Abstract
Background
Improving women’s access to and use of modern contraceptives is a key global strategy for improving the sexual and reproductive health of women. However, the use of modern contraceptives among adolescent girls and young women in sub-Saharan Africa (SSA) remains relatively low, despite the numerous interventions to increase patronage. This study examined adolescent girls and young women’s receipt of quality contraceptive counselling and its associated factors in SSA.
Methods
Data for the study were extracted from the recent Demographic and Health Surveys of 20 countries in SSA, spanning from 2015 to 2021. A sample of 19,398 adolescent girls and young women aged 15 to 24 years was included in the study. We presented the proportion of adolescent girls and young women who received quality contraceptive counselling using a spatial map. Multilevel binary logistic regression analysis was carried out to examine the factors associated with the receipt of quality contraceptive counselling.
Results
Overall, 33.2% of adolescent girls and young women had access to quality contraceptive counselling, ranging from 13.0% in Cameroon to 67.0% in Sierra Leone. The odds of receiving quality contraceptive counselling was higher among adolescent girls and young women aged 20–24 (AOR = 1.48, CI: 1.32–1.67), those with primary (AOR = 1.32, CI: 1.11–1.57) and secondary or higher education (AOR = 1.31, CI: 1.09–1.58), and those married (AOR = 1.32, CI: 1.15–1.52), cohabiting (AOR = 1.47, CI: 1.23–1.76), and previously married (AOR = 1.48, CI: 1.20–1.83) compared to their counterparts in the reference groups. Adolescent girls and young women who were currently working (AOR = 1.22, CI: 1.09–1.37), those who heard of family planning from radio in the last few months (AOR = 1.34, CI:1.21–1.50), those who visited the health facility in the last 12 months (AOR = 1.69, CI: 1.52–1.88), and those residing in the Southern (AOR = 5.01, CI: 3.86–6.51), Eastern (AOR = 2.54, CI: 1.96–3.30), and Western (AOR = 4.09, CI: 3.19–5.25) SSA were more likely to receive quality contraceptive counselling compared to their counterparts in the reference groups. Conversely, adolescent girls and young women who used the internet, those who had problem getting permission to seek medical help, those facing problem in seeking medical help for not wanting to go alone, those from the middle and richest wealth indices, and those from the rural areas were less likely to receive quality contraceptive counselling compared to their counterparts in the reference groups.
Conclusion
Receipt of quality contraceptive counselling among adolescent girls and young women was low. Considering the importance of quality contraceptive counselling on the uptake and continuation of contraception, policymakers need to institute measures that improve adolescent girls and young women’s access to quality contraceptive counselling in SSA, especially in countries like Cameroon, Angola, Madagascar, Mauritania, and Guinea, taking into consideration the factors identified in the study. Increasing adolescent girls and young women’s access to quality contraceptive counselling could greatly minimize the risk of unintended pregnancies and its associated maternal and child health burden in SSA and subsequently contribute to the attainment of the Sustainable Development Goal 3, target 3.7.
Similar content being viewed by others
Introduction
Generally, improving women’s access to and use of modern contraceptives remains a major public health strategy for reducing the burden of sexual and reproductive health problems [1, 2]. As such, the Sustainable Development Goal (SDG) 3, target 3.7 emphasizes the need to increase access and use of modern contraceptives among women of reproductive age (15–49 years) worldwide, with adolescent girls and young women aged 15–24 constituting an important aspect [1]. However, despite numerous interventions aimed at improving access to and use of modern contraceptives, the unmet need for contraception among women in sub-Saharan Africa (SSA) remains high [2]. Poor access to quality contraceptives may contribute to low contraception uptake and early discontinuation among women in SSA [3]. Therefore, quality contraceptive counselling remains one of the most viable approaches to improving the use of modern contraceptives among adolescent girls and young women in SSA [4].
Most high-income countries are observing a surge in the prevalence of contraceptive use, providing them an advantage in their quest to achieve SDG 3.7, possibly through the acquisition of knowledge and the provision of access to reliable information, suitable family planning services, and counselling [5, 6]. Evidence from a study conducted in 23 countries in Latin America and the Caribbean indicates that significant progress has been made towards boosting the use of contraceptives [7]. Major attempts are made with regular surveys to assess their success despite some existing gaps, such as improving contraceptive method choice and the use of modern contraceptives to meet family planning needs [8, 9]. With the advancement in the accessibility of high-quality contraceptive information and counseling, individuals now have the ability to decide on the number and spacing of their children. This is achievable through family planning, which also has numerous positive impacts on women’s education and empowerment [7, 10].
