Abstract
Background
Postpartum family planning is defined as the prevention of unintended pregnancy and closely spaced pregnancies through the first twelve months following childbirth. The immediate postpartum period is particularly favorable time to provide long-acting reversible contraception methods; and postpartum provision is safe and effective. Despite the advantages of long acting reversible contraception methods, they may be infrequently used in Ethiopia.
Objective
This study assessed the prevalence and associated factors of long-acting reversible contraceptive methods utilization among counseled mothers in immediate postpartum period.
Methods
A cross-sectional study was conducted on 393 women who gave birth at Jimma University Medical Centre from 12 November 2016 to 21 January 2017, Ethiopia. Data were collected by face-to-face interview using pre-tested structured questionnaire and by record reviewing using data compiling form; and analyzed using SPSS version 20. Logistic regression was used to identify associated factors for long acting contraceptive methods use. P-value less than 0.05 at 95% confidence level was taken as significance level.
Results
Prevalence of reversible long acting contraceptive methods utilization among immediate postpartum mothers was 53.2% (209/393) and more than three-fourths (78.0%) of participants used implanon. The most common reported reason for not using reversible long acting contraceptive methods was preference of other contraceptive methods like short acting contraceptives (25.5%). Having more than four alive kids (AOR 2.6, 95% CI: 1.15,5.95), high monthly income (≥1000 ETB) (AOR 2.4, 95% CI: 1.08,7.20), planning to delay next pregnancy by more than 2 years (AOR 4.0, 95% CI: 1.60,9.28), mothers with no fertility desire (AOR 2.0, 95% CI: 1.12,3.15), prior use of reversible long acting contraceptive methods (AOR 3.0, 95% CI: 1.30,7.20) and receiving counseling during antenatal care follow-up and before delivery (AOR 2.0, 95% CI: 1.01, 4.73) were associated with immediate postpartum reversible long acting contraceptive methods use.
Conclusion and recommendations
Although the prevalence of reversible long acting contraceptive methods utilization in immediate postpartum was high, counseling mothers during ANC follow-up and before delivery can further increase its utilization. Therefore, the need for providing counseling during ANC follow up and before delivery to increase utilization of immediate postpartum reversible long acting contraceptive methods use is emphasized.
Similar content being viewed by others
Background
Globally, the contribution of unintended pregnancy to maternal morbidity and mortality is significant [1]. Modern contraception is highly effective in preventing unintended pregnancy and reducing maternal mortality [2].
Reasons for unmet need are lack of services, limited choices, social disapproval, partner’s opposition, side effects and lack of knowledge about contraceptive options and their use [3,4,5]. Majority of women and girls with an unmet need for family planning are those who have recently given birth [6]. These vary by population and individual and made postpartum family planning programs difficult to design and administer [7].
Women are at risk of an unintended pregnancy in the period immediately after delivery [8]. Between 40 and 57% of women reported having unprotected intercourse before the routine 6-week postpartum visit [8,9,10]. Currently, WHO and USAID recommend the minimal live birth interval of 2 years to reduce the risks of abortion, miscarriage and still births [11, 12].
Postpartum contraceptive utilization is a primary strategy for reducing unintended pregnancy and optimizing birth spacing [13]. Long-acting reversible contraception methods are the most effective method of modern contraception [14]. LARC method is user-independent and once the device is inserted, the woman does not need any action to support ongoing effective utilization of the contraceptive [14]. It is more effective in preventing unintended pregnancy [15, 16]; has higher continuation rates than shorter-acting methods [16] and the return of fertility is rapid when removed [14, 16]. ACOG guidelines revised in 2012 advises that adolescents at high risk of unintended pregnancy should be encouraged to consider LARC methods as a contraceptive option [17]. WHO also supports the utilization of LARC methods for women of all ages [18]. LARC methods could prevent one in every three maternal deaths that causes related to pregnancy [19]. Immediate postpartum LARC methods insertion is recommended as best practices [20, 21]. Despite the higher expulsion rate, cost-benefit analysis data strongly suggest the superiority of immediate placement in the reduction of unintended pregnancy [22]. The hospital setting facilitates the availability of the contraception for the patient and the healthcare provider to motivate women for utilization of LARCs [8]. Ideally, women should be counseled prenatally about immediate postpartum LARC methods option for enabling informed decision making [21].
Ethiopia is the second most populous country in Africa with high maternal mortality ratio of 412 per 100,000 live births [12]. The Ethiopian government also set the goal to achieve a total fertility rate (TFR) of 2.1 by 2016 [23]. The government targeted 55% contraceptive prevalence rate by the year 2020, and 35% was expected to be LARC methods [23, 24]. From the statistics of EDHS 2016, LARC methods utilization was 8% for implant and 2% for IUD among married women whereas 11% for implant and 1% for IUD among sexually active unmarried women [12].
Although immediate postpartum is the best opportunity for LARC methods insertion, studies that documented LARC methods utilization and associated factors are very limited in Ethiopia. So, this study assessed prevalence and associated factors of LARC methods utilization among immediate postpartum mothers at one tertiary level teaching hospital in Jimma, Ethiopia. The findings of this study will have significant contribution at establishing strategic plans for local policy makers and NGOs working in the area.
Conceptual framework (Fig. 1).
Methods and materials
Study area and period
The study was conducted in Jimma University Medical Center (JUMC) at maternity ward from November 12, 2016 - January 21, 2017. JUMC is located in Jimma town at around 352 Km Southwest of Addis Ababa. It is the only teaching and referral hospital in the Southwestern part of the country, providing services for approximately 15 million people living in Jimma zone and Southwest Ethiopia. It is also serving as a clinical post graduate specialty teaching hospital for Obstetrics and Gynecology, Internal Medicine, Pediatrics and Child Health since 2005 and for Ophthalmology and Surgery since 2007. Department of Obstetrics and Gynecology has MCH unit, OPD, Family Planning unit, Referral unit, Gynecology and Maternity wards. The Maternity, Labor and Delivery ward has 60 beds in addition to seven first stage beds and 4 s stage couches. Services are provided by midwifes, medical interns and resident physicians and consultant Obstetricians and Gynecologists.
Study design
Institution based cross-sectional study design was used.
Study population
All immediate postpartum mothers counseled for LARCs utilization during the study period were the study population.
Inclusion criteria
All immediate postpartum mothers who counseled for LARCs utilization during the study period.
Exclusion criteria
Mothers with puerperal sepsis, chorioamnionitis, deep venous thrombosis (DVT), congestive heart failure (CHF), severe liver disease, and previous breast cancer.
Sample size determination and sampling technique
The required sample size was determined by using single population proportion formula considering 36.7% prevalence (taken from community based study) [25], 5% level of significance, 5% margin of error and 10% non-response rate.
Convenience consecutive sampling technique was used. Beginning from the first date of data collection, all postpartum mothers who were candidate and counseled for LARC methods use were involved till the desired sample size was reached.
Study variables
Dependent variable
Long acting reversible contraceptive methods utilization (Implanon, Jadle and IUDs) at immediate postpartum period.
Independent variables
Socio-demographic/economic variables (age, marital status, educational level, religion, ethnicity, occupation and residence, income, family size and husband support). Reproductive history of women (parity, number of live birth, prior outcome, mode of delivery, current birth outcome, and previous history of LARC methods use) and Prior LARC awareness (Prior used,Prior counseled and Ever heard).
Data collection process
Data were collected by face-to-face interview using pre-tested structured questionnaire and by record reviewing using data compiling form. The questionnaire was developed according to objective of the study after reviewing different literature relevant to the study. The data collectors were two midwives working at maternity ward and one resident physician assigned to family planning unit who were also counseling about family planning. Data collectors and supervisors were briefed about the objectives of the study and the data collection tool by the principal investigator. The principal investigator and supervisors closely supervised the overall activities of the data collection on daily basis to insure the completeness of the questionnaire, to give further clarification and support for data collectors.
Data quality management
The questionnaire was originally prepared in English and then translated to local languages (Afan Oromo and Amharic) and back translated to English to check for consistency of translation. The tool was pre-tested on 5% of the sample before actual data collection out of the selected health facility and necessary modifications were made based on nature of gaps identified. The midwives who collected the data were briefed on objective of the study, contents of the tool and how to approach participants for interview. On site supervision was carried out every day during the whole data collection period. At the end of each day, filled questionnaires were reviewed for completeness and consistency by supervisor and principal investigator. The data were cleaned and explored before analysis.
Operational definitions
Immediate postpartum period is the time duration the women stayed in hospital before discharge after delivery of the baby [8].
Long-acting revisable contraception methods are contraception that prevent pregnancy ranging from 3 to 12 years [12].
Data analysis
Data were entered into Epi Data Version 3.1, cleaned and analyzed using SPSS version 20. A descriptive analysis was carried out for each variable. Bivariate logistic regression was performed for independent variables that have adequate cell count to identify candidate variables for the multivariable logistic regression. Variables with p-value < 0.25 in bivariate analysis were entered into multivariable logistic regression model to determine independent effect of each covariate. Multicolinearity was assessed in linear regression with variance inflation factor (VIF) and none was found. Interaction was also assessed with Breslow-Day test and none was found. Model fitness was assessed by Hosmer-Lemeshow test and percentage of correct classification. In multivariable regression, association was analyzed at confidence level of 95% with their respective adjusted odds ratio and p-value of < 0.05.
Result
Socio- demographic/economic characteristics
Out of 393 mothers participated in the study, 41.7% of them were in the range of 25–29 years age group. The mean age value of these participants was 27 years. The majorities of participants were Muslims (239, [60.8%]), and Oromo (251, [63.9%]). Nearly all were married (373, [94.9%]), and near to one-third (31.6%) were housewives. Two third (63.1%) attended formal education of different levels and nearly half (185, [47.1%]) had monthly income between 1000 and 2500 ETB. The majorities (219, [55.7%]) of mothers were from rural (Table 1).
Reproductive characteristics
Close to two-thirds (257, [65.4%]) of mothers were between para 2 and 4; almost all (98.7%) of participants have at least one alive kid. About 30.8% of mothers had two children; and the mean number of alive children of participants was 2.59. Nearly one-third (118, [30.0%]) of the current births were not planned for a time. Just two-thirds (66.2%) of the respondent had a plan to have children in the future. For those mothers who had a plan to have a child in the future, over three-fourths (200, [76.9%]) want to have a child after 2 years (Table 2).
Awareness towards LARC, ANC follow up and prior LARC utilization history
Over three-fourths (309, [78.6%]) of the study participants ever heard about LARC methods from different sources. The main source of information was health workers (247, [79.9%]). Nearly 9 in ten (352, [89.6%]) of the study participant had at least one antenatal care visit (ANC) during the current last pregnancy. Only 106 (27%) had received counseling service on LARC methods during ANC visit. Ninety-two (23.4%) had previously used LARC method.
Out of these, 76(82.6%) used Implanon, 10(10.9%) used Jadelle/Sino implant and 6(6.5%) used IUD. Majorities of participants discontinued LARC because of the desire for pregnancy (Table 3).
Prevalence of LARC methods utilization
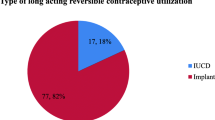
The prevalence of current LARC use was (209, [53.2%]) (95% CI: 48.2–58.1). Over three-fourths (78%) used Implanon, 11.5% used Jadelle/Sino Implant and 10.5% used IUD (Fig. 2). Various reasons were reported for not using LARC methods during study period. The commonest reported reason was preference of other form of contraceptive methods (25.5%) and others were fear of side effects, religious prohibition, want to use LARC methods other time, opposition from partner and want to have more children (Fig. 3).
Factors associated with LARC use
Bivariate and multivariable logistic regression analyses were done to identify factors associated with LARC method use. The results of these analyses showed that being counseled at ANC, monthly income greