III patients following bimaxillary surgery: a cone beam computed tomography evaluation. Int J Oral Maxillofac Surg 43(7):862–867. https://doi.org/10.1016/j.ijom.2014.03.009
Kim NR, Kim YI, Park SB, Hwang DS (2010) Three dimensional cone-beam CT study of upper airway change after mandibular setback surgery for skeletal class III malocclusion patients. Korean J Orthod 40(3):145–155. https://doi.org/10.4041/kjod.2010.40.3.145
Kim MA, Kim BR, Youn JK, Kim YJ, Park YH (2014) Head posture and pharyngeal airway volume changes after bimaxillary surgery for mandibular prognathism. J Craniomaxillofac Surg 42(5):531–535. https://doi.org/10.1016/j.jcms.2013.07.022
He J, Wang Y, Hu H, Liao Q, Zhang W, Xiang X, Fan X (2017) Impact on the upper airway space of different types of orthognathic surgery for the correction of skeletal class III malocclusion: a systematic review and meta-analysis. Int J Surg 38:31–40. https://doi.org/10.1016/j.ijsu.2016.12.033
Hatab NA, Konstantinovic VS, Mudrak JK (2015) Pharyngeal airway changes after mono-and bimaxillary surgery in skeletal class III patients: cone-beam computed tomography evaluation. J Craniomaxillofac Surg 43(4):491–496. https://doi.org/10.1016/j.jcms.2015.02.007
Hart PS, McIntyre BP, Kadioglu O, Currier GF, Sullivan SM, Li J, Shay C (2015) Postsurgical volumetric airway changes in 2-jaw orthognathic surgery patients. Am J Orthod Dentofacial Orthop 147(5):536–546. https://doi.org/10.1016/j.ajodo.2014.12.023
Fernández-Ferrer L, Montiel-Company JM, Pinho T, Almerich-Silla JM, Bellot-Arcis C (2015) Effects of mandibular setback surgery on upper airway dimensions and their influence on obstructive sleep apnoea–a systematic review. J Craniomaxillofac Surg 43:248–253
Azevêdo MS, Machado AW, Barbosa IS, Esteves LS, Rocha VÁC, Bittencourt MAV (2016) Evaluation of upper airways after bimaxillary orthognathic surgery in patients with skeletal class III pattern using cone-beam computed tomography. Dental Press J Orthod 21(1):34–41. https://doi.org/10.1590/2177-6709.21.1.034-041.oar
Santagata M, Tozzi U, Lamart E, Tartaro G (2015) Effect of orthognathic surgery on the posterior airway space in patients affected by skeletal class III malocclusion. J Maxillofac Oral Surg 14(3):682–686. https://doi.org/10.1007/s12663-014-0687-8
Panou E, Motro M, Ates M, Acar A, Erverdi N (2013) Dimensional changes of maxillary sinuses and pharyngeal airway in class III patients undergoing bimaxillary orthognathic surgery. Angle Orthod 83(5):824–831. https://doi.org/10.2319/100212-777.1
Mattos CT, Vilani GN, Sant'Anna EF, Ruellas AC, Maia LC (2011) Effects of orthognathic surgery on oropharyngeal airway: a meta-analysis. Int J Oral Maxillofac Surg 40(12):1347–1356. https://doi.org/10.1016/j.ijom.2011.06.020
Uesugi T, Kobayashi T, Hasebe D, Tanaka R, Ike M, Saito C (2014) Effects of orthognathic surgery on pharyngeal airway and respiratory function during sleep in patients with mandibular prognathism. Int J Oral Maxillofac Surg 43(9):1082–1090. https://doi.org/10.1016/j.ijom.2014.06.010
Degerliyurt K, Ueki K, Hashiba Y, Marukawa K, Nakagawa K, Yamamoto E (2008) A comparative CT evaluation of pharyngeal airway changes in class III patients receiving bimaxillary surgery or mandibular setback surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105(4):495–502. https://doi.org/10.1016/j.tripleo.2007.11.012
Chen F, Terada K, Hua Y, Saito I (2007) Effects of bimaxillary surgery and mandibular setback surgery on pharyngeal airway measurements in patients with class III skeletal deformities. Am J Orthod Dentofacial Orthop 131(3):372–377. https://doi.org/10.1016/j.ajodo.2005.06.028
Hong JS, Park YH, Kim YJ, Hong SM, Oh KM (2011) Three-dimensional changes in pharyngeal airway in skeletal class III patients undergoing orthognathic surgery. J Oral Maxillofac Surg 69(11):e401–e408. https://doi.org/10.1016/j.joms.2011.02.011
Liukkonen M, Vahatalo K, Peltomaki T, Tiekso J, Happonen RP (2002) Effect of mandibular setback surgery on the posterior airway size. Int J Adult Orthodon Orthognath Surg 17(1):41–46
Pereira-Filho VA, Castro-Silva LM, de Moraes M, Gabrielli MF, Campos JA, Juergens P (2011) Cephalometric evaluation of pharyngeal airway space changes in class III patients undergoing orthognathic surgery. J Oral Maxillofac Surg 69(11):e409–e415. https://doi.org/10.1016/j.joms.2011.02.132
