Abstract
More than 30 randomized controlled trials, supported by individual patient-level and group-level meta-analyses and a Delphi analysis of expert opinion, unequivocally show isometric resistance training (IRT) elicits antihypertensive benefits in healthy people and those with chronic illness. We aim to provide efficacy and safety evidence, and a guide for IRT prescription and delivery. Recommendations are made for the use of IRT in specific patient populations and appropriate methods for IRT delivery. Published data suggest IRT consistently elicits mean blood pressure reductions of 7.4/3.3 mmHg systolic blood pressure/diastolic blood pressure, equivalent to antihypertensive medication monotherapy. Blood pressure reductions of this size are associated with an approximate 13% to 22% reduction in major cardiovascular events. Moreover, IRT is safe in a range of patient populations. We suggest that IRT has the greatest potential benefit when used as an antihypertensive therapy in individuals unwilling and/or unable to complete aerobic exercise, or who have had limited adherence or success with it; individuals with resistant or uncontrolled hypertension, already taking at least two pharmacological antihypertensive agents; and healthy or clinical populations, as an adjunct to aerobic exercise and dietary intervention in those who have not yet attained control of their hypertension. IRT is efficacious and produces clinically meaningful blood pressure reductions (systolic blood pressure, 7 mmHg; diastolic blood pressure, 3 mmHg). IRT is safe and typical program delivery requires only about 17 min weekly. IRT should be used as an adjunct to other exercise modalities, in people unable to complete other types of exercise, or in resistant hypertension.
Similar content being viewed by others
Background
In the last two decades more than 30 randomized controlled trials (RCTs) [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16], supported by individual patient-level [17] and group-level meta-analyses [18,19,20,21,22,23,24,25,26], have unequivocally demonstrated that isometric resistance training (IRT) elicits antihypertensive benefits in people who are healthy [8, 9, 14, 15] and those who exhibit prehypertension [2, 10], hypertension [1, 11, 13, 16], peripheral artery disease [4], coronary heart disease [3] and heart failure [5]. Current guidelines suggest the gold standard exercise prescription for managing hypertension is aerobic exercise [27] with emphasis more recently attributed to IRT [28, 29]. While recognizing current guidelines, Cornelissen and Smart [30] first demonstrated, using a pooled data analysis, that reductions in systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP), following a 4 to 8 weeks program of IRT, are greater than those observed with an aerobic exercise training (AET) or dynamic resistance training (DRT) program of similar duration [30].
IRT has also been shown to elicit improvements in endothelial function [4, 31,32,33,34] and coronary collateral vessel blood flow in people with coronary artery disease [35]. IRT can achieve these beneficial physiological adaptations while eliciting a much lower rate pressure product (RPP) index than both AET and DRT [36]. RPP is the product of SBP and heart rate (HR), and cardiologists often use this as an estimate of myocardial oxygen uptake (clinically, RPP is a reliable indicator of myocardial oxygen demand and valuable marker of cardiac function). In cardiac patients diagnosed with exertional symptoms, such as angina, a RPP threshold can be set to avoid symptom exacerbation and related adverse events, such as exercise-induced arrhythmia. During isometric contractions there are only small increases in HR, and pressor responses are often smaller than when performing recommended levels of AET and DRT, resulting in a lower RPP with IRT [36]. Intuitively, this would mean that IRT is less likely to provoke exertional stress and cardiac events than AET or DRT. Early IRT cohort studies [37,38,39,40] in the 1970s used very high exertional intensity and evoked hypertensive responses [37] that suggested IRT may be dangerous [37, 41], especially for those with hypertension. IRT studies in the last 30 years have used exertional intensities mostly in the range of 30% of an individual’s maximum capacity and this has led to well documented antihypertensive effects [17] and abrogation of safety concerns related to IRT [19].
As the use of IRT to treat hypertension, is a relatively new concept, there remain, understandably, concerns amongst exercise specialists and other health professionals about whether this form of therapy can be used safely and in which patient populations. Even though more than 30 RCTs since the 1990s have suggested a sustained post training antihypertensive benefit [42], and the initial scientific opinion, to avoid IRT, has reversed somewhat in the last two decades, this form of therapy remains under-utilized and some bodies still have reservations about its use [43].
The aim of this work is to provide a systematic summary and practical guide to IRT, based upon the available published evidence for efficacy and safety.
Isometric resistance training
An isometric muscle contraction is one where there is no change in muscle length, but a force is applied, and muscle tension may increase (Fig. 1A). This may occur because the force produced by the muscle(s) is the same as the external resistance (e.g., holding a dumbbell) or because the opposing load is greater than the force generated (e.g., trying to push over a large, stable tree trunk). As there is no observable change in joint angle and muscle length during the contraction, it is often referred to as a “static” contraction. Simply, dynamic or isotonic contractions (concentric and eccentric) move loads, while isometric contractions create force and/or tension without movement.