However, the rates of inadequate family planning and lack of information on contraceptives are still prevalent in low-and middle-income countries, where one in four women of childbearing age are at risk of unwanted pregnancies or unable to delay childbirth [11]. Although 218 million women of reproductive age in low- and middle-income countries lacked access to contraception in 2019, addressing this issue could significantly reduce the number of unplanned pregnancies, illegal abortions, and maternal deaths from 299,000 to 113,000 annually [10]. Decreasing the unmet need for contraception can be achieved by selecting a family planning method that meets their needs and expectations, minimizes side effects, and is consistently used, or by considering alternative options [8, 12]. In SSA, there is currently a public health crisis as many contraceptive users either stop using their chosen methods or fail to use them correctly due to inadequate contraceptive counselling [13, 14].
There is a varied prevalence of informed contraceptive method choices across the globe [15]. Despite government objectives, a study conducted in 32 countries in SSA demonstrates that the prevalence of informed contraceptive method choice is low, with substantial country variations [16]. The low level of knowledge about contraceptive method choice in SSA is influenced by various factors, such as maternal age, residency, financial status, media exposure, internet use, marital status, education, occupational status, access to health facility, and access to contraceptives [17,18,19]. This misperception about contraceptives is a significant public health issue, and it affects the prevalence of contraceptive access and use in SSA, which remains unacceptably low [20].
Access to quality contraceptive counselling in SSA is crucial for improving the health and wellbeing of adolescent girls and young women. It also helps to emphasize the importance of educating women to increase their use of modern contraceptives [20, 21]. Modern contraceptives have several advantages, such as protecting against unwanted pregnancies and mortality from unsafe abortions, both of which are prevalent issues in SSA [21, 22]. Given that SSA has a 22.0% prevalence of modern contraceptive use [20], it is essential to ensure that contraceptive counselling is readily available to women of reproductive age.
Despite the availability of resources in SSA like youth-friendly services that provide information on development, unsafe abortion, gender-based violence, sexuality, and family planning, they are not readily accessible [23, 24]. This study sought to examine adolescent girls and young women’s receipt of quality contraceptive information and its associated in SSA. Findings from this study would extend evidence on the need to improve access to quality contraceptive counselling among adolescent girls and young women.
Methods
Data source
Data for the study were pooled from the recent Demographic and Health Surveys (DHS) of 20 countries in SSA, spanning from 2015 to 2021. Table 1 contains the list of countries included in the study. We extracted the data from the individual recode files of each of the 20 countries, which can be accessed from the DHS Program [25]. Within the stipulated timeframe (2015–2021), only 20 countries had data on the variables of interest. DHS is a nationally representative survey that has been conducted in over 90 low-and middle-income countries worldwide since its inception [26]. The DHS employed a cross-sectional design with respondents sampled using a two-stage cluster sampling technique. Detailed explanation of the survey methodology can be found in the literature [27, 28]. DHS utilised well-validated questionnaires to collect data from the respondents, with trained data collectors administering the questionnaire. We included a sample of 19,398 adolescent girls (15–19 years) and young women (20–24 years) in the study. This paper was written following the Strengthening Reporting of Observational Studies in Epidemiology (STROBE) guidelines [29].
Variables
Receipt of quality contraceptive counselling was the outcome variable. This variable was measured as a composite variable from three questions, which form the basis of the Method Information Index in quality counselling [18, 30, 31]. In the DHS, women were asked to indicate whether they were told about side effects, how to deal with side effects, and other family planning methods during their family planning counselling services. The response options were “no” and “yes”. We created an index using the responses from the three indicators, with a score of three (3) showing that the respondent received quality contraceptive counselling whilst a score of two (2) or less demonstrates no quality counselling [30, 31]. We coded the quality contraceptive counselling as “1 = yes” and no quality counselling as “0 = no” in the final analysis.
Twenty explanatory variables were included in the study. We selected these variables for inclusion in the study based on their influence on the receipt of quality family planning or contraceptive counselling from the review of pertinent literature [18, 30,31,32,33] and their availability in the DHS dataset. The variables consisted of the age of the adolescent girls and young women, level of education, marital status, current working status, watch television, listen to radio, read newspapers or magazines, heard of family planning from newspaper or magazine last few months, heard of family planning from the radio last few months, heard of family planning from television last few months. Others were internet usage, getting medical help for self: permission to go, getting medical help for self: distance to health facility, getting medical help for self: getting money for treatment, getting medical help for self: not wanting to go alone, visit to health facility in the last 12 months, sex of household head, household wealth index, place of residence, and geographical sub-region. For geographical sub-region, all the 20 countries included in the study were grouped into Southern SSA (South Africa, Zambia, and Zimbabwe), Central SSA (Angola and Cameroon), Eastern SSA (Burundi, Ethiopia, Madagascar, Malawi, Rwanda, Uganda, and Tanzania), and Western SSA (Benin, Gambia, Guinea, Liberia, Mali, Mauritania, Nigeria, and Sierra Leone). The last four variables were grouped as contextual level variables (household and community level variables) whilst the remaining variables were termed as individual-level variables.
Statistical analyses
Data analyses were conducted using Stata software, version 17.0 (Stata Corporation, College Station, TX, USA). We used a spatial map to present the proportion of adolescent girls and young women who received quality contraceptive counselling. Next, we performed a bivariate analysis of the distribution of quality contraceptive counselling across the explanatory variables and used chi-square test of to examine the independent associations between the explanatory and outcome variables. All the variables with p-values < 0.05 from the chi-square test were considered statistically significant and placed in a regression model. We utilised a multilevel binary logistic regression analysis to examine the factors associated with the receipt of quality contraceptive counselling. Four models (Model 0-III) were developed. Model 0 was the model with no explanatory variable, and the results showed the variation in the outcome variable, attributed to the primary sampling unit. Model I, Model II, and Model III included the individual level, contextual level, and all explanatory variables, respectively. Model 0 had random effects results while Models I, II, and III included fixed and random effects results. The fixed effect results showed the association between the explanatory variables and the outcome variable. The results were presented using adjusted odds ratio (AOR) with their respective 95% confidence intervals (CIs). The random effects results denoted the measure of variation in the outcome variable based on the primary sampling unit (measured by Intra-Cluster Correlation Coefficient [ICC]). The Akaike Information Criterion (AIC) and the log-likelihood were used to check for model fitness, or how well different models matched the data. The model with the least AIC and highest log-likelihood was chosen as the best-fitted model for the study and its results were interpreted and discussed. The multilevel regression analysis was conducted using the “melogit” command in Stata. Statistical significance was set at p < 0.05. All the analyses were weighted to adjust for disproportionate sampling and the svyset command was employed to cater for the complex nature of the DHS data.
Ethical consideration
This study utilised publicly available secondary data from the DHS Program. Hence, ethical clearance was not sought for the study. We obtained permission to use the dataset from the Monitoring and Evaluation to Assess and Use Results Demographic and Health Surveys (MEASURE DHS). The detailed ethical issues regarding the DHS are freely available at http://goo.gl/ny8T6X.
Results
Receipt of quality contraceptive counselling
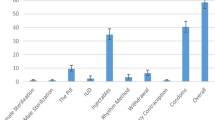
Overall, 33.2% [32.1, 34.2] of adolescent girls and young women received quality contraceptive counselling (Table 2), which ranges from 13.0% in Cameroon to 67.0% in Sierra Leone. Aside from Sierra Leone, more than half of adolescent girls and young women in Gambia (51.8%), Malawi (59.5%), and Zambia (60.3%) received quality contraceptive counselling. On the other hand, less than 20% of adolescent girls and young women in Cameroon (13%), Angola (14.7%), Madagascar (15.7%), Mauritania (16.3%), and Guinea (19.5%) received quality contraceptive counselling (Fig. 1).
Bivariate results of receipt of contraceptive counselling
Table 2 shows the distribution of quality contraceptive counselling across the explanatory variables in SSA. All the explanatory variables were significantly associated with quality contraceptive counselling among adolescent girls and young women at p < 0.05, except listening to radio, heard of family planning from newspapers or magazines in the last few months, heard of family planning from television in the last few months, and have no distance-related problem in getting medical help. A greater proportion of the adolescent girls and young women from the Central part of SSA (86.1%), those never in union (76.0%), those aged 15–19 (75.1%), those who did not visit a health facility in the last 12 months (75.1%), those who use the internet (73.7%), and those having a problem with getting permission to seek medical help (72.5%) received no quality contraceptive counselling.