Becker OE, Avelar RL, Göelzer JG, do Nascimento Dolzan A, OLH J, de Oliveira RB (2012) Pharyngeal airway changes in class III patients treated with double jaw orthognathic surgery—maxillary advancement and mandibular setback. J Oral Maxillofac Surg 70(11):e639–e647. https://doi.org/10.1016/j.joms.2012.07.052
Burkhard JPM, Dietrich AD, Jacobsen C, Roos M, Lübbers H-T, Obwegeser JA (2014) Cephalometric and three-dimensional assessment of the posterior airway space and imaging software reliability analysis before and after orthognathic surgery. J Craniomaxillofac Surg 42(7):1428–1436. https://doi.org/10.1016/j.jcms.2014.04.005
Foltan R, Hoffmannova J, Donev F, Vlk M, Sedy J, Kufa R, Bulik O (2009) The impact of Le Fort I advancement and bilateral sagittal split osteotomy setback on ventilation during sleep. Int J Oral Maxillofac Surg 38(10):1036–1040. https://doi.org/10.1016/j.ijom.2009.06.001
Jiang YY (2016) Correlation between hyoid bone position and airway dimensions in Chinese adolescents by cone beam computed tomography analysis. Int J Oral Maxillofac Surg 45(7):914–921. https://doi.org/10.1016/j.ijom.2016.02.005
Gokce SM, Gorgulu S, Gokce HS, Bengi AO, Karacayli U, Ors F (2014) Evaluation of pharyngeal airway space changes after bimaxillary orthognathic surgery with a 3-dimensional simulation and modeling program. Am J Orthod Dentofacial Orthop 146(4):477–492. https://doi.org/10.1016/j.ajodo.2014.06.017
Riley RW, Powell NB (1990) Maxillofacial surgery and obstructive sleep apnea syndrome. Otolaryngol Clin North Am 23(4):809–826. https://doi.org/10.1016/S0030-6665(20)31254-8
Lenza MG, Lenza MM, Dalstra M, Melsen B, Cattaneo PM (2010) An analysis of different approaches to the assessment of upper airway morphology: a CBCT study. Orthod Craniofac Res 13(2):96–105. https://doi.org/10.1111/j.1601-6343.2010.01482.x
Park SB, Kim YI, Son WS, Hwang DS, Cho BH (2012) Cone-beam computed tomography evaluation of short- and long-term airway change and stability after orthognathic surgery in patients with class III skeletal deformities: bimaxillary surgery and mandibular setback surgery. Int J Oral Maxillofac Surg 41(1):87–93. https://doi.org/10.1016/j.ijom.2011.09.008
Holmberg H, Linder-Aronson S (1979) Cephalometric radiographs as a means of evaluating the capacity of the nasal and nasopharyngeal airway. Am J Orthod 76(5):479–490. https://doi.org/10.1016/0002-9416(79)90252-5
Wenzel A, Williams S, Ritzau M (1989) Changes in head posture and nasopharyngeal airway following surgical correction of mandibular prognathism. Eur J Orthod 11(1):37–42. https://doi.org/10.1093/oxfordjournals.ejo.a035962
Enacar A, Aksoy AU, Sencift Y, Haydar B, Aras K (1994) Changes in hypopharyngeal airway space and in tongue and hyoid bone positions following the surgical correction of mandibular prognathism. Int J Adult Orthodon Orthognath Surg 9:285–290
Tselnik M, Pogrel MA (2000) Assessment of the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg 58(3):282–285. https://doi.org/10.1016/S0278-2391(00)90053-3
Hochban W, Conradt R, Brandenburg U, Heitmann J, Peter JH (1997) Surgical maxillofacial treatment of obstructive sleep apnea. Plast Reconstr Surg 99(3):619–626. https://doi.org/10.1097/00006534-199703000-00002
Greco JM, Frohberg U, Van Sickels JE (1990) Long-term airway space changes after mandibular setback using bilateral sagittal split osteotomy. Int J Oral Maxillofac Surg 19(2):103–105. https://doi.org/10.1016/S0901-5027(05)80204-8
Acknowledgements
Not applicable
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
SIS carried out the surgical treatment of the patient and contributed to the conception of the report and critical revising. NEK and DHL participated in the treatment, collection of the data, and drafting of the manuscript. NEK and JIS performed the statistical analysis. SIS and JKL contributed to the critical revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ajou University School of Medicine Institutional Review Board (Approval No. AJIRB-MED-MDB-20-078) approved the study protocol.
Consent for publication
Not Applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kang, N.E., Lee, D.H., In Seo, J. et al. Postoperative changes in the pharyngeal airway space through computed tomography evaluation after mandibular setback surgery in skeletal class III patients: 1-year follow-up. Maxillofac Plast Reconstr Surg 43, 31 (2021). https://doi.org/10.1186/s40902-021-00319-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40902-021-00319-1