Abstract
Background
Previous studies have suggested that the effects of medical interventions tend to diminish over time. We investigated whether the effects of blood pressure lowering treatment on all-cause mortality and stroke have diminished over time.
Methods
We conducted meta-regression analyses. We extracted the target trials from two recently published comprehensive systematic reviews and meta-analyses. Adopted variables were relative risk (RR) of all-cause mortality and stroke, trial start year, mean age, sample size, baseline systolic blood pressure (SBP), difference in attained SBP reduction between intervention groups and control groups (SBP difference), and regional dummies. We implemented single meta-regressions, in which the dependent variable was the log of RR and the explanatory variable was each of other adopted variables. We also conducted multiple meta-regressions, in which the dependent variable was the log of RR and explanatory variables were all of other adopted variables. Our variable of greatest interest was trial start year.
Results
The included reviews assessed 85 trials with a total of 343,126 participants. Although trial start year was positively associated with the log of RR in the results of single meta-regressions, it lost significance in multiple meta-regressions for both all-cause mortality and stroke.
Conclusions
The effects of blood pressure lowering treatment on all-cause mortality and stroke have not diminished over time.
Similar content being viewed by others
Background
Previous studies suggest that the effects of medical interventions tend to diminish over time [1,2,3,4,5,6,7]. For example, recent analyses using meta-regression of the relevant trials suggested that the effects of antidepressants and cognitive behavioral therapy as treatments for depression diminished over time [8,9,10,11]. Nevertheless, whether this diminishing phenomenon can be observed in other medical fields seems to be underexplored.
Given this, we investigated whether the effects of blood pressure lowering treatments on all-cause mortality and stroke have diminished over time. Numerous clinical trials and meta-analyses indicated that blood pressure lowering treatments lessen serious cardiovascular events and all-cause mortality [12, 13]. To our knowledge, however, it has not been sufficiently explored in previous studies whether the effect of blood pressure lowering treatment has changed over time.
Therefore, the objective of this study was to examine whether the effects of blood pressure lowering treatment on all-cause mortality and stroke have diminished over time.
Methods
Ideas for inclusion of trials
Although there are several systematic reviews and meta-analyses regarding the effects of blood pressure lowering treatment on cardiovascular diseases and mortality, the most recent and comprehensive we are aware of are Ettehad et al. [13], which was published in 2016, and Brunström and Carlberg [14], which was published in 2018.
The Ettehad paper included a whole range of randomized controlled trials on blood pressure lowering treatment. The authors searched MEDLINE from January 1, 1966 till July 7, 2015. They also searched the medical literature and identified trials till November 9, 2015. Their search strategy was compatible to that of Law et al. [12] and used search terms related to hypertension, blood pressure, major classes of blood pressure lowering drugs (for example, diuretics), and the specific names of blood pressure lowering drugs listed in the British National Formulary. The studies Ettehad et al. included had a minimum of 1000 patient-years of follow-up in each trial group. The paper selected trials which compared active drug treatment groups with control groups, which mostly used placebo. The paper also selected trials which compared groups with different blood pressure targets. Although the paper did not exclude trials based on the existence of comorbidities at baseline, they excluded trials in patients with heart failure or left ventricular dysfunction.
The Brunström and Carlberg paper identified previous systematic reviews on the effect of blood pressure lowering from PubMed, the Cochrane Database of Systematic Reviews, and the Database of Abstracts of Reviews of Effect. They identified trials by scrutinizing reference lists from relevant reviews. They additionally searched PubMed and Cochrane Central Register for Controlled Trials in order to find trials after November 1, 2015 up till February 2017. The Brunström and Carlberg paper included mostly the same type of trials as the Ettehad paper, except for the following points. Unlike the Ettehad paper, the Brunström and Carlberg paper excluded trials in the acute phase after myocardial infarction from meta-analysis. They also excluded trials they deemed to be at high risk of bias. Unlike the Ettehad paper, which required a minimum of 1000 patient-years of follow-up for each trial group, the Brunström and Carlberg paper required a minimum of 1000 patient-years of follow-up for the whole study sample. We constructed our dataset for meta-analysis and meta-regression by adopting the trials included in these two papers. We used the names of included trials as used in the Ettehad paper and/or the Brunström and Carlberg paper.