Factors associated with receipt of quality contraceptive counselling
Table 3 presents the results of the factors associated with receipt of quality contraceptive counselling among adolescent girls and young women in SSA. With the lowest AIC and highest log-likelihood values, Model III was considered the best fitted model and the interpretations of the results were based on that model. The results showed the odds of recieving quality contraceptive counseling was higher among young women aged 20–24 (AOR = 1.48, CI: 1.32–1.67) compared to adolescent girls (15–19). Adolescent girls and young women who had primary (AOR = 1.32, CI: 1.11–1.57) and secondary or higher education (AOR = 1.31, CI: 1.09–1.58) were more likely to receive quality contraceptive counselling compared to those who had no education. Married (AOR = 1.32, CI: 1.15–1.52), cohabiting (AOR = 1.47, CI: 1.23–1.76), and previously married (AOR = 1.48, CI: 1.20–1.83) adolescent girls and young women were more likely to receive quality contraceptive counselling relative to those who had never being in union. The odds of receiving quality contraceptive counselling was higher among currently working adolescent girls and young women compared to those who were not working (AOR = 1.22, CI: 1.09–1.37). Additionally, the odds of receipt of quality contraceptive counselling was higher among adolescent girls and young women who heard of family planning from radio in the last few months (AOR = 1.34, CI:1.21–1.50), visited a health facility in the last 12 months (AOR = 1.69, CI: 1.52–1.88), and those residing in the Southern (AOR = 5.01, CI: 3.86–6.51), Eastern (AOR = 2.54, CI: 1.96–3.30), and Western (AOR = 4.09, CI: 3.19–5.25) parts of SSA. Meanwhile, those who use the internet (AOR = 0.78, CI: 0.67–0.91), had problems getting permission to seek medical help (AOR = 0.83, CI: 0.72–0.97), had problems in seeking medical help for not wanting to go alone (AOR = 0.79, CI: 0.70–0.89), those from the middle (AOR = 0.80, CI: 0.68–0.94) and richest (AOR = 0.80, CI: 0.64–0.99) wealth index, and those in rural areas (AOR = 0.85, CI: 0.73–0.99) were less likely to receive quality contraceptive counselling.
Discussion
In this study, we found that the proportion of adolescent girls and young women who received quality contraceptive counselling in SSA is low (33.2%), ranging from 13% in Cameroon to 67% in Sierra Leone. Aside from Sierra Leone, only Zambia, Malawi, and Gambia had more than half of their adolescent girls and young women receiving quality contraceptive counselling. Meanwhile, about 80% of the adolescent girls and young women in Cameroon, Angola, Madagascar, Mauritania, and Guinea did not receive quality contraceptive counselling. Further, we found that age, education, marital status, employment, media exposure, healthcare access, and geographic location were significantly associated with receipt of quality contraceptive counselling among adolescent girls and young women.
In concordance with the findings from previous studies [30, 34, 35], we found that most adolescent girls and young women in SSA do not receive quality contraceptive counselling. Perhaps, the ineffective implementation of sexual and reproductive health policy strategies [36] as well as the attitude toward contraceptive counselling [37, 38] might have contributed to the limited access to quality contraceptive counselling among adolescent girls and young women in SSA. Thus, considering the importance of quality contraceptive counselling in reducing the fertility rate [39], evidenced-based country-specific counselling strategies are needed to improve women’s access to quality contraceptive counselling in SSA.
We also observed wide inter-country variations in the proportion of adolescent girls and young women who received quality contraceptive counselling in SSA. Although we could not make a direct comparison due to the non-availability of a similar multi-country level study, a few individual country-level comparisons revealed varied discrepancies. For example, while our finding in Sierra Leone was marginally higher (67%) than what was previously reported [63.4%] [31], we recorded a lower (21.6%) proportion of adolescent girls and young womenȉs receipt of quality contraceptive counselling than previously estimated (30%) in Ethiopia [30]. These observed differences could be partly explained by the variations in study designs, timing, and target population. For example, while Sserwanja et al. [31] studied women aged 15–24 years in Sierra Leone, Hrusa et al. [30] surveyed women of reproductive age (15–49 years) in Ethiopia. Nonetheless, the observed differences in our findings relative to the findings from the previous studies give some credence to the raging concern that while access to quality contraceptive counselling is improving in some countries in SSA, others are witnessing a decline [34]. This highlights the need for concerted efforts to improve women’s access to quality contraceptive counselling in SSA. Lack of access to quality contraceptive counselling has been associated with women’s likelihood not to choose any form of contraceptive [39] as well as a high rate of contraceptive discontinuation [40], which contributes to increased fertility rate in SSA [41].
Although previous studies [30, 31] reported no significant association between women’s age and receipt of quality contraceptive counselling information, our findings revealed that young women aged 20–24 years were more likely to receive quality contraceptive counselling relative to adolescent girls. The observed discrepancies in our findings relative to the previous studies could be due to methodological variations since previous studies were conducted at an individual country level compared to our use of multi-country settings. Meanwhile, among women of reproductive age, Semachew Kasa et al. [42] reported that awareness, attitude, and practices toward family planning increase with advancing age. This might contribute to increased demand or search for information on contraception and thus, increase access to quality contraceptive counselling among women aged 20–24 years. Perhaps, providing adolescent-friendly contraceptive counselling services could significantly improve quality contraceptive counselling information and contraceptive uptake among adolescent girls. Also, concerted efforts should be made in providing comprehensive sexual education to adolescent girls, equipping them with the quality information on contraceptives that might influence its use.
