Abstract
Background
Uganda has a high population growth rate of 3%, partly due to limited access to and low usage of contraception. This study assessed the cost-effectiveness of the family planning benefits cards (FPBC) program compared to standard of care (SOC). The FPBC program was initiated to increase access to modern contraception among young women in slums in Kampala, Uganda.
Methods
We developed a decision-analytic model (decision tree) and parameterized it using primary intervention data together with previously published data. In the base case, a sexually active woman from an urban slum, aged 18 to 30 years, was modelled over a one-year time horizon from both the modified societal and provider perspectives. The main model outcomes included the probability of unintended conception, costs, and incremental cost-effectiveness ratio (ICER) in terms of cost per unwanted pregnancy averted. Both deterministic and probabilistic sensitivity analyses were conducted to assess the robustness of the modelling results. All costs were reported in 2022 US dollars, and analyses were conducted in Microsoft Excel.
Results
In the base case analysis, the FPBC was superior to the SOC in outcomes. The probability of conception was lower in the FPBC than in the SOC (0.20 vs. 0.44). The average societal and provider costs were higher in the FPBC than in the SOC, i.e., $195 vs. $164 and $193 vs. $163, respectively. The ICER comparing the FPBC to the SOC was $125 per percentage reduction in the probability of unwanted conception from the societal perspective and $121 from the provider perspective. The results were robust to sensitivity analyses.
Conclusion
Given Uganda’s GDP per capita of $1046 in 2022, the FPBC is highly cost-effective compared to the SOC in reducing unintended pregnancies among young women in low-income settings. It can even get cheaper in the long run due to the low marginal costs of deploying additional FPBCs.
Trial registration
MUREC1/7 No. 10/05-17. Registered on July 19, 2017.
Similar content being viewed by others
Background
Uganda’s population of 45 million grows at an annual rate of 3.34%, one of the highest growth rates in the World [1]. This is, at least in part, due to limited access to and use of modern contraceptive methods [2, 3]. Like in many low-income countries, women in Uganda face many challenges and risks related to sexual and reproductive health, such as a high unmet need for contraception (approximately 30%), which leads to 43% of all pregnancies being unintended. Low contraception use also leads to a high rate of abortion and unsafe abortion: 30% of all abortions in Uganda are unsafe [3]. Other barriers to using contraception include fear of side effects, infrequent sex, financial incapability, ignorance about methods, and partner opposition towards contraception [2, 4]. Among women with an unmet need for contraception, the largest proportion is poor and less educated [2], predominant characteristics of an urban slum population.
Despite the slowly diminishing unmet need for contraception, more work is needed to ensure that all women, irrespective of their background and socio-economic status, have access to modern contraception methods and are sensitized, along with their partners, about the costs of unintended pregnancies and unplanned families [2]. This aligns with the view that everyone has the right to health under article 25 of the Universal Declaration of Human Rights [5]. Fulfilling the unmet need for contraception in Uganda would have substantial benefits, including averting an estimated 76,000 annual maternal deaths, saving $8.3 billion in costs of unintended pregnancies, and generating net savings of about $7 billion that would have been spent on child and maternal care [6]. This is also fundamental to the achievement of sustainable development goals (SDGs) 2 and 3 (zero hunger and good health and wellbeing) [6]. Despite the evidence of high returns of investing in contraception, Uganda has not prioritized access to contraception [7].
The inequality of access to modern contraception is a reality not only in low-income countries but also in high-income countries. Different studies have shown that the utilization of long-term modern contraception methods varies across the area (region of residence), age, and socioeconomic status – with poor access among low-income earners, the unemployed, and rural dwellers [8,9,10,11,12,13,14]. The question researchers and policymakers worldwide should be asking is, what interventions or strategies are currently in place to reduce inequalities in accessing modern contraception?
Several innovative service delivery approaches have been pilot-tested to increase contraception uptake, including community outreaches, mobile phone applications, youth corner spaces, social marketing, and franchising and community-based distribution [15,16,17,18]. Voucher-based initiatives are a feasible means of increasing contraception usage in low-and middle-income countries (LMICs) [19,20,21,22].
Economic evaluation is the comparative analysis of two or more healthcare interventions in terms of both their costs and benefits (outcomes) [23]. Many contraception interventions in LMICs have been assessed and reported to be cost-effective [24,25,26,27,28]. Similarly, many cost-effective contraception interventions have been documented in Uganda [29,30,31,32,33]. However, no study has been conducted regarding incentive-based contraception interventions in Uganda.
In this study, we assessed the one-year cost-effectiveness of using an incentive-based family planning benefits card (FPBC) to increase access to contraception services among young women in slums in Kampala, Uganda, compared to the standard of care (SOC), i.e., a “status quo” situation.
Studies suggest that many potential contraception users lack access due to poverty [7, 34]. For example, the price of a copper implant in Uganda ranges from $ 6 -$12 [35]. Most of the service providers in Kampala’s urban slums are private health facilities that charge up to four times higher than public facilities [36]. This is in the context of an urban population where most inhabitants live on less than a dollar per day [37]. The study will add to the evidence base to support the economic efficiency of universal access to contraception in low-income countries in general and marginalized populations in particular.
Methods
Design
We conducted a model-based cost-effectiveness analysis using data from a one-year prospective impact evaluation of the FPBC intervention conducted in Uganda. Data on costs and outcomes were obtained from this evaluation, which was a quasi-experimental study conducted in the urban slums of Kampala [38]. Additional data were obtained from the published literature.
The family planning benefits card program
The FPBC program was a one-year pilot project, a novel incentive system intended to increase uptake of contraception services among adults aged 18 to 30 in the Kamwokya slum area of Kampala, Uganda’s capital city [4, 38]. The program provided a card that allowed access to free male and female condoms, implants, intrauterine devices (IUDs), injections, vaginal rings, contraceptives and emergency contraceptive pills, diaphragms, counselling and guidance, and pregnancy and HIV testing. The incentives were given to partner clinics to boost contraception provision in the form of subsidized prices to all administered contraception methods compared to the normal market prices. The FPBC was found to be highly acceptable and was utilized to a significant extent in this population [28].
Target population
The reference case population in the current study included young female adults aged 18 to 30 years, non-users of modern contraception methods, sexually active and not pregnant, and willing to give informed consent [4, 38]. This criterion was the basis for eligibility for the prospective study as well as the current study. Therefore, this study reported outcomes and costs on a per-person basis.
Setting
The study setting and context were urban slums located in the city suburbs of Kampala, Uganda’s capital city. These two slums were purposively selected to assess the effectiveness of the FPBC due to their similar socio-demographic characteristics—the largest population is unemployed, falls in the lowest wealth quintile, and has the highest unmet need for contraception (30%) [3, 37, 39]. The current study findings may be applied in informing health policy in similar urban slum settings in low-income countries.
Comparators
We compared the FPBC with the SOC, considered as a status quo situation, an out-of-pocket venture, where the young female adults visited clinics or health facilities of their choices and paid for all the services requested and provided. Baseline and endline data for the SOC was collected at the same time as in the intervention group, and the intention-to-treat analysis was applied to estimate the intervention effect.
Time horizon
The time horizon of the analysis was one-year, consistent with the length of the prospective study from which cost data came [38].
Decision analytic model
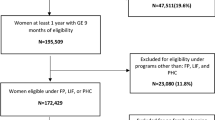
The decision-analytic model (decision tree) was developed to follow a young female adult’s likely course of action following the FPBC intervention. Data to parameterize the model were obtained from the one-year pilot extensive study [40] and published literature [30, 32]. The decision node represents the choice between the FPBC program and the SOC. [38] After being selected to the FPBC intervention, young women were divided into those who received the FPBC and those who did not. Young women who received the card were further divided into those who used it to access modern contraception methods and those who did not. Young women who accessed modern contraception methods using the card were also divided into those who suffered the adverse effects (the negative side effects of using modern contraception methods, such as mood change, low sex drive, weight gain, amenorrhea, bleeding, etc) and those who did not. It should be noted that some young women in the FPBC did not receive cards due to logistic reasons and delayed consenting. Thus, we made a conservative assumption that those who missed cards accessed modern contraception through out of pocket similar to the SOC arm, but with a triage path of an FPBC beneficiary. Further still, some of the card beneficiaries decided not to use the cards due to the fear of the side effects of modern contraception methods and the desire to conceive.
In the control arm (SOC), young women were divided into those who paid out of pocket to access modern contraception methods and those who did not. These were further divided into those who suffered adverse effects due to modern contraception methods and those who did not.
In both the FPBC and SOC, the end node represents the proportion of young women who reported unintended pregnancies at the end of the study [40]. Figure 1 below shows a schematic structure of the decision tree model.
Outcomes
This study measured the probability of unintended conception (pregnancy) as the main outcome.
Pregnancy
This study did not treat normal pregnancies as a burden or a bad thing but rather looked at unintended pregnancies as a burden to the families and societies due to their negative impact on economic growth, economic development, and public health [41, 42]. The study used the proportions of young female adults who reported having unintended pregnancies – mistimed or unwanted with no desire of having children— at the end of the study to estimate the probability of conception in the two groups. From the intention-to-treat analysis, young women who reported being pregnant at the end of six months (the follow-up period) were further stratified into: 1) pregnant without using modern contraception, 2) pregnant while using modern contraception and experiencing adverse effects, and 3) pregnant while using modern contraception without experiencing any adverse effects.
Perspective
The analysis was conducted from both the modified societal and provider (government of Uganda through the Ministry of Health and other non-government organizations) perspectives. The ministry of health covers only 10% of the contraception budget [43]; 90% is catered for by non-government organizations and individuals through out-of-pocket expenditure. Therefore, considering the provider and modified societal perspectives would include all direct medical costs and indirect costs incurred by individuals, as well as direct non-medical costs incurred by providers.
Costs
Direct medical costs (personnel time, training costs, laboratory tests, drugs, medical devices, and supplies), direct non-medical costs (administration, overhead, utilities) were analyzed to suit the provider (in this case, Ministry of Health) perspective. In contrast, costs related to lost productivity were added to cater for the modified societal perspective. We conducted key informant interviews (KIIs) with the medical personnel from partner clinics and the FPBC beneficiaries to estimate the time spent administering each modern contraception method, and the waiting time at the clinics, respectively. These KIIs were conducted on an appointment basis, where the medical personnel and FPBC beneficiaries were notified about the purpose and location of the meeting with the help of community health workers (CHWs), and each session lasted for 15 to 20 minutes. The average time for administering each modern contraception method was estimated from the recorded notes, as well as the average waiting time by the FPBC beneficiaries. These time estimates were multiplied by the average wage in both public and private sectors [44].
The beneficiaries’ occupations and the average waiting time were key components in estimating the lost productivity costs (indirect costs) [40]. Costs on the medical supplies and drugs were estimated from the Management Sciences for Health (MSH) price catalogues [45] since the prices paid to the partner clinics by the insurance company embedded an incentive component, thus a slightly higher price. Costs on equipment, including cars and computers, were annuitized at an annual discount rate of 3% to account for depreciation. Other direct medical (salaries for personnel, training, and medical supplies) and non-medical (administration, program costs, and overhead) costs were estimated by reviewing account records from the GHE database using the line-by-line cost estimation method [46].
The primary study did not incur any other cost in the SOC group except for the research related costs, which were not considered, but these costs were estimated based on the reported proportions of usage of different modern contraception methods at the end of the study [40]. Like in the FPBC, these proportions were also used to estimate medical personnel time, childcare costs, drugs, and medicine. Indirect costs were estimated based on the participants’ reported occupations multiplied by the average waiting time. Other costs, such as personnel and overhead costs, were assumed to be similar, and the SOC did not incur any program-related costs (administration), as shown in Table 1.
Overall, in both the FPBC and SOC, the summation of these costs was multiplied by the proportion of respondents who used different modern contraception methods to determine the cost related to each contraception method.
Currency, price date, and conversion
All costs were adjusted for inflation to cater for the exchange rate fluctuations using the bank of Uganda exchange rates [47] and consumer price indices for Uganda [48] since these data were obtained from several years, i.e., 2017, for both the FPBC and SOC. All costs were reported in 2022 US dollars.
Analysis
In the base-case analysis, we compared the average cost per young female adult from the modified societal and payer perspectives, the probability of conception, and the ICER using the cost per unintended pregnancy averted. This enabled us to identify the dominant and dominated interventions between the FPBC and the SOC.
We conducted the deterministic (one way) sensitivity analysis to identify model parameters that most influenced the ICERs. Since there was no data on 95% confidence intervals on cost parameters, a range of +/− 50% was applied [30, 32]. Monte Carlo simulation was employed to generate 1000 iterations to calculate the expected outcome values and perform the probabilistic sensitivity analysis to assess further the impact of uncertainties surrounding key model parameters on the ICERs and the results’ robustness. A beta distribution was assumed for all probabilities while a normal distribution was applied to all costs, assuming that they were normally distributed [49, 50]. All analyses were conducted in Microsoft Excel, and as much as possible, this study followed the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement [51]. Table 2 shows the different model parameters with their probability distributions.
Approach to engagement with beneficiaries and others affected by the study
Besides engaging with the medical personnel from partner clinics and the FPBC beneficiaries to estimate the time spent administering each modern contraception method and the waiting time at the clinics, their contribution to the modelling process was considered, particularly in generating decision tree branches.
Ethical considerations
The respective institutional review boards approved the current study—Mbarara University of Science and Technology [MUREC1/7 No. 10/05-17], the Uganda National Council for Science and Technology, and other local authorities.
All study participants were initially sensitized about the purpose of the study with the help of CHWs and provided informed consent before being recruited to participate in the study.
Results
Base case analysis
Table 3 shows the results summary from the base case analysis. The average probability of unintended conception was lower in the FPBC than in the SOC (0.20 vs. 0.44).
The average societal cost per young woman was higher for the FPBC from the modified societal perspective ($195 vs. $164) and the provider perspective ($193 vs. $163). The absolute ICER comparing the FPBC to the SOC was $125 per unintended pregnancy averted from the societal perspective and $121 from the provider perspective.
Sensitivity analyses
As shown in Fig. 2, the deterministic sensitivity analysis indicated that the ICERs were most sensitive to the uncertainties surrounding the direct medical costs and direct non-medical costs related to the FPBC and SOC, and the probability of pregnancy while not using modern contraception and using the FPBC to access modern contraception. The ICERs remained within plausible ranges of the cost-effectiveness threshold, thus robust to sensitivity analyses (Fig. 2).
In Fig. 3, the incremental cost-effectiveness plane from the probabilistic sensitivity analysis through Monte Carlo simulation showed that most cost-effectiveness pairs were distributed in the northeast and southeast quadrants of the cost-effectiveness plane. The widespread pair points across the cost-effectiveness plane indicate a high level of certainty that the FPBC is more cost-effective than the SOC, but with some uncertainty on whether the FPBC is less costly than the SOC.
Incremental Cost-effectiveness scatter plot obtained from the probabilistic sensitivity analysis showing the distribution of pairs for incremental costs and averted pregnancies on the cost-effectiveness plane. The largest distribution is in the northeast quadrant and fairly distributed in the southeast quadrant
In Fig. 4, the cost-effectiveness acceptability curve indicates the probability that the FPBC is more cost-effective than the SOC at a certain range of willingness to pay values curbed at 3 times Uganda’s GDP per capita, the gold standard for LMICs. It suggests that the percentage of iterations in which the FPBC is more cost-effective than the SOC nears 100% at a cost-effectiveness threshold of less than $1046, the GDP per capita of Uganda.
Discussion
This study used a decision tree model and data from a quasi-experimental study design to assess the one-year cost-effectiveness of the FPBC compared to the SOC. The results showed that the FPBC was highly cost-effective –largely dominated the SOC—from both the modified societal perspective and the provider perspective. In other words, the FPBC led to increased costs, and a lower probability of unintended conception for one year compared to the SOC. The difference in the annual probability of conception between the two groups (FPBC Vs. SOC) was considerable at 24%. Arguably, this can be attributed to contraception failure since most young women in the SOC used short-term contraception methods with a reported failure rate of about 3% [52]. In addition, the low probability of conception in the FPBC could be explained by the large proportions of users who entered the FPBC program (93%) and used the FPBC to access modern contraception (72%), particularly long-term methods, such as implants, and IUDs. Notably, these results were robust to both the deterministic and the probabilistic sensitivity analyses, i.e., there were no significant changes in the results—high costs and better outcomes—in favour of the FPBC like in the base case analysis.
In the deterministic sensitivity analysis, the ICERs were most driven by the uncertainties surrounding the direct medical costs, and direct non-medical costs related to the FPBC and SOC, as well as the probability of pregnancy while not using modern contraception and using the FPBC to access modern contraception. The most significant component of direct medical costs were the personnel costs (60%), while program costs largely contributed to direct non-medical costs (13%). The large program costs could be attributed to the fact that the FPBC model gave incentives to partner clinics in the form of higher prices than the normal prices, as a motivation to provide free services to all FPBC beneficiaries. Perhaps if these incentives were not huge or if it were an entirely free service venture, the FPBC would even be cheaper. Additionally, the high indirect costs related to the FPBC can be explained by the fact that many FPBC beneficiaries opted for long term contraception methods like IUDs, and implants, which required a lot of administration time by the service providers—the time spent on administering different methods by the healthcare service providers was a key component in estimating indirect costs. A cost consequences analysis study on induced abortion in Uganda reported similar results, i.e., the largest component of both the societal and provider costs were direct medical and indirect costs [53].
Our results are consistent with the considerable literature on non-incentive-based contraception interventions in other LMICs, including Nigeria, Mexico, India, Afghanistan, Vanuatu and the Solomon Islands [24,25,26,27,28], which were found to be cost-effective. Similarly, these results agree with results from several non-incentive-based contraception interventions in Uganda that proved highly cost-effective and cost-effective [29,30,31,32,33]. Such interventions included; the universal access of contraception among all women in Uganda using hypothetical interventions [$ 105 per DALY averted and $ 629 per DALY averted, respectively] [30, 32], actual contraception methods such as injectables [$ 2.94 per birth averted], condoms [$ 2.06 per birth averted] and oral contraceptives [$ 1.65 per birth averted] [31], and a community-based provision vs. facility-based provision in a non-government organization setting [$ 21.21 per couple year of protection vs. $37.7 per couple year of protection, respectively] [33].
In dominating the SOC, the FPBC matches up with other incentive-based healthcare approaches and interventions that are cost-effective in Uganda, such as vouchers for treatment of sexually transmitted infections and maternal health [$ 302 per DALY averted] [54], vouchers for maternal health services with transport facilitation at any health facility in a rural setting [$ 302 per DALY averted] [55] and a savings scheme among adolescents orphaned by AIDS [$ 267 per 0.2 standard deviation range] [56]. It should be noted that the FPBC program structure was conceptually similar to an insurance model that thrives on significant economies of scale with higher numbers. And, given the successful proof of concept, feasibility (high acceptability and utilization) [4], and effectiveness [40], the marginal cost of the FPBC deployment (cost per additional user) would substantially reduce. This implies that the program and administration costs are incurred upfront and considered “sunk” costs. With this consideration, the ICERs could drop substantially and would be considered cheaper in a low-income setting. This may potentially be an area for future research to ascertain these results using different approaches.
Besides, the implementation of these interventions, including the FPBC, entirely depends on policymakers. The FPBC could potentially lead to increased savings, reduced mortalities, and contribute towards long-life span, attaining the SDGs and economic growth and development in the long run. The FPBC could also be used as one of the panaceas to the worldwide gross inequalities in accessing modern contraception since it covers the financial risk of out-of-pocket expenditure on modern contraception among marginalized groups [8,9,10,11,12,13,14].
Study limitations
Like other models, the current analysis could not elude from limitations, which emanate from data availability issues and assumptions. By conducting interviews with the FPBC beneficiaries to estimate indirect costs (lost productivity) after one year of the program closure, we likely overestimated the costs due to recall bias. We also could have underestimated the actual costs by assuming that the personnel and overhead costs in the SOC group were similar to the FPBC. Nevertheless, we believe that the effect was not too huge to affect the ICER estimates.
We conducted the analysis from both the modified societal and provider perspectives, and the outcomes data were adopted from a quasi-experimental study—conceptually similar to a randomized controlled trial using the intention-to-analysis technique. Therefore, our results are generalizable and applicable to other low-and middle-income settings.
Conclusion
The FPBC is a highly cost-effective intervention in the short-term compared to the SOC, and with greater certainty that it can be favourably cheaper in the long run due to the low marginal costs of deploying additional FPBCs. This bodes well towards the implementation of the FPBC to increase access to modern contraception methods among young women living in slums and other vulnerable groups, as Uganda transitions towards achieving five of the seventeen 2030 SDGs through the reduction of unintended pregnancies, infant and maternal mortalities, as well as having well-planned for children.
Availability of data and materials
All the data used and presented in this study are available upon request.
Abbreviations
- CHEERS:
-
Consolidated Health Economic Evaluation Reporting Standards
- CHWs:
-
Community health workers
- DALYs:
-
Disability-adjusted life years
- FPBC:
-
Family planning benefits card
- GDP:
-
Gross domestic product
- ICER:
-
Incremental cost-effectiveness ratio
- IUDs:
-
Intrauterine devices
- KIIs:
-
Key Informant interviews
- LMICs:
-
Low-and middle-income countries
- MSH:
-
Management Sciences for Health
- SGDs:
-
Sustainable development goals
- SOC:
-
Standard of care
- WHO:
-
World Health Organization
References
World Bank. The World Bank in Uganda. [cited 2020 Nov 10]. Available from: https://www.worldbank.org/en/country/uganda/overview
Reasons for unmet need for contraception in developing Countries: Guttmacher institute. New York; 2016. (Fact sheet). Available from: https://www.guttmacher.org/sites/default/files/report_pdf/unmet-need-for-contraception-in-developing-countries-report.pdf.
Uganda Bureau of Statistics. Uganda demographic and health survey (2016 UDHS). 2016. Available from: http://www.ubos.org/onlinefiles/uploads/ubos/pdfdocuments/Uganda_DHS_2016_KIR.pdf.
Nuwasiima A, Nuwamanya E, Babigumira JU, Nalwanga R, Asiimwe FT, Babigumira JB. Acceptability and utilization of family planning benefits cards by youth in slums in Kampala, Uganda. Contracept Reprod Med. 2019;4(1):1–11.
UN General Assembly. Universal Declaration of Human Rights. 1948 [cited 2019 May 13]. Available from: https://www.ohchr.org/EN/UDHR/Documents/UDHR_Translations/eng.pdf
Adding it up: investing in contraception and maternal and newborn health.. Guttmacher Institute. New York; 2017. Available from: http://www.gatesfoundation.org/What-We-Do/Global-Development/Family-Planning%0Ahttps://www.guttmacher.org/fact-sheet/adding-it-up-contraception-mnh-2017
Kiwanuka SN, Ekirapa EK, Peterson S, Okui O, Rahman MH, Peters D, et al. Access to and utilisation of health services for the poor in Uganda: a systematic review of available evidence. Trans R Soc Trop Med Hyg. 2008;102(11):1067–74.
Abekah-Nkrumah G. Trends in utilisation and inequality in the use of reproductive health services in sub-Saharan Africa. BMC Public Health. 2019;19(1):1–15.
Sharma H, Singh SK. Socioeconomic inequalities in contraceptive use among female adolescents in south Asian countries: a decomposition analysis. BMC Womens Health. 2022;22(1):1–15. https://doi.org/10.1186/s12905-022-01736-8.
Machado AKF, Gräf DD, Höfs F, Hellwig F, Barros KS, Moreira LR, et al. Prevalence and inequalities in contraceptive use among adolescents and young women: data from a birth cohort in Brazil. Cad Saude Publica. 2021;37(10):1–12.
Rice WS, Redd SK, Luke AA, Komro K, Jacob Arriola K, Hall KS. Dispersion of contraceptive access policies across the United States from 2006 to 2021. Prev Med Reports. 2022;27(October 2021):101827. https://doi.org/10.1016/j.pmedr.2022.101827.
Cioffi A, Cecannecchia C, Cioffi F, Rinaldi R, Bolino G. Free access to emergency oral contraceptives (EOCs) in the European union: a regulatory vacuum to be filled. Int J Risk Saf Med. 2022;1:1–6.
Li Z, Patton G, Sabet F, Zhou Z, Subramanian SV, Lu C. Contraceptive use in adolescent girls and adult women in low- and middle-income countries. JAMA Netw Open. 2020;3(2):1–15.
Machado-Alba JE. Inequalities in contraceptive use in Latin America and the Caribbean. Lancet Glob Heal. 2019;7(2):e169–70. https://doi.org/10.1016/S2214-109X(18)30534-5.
Munroe E, Hayes B. Private-sector social franchising to accelerate family planning access, Choice, and Quality : Results From Marie Stopes International. Global Health: Science and Practice. 2020;3(2):195–208.
Nuwamanya E, Nuwasiima A, Babigumira JU, Asiimwe FT, Lubinga SJ, Babigumira JB. Study protocol : using a mobile phone- based application to increase awareness and uptake of sexual and reproductive health services among the youth in Uganda. A randomized controlled trial. Reprod Health. 2018;15(1):1–12.
Nuwamanya E, Nalwanga R, Nuwasiima A, Babigumira J, Asiimwe F, Babigumira J, et al. Effectiveness of a Mobile phone application to increase access to sexual and reproductive health information, goods, and services Among University students in Uganda: a randomized controlled trial. Contracept Reprod Med. 2020;5(31):1–8.
Nalwanga R, Nuwamanya E, Nuwasiima A, Babigumira J, Asiimwe F, Babigumira J. Utilization of a mobile phone application to increase access to sexual and reproductive health information, goods, and services among university students in Uganda. Reprod Health. 2021;18(95):1–10.
Eva G, Quinn A, Ngo TD. Vouchers for family planning and sexual and reproductive health services: a review of voucher programs involving Marie Stopes international among 11 Asian and African countries. Int J Gynecol Obstet. 2015;130:E15–20.
Eva BG, Shah S, Quinn A, Ngo T. Are our voucher programmes working ? Evaluating our methods and results in six countries. 2015. (Research brief series). Available from: https://www.msichoices.org/media/2124/are-our-voucher-programmes-working-evaluating-methods-and-results-in-six-countries.pdf
Bellows B, Bulaya C, Inambwae S, Lissner CL, Ali M, Bellows B, et al. Family Planning Vouchers in Low and Middle Income Countries: A Systematic Review. Stud Fam Plann. 2016;47(4):357–70.
Nuccio BO, Reichwein B. Understanding clients and achieving FP2020 goals : Exit interviews help deliver client-centred services. 2013. (Research brief series). Available from: https://www.msichoices.org/media/2125/understanding-clients-and-achieving-fp2020-goals.pdf
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care Programmes. 4th ed: Oxford University Press; 2015. p. 461.
Kennedy EC, Mackesy-Buckley S, Subramaniam S, Demmke A, Latu R, Robertson AS, et al. The case for investing in family planning in the Pacific: costs and benefits of reducing unmet need for contraception in Vanuatu and the Solomon Islands. Reprod Health. 2013;10(1).
Erim DO, Resch SC, Goldie SJ. Assessing health and economic outcomes of interventions to reduce pregnancy-related mortality in Nigeria. BMC Public Health. 2012;12(1):1.
Hu D, Bertozzi SM, Gakidou E, Sweet S, Goldie SJ. The costs, benefits, and cost-effectiveness of interventions to reduce maternal morbidity and mortality in Mexico. PLoS One. 2007;2(8).
Goldie SJ, Sweet S, Carvalho N, Natchu UCM, Hu D. Alternative strategies to reduce maternal mortality in India: a cost-effectiveness analysis. PLoS Med. 2010;7(4).
Carvalho N, Salehi AS, Goldie SJ. National and sub-national analysis of the health benefits and cost-effectiveness of strategies to reduce maternal mortality in Afghanistan. Health Policy Plan. 2013;28(1):62–74.
Zakiyah N, Van Asselt ADI, Roijmans F, Postma MJ. Economic evaluation of family planning interventions in low and middle income countries. A systematic review. PLoS One. 2016;11(12):1–19.
Zakiyah N, van Asselt ADI, Setiawan D, Cao Q, Roijmans F, Postma MJ. Cost-effectiveness of scaling up modern family planning interventions in low- and middle-income countries: an economic modeling analysis in Indonesia and Uganda. Appl Health Econ Health Policy. 2019;17(1):65–76.
Ssewanyana S, Kasirye I. The cost effectiveness of family planning Services in Uganda. J African Dev. 2018;20(1):1–11.
Babigumira JB, Stergachis A, Veenstra DL, Gardner JS, Ngonzi J, Mukasa-Kivunike P, et al. Potential cost-effectiveness of universal access to modern contraceptives in Uganda. PLoS One. 2012;7(2):1–9.
Kaganda PN, Ssengooba F, Baine SO. PHP71 cost effectiveness analysis of facility and community based provision of family planning in Kampala. Value Heal. 2012;15(7):A301. https://doi.org/10.1016/j.jval.2012.08.613.
Chandra-Mouli V, McCarraher DR, Phillips SJ, Williamson NE, Hainsworth G. Contraception for adolescents in low and middle income countries: needs, barriers, and access. Reprod Health. 2014;11(1):1–8.
There Is Now More Public Access To The Implant. [cited 2020 Apr 19]. Available from: https://www.newvision.co.ug/new_vision/news/1316557/public-access-implant
Ministry of Health Uganda. Pharmaceutical Situation Assessment-Level II: Health Facilities Survey in Uganda. 2008; Available from: http://digicollection.org/hss/documents/s16377e/s16377e.pdf
Uganda Bureau of Statistics. National Population and Housing Census 2014- Main Report. Kampala; 2016. Available from: https://uganda.unfpa.org/sites/default/files/pub-pdf/CENSUS2014FinalResults_0.pdf.
Nuwasiima A, Nuwamanya E, Navvuga P, Babigumira JU, Asiimwe FT, Lubinga SJ, et al. Study protocol: incentives for increased access to comprehensive family planning for urban youth using a benefits card in Uganda. A quasi-experimental study. Reprod Health. 2017;14(1):1–10.
Alfred A. Living in Kampala Slum: A Socio-Economic Analysis in Ten Informal Settlements of Kampala. Kampala—Uganda. 2011. [cited 2020 Nov 14]. Available from: https://www.africabib.org/htp.php?RID=373489897
Nuwasiima A, Nuwamanya E, Nalwanga R, Babigumira J, Asiimwe F, Babigumira J. Effectiveness of the family planning benefits card (FPBC) program on increasing uptake of modern family planning services among the urban poor youth aged 18 to 30 years in Uganda, a quasi-experimental study. Forthcoming.
Prasad Sapkota V, Dhakal L, Raj AS. Economic burden of unintended pregnancies from societal perspective: a case of Nepal. Econ J Dev Issues. 2015;19(20):83–99.
Yazdkhasti M, Pourreza A, Pirak A, Abdi F. Unintended pregnancy and its adverse social and economic consequences on health system: a narrative review article. Iran J Public Health. 2015;44(1):12–21.
Deutsche Stiftung Weltbevoelkerung (DSW). Uganda Family Planning Budget Analysis 2019/20. 2020. [cited 2020 Nov 14]. Available from: www.dsw.org/en/wp-content/uploads/2020/05/A4HU-Infographic-National-v2.pdf
Uganda Bureau of Statistics. Statistical Abstract. 2018. [cited 2019 Jul 27]. Available from: www.ubos.org.
Management Sciences for Health. International medical products Price guide. Manag Sci Heal. 2016;443 Available from: www.msh.org.
Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–103.
Bank of Uganda| Exchange Rates. [cited 2020 Jan 22]. Available from: https://www.bou.or.ug/bou/bouwebsite/exchangerates.html
Uganda - Consumer price index. [cited 2020 Apr 28]. Available from: https://www.indexmundi.com/facts/uganda/consumer-price-index
Briggs A, Claxton C, Sculpher M. Decision modelling for health economics: Oxford University Press; 2006. p. 127.
Briggs AH. Handling uncertainty in combined endpoints. Pharmacoecnomics. 2000;17(5):479–500.
Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated health economic evaluation reporting standards (CHEERS) 2022 explanation and elaboration: a report of the ISPOR CHEERS II good practices task force. Value Heal. 2022;25(1):10–31. https://doi.org/10.1016/j.jval.2021.10.008.
Polis CB, Bradley SEK, Bankole A, Onda T, Croft T, Singh S. Contraceptive failure rates in the developing world: an analysis of demographic and health survey data in 43 countries. New York: Guttmacher Institute; 2016. Available from: https://www.guttmacher.org/sites/default/files/report_pdf/contraceptive-failure-rates-in-developing-world_1.pdf
Babigumira JB, Stergachis A, Veenstra DL, Gardner JS, Ngonzi J, Mukasa-kivunike P, et al. Estimating the costs of induced abortion in Uganda : a model-based analysis. BMC Public Health. 2011;11(1):904.
Cost-effectiveness of Reproductive Health Vouchers and Community Based Health Insurance in Uganda: African Strategies for Health. 2015. (Summary brief). Available from: https://www.msh.org/sites/msh.org/files/technical_brief_cbhi_rhv_cea_june_2015.pdf
Alfonso YN, Bishai D, Bua J, Mutebi A, Mayora C, Ekirapa-kiracho E. Cost-effectiveness analysis of a voucher scheme combined with obstetrical quality improvements: quasi experimental results from Uganda. Health Policy Plan. 2015;30(1):88–99.
Tozan Y, Sun S, Capasso A, Wang JS. Evaluation of a savings-led family-based economic empowerment intervention for AIDS-affected adolescents in Uganda : a four- year follow-up on efficacy and cost- effectiveness. PLoS One. 2019;14(12):1–13.
Acknowledgements
We want to thank all our partners, particularly International Medical Link Uganda, partner clinics, local leaders, and community health workers, for their contribution towards the success of this study.
Funding
The study was funded by Grand Challenges Canada under grand number R-ST-POC-1707-07296. Grand Challenges Canada did not have any role in the preparation of the protocol, analysis of the data, or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
EN conceived the study, analysed the data, and wrote the first draft of the manuscript. All authors revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The trial was approved by the Mbarara University of Science and Technology Ethical Review Committee and the Uganda National Council of Science and Technology and was registered at MUREC1/7 No. 10/05-17 on July 19, 2017. All participants consented before participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nuwamanya, E., Babigumira, J.B. & Svensson, M. Cost-effectiveness of increased contraceptive coverage using family planning benefits cards compared with the standard of care for young women in Uganda. Contracept Reprod Med 8, 21 (2023). https://doi.org/10.1186/s40834-022-00206-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40834-022-00206-8