Data extraction
One of the authors (YS) extracted the following data from each trial: trial start year, sample size of trial (number of total participants), number of events (all-cause mortality and stroke), mean age at baseline, mean systolic blood pressure (SBP) at baseline, difference in SBP reduction between the two groups, SBP reduction from the baseline in each group, attained SBP in each group, and the region in which each trial was carried out.
As defined in both the Ettehad paper and the Brunström and Carlberg paper, stroke included fatal and non-fatal stroke and excluded transient ischemic attack (TIA). In addition to data on stroke as a whole, we aimed to extract data on its subtypes (e.g., cerebral infarction, cerebral hemorrhage, and subarachnoid hemorrhage) from each trial and, where possible, performed analyses based on the subtypes. In the process of data extraction, we found that several papers covered only fatal stroke or non-fatal stroke. For these papers, we recorded the cases shown in each paper. We also found that several papers included TIA in the number of cases, and exclusion of TIA was not possible. In these cases, we extracted the number of cases including TIA.
As the Ettehad paper showed the number of events (all-cause mortality and stroke) in its appendix, we compared our extraction results with those of the Ettehad paper. When there were differences, we explored the causes of the differences. This exploration revealed that some data were different from those in the Ettehad paper. Regarding all-cause mortality, there were three differences compared with the Ettehad paper (Supp. Figure 11 [13]). In PREVEND IT [15], we calculated the number of non-cardiovascular deaths from the indicated ratio and added them to the cardiovascular death number. In BBB [16], we could not extract all-cause mortality data because it was not indicated in the paper. In EWPHE [17], we used the number from the intention-to-treat analysis. Regarding stroke, there were five differences compared with the Ettehad paper (Supp. Figure 8 [13]). In PHARAO [18], we added hemorrhage. In Oslo [19], we added fatal subarachnoidal hemorrhage. In JATOS [20], we subtracted the number of TIA. In EWPHE [17], we used the numbers from the intention-to-treat analysis. In the Hunan Province study [21], we used the data indicated in the original publication.
Regarding the variable to identify when each trial was carried out, we used the data of trial start year. To extract the trial start year, we first checked the papers for each trial. When we could not find the trial start year, we checked ClinicalTrials.gov. When these did not work, we emailed the corresponding or first author of the original papers.
Differences in the attained SBP reduction between intervention groups and control groups (hereinafter, “SBP difference”) were determined in the following way. We retrieved three patterns of figures for SBP difference: (1) difference in SBP reduction between the two groups, (2) SBP reduction from the baseline in each group, and (3) attained SBP in each group. We prioritized (1) when reported. If (1) was not reported, we calculated the difference from (2). If neither (1) nor (2) were reported, we calculated the difference from (3). We used mean figures of the whole measurements when reported. When plural measurements were reported and mean figures were not reported, we calculated the mean of plural measurements. When only graphs of SBP transition were shown, we calculated the SBP levels using an online tool [22]. Regarding the Lewis study [23], SBP data were extracted from Black et al. [24]. In BBB [16], the number in each group was not mentioned, so we split the total amount (N = 2127) and assumed both groups included 1064 participants.
The regions in which trials were carried out were categorized as follows: Asia, Europe, North America, Oceania, South America, and mixed regions. Trials carried out in two or more regions were included in the mixed region category. Turkey and Israel were included in Europe.
Statistical analysis
The statistical analyses in this study were carried out in the following two steps. First, we conducted single meta-regressions, in which the dependent variable was the log RR of all-cause mortality or stroke and the explanatory variable was each of the extracted variables, namely trial start year, sample size, age, baseline SBP, SBP difference, and region (Model 1M for all-cause mortality and Model 1S for stroke). RR was calculated by dividing the risk of outcome events of intervention groups by the risk of outcome events of control groups. Risk of outcome events of each group was calculated by dividing the number of participants experiencing outcome events by the number of participants. With regard to the variable of region, there were several variables for regional dummies in the model, but we included it in the table of single meta-regression because they all belonged to the regional category.