Adolescent girls and young women who were employed (currently working) as well as those having primary, secondary, or higher education were more likely to receive quality contraceptive counselling relative to the unemployed and those with no formal education. Similar findings were reported in previous studies [30, 43]. Education and employment have been identified as major empowerment tools in women’s autonomy and decision-making capacity towards contraception practices [44,45,46] such as accessing contraceptive counselling. Perhaps, interventions targeted at increasing adolescent girls and young women’s access to quality contraceptive counselling must pay particular attention to those with no education and the unemployed to equip them with the requisite skills and agency to seek health care including contraceptives.
Also, our findings revealed that adolescent girls and young women who were married, cohabiting, or previously married had higher odds of receiving quality contraceptive counselling relative to those who were never in a union. This finding contradicts findings from previous studies in SSA [30, 31] that reported no significant relationship between women’s marital status and their likelihood of receiving quality contraceptive counselling. Meanwhile, available evidence suggests that married and cohabiting women are more interested in the use of contraceptives [47], since they engage more in sexual intercourse relative to those who were never in a union [48]. Perhaps, this may contribute to their increased likelihood of receiving quality contraceptive counselling information.
Further, we found that adolescent girls and young women who heard of family planning from the radio in the last few months were more likely to receive quality contraceptive counselling. A similar finding was reported in a previous study in Ethiopia [43]. The importance of radio in promoting sexual and reproductive health education and practices in SSA has been highlighted in several studies [43, 49, 50]. Local radio stations in SSA commonly engage resource persons to educate the public on important health matters such as contraception [51], which could improve women’s ability to access quality contraceptive counselling.
Interestingly, adolescent girls and young women who use the internet had lower odds of receiving quality contraceptive counselling. Although the internet is a very useful tool for disseminating important health information, it is also a breeding ground for disinformation, particularly on contraception [52]. Given that many women in SSA Africa have limited education, they may have less ability to access quality contraceptive counselling from internet sources. Therefore, strategies to improve adolescent girls and young women’s access to quality contraceptive counselling could include education on responsible usage of internet-based health information. Also, internet-based campaigns can be developed and implemented in SSA to provide quality information on contraceptives.
Further, adolescent girls and young women who had increased or easy access to healthcare services (e.g., those who visited a health facility in the last 12 months or those who had no problem getting permission to seek medical help) were more likely to receive quality contraceptive counselling. Understandably, visiting healthcare facilities increases women’s interaction with trained healthcare staff, which could improve their ability to access quality contraceptive counselling from healthcare workers [39]. Scott et al. [53] reported that increased access to contraceptive and services from healthcare workers significantly improves the use of modern contraception among women. This finding highlights the importance of continuously educating young women on the need to access contraceptive counselling and services from trained healthcare workers.
Previous studies in Ethiopia [30], Sierra Leone [31], and Uganda [35] reported significant geographic variations in women’s receipt of quality contraceptive counselling, albeit at the intra-country level. In this study, we observed high access to quality contraceptive counselling among the young women who resided in the Southern, Eastern, and Western parts of SSA relative to those from Central SSA. Perhaps, the varied socio-economic and cultural differences of the various sub-regions might have contributed to the observed variations. For instance, Lukyamuzi et al. [35] reported that people in geographical locations with increased access to healthcare services often receive quality contraceptive counselling.
We observed that adolescent girls and young women from rural areas had lower odds of receiving quality contraceptive counselling information. This may be attributed to their limited access to healthcare services, including contraceptive counselling services [54]. Limited healthcare infrastructural facilities and personnel could have contributed to the lower likelihood of adolescent girls and young women receiving quality contraceptive counselling. Also, deep-rooted sociocultural beliefs could have negatively affected the adolescent girls and young women’s likelihood of accessing healthcare including quality contraceptive counselling.
Strength and limitations
Our use of nationally representative datasets to examine receipt of quality contraceptive counselling among adolescent girls and young women across 20 countries in SSA enhances the generalizability of our findings to adolescent girls and young women in SSA. Nonetheless, this study had some limitations. Although our analysis was based on the most recent DHS datasets of the individual countries, the survey years varied. This could limit the interpretation of our findings, particularly when comparing women’s receipt of quality contraceptive counselling information from one country to another. Also, while facility and healthcare worker-related factors could influence women’s access to and receipt of quality contraceptive counselling, our analysis focused on only client-level variables. The DHS survey adopts cross-sectional study design, hence only associations are reported. Additionally, since adolescent girls and young women’s receipt of quality contraceptive counselling was self-reported, it is open to recall and social desirability biases.