Visual depiction of (A) isometric and (B) isotonic muscular contractions (arrows indicate arm movement; no movement (A) and flexion (B)). During an isometric contraction, muscle length does not change; however, tension might increase. During an isotonic contraction, muscle length either shortens (concentric contraction) or lengthens (eccentric contraction) and tension remains the same
During isometric work the contraction is static and sustained and therefore the intramuscular pressure generated is often enough to partially or fully inhibit vascular blood flow in the vessels that serve that particular muscle or muscle group [36]. For example, handgrip squeezing exercise requires a static forearm contraction and therefore the flow in the brachial artery may be partially or fully occluded. The extent of the disruption to blood flow is dependent on the relative intensity of the contraction [39, 44]. After the isometric contraction ceases reactive hyperemia occurs; this is transient blood flow, at a raised rate, that occurs in healthy blood vessels following an ischemic episode, such as IRT at a sufficient proportion or percentage of maximal voluntary contraction (MVC; the maximal force-generating capacity of a muscle or group of muscles in humans), usually this is 15% to 30% of MVC [14, 45]. This reactive hyperemia is facilitated by vasodilation, and this results in a sustained blood pressure reduction that lasts for an undefined period of time but commonly several hours [46]. As with other types of exercise training, repeated exposure to cycles of ischemia-hyperemia-reperfusion can lead to stable blood pressure changes (lowering) which are sustained if one continues to train. This training status dependent lowering of blood pressure has been shown to be a result of anatomical increases in blood vessel diameter with aerobic exercise [47], but similar data is not available for IRT. However, IRT causes an acute stimulation of the metaboreflex in an attempt to restore muscle blood flow. This and other long-term physiological responses (occurring from approximately 4 weeks onwards) may reduce tissue oxidative stress, and improve vascular endothelial function, baroreflex sensitivity, and autonomic balance [48].
To put this into context, a healthy man aged 20 to 50 years would be expected to generate a maximal isometric handgrip contraction of about 40 to 50 N. It is thought that at about 20% to 30% of one’s handgrip MVC, there is a measurable disruption to blood flow. For lower limb isometric contractions (e.g., squatting with one’s back resting against a wall with knees at a 90° angle), it is believed that the disruption to blood flow occurs at a slightly lower relative intensity of 15% to 25% MVC; this is probably due to the greater force generated and specific fiber arrangement [49] in the muscles of the lower limb. The relative exercise intensity (equivalent to %MVC) generated in isometric wall squats can be adjusted by changing the knee joint angle [50, 51].
A rapidly growing body of evidence continues to highlight the benefits of IRT in lowering blood pressure (BP). However, to date, the exact mechanisms responsible for the BP lowering effects of IRT have not been fully elucidated. The effects of IRT most likely involve interactions of a number of pathways and mechanisms, including endothelial function, structural vascular adaptations, oxidative stress, and autonomic nervous system activity [13, 52].
Efficacy of IRT
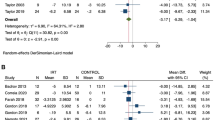
A 2013, meta-analysis showed typical changes in BP for published studies of exercise training with a training duration of 8 to 12 weeks (Fig. 2, based on Cornelissen and Smart 2013) [30]. The sizes of these differences are both statistically significant and clinically meaningful. There was no overlap in 95% confidence intervals (CIs) between IRT and the other three types of exercise training; however, there was considerable overlap in the 95% CIs for the three other types of exercise (Fig. 2).
Change in systolic blood pressure (SBP) and diastolic blood pressure (DBP) by exercise modality. Based on Cornelissen and Smart [30]
In 2014, a group-level meta-analysis was conducted on all nine published RCTs of IRT (223 participants) and confirmed that the antihypertensive effects were greater than those reported in most aerobic and DRT studies [18]. In progressing the evidence base, a 2016 group-level meta-analysis was performed of all 11 published RCTs of IRT. Again, the analyses confirmed antihypertensive effects, the additional findings from this work were that certain patient subgroups may benefit more [20]. Specifically, people over 45 years appear to benefit more than younger people, and people diagnosed with hypertension appeared to derive a greater hypertensive benefit than those who were normotensive [20]. This work also suggested a greater benefit in IRT trials lasting > 8 weeks, compared to shorter studies.
In 2019 an individual patient data (IPD) meta-analysis was performed on 12 randomized, controlled trials of IRT [17]. The purpose of taking the IPD approach was that, while retaining the characteristics of individual study designs (e.g., exercise program variables), it was possible to make direct comparisons between subject characteristics and effect sizes. The IPD methodology is considered superior to group-level meta-analyses [53,54,55]. This IPD analyses confirmed similar antihypertensive effect sizes for SBP (–7.35 mmHg; 95% CI, –8.95 to –5.75 mmHg) and DBP (–3.29 mmHg; 95% CI, –5.12 to –1.46 mmHg), with very small 95% CIs, that were observed in previous systematic reviews and pooled analyses in the period of 2013 to 2016. The size of this effect is thought to be similar to the antihypertensive benefit elicited from taking one antihypertensive medication [56].
Most recently, in 2021 a Delphi method was employed to seek expert consensus-building on items related to the safety, efficacy, and delivery of IRT, in light of the current trend towards use of IRT as an adjunct treatment for hypertension [57]. This study showed experts’ consensus that IRT is as efficacious as an antihypertensive therapy. Furthermore, the antihypertensive efficacy of IRT has stood the test of time over the last three decades.
Safety
Cardiovascular responses to exercise
An intensity-dependent rise in HR and BP occurs with all types of physical exercise. Central command, muscle reflexes, and the arterial baroreflex are important regulators of the cardiovascular system during exercise [58, 59]. An exaggerated BP response to exercise is a predictor of future chronic hypertension which may lead to risk of organ damage, cardiac events, and mortality [60,61,62]. Somewhat paradoxically regular exercise, at an appropriate intensity and volume, has been shown to reduce BP and reduce the risk of organ damage and cardiovascular disease. As with many novel medical treatment approaches there is often an inherent concern that new ideas may cause harm. In hypertensive individuals compared to normotensive individuals, it is this “possible” exaggerated pressor (hypertensive) response, resulting in an increase in pressure load on the heart, that appears to raise the most concern among professionals in relation to the safety of IRT. However, as outlined below, evidence indicates that the acute increase in BP during IRT is no larger, and in fact in some studies smaller [36, 63, 64], than that observed with AET.