Second, we conducted multiple meta-regressions, in which the dependent variable was the log RR and the explanatory variables were all of the abovementioned variables (Model 2M for all-cause mortality and Model 2S for stroke). We judged whether the effects of blood pressure lowering treatment on all-cause mortality and stroke have diminished over time from Model 2M and Model 2S. Diminishing was confirmed only when the variable of trial start year was significant at the 5% level.
When there was no event in either group in a trial, we added 0.5 to the number of events and the number of non-events in both groups before performing the meta-regressions. All analyses were performed using STATA 15 (Stata Corp., College Station, TX, USA). For meta-regressions, we used the “metareg” command [25], which estimates the random-effects model via the restricted maximum likelihood method.
For trials with three or more arms, we followed the classification performed in the Ettehad paper or the Brunström and Carlberg paper. The two papers defined the control group in the ONTARGET study [26] differently; here, we followed the Brunström and Carlberg paper’s classification.
Results
Number of trials and participants
The list of all trials in our study is shown in Additional file 1: Table S1. Data for trial start year, sample size, mean age, mean baseline SBP, mean SBP difference of each trial, and the region in which each trial was carried out are also shown in Additional file 1: Table S1. Outcome events and the number of participants of intervention groups and control groups are shown in Additional file 2: Table S2 for all-cause mortality and in Additional file 3: Table S3 for stroke.
A total of 85 trials were selected, representing 343,126 participants. Among these, there were 82 trials for all-cause mortality and 74 trials for stroke. Summary statistics of the trials are shown in Table 1.
Results of meta-regressions for all-cause mortality
In Table 2, we reported the results of meta-regressions for all-cause mortality. The dependent variable was log RR of all-cause mortality. With the increase in RR, the effect of blood pressure lowering treatment is interpreted to decrease. In the table, exponentiated coefficients (exp(b)) instead of coefficients per se are reported. Exp(b) is the exponential of the unstandardized coefficient and shows a proportional change in RR per unit change in each explanatory variable. This makes more straightforward interpretation possible by denoting the multiplicative effects upon RR. If exp(b) is greater than 1, when the explanatory variable rises by one unit, RR increases (effect of blood pressure lowering treatment on all-cause mortality diminishes) by the ratio of exp(b) minus one. If exp(b) is smaller than 1, when the explanatory variable rises by one unit, RR falls (effect of blood pressure lowering treatment on all-cause mortality increases) by the ratio of one minus exp(b).
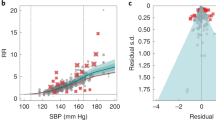
The results of single meta-regressions (Model 1M in Table 2), in which other explanatory variables were not adjusted for, are as follows. Regarding the trial start year, which was the explanatory variable of greatest interest, RR rose with the increase in trial start year; for every 10 years added to the trial start year, RR of all-cause mortality increased significantly by 5% (exp(b) = 1.05; 95% CI 1.02, 1.09; p = 0.004) in the case of no adjustment for other explanatory variables. For other explanatory variables, RR significantly grew with the rise in sample size and decreased with the enlarged SBP difference. RR was significantly lower in trials carried out in North America and Asia than in mixed region trials.
According to multiple meta-regression that included all of the explanatory variables, the association between trial start year and log RR of all-cause mortality lost significance (exp(b) = 1.05; 95% CI 0.99, 1.10; p = 0.078) after adjusting for other explanatory variables. Similarly, associations of log RR of all-cause mortality with sample size, SBP difference, and regional dummies for North America lost significance after adjusting for other explanatory variables. Trials in Asia still had a significantly lower log RR than mixed region trials after adjusting for other explanatory variables; RR of all-cause mortality of trials in Asia was 16% lower than mixed region trials (exp(b) = 0.84; 95% CI 0.73, 0.97; p = 0.020) after adjusting for other explanatory variables (Model 2M in Table 2).
As the trial start year variable was not significant at the 5% level in multiple meta-regression, we concluded that the effects of blood pressure lowering treatment on all-cause mortality have not diminished over time.