Conclusion
This study highlights the limited access to quality contraceptive counselling among adolescent girls and young women across SSA. Considering the importance of quality contraceptive counselling on the uptake and continuation of contraception, policymakers need to institute measures that improve young women’s access to quality contraceptive counselling in SSA, especially in countries like Cameroon, Angola, Madagascar, Mauritania, and Guinea. Such measures could be targeted at adolescent girls and young women aged 15–19 years, those with no education, those who are single, those unemployed, those with limited access to radio, those with difficulty accessing healthcare, and those from the central part of SSA. Perhaps, increasing adolescent girls and young women’s receipt of quality contraceptive counselling could greatly minimize the risk of unintended pregnancies and its associated maternal and child health burden in SSA.
Data Availability
The data used for this study is freely available at http://dhsprogram.com/data/available-datasets.cfm.
References
Sully EA, Biddlecom A, Darroch JE, Riley T, Ashford LS, Lince-Deroche N, Firestein L, Murro R. Adding it up: investing in sexual and reproductive health 2019. New York: Guttmacher Institute; 2020. https://www.guttmacher.org/report/adding-it-up-investing-in-sexual-reproductive-health-2019.
Phiri M, Odimegwu C, Kalinda C. Unmet need for family planning among married women in sub-saharan Africa: a meta-analysis of DHS data (1995–2020). Contracept Reproductive Med. 2023;8(1):1–11.
Blackstone SR, Nwaozuru U, Iwelunmor J. Factors influencing contraceptive use in sub-saharan Africa: a systematic review. Int Q Community Health Educ. 2017;37(2):79–91.
Schivone GB, Glish LL. Contraceptive counseling for continuation and satisfaction. Curr Opin Obstet Gynecol. 2017;29(6):443–8.
Bertrand JT, Ross J, Sullivan TM, Hardee K, Shelton JD. Contraceptive method mix: updates and implications. Global Health: Science and Practice. 2020;8(4):666–79.
Zhang X, Guan Q, Yu Q, Xiao W, Chen Z, Dong C, Deng S, Zhuang Y, Xia Y. Estimating the effects of policies on infertility prevalence worldwide. BMC Public Health. 2022;22(1):1–11.
de Leon RG, Ewerling F, Serruya SJ, Silveira MF, Sanhueza A, Moazzam A, Becerra-Posada F, Coll CV, Hellwig F, Victora CG, Barros AJ. Contraceptive use in Latin America and the Caribbean with a focus on long-acting reversible contraceptives: prevalence and inequalities in 23 countries. The Lancet Global Health. 2019;7(2):e227–35.
Kantorová V, Wheldon MC, Ueffing P, Dasgupta AN. Estimating progress towards meeting women’s contraceptive needs in 185 countries: a bayesian hierarchical modelling study. PLoS Med. 2020;17(2):e1003026.
Wang MY, Temmerman M, Zhang WH, Fan Y, Mu Y, Mo SP, Zheng A, Li JK. Contraceptive and reproductive health practices of unmarried women globally, 1999 to 2018: systematic review and meta-analysis. Medicine. 2020;99(49).
Ali M, Tran NT. Defining counselling in contraceptive information and services: outcomes from an expert think tank. BMJ Sex Reproductive Health. 2022;48(2):79–81.
Radovich E, Dennis ML, Wong KL, Ali M, Lynch CA, Cleland J, Owolabi O, Lyons-Amos M, Benova L. Who meets the contraceptive needs of young women in sub-saharan Africa? J Adolesc Health. 2018;62(3):273–80.
Senderowicz L. Contraceptive autonomy: conceptions and measurement of a novel family planning indicator. Stud Fam Plann. 2020;51(2):161–76.
Ameyaw EK, Budu E, Sambah F, Baatiema L, Appiah F, Seidu AA, Ahinkorah BO. Prevalence and determinants of unintended pregnancy in sub-saharan Africa: a multi-country analysis of demographic and health surveys. PLoS ONE. 2019;14(8):e0220970.
Bain LE, Zweekhorst MB, de Cock Buning T. Prevalence and determinants of unintended pregnancy in sub–saharan Africa: a systematic review. Afr J Reprod Health. 2020;24(2):187–205.
Karp C, OlaOlorun FM, Guiella G, Gichangi P, Choi Y, Anglewicz P, Holt K. Validation and predictive utility of a person-centered quality of Contraceptive Counseling (QCC‐10) scale in sub‐Saharan Africa: a Multicountry Study of Family Planning clients and a New Indicator for Measuring High‐Quality, rights‐based care. Stud Fam Plann. 2023;54(1):119–43.
Tsega NT, Haile TT, Asratie MH, Belay DG, Endalew M, Aragaw FM, Tsega SS, Gashaw M. Pooled prevalence and determinants of informed choice of contraceptive methods among reproductive age women in Sub-saharan Africa: a multilevel analysis. Front Public Health. 2022;10:962675.
Handebo S. Informed choice of contraceptive methods among women in Ethiopia: further analysis of the 2016 Ethiopian demographic health survey. Open Access Journal of Contraception 2021 Mar 16:83–91.
Ontiri S, Kabue M, Biesma R, Stekelenburg J, Gichangi P. Assessing quality of family planning counseling and its determinants in Kenya: analysis of health facility exit interviews. PLoS ONE. 2021;16(9):e0256295.
Sato R, Elewonibi B, Msuya S, Manongi R, Canning D, Shah I. Why do women discontinue contraception and what are the post-discontinuation outcomes? Evidence from the Arusha Region, Tanzania. Sex Reproductive Health Matters. 2020;28(1):1723321.
Boadu I. Coverage and determinants of modern contraceptive use in sub-saharan Africa: further analysis of demographic and health surveys. Reproductive Health. 2022;19(1):1–11.
Festin MP. Overview of modern contraception. Best Pract Res Clin Obstet Gynecol. 2020;66:4–14.
Sserwanja Q, Musaba MW, Mukunya D. Prevalence and factors associated with modern contraceptives utilization among female adolescents in Uganda. BMC Womens Health. 2021;21:1–7.
Ninsiima LR, Chiumia IK, Ndejjo R. Factors influencing access to and utilisation of youth-friendly sexual and reproductive health services in sub-saharan Africa: a systematic review. Reproductive Health. 2021;18(1):1–17.
Kitui LN. Youth Friendly Health Services in Kenya: Characteristics, Knowledge, Attitude, Practices and Experiences (Masters Dissertation, JKUAT-COHES). 2023. http://ir.jkuat.ac.ke/handle/123456789/6110.
The DHS Program. Data– Available Datasets. https://dhsprogram.com/data/available-datasets.cfm (Accessed May, 20, 2023).
Croft TNC, Marshal AMJ, Allen CK. Guide to DHS statistics, DHS-7 [Internet]. Maryland, USA: ICF,: Rockville; 2018. https://dhsprogram.com/pubs/pdf/DHSG1/Guide_to_DHS_Statistics_DHS-7.pdf.
Corsi DJ, Neuman M, Finlay JE, Subramanian SV. Demographic and health surveys: a profile. Int J Epidemiol. 2012;41(November):1602–13.
International ICF. Demographic and Health Survey, Sampling and Household Listing Manual:Demographic and Health Survey [Internet]. ICF International. 2012. Available from: https://dhsprogram.com/pubs/pdf/DHSM4/DHS6_Sampling_Manual_Sept2012_DHSM4.pdf.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int J Surg [Internet]. 2014;12(12):1495–9. https://doi.org/10.1016/j.ijsu.2014.07.013.
Hrusa G, Spigt M, Dejene T, Shiferaw S. Quality of Family Planning Counseling in Ethiopia: Trends and determinants of information received by female modern contraceptive users, evidence from national survey data,(2014–2018). PLoS ONE. 2020;15(2):e0228714.
Sserwanja Q, Nuwabaine L, Kamara K, Musaba MW. Determinants of quality contraceptive counselling information among young women in Sierra Leone: insights from the 2019 Sierra Leone demographic health survey. BMC Womens Health. 2023;23(1):1–9.
Galle A, Vermandere H, Griffin S, de Melo M, Machaieie L, Van Braeckel D, Degomme O. Quality of care in family planning services in rural Mozambique with a focus on long acting reversible contraceptives: a cross-sectional survey. BMC Womens Health. 2018;18(1):1–3.
Bruce J. Fundamental elements of the quality of care: a simple framework. Stud Fam Plann. 1990;21(2):61–91.
Jain AK. Examining progress and equity in information received by women using a modern method in 25 developing countries. Int Perspect Sex Reproductive Health. 2016;42(3):131–40.
Lukyamuzi Z, Tetui M, Fonseca-Rodríguez O, Atuyambe L, Makumbi FE, Baroudi M. Quality of care in Family Planning services: differences between formal and Informal settlements of Kira Municipality, Uganda. Front Global Women’s Health. 2021;2:656616.
Kabra R, Ali M, Kiarie J. Design and initial implementation of the WHO FP umbrella project-to strengthen contraceptive services in the sub Saharan Africa. Reproductive Health. 2017;14(1):1–6.
Gahungu J, Vahdaninia M, Regmi PR. The unmet needs for modern family planning methods among postpartum women in Sub-saharan Africa: a systematic review of the literature. Reproductive Health. 2021;18:1–15.
Olakunde BO, Sam-Agudu NA, Patel TY, Hunt AT, Buffington AM, Phebus TD, Onwasigwe E, Ezeanolue EE. Uptake of permanent contraception among women in sub-saharan Africa: a literature review of barriers and facilitators. Contraception. 2019;99(4):205–11.
Dey AK, Averbach S, Dixit A, Chakraverty A, Dehingia N, Chandurkar D, Singh K, Choudhry V, Silverman JG, Raj A. Measuring quality of family planning counselling and its effects on uptake of contraceptives in public health facilities in Uttar Pradesh, India: a cross-sectional analysis. PLoS ONE. 2021;16(5):e0239565.
Tsui AO, Brown W, Li Q. Contraceptive practice in sub-saharan Africa. Popul Dev Rev. 2017;43(Suppl Suppl 1):166–91.
Iyanda AE, Dinkins BJ, Osayomi T, Adeusi TJ, Lu Y, Oppong JR. Fertility knowledge, contraceptive use and unintentional pregnancy in 29 African countries: a cross-sectional study. Int J Public Health. 2020;65:445–55.
Semachew Kasa A, Tarekegn M, Embiale N. Knowledge, attitude and practice towards family planning among reproductive age women in a resource limited settings of Northwest Ethiopia. BMC Res Notes. 2018;11(1):1–6.
Ejigu BA, Seme A, Zimmerman L, Shiferaw S. Trend and determinants of quality of family planning counseling in Ethiopia: evidence from repeated PMA cross-sectional surveys,(2014–2019). PLoS ONE. 2022;17(5):e0267944.
Al Riyami A, Afifi M, Mabry RM. Women’s autonomy, education and employment in Oman and their influence on contraceptive use. Reprod Health Matters. 2004;12(23):144–54.
Cavallaro FL, Benova L, Owolabi OO, Ali M. A systematic review of the effectiveness of counselling strategies for modern contraceptive methods: what works and what doesn’t? BMJ Sex Reproductive Health. 2020;46(4):254–69.
Patrikar SR, Basannar DR, Sharma MS. Women empowerment and use of contraception. Med J Armed Forces India. 2014;70(3):253–6.
Mandiwa C, Namondwe B, Makwinja A, Zamawe C. Factors associated with contraceptive use among young women in Malawi: analysis of the 2015–16 Malawi demographic and health survey data. Contracept Reproductive Med. 2018;3(1):1–8.
Ueffing P, Dasgupta AN, Kantorová V. Sexual activity by marital status and age: a comparative perspective. J Biosoc Sci. 2020;52(6):860–84.
Ahinkorah BO, Budu E, Aboagye RG, Agbaglo E, Arthur-Holmes F, Adu C, Archer AG, Aderoju YB, Seidu AA. Factors associated with modern contraceptive use among women with no fertility intention in sub-saharan Africa: evidence from cross-sectional surveys of 29 countries. Contracept Reproductive Med. 2021;6(1):1–13.
Iacoella F, Gassmann F, Tirivayi N. Which communication technology is effective for promoting reproductive health? Television, radio, and mobile phones in sub-saharan Africa. PLoS ONE. 2022;17(8):e0272501.
Ahn J, Briers G, Baker M, Price E, Strong R, Piña M, Zickafoose A, Lu P. Radio communications on family planning: case of West Africa. Int J Environ Res Public Health. 2022;19(8):4577.
Weiss E, Moore K. An assessment of the quality of information available on the internet about the IUD and the potential impact on contraceptive choices. Contraception. 2003;68(5):359–64.
Scott VK, Gottschalk LB, Wright KQ, Twose C, Bohren MA, Schmitt ME, Ortayli N. Community health workers’ provision of family planning services in low-and middle‐income countries: a systematic review of effectiveness. Stud Fam Plann. 2015;46(3):241–61.
Tessema ZT, Worku MG, Tesema GA, Alamneh TS, Teshale AB, Yeshaw Y, Alem AZ, Ayalew HG, Liyew AM. Determinants of accessing healthcare in Sub-saharan Africa: a mixed-effect analysis of recent demographic and health surveys from 36 countries. BMJ Open. 2022;12(1):e054397.
Acknowledgements
The authors thank the Measure DHS project for their support and free access to the original data.
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Contributions
MA, RGA, and BOA contributed to the study design and conceptualization. MA, IED, RGA, AS, and BOA drafted the initial draft and performed the analysis. BOA, RGA, and AS provided technical support and critically reviewed the manuscript for its intellectual content. RGA had the final responsibility to submit for publication. All authors read and amended drafts of the paper and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was not required for this study since the data is secondary and is available in the public domain. Detailed information concerning the DHS data and ethical standards are available via http://goo.gl/ny8T6X.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mohammed, A., Donkoh, I.E., Aboagye, R.G. et al. Access to quality contraceptive counselling among adolescent girls and young women in sub-Saharan Africa. Contracept Reprod Med 9, 16 (2024). https://doi.org/10.1186/s40834-024-00267-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40834-024-00267-x