We acknowledge that the threshold for an extreme or exaggerated hypertensive response does vary with different datasets [65]. The threshold for a hypertensive response to physical stress is as low as 190/90 mmHg and as high as 250/120 mmHg in different settings [65]. The physiological basis of why isometric contractions at or above 50% MVC may cause extreme hypertensive responses was outlined in the early 1970s. In 1970, Lind [41] described that at 10% to 15% MVC, isometric contractions can be maintained for 30 min or more. At these low tensions, the HR increases by only a few beats per minute (bpm) and BP by only 5 to 15 mmHg, for as long as the tension is maintained. Muscle blood flow also increases to a steady state, which corresponds with the indefinite period contractions can be held for. At 20% MVC and higher, fatigue occurs rapidly. At 20% MVC, contractions can be held for around 10 min. At 30% MVC, the duration is about 5 min, while at 50% MVC, it is 1 to 2 min. When working to a constant force above 20% MVC, the blood flow in the muscle does not reach a steady state, nor does the HR or BP. Instead, all these factors continue to increase until fatigue, as a function of duration intervenes. At the point of fatigue, it is uncommon for HR to be over 120 bpm. However, both SBP and DBP increase dramatically and almost in parallel, and MAP at fatigue is commonly 140 mmHg or more. By contrast, in fatiguing rhythmic exercise (a treadmill test of progressive severity), the HR characteristically reaches near maximum values, while the MAP shows only slight changes. In isometric exercise, widespread peripheral vasoconstriction occurs, so increased cardiac output then elicits a BP rise, but stroke volume does not increase and at higher tensions (for example, 50% MVC) it decreases, so that increased HR is the sole contributor to the increase in cardiac output [41].
For the reasons outlined in the previous paragraph, there was a historical reluctance to use IRT in people with even mild hypertension, but recent trials have used low to moderate training intensities (10%–30% MVC) [2, 9] normally performed for a short 2-min duration; these are associated with, relatively modest [64] rises in BP during IRT. In summary, during both isotonic and isometric muscular contractions there is a notable pressor (BP raising) response at intensities of 50% MVC or above, but this is mitigated by the lower (10%–30% MVC) training intensities and shorter durations that have become common practice. Finally, one should not forget that there is also evidence of blood flow impairment with repeated concentric contractions [66].
Early concerns about IRT safety
As mentioned previously, from a historical perspective IRT was contraindicated for people with hypertension [67, 68]. In some of the early studies, IRT was employed at a relatively high proportion (> 50%) of MVC, with some studies asking research subjects to contract at maximal capacity (100% MVC) resulting in an exaggerated pressor response [69, 70]. Contractions 50% MVC, or above, are likely to generate a notable pressor (hypertensive) response > 200/100 mmHg and should be avoided in all but young, healthy people clinically free of cardiovascular disease.
One should point out that once IRT ceases, BP will return very close to baseline levels in a matter of seconds [71, 72], whereas the normal time course of recovery to prolonged aerobic exercise is of longer duration, usually several minutes, but can be several hours [73]. Previous work has identified that people are at a raised risk of adverse exertional-related health events during aerobic exercise and the 30 to 60 min post exercise recovery period [74]. Three key points are evident from our observations of BP responses to IRT. First, one can see from Fig. 3 that RPP exhibits a positive linear correlation with %MVC during IRT activity. Second, despite a slight cumulative upward drift, the RPP values still remain less that the RPP values for moderate aerobic intensity in hypertensive individuals at equivalent %MVC (Fig. 3, Table 1). Third, individuals with hypertension exhibit slightly higher RPP values than people with normal BP, at the same %MVC intensity (Table 1).
Peak rate pressure product across isometric handgrip exercise at various maximal voluntary contraction [36]. Rate pressure product (RPP) values following the first and fourth isometric resistance training bout in normotensive and prehypertensive populations at 5%, 10% and 30% maximal voluntary contraction (MVC)
Current evidence for IRT safety
A recently published meta-analysis [19] of RCTs of IRT showed long-term BP lowering effects are achieved with isometric contractions at 15% to 30% MVC. While contractions at this intensity do raise BP, the increase is much smaller (20–30 mmHg) than would be seen with moderate intensity aerobic exercise. IRT also results in much smaller (10–30 bpm) increases in HR. The net RPP is much lower with IRT versus aerobic exercise (Table 1). Available data suggests that this difference is greatest when participants use small muscle mass isometric handgrip training, compared to a RPP value of 18,000 bpm × mmHg (based upon BP and HR average over the last 30 s of the final/fourth wall squat bout) for participants (with high-normal BP) performing double-leg IRT [64]. RPP is used primarily by cardiologists to estimate oxygen utilization in the myocardial tissues. Often people with symptoms of angina pectoris become symptomatic at a reproducible threshold [75]. In people with exertional angina symptoms, or cardiac arrhythmia, an RPP threshold can be set in order to minimize symptom exacerbation and lower the risk of serious cardiovascular events.
IRT produces an ischemic preconditioning response that is cardio protective [3, 76]. This effect is also seen with aerobic and possibly dynamic resistance exercise, but a much higher RPP is generated during these latter two forms of exercise. IRT produces a reactive hyperemic response immediately post exercise that improves endothelial function long-term [73]. IRT elicits greater uptake of blood into the coronary collateral circulation in people with coronary artery disease [35]. Similarly, in people with peripheral arterial disease, IRT was reported to reduce brachial DBP, and increase flow mediated dilatation [4], a measure of endothelial function. IRT also elicits rises in vascular endothelial growth factor (stimulant for new blood vessel growth) in heart failure patients [5]. The available evidence therefore suggests that the “default” position that IRT is unsafe is perhaps unsupported, and indeed contradicted somewhat, by the published literature. Benefits can also be seen in other patient populations, as shown in Table 2, which provides a summary of analyses and studies across different populations indicating any safety concerns or possible contraindications to the use of IRT.