Results of meta-regressions for stroke
In Table 3, we reported the results of meta-regressions for stroke. The dependent variable was log RR of stroke. Results of single meta-regressions (Model 1S in Table 3), in which other explanatory variables were not adjusted for, are as follows. Regarding the trial start year which is the explanatory variable of greatest interest, RR rose with the increase in trial start year; for every 10 years added to the trial start year, RR of stroke grew significantly by 12% (exp(b) = 1.12; 95% CI 1.06, 1.19; p < 0.001) in the case of no adjustment for other explanatory variables. For other explanatory variables, RR significantly climbed with the rise in sample size and fell with the growing baseline SBP and SBP difference. RR was significantly lower in trials carried out in North America, Europe, and Asia than in mixed region trials.
According to multiple meta-regression that included all of the explanatory variables, the association between trial start year and log RR of stroke lost significance (exp(b) = 1.07; 95% CI 0.97, 1.19; p = 0.154) after adjusting for other explanatory variables. Similarly, associations of log RR of stroke with sample size, baseline SBP, and regional dummies for North America and Europe lost significance after adjusting for other explanatory variables. SBP difference still had a significant association with log RR; for every 10 mmHg increase in SBP difference, RR of stroke decreased significantly by 19% (exp(b) = 0.81; 95% CI 0.69, 0.94; p = 0.008) after adjusting for other explanatory variables. Trials in Asia still had a significantly lower log RR than mixed region trials after adjusting for other explanatory variables; RR of stroke for trials in Asia was 17% lower than mixed region trials (exp(b) = 0.83; 95% CI 0.70, 0.99; p = 0.042) after adjusting for other explanatory variables (Model 2S in Table 3).
As the trial start year variable was not significant at the 5% level in multiple meta-regression, we concluded that the effects of blood pressure lowering treatment on stroke have not diminished over time.
Regarding analyses by stroke subtypes, out of the 74 trials we covered, we found only five trials [20, 27,28,29,30] which indicated data based on ischemic type and hemorrhagic type. Hence, we discontinued our analyses of stroke subtypes.
Discussion
In this study, we investigated whether the effects of blood pressure lowering treatment on all-cause mortality and stroke have diminished over time by performing meta-regressions in which log RRs of the outcome events were the dependent variable and trial start year was the explanatory variable of greatest interest. Although trial start year was positively associated with log RR in the results of single meta-regressions, it lost significance in multiple meta-regressions which adjusted for mean age, sample size, baseline SBP, SBP difference, and regional dummies for both all-cause mortality and stroke. We concluded that the effects of blood pressure lowering treatment on all-cause mortality and stroke have not diminished over time from the results of the multiple meta-regressions.
In this study, we used the data of trial start year instead of year of publication as the variable to identify when each trial was performed. One problem in using data of trial start year was that some studies do not report this variable in published papers. Although we did our best to identify trial start year by checking the ClinicalTrials.gov website and emailing the corresponding authors, we were still unable to identify the trial start year for three trials. This may have caused some bias and/or lessened statistical power.
In this study, SBP difference (difference in attained SBP reduction between intervention groups and control groups) was not associated with risk reduction of all-cause mortality in multiple meta-regression. Although Ettehad et al. [13] indicated that there was a significant association between the extent of SBP reduction and improved RR outcome in all-cause mortality from single meta-regression analysis, and we also found similar results in our single meta-regression, the results gained from single meta-regression were not supported by multiple meta-regression analysis as done in this study. By contrast, our results on stroke, which showed that SBP difference was associated with a lower RR of stroke in both single and multiple meta-regressions, support and strengthen the findings of Ettehad et al. [13] and another meta-regression analysis [31].
In this study, trials in Asia showed significantly lower RR compared with mixed region trials in both all-cause mortality and stroke. Of the 11 trials carried out in Asia, six were from China, four from Japan, and one from Hong Kong and Japan. The reasons why such higher effects are shown in Asia need to be explored in future studies.