While the benefits of IRT can be seen in a range of patient populations, concerns about safety of this type of exercise may be further alleviated if one recalls IRT is only sustained for 1 to 2 min, which is below the 3-min threshold scientists believe is necessary to develop reperfusion injury [77]. With 2 to 3 min rest periods for IRT the minimal increase in HR and mild/moderate hypertensive responses are brief. IRT protocols allow for adequate (complete) recovery periods, which are achieved in seconds with IRT and not minutes as with aerobic exercise. We have reported the findings from IRT training and studies below. A detailed summary of analyses and recent RCTs can be found in Table 2.
Clinical implications
Clinical relevance of IRT
Current evidence indicates IRT lowers BP, but one may ask if these changes are clinically meaningful and hence supportive of the transition of IRT into “real world” clinical practice. In order to provide a “clinical” meaning, we conducted secondary analyses from our earlier IPD and categorized participants as responders versus nonresponders [17]. We defined “responders” as any participant who showed a 5 mmHg or greater reduction in SBP, a 3 mmHg or greater reduction in DBP, and/or a 3 mmHg or greater reduction in MAP [78].
For each of SBP, DBP, and MAP, we calculated responder rate, absolute risk reduction (ARR) and number needed to treat (NNT). The 28.1% ARR is the difference between the proportion of responders in the IRT (55.5%) minus control (27.4%). The NNT is the inverse of the ARR. Approximately three times as many people who undertake IRT experience a favorable BP lowering response compared to controls who do not undertake IRT. This means that about one-quarter (27.4%) of people will lower their BP independent of IRT, probably due to any of the following approaches, or combination thereof—medication changes, weight loss, or improved diet. Moreover, if someone with hypertension undertakes a program of IRT then their likelihood of reducing their BP increases to about 55% (Table 3).
A landmark meta-analysis by Xie et al. [79] demonstrated that if one were able to reduce a participant’s SBP by 7 mmHg this would equate to a 13% risk reduction for myocardial infarction and a 22% risk reduction for stroke. Moreover, our 2019 IPD meta-analysis [17] demonstrates that this magnitude of BP reduction is possible to detect in a sample of > 320 participants, as demonstrated in our two-step model of our IPD data. Additionally, the recent Delphi study of experts’ consensus fully supports IRT as it produces clinically meaningful BP reductions [57].
Transition of IRT into clinical practice
Who is most likely to benefit from IRT?
IRT has been safely conducted with no adverse events reported to date (Table 2). The only contraindication to IRT identified is that there may be a raised risk of mild cognitive impairment in postmenopausal women who have a history of preeclampsia [80]. It should be clarified though, that this possible association was not generated from a longitudinal follow-up study design that allowed direct causation to be attributed.
As a guide to exercise practitioners who may wish to use IRT in their patients, the recommendations listed below may help to optimize IRT utilization. While IRT can be used in most people, it is suggested that IRT has the greatest potential benefit when utilized as an antihypertensive therapy in: (1) individuals unwilling or unable to complete aerobic exercise, or who have had limited adherence or success with it; (2) individuals with resistant or uncontrolled hypertension, already taking at least two pharmacological antihypertensive agents; (3) healthy or clinical populations, as an adjunct to aerobic exercise and dietary intervention in those who have yet to attain control of their hypertension.
What are the other potential applications for IRT use?
Recent work has postulated that IRT may also be beneficial for managing BP in patients with mild cognitive impairment as vascular integrity is likely improved. There is the potential for IRT to initiate a cascade of vascular, neurotrophic, and neuroendocrine events that could enhance cognitive function [81].
In healthy pregnant women, testing of maternal and fetal hemodynamic responses to IRT has indicated no specific safety concerns, concluding that isometric exercise may facilitate exercise compliance in pregnant women [82]. Given the benefits of IRT in hypertensive individuals, future work examining IRT in pregnant women who exhibit prehypertension during pregnancy, may indicate beneficial effects on BP, and this may possibly prevent progression to hypertension and the incidence of preeclampsia in later stages in some individuals. However, future work is required in this area before using IRT in this population.
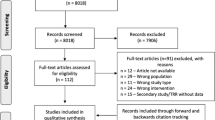
How should the exercise specialist triage people to IRT?
As is recommended for the commencement of any new exercise training, individuals should be adequately screened and cleared by a suitably qualified health professional. In prescreening and assessing an individual to ascertain suitability for IRT, certain questions can be asked by an exercise specialist to assist in guiding patients in selecting an appropriate IRT protocol (Fig. 4).
Questions an exercise specialist must ask or consider are the following: (1) Would this person be suitable for moderate intensity aerobic exercise? If yes, then they are probably suitable for IRT from a CV standpoint. Obvious red flags requiring further clinical evaluation include unstable angina, grade II or higher hypertension that is uncontrolled, or arrhythmia, but these flags are relevant to any form of exercise. If no, then it is recommended to wait until the patient is treated/stabilized before proceeding. (2) In women, is the person over 50 years (postmenopausal) and/or has a history of preeclampsia? If so, contact the medical practitioner and ask about other risk factors. (3) Is there any musculoskeletal injury that may require modification of the IRT protocol, from arm to leg or vice versa?
Prescription and delivery of IRT
Table 4 illustrates an IRT exercise prescription model for translation to clinical practice for BP management.
Upper limb IRT can be prescribed simply with the use of a hand dynamometer, numerous models are available, ranging from expensive research grade to simple low technology versions. As long as the dynamometer can accurately record the force generated and display maximum force generated (100% MVC) it can be used to prescribe handgrip IRT, we suggest using 30% MVC and retesting MVC and recalculating 30% MVC, every session.
Based upon current practice, lower limb IRT is more difficult to prescribe using a low technology approach. Researchers have previously demonstrated a reliable linear relationship between lower limb intensity (at that point it was defined by vastus lateralis surface electromyography) and exercising HR measured during an incremental isometric exercise test performed using double-leg extension. HR was shown to be relatively stable in the last 30 s of each 2-min workload, allowing reliable prescription from the final 2-min workload reached [51]. More recently, a similar robust (inverse) relationship was demonstrated between HR and knee joint angle during a laboratory-based incremental wall squat test [64]. This allows for an effective home-based isometric wall squat prescription with accurate control of exercise intensity based upon the knee joint angle required to elicit a given percentage (normally 95%) of HR peak/mean HR during the final 30 s of the incremental test [13, 15].
Since the adoption of lower limb IRT is currently limited by the need for an initial laboratory-based assessment to allow an individualized prescription, we propose that a first bout rating of perceived exertion (RPE) response of five to six out of 10 on the modified Borg scale is probably a simpler and equally reliable method to ascertain the correct lower limb intensity (%MVC). Indeed, recent publications by Lea et al. [83] assessed the validity and reliability of RPE as a measure of intensity during isometric wall squat exercise and have shown that the Isometric Exercise Scale (IES) provides valid and reliable measurements of RPE, exercise intensity; and IES results had strong positive relationships with the criterion measures of the changes in physiological exertion (HR and BP) during continuous incremental isometric exercise interventions [84]. Thus, the IES could prove to be useful in selecting and monitoring of workloads for those (especially vulnerable populations) wishing to utilize isometric wall squat exercise, or other IRT interventions.
Key clinical issues
Time, accessibility, and cost are commonly reported barriers to exercise participation and adherence [85,86,87]. The evidence for the benefits of IRT in improving general health including chronic conditions is unequivocal. Given the low rate of participation and the problem of long-term adherence, where possible, exercise specialists need to consider interventions that can reduce barriers, promote adherence and in turn have patients reap the benefits. IRT has the potential to do this. It is accessible to most people, takes as little as 17 min per session three times weekly, and the cost is negligible, especially when appropriately transitioned to a home exercise program.
Conclusions
The aim of this work was to provide a summary of the available evidence as to the efficacy and safety of IRT and how this can best be transitioned into a real-world clinical setting. A rapidly expanding evidence base indicates IRT to be very effective for managing hypertension. There is no published data suggesting IRT is unsafe at prescribed MVC intensities typically used to elicit antihypertensive effects. Published data in potentially high-risk populations (e.g., heart failure) shows relevant benefits beyond BP lowering (e.g., improved endothelial and collateral vessel function). The size of BP reductions which have consistently been shown equate to > 10% myocardial infarction and > 20% stroke reductions. However, despite the recent American College of Cardiology and American Heart Association endorsement of IRT [29], to date it has not been widely accepted and is underused globally as an adjunct treatment, indicating that translation into practice may require resourcing to improve awareness and assist with delivery.
Availability of data and materials
Not applicable.
Abbreviations
- AET:
-
Aerobic exercise training
- ARR:
-
Absolute risk reduction
- bpm:
-
Beats per minute
- BP:
-
Blood pressure
- CI:
-
Confidence interval
- CV:
-
Cardiovascular
- DBP:
-
Diastolic blood pressure
- DRT:
-
Dynamic resistance training
- HEP:
-
Home-based exercise program
- HR:
-
Heart rate
- IES:
-
Isometric Exercise Scale
- IPD:
-
Individual patient data
- IRT:
-
Isometric resistance training
- MAP:
-
Mean arterial pressure
- MVC:
-
Maximal voluntary contraction
- N:
-
Newton
- NNT:
-
Number needed to treat
- RCT:
-
Randomized controlled trial
- RPE:
-
Rating of perceived exertion
- RPP:
-
Rate pressure product
- SBP:
-
Systolic blood pressure
- VEGF:
-
Vascular endothelial growth factor
References
Cahu Rodrigues SL, Farah BQ, Silva G, Correia M, Pedrosa R, Vianna L, et al. Vascular effects of isometric handgrip training in hypertensives. Clin Exp Hypertens. 2020;42:24–30.
Carlson DJ, Inder J, Palanisamy SK, McFarlane JR, Dieberg G, Smart NA. The efficacy of isometric resistance training utilizing handgrip exercise for blood pressure management: a randomized trial. Medicine (Baltimore). 2016;95: e5791.
Chen W, Ni J, Qiao Z, Wu Y, Lu L, Zheng J, et al. Comparison of the clinical outcomes of two physiological ischemic training methods in patients with coronary heart disease. Open Med (Wars). 2019;14:224–33.
Correia MA, Oliveira PL, Farah BQ, Vianna LC, Wolosker N, Puech-Leao P, et al. Effects of isometric handgrip training in patients with peripheral artery disease: a randomized controlled trial. J Am Heart Assoc. 2020;9: e013596.
Gao M, Lu X, Chen W, Xiao GH, Zhang Y, Yu R, et al. Randomized clinical trial of physiological ischemic training for patients with coronary heart disease complicated with heart failure: safety of training, VEGF of peripheral blood and quality of life. Exp Ther Med. 2018;16:260–4.
Gordon BD, Whitmire S, Zacherle EW, Doyle S, Gulati S, Leamy LJ, et al. “Get a grip on hypertension”: exploring the use of isometric handgrip training in cardiopulmonary rehabilitation patients. J Cardiopulm Rehabil Prev. 2019;39:E31–4.
Ahmed YR, Hanfy HM, Kamal WM, Fouad MM. The effect of isometric hand grip on blood pressure in post menopausal hypertension. Med J Cairo Univ. 2019;87:2685–91.
Herrod PJ, Blackwell JE, Moss BF, Gates A, Atherton PJ, Lund JN, et al. The efficacy of ‘static’ training interventions for improving indices of cardiorespiratory fitness in premenopausal females. Eur J Appl Physiol. 2019;119:645–52.
Hess NC, Carlson DJ, Inder JD, Jesulola E, McFarlane JR, Smart NA. Clinically meaningful blood pressure reductions with low intensity isometric handgrip exercise: a randomized trial. Physiol Res. 2016;65:461–8.
Ogbutor GU, Nwangwa EK, Uyagu DD. Isometric handgrip exercise training attenuates blood pressure in prehypertensive subjects at 30% maximum voluntary contraction. Niger J Clin Pract. 2019;22:1765–71.
Okamoto T, Hashimoto Y, Kobayashi R. Isometric handgrip training reduces blood pressure and wave reflections in East Asian, non-medicated, middle-aged and older adults: a randomized control trial. Aging Clin Exp Res. 2020;32:1485–91.
Punia S, Kulandaivelan S. Home-based isometric handgrip training on RBP in hypertensive adults: partial preliminary findings from RCT. Physiother Res Int. 2020;25: e1806.
Taylor KA, Wiles JD, Coleman DA, Leeson P, Sharma R, O’Driscoll JM. Neurohumoral and ambulatory haemodynamic adaptations following isometric exercise training in unmedicated hypertensive patients. J Hypertens. 2019;37:827–36.
Wiles JD, Coleman DA, Swaine IL. The effects of performing isometric training at two exercise intensities in healthy young males. Eur J Appl Physiol. 2010;108:419–28.
Wiles JD, Goldring N, Coleman D. Home-based isometric exercise training induced reductions resting blood pressure. Eur J Appl Physiol. 2017;117:83–93.
Yoon ES, Choo J, Kim JY, Jae SY. Effects of isometric handgrip exercise versus aerobic exercise on arterial stiffness and brachial artery flow-mediated dilation in older hypertensive patients. Korean J Sports Med. 2019;37:162–70.
Smart NA, Way D, Carlson D, Millar P, McGowan C, Swaine I, et al. Effects of isometric resistance training on resting blood pressure: individual participant data meta-analysis. J Hypertens. 2019;37:1927–38.
Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89:327–34.
Hansford HJ, Parmenter BJ, McLeod KA, Wewege MA, Smart NA, Schutte AE, et al. The effectiveness and safety of isometric resistance training for adults with high blood pressure: a systematic review and meta-analysis. Hypertens Res. 2021;44:1373–84.
Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NC, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. 2016;39:88–94.
Jin YZ, Yan S, Yuan WX. Effect of isometric handgrip training on resting blood pressure in adults: a meta-analysis of randomized controlled trials. J Sports Med Phys Fitness. 2017;57:154–60.
Kelley GA, Kelley KS. Isometric handgrip exercise and resting blood pressure: a meta-analysis of randomized controlled trials. J Hypertens. 2010;28:411–8.
Kelley GA, Kelley KS, Stauffer BL. Isometric exercise and inter-individual response differences on resting systolic and diastolic blood pressure in adults: a meta-analysis of randomized controlled trials. Blood Press. 2021;30:310–21.
Loaiza-Betancur AF, Pérez Bedoya E, Montoya Dávila J, Chulvi-Medrano I. Effect of isometric resistance training on blood pressure values in a group of normotensive participants: a systematic review and meta-analysis. Sports Health. 2020;12:256–62.
López-Valenciano A, Ruiz-Pérez I, Ayala F, Sánchez-Meca J, Vera-Garcia FJ. Updated systematic review and meta-analysis on the role of isometric resistance training for resting blood pressure management in adults. J Hypertens. 2019;37:1320–33.
Owen A, Wiles J, Swaine I. Effect of isometric exercise on resting blood pressure: a meta analysis. J Hum Hypertens. 2010;24:796–800.
Global action plan on physical activity 2018–2030: more active people for a healthier world. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. https://apps.who.int/iris/bitstream/handle/10665/272722/9789241514187-eng.pdf.
Sharman JE, Smart NA, Coombes JS, Stowasser M. Exercise and sport science Australia position stand update on exercise and hypertension. J Hum Hypertens. 2019;33:837–43.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127-248.
Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2: e004473.
Badrov MB, Bartol CL, DiBartolomeo MA, Millar PJ, McNevin NH, McGowan CL. Effects of isometric handgrip training dose on resting blood pressure and resistance vessel endothelial function in normotensive women. Eur J Appl Physiol. 2013;113:2091–100.
Badrov MB, Freeman SR, Zokvic MA, Millar PJ, McGowan CL. Isometric exercise training lowers resting blood pressure and improves local brachial artery flow-mediated dilation equally in men and women. Eur J Appl Physiol. 2016;116:1289–96.
McGowan CL, Levy AS, Millar PJ, Guzman JC, Morillo CA, McCartney N, et al. Acute vascular responses to isometric handgrip exercise and effects of training in persons medicated for hypertension. Am J Physiol Heart Circ Physiol. 2006;291:H1797–802.
McGowan CL, Visocchi A, Faulkner M, Verduyn R, Rakobowchuk M, Levy AS, et al. Isometric handgrip training improves local flow-mediated dilation in medicated hypertensives. Eur J Appl Physiol. 2007;99:227–34.
Lin S, Lu X, Chen S, Ye F, Zhang J, Ma Y, et al. Human coronary collateral recruitment is facilitated by isometric exercise during acute coronary occlusion. J Rehabil Med. 2012;44:691–5.
Carlson DJ, McFarlane JR, Dieberg G, Smart NA, Nobuo H. Rate pressure product responses during an acute session of isometric resistance training: a randomized trial. J Hypertens Cardiol. 2017;2:1–11.
Ewing DJ, Irving JB, Kerr F, Kirby BJ. Static exercise in untreated systemic hypertension. Br Heart J. 1973;35:413–21.
Fisher ML, Nutter DO, Jacobs W, Schlant RC. Haemodynamic responses to isometric exercise (handgrip) in patients with heart disease. Br Heart J. 1973;35:422–32.
Lind AR, Williams CA. The control of blood flow through human forearm muscles following brief isometric contractions. J Physiol. 1979;288:529–47.
Stefadouros MA, Grossman W, el-Shahawy M, Witham C. The effect of isometric exercise on the left ventricular volume in normal man. Circulation. 1974;49(6):1185-9. https://doi.org/10.1161/01.cir.49.6.1185.
Lind AR. Cardiovascular responses to static exercise. (Isometrics, anyone?). Circulation. 1970;41(2):173-6. https://doi.org/10.1161/01.cir.41.2.173. PMID: 5412979.
Wiley RL, Dunn CL, Cox RH, Hueppchen NA, Scott MS. Isometric exercise training lowers resting blood pressure. Med Sci Sports Exerc. 1992;24:749–54.
Pescatello LS, Buchner DM, Jakicic JM, Powell KE, Kraus WE, Bloodgood B, et al. Physical activity to prevent and treat hypertension: a systematic review. Med Sci Sports Exerc. 2019;51:1314–23.
Brown SP, Miller WC, Eason JM. Exercise physiology: basis of human movement in health and disease. Philadelphia: Lippincott Williams & Wilkins; 2006.
Baross AW, Wiles JD, Swaine IL. Effects of the intensity of leg isometric training on the vasculature of trained and untrained limbs and resting blood pressure in middle-aged men. Int J Vasc Med. 2012;2012: 964697.
MacDonald JR. Potential causes, mechanisms, and implications of post exercise hypotension. J Hum Hypertens. 2002;16:225–36.
Dinenno FA, Tanaka H, Monahan KD, Clevenger CM, Eskurza I, DeSouza CA, et al. Regular endurance exercise induces expansive arterial remodelling in the trained limbs of healthy men. J Physiol. 2001;534(Pt 1):287–95.
Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, Elliott WJ, et al. Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the american heart association. Hypertension. 2013;61:1360–83.
Rowell LB. Human cardiovascular control. New York: Oxford University Press; 1993.
Goldring N, Wiles JD, Coleman D. The effects of isometric wall squat exercise on heart rate and blood pressure in a normotensive population. J Sports Sci. 2014;32:129–36.
Wiles JD, Allum SR, Coleman DA, Swaine IL. The relationships between exercise intensity, heart rate, and blood pressure during an incremental isometric exercise test. J Sports Sci. 2008;26:155–62.
Millar PJ, McGowan CL, Cornelissen VA, Araujo CG, Swaine IL. Evidence for the role of isometric exercise training in reducing blood pressure: potential mechanisms and future directions. Sports Med. 2014;44:345–56.
Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ. 2010;340: c221.
Stewart GB, Altman DG, Askie LM, Duley L, Simmonds MC, Stewart LA. Statistical analysis of individual participant data meta-analyses: a comparison of methods and recommendations for practice. PLoS ONE. 2012;7: e46042.
Tierney JF, Vale C, Riley R, Smith CT, Stewart L, Clarke M, et al. Individual participant data (IPD) meta-analyses of randomised controlled trials: guidance on their use. PLoS Med. 2015;12: e1001855.
Wong GW, Boyda HN, Wright JM. Blood pressure lowering efficacy of beta-1 selective beta blockers for primary hypertension. Cochrane Database Syst Rev. 2016;3(3):CD007451. https://doi.org/10.1002/14651858.CD007451.pub2. PMID: 26961574; PMCID: PMC6486283.
Baffour-Awuah B, Pearson MJ, Smart NA, Dieberg G. Safety, efficacy and delivery of isometric resistance training as an adjunct therapy for blood pressure control: a modified Delphi study. Hypertens Res. 2022;45:483–95.
Crisafulli A, Marongiu E, Ogoh S. Cardiovascular reflexes activity and their interaction during exercise. Biomed Res Int. 2015;2015: 394183.
Raven PB, Fadel PJ, Ogoh S. Arterial baroreflex resetting during exercise: a current perspective. Exp Physiol. 2006;91:37–49.
Jae SY, Fernhall B, Heffernan KS, Kang M, Lee MK, Choi YH, et al. Exaggerated blood pressure response to exercise is associated with carotid atherosclerosis in apparently healthy men. J Hypertens. 2006;24:881–7.
Wahab KA, MA. Is an exaggerated blood pressure response to exercise in hypertensive patients a benign phenomenon or a dangerous alarm? Eur J Prev Cardiol. 2016;23:572–6.
Perçuku L, Bajraktari G, Jashari H, Bytyçi I, Ibrahimi P, Henein MY. Exaggerated systolic hypertensive response to exercise predicts cardiovascular events: a systematic review and meta-analysis. Pol Arch Intern Med. 2019;129:855–63.
Silva GO, Farah BQ, Germano-Soares AH, Andrade-Lima A, Santana FS, Rodrigues SL, et al. Acute blood pressure responses after different isometric handgrip protocols in hypertensive patients. Clinics (Sao Paulo). 2018;73: e373.
Wiles JD, Taylor K, Coleman D, Sharma R, O’Driscoll JM. The safety of isometric exercise: Rethinking the exercise prescription paradigm for those with stage 1 hypertension. Medicine (Baltimore). 2018;97: e0105.
Keller K, Stelzer K, Ostad MA, Post F. Impact of exaggerated blood pressure response in normotensive individuals on future hypertension and prognosis: systematic review according to PRISMA guideline. Adv Med Sci. 2017;62:317–29.
Dobson JL, Gladden LB. Effect of rhythmic tetanic skeletal muscle contractions on peak muscle perfusion. J Appl Physiol. 1985;2003(94):11–9.
Franklin BA, Gordon S, Timmis GC. Exercise prescription for hypertensive patients. Ann Med. 1991;23:279–87.
Lavie CJ, Milani RV, Marks P, de Gruiter H. Exercise and the heart: risks, benefits, and recommendations for providing exercise prescriptions. Ochsner J. 2001;3:207–13.
Baross AW, Wiles JD, Swaine IL. Double-leg isometric exercise training in older men. Open Access J Sports Med. 2013;4:33–40.
Devereux GR, Wiles JD, Swaine I. Markers of isometric training intensity and reductions in resting blood pressure. J Sports Sci. 2011;29:715–24.
Gladwell VF, Coote JH. Heart rate at the onset of muscle contraction and during passive muscle stretch in humans: a role for mechanoreceptors. J Physiol. 2002;540(Pt 3):1095–102.
Iellamo F, Legramante JM, Raimondi G, Castrucci F, Damiani C, Foti C, et al. Effects of isokinetic, isotonic and isometric submaximal exercise on heart rate and blood pressure. Eur J Appl Physiol Occup Physiol. 1997;75:89–96.
Kenney MJ, Seals DR. Postexercise hypotension. Key features, mechanisms, and clinical significance. Hypertension. 1993;22(5):653-64. https://doi.org/10.1161/01.hyp.22.5.653. PMID: 8225525.
Albert CM, Mittleman MA, Chae CU, Lee IM, Hennekens CH, Manson JE. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med. 2000;343:1355–61.
Garber CE, Carleton RA, Camaione DN, Heller GV. The threshold for myocardial ischemia varies in patients with coronary artery disease depending on the exercise protocol. J Am Coll Cardiol. 1991;17:1256–62.
Lin S, Chen Y, Li Y, Li J, Lu X. Physical ischaemia induced by isometric exercise facilitated collateral development in the remote ischaemic myocardium of humans. Clin Sci (Lond). 2014;127:581–8.
Verma S, Fedak PW, Weisel RD, Butany J, Rao V, Maitland A, et al. Fundamentals of reperfusion injury for the clinical cardiologist. Circulation. 2002;105:2332–6.
Salam A, Atkins ER, Hsu B, Webster R, Patel A, Rodgers A. Efficacy and safety of triple versus dual combination blood pressure-lowering drug therapy: a systematic review and meta-analysis of randomized controlled trials. J Hypertens. 2019;37:1567–73.
Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387:435–43.
Miller KB, Miller VM, Harvey RE, Ranadive SM, Joyner MJ, Barnes JN. Augmented cerebral blood velocity in response to isometric handgrip exercise in women with a history of preeclampsia. Am J Physiol Regul Integr Comp Physiol. 2019;317:R834–9.
Hess NC, Smart NA. Isometric exercise training for managing vascular risk factors in mild cognitive impairment and Alzheimer’s disease. Front Aging Neurosci. 2017;9:48.
Soares KB, Gallarreta FM, Neme WS. Fetal hemodynamic response to maternal isometric exercise. Open J Obstet Gynecol. 2018;8:541–52.
Lea JWD, O’Driscoll JM, Coleman DA, Wiles JD. Validity and reliability of RPE as a measure of intensity during isometric wall squat exercise. J Clin Transl Res. 2021;7:248–56.
Lea JW, O’Driscoll JM, Coleman DA, Wiles JD. Validity and reliability of the ‘Isometric Exercise Scale’ (IES) for measuring ratings of perceived exertion during continuous isometric exercise. Sci Rep. 2021;11:5334.
Carraça EV, Mackenbach JD, Lakerveld J, Rutter H, Oppert JM, De Bourdeaudhuij I, et al. Lack of interest in physical activity: individual and environmental attributes in adults across Europe: the SPOTLIGHT project. Prev Med. 2018;111:41–8.
Schutzer KA, Graves BS. Barriers and motivations to exercise in older adults. Prev Med. 2004;39:1056–61.
Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34:1996–2001.
Funding
This work was supported by a University of New England International Postgraduate Research Award (UNE IPRA) scholarship received by Biggie Baffour-Awuah for her PhD research.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this work—conception and design (BBA, MJP, GD, and NAS), acquisition of data and interpretation of data (BBA, MJP, GD, JDW and NAS), drafting the article (BBA, NAS) and critically revising it (MJP, GD, JDW). All authors approved the final version of this article and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Baffour-Awuah, B., Pearson, M.J., Dieberg, G. et al. An evidence-based guide to the efficacy and safety of isometric resistance training in hypertension and clinical implications. Clin Hypertens 29, 9 (2023). https://doi.org/10.1186/s40885-022-00232-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40885-022-00232-3