There are several limitations to this study. First, we included the trials covered by two recent comprehensive systematic reviews. Additional trials not covered by the included systematic reviews may alter these findings. Second, the definition of stroke varied among trials. Variation in definition may have caused biases in our meta-regression on stroke. Third, since most trials included participants with comorbidities, the trials covered in this study might be heterogeneous. Fourth, we assumed a linear relationship between log RRs and trial start year. This assumption may be questioned, and the analysis could be improved by better reflecting the behavior of the data when constructing the model. Fifth, adjusted R2 for multiple regressions was not large enough (68.9% for all-cause mortality and 79.8% for stroke), suggesting the possibility of other important factors which would substantially change the results of this paper.
Conclusions
The effects of blood pressure lowering treatment on all-cause mortality and stroke have not diminished over time.
Abbreviations
- CI:
-
Confidence interval
- RR:
-
Relative risk
- SBP difference:
-
Difference in attained SBP reduction between intervention groups and control groups
- SBP:
-
Systolic blood pressure
- TIA:
-
Transient ischemic attack
References
Gehr BT, Weiss C, Porzsolt F. The fading of reported effectiveness. A meta-analysis of randomised controlled trials. BMC Med Res Methodol. 2006;6:25.
Protzko J, Schooler JW. Decline Effects. In: Lilienfeld SO, Waldman, editors. Psychological Science Under Scrutiny. West Sussex: Wiley-Blackwell; 2017. p. 85–107.
Baker R, Jackson D. Inference for meta-analysis with a suspected temporal trend. Biom J. 2010;52:538–51. https://doi.org/10.1002/bimj.200900307.
Ioannidis JPA. Evolution and translation of research findings: from bench to where. PLoS Clin Trials. 2006;1:e36. https://doi.org/10.1371/journal.pctr.0010036.
Dogo SH, Clark A, Kulinskaya E. Sequential change detection and monitoring of temporal trends in random-effects meta-analysis. Res Synth Methods. 2017;8:220–35. https://doi.org/10.1002/jrsm.1222.
Fanshawe TR, Shaw LF, Spence GT. A large-scale assessment of temporal trends in meta-analyses using systematic review reports from the Cochrane library. Res Synth Methods. 2017;8:404–15. https://doi.org/10.1002/jrsm.1238.
Trikalinos TA, Ioannidis J. Assessing the evolution of effect sizes over time. In: Rothstein HR, Sutton AJ, Borenstein M, editors. Publication bias in meta-analysis: prevention, assessment and adjustments. West Sussex: Wiley-Blackwell; 2005. p. 241–59.
Johnsen TJ, Friborg O. The effects of cognitive behavioral therapy as an anti-depressive treatment is falling: a meta-analysis. Psychol Bull. 2015;141:747–68. https://doi.org/10.1037/bul0000015.
Leucht S, Hierl S, Kissling W, Dold M, Davis JM. Putting the efficacy of psychiatric and general medicine medication into perspective: review of meta-analyses. Br J Psychiatry. 2012;200:97–106. https://doi.org/10.1192/bjp.bp.111.096594.
Jakobsen JC, Katakam KK, Schou A, Hellmuth SG, Stallknecht SE, Leth-Moller K, et al. Selective serotonin reuptake inhibitors versus placebo in patients with major depressive disorder. A systematic review with meta-analysis and Trial sequential analysis. BMC Psychiatry. 2017;17:58. https://doi.org/10.1186/s12888-016-1173-2.
Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391:1357–66. https://doi.org/10.1016/s0140-6736(17)32802-7.
Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. 2009;338:BMJ. https://doi.org/10.1136/bmj.b1665.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67. https://doi.org/10.1016/s0140-6736(15)01225-8.
Brunström M, Carlberg B. Association of Blood Pressure Lowering with Mortality and Cardiovascular Disease across Blood Pressure Levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178:28–36. https://doi.org/10.1001/jamainternmed.2017.6015.
Asselbergs FW, Diercks GF, Hillege HL, van Boven AJ, Janssen WM, Voors AA, et al. Effects of fosinopril and pravastatin on cardiovascular events in subjects with microalbuminuria. Circulation. 2004;110:2809–16. https://doi.org/10.1161/01.CIR.0000146378.65439.7A.
Hansson L. The BBB study: the effect of intensified antihypertensive treatment on the level of blood pressure, side-effects, morbidity and mortality in “well-treated” hypertensive patients. Blood Press. 1994;3:248–54. https://doi.org/10.3109/08037059409102265.
Amery A, Berthaux P, Birkenhäger W, Boel A, Brixko P, Bulpitt C, et al. Antihypertensive therapy in patients above age 60 years (fourth interim report of the European working party on high blood pressure in elderly: EWPHE). Clin Sci. 1978;55:263s–70s. https://doi.org/10.1042/cs055263s.
Luders S, Schrader J, Berger J, Unger T, Zidek W, Bohm M, et al. The PHARAO study: prevention of hypertension with the angiotensin-converting enzyme inhibitor ramipril in patients with high-normal blood pressure: a prospective, randomized, controlled prevention trial of the German hypertension league. J Hypertens. 2008;26:1487–96. https://doi.org/10.1097/HJH.0b013e3282ff8864.
Helgeland A. Treatment of mild hypertension: a five year controlled drug trial. The Oslo study Am J Med. 1980;69:725–32.
Jatos Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertens Res. 2008;31:2115. https://doi.org/10.1291/hypres.31.2115.
Sun M, Zhou H, Jia Z. Prevention and treatment of stroke after hypertension for ten years in Hunan Province. Zhonghua Nei Ke Za Zhi. 1997;36:312–4.
Rohatgi A. WebPlotDigitizer. 2018. https://automeris.io/WebPlotDigitizer. Accessed 3 Aug 2018.
Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med. 1993;329:1456–62. https://doi.org/10.1056/nejm199311113292004.
Black HR, editor. Clinical trials in hypertension. New York: Marcel Dekker Inc; 2001.
Harbord RM, Higgins J. Meta-regression in Stata. Stata J. 2008;8:493–519.
The ONTARGET Investigators. Telmisartan, Ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547–59. https://doi.org/10.1056/NEJMoa0801317.
Yusuf S, Diener HC, Sacco RL, Cotton D, Ounpuu S, Lawton WA, et al. Telmisartan to prevent recurrent stroke and cardiovascular events. N Engl J Med. 2008;359:1225–37. https://doi.org/10.1056/NEJMoa0804593.
The SPS3 Study Group. Blood-pressure targets in patients with recent lacunar stroke: the SPS3 randomised trial. Lancet. 2013;382:507–15. https://doi.org/10.1016/S0140-6736(13)60852-1.
PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033–41. https://doi.org/10.1016/S0140-6736(01)06178-5.
Yusuf S, Healey JS, Pogue J, Chrolavicius S, Flather M, Hart RG, et al. Irbesartan in patients with atrial fibrillation. N Engl J Med. 2011;364:928–38. https://doi.org/10.1056/NEJMoa1008816.
Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. 2014;32:2285–95. https://doi.org/10.1097/HJH.0000000000000378.
Acknowledgements
The authors would like to thank Yoshiko Mizuno and Kazuhiro Uchimura for their invaluable help with the manuscript.
Funding
This work was supported by the Research Institute of Economy, Trade and Industry, Japan. The institute had no role in the study design, data analyses, decision to publish, or preparation of the manuscript.
Availability of data and materials
All data generated or analyzed during the current study are included in this published paper and its additional files.
Author information
Authors and Affiliations
Contributions
YS and YK drafted the manuscript. YS extracted the data. YK performed the analyses. All authors read, provided feedback and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Table S1. Summary of Included Trials. (DOCX 31 kb)
Additional file 2:
Table S2. Summary of Outcome Events on All-cause Mortality. (DOCX 28 kb)
Additional file 3:
Table S3. Summary of Outcome Events on Stroke. (DOCX 28 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sekizawa, Y., Konishi, Y. & Kimura, M. Are the effects of blood pressure lowering treatment diminishing?: meta-regression analyses. Clin Hypertens 24, 16 (2018). https://doi.org/10.1186/s40885-018-0101-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40885-018-0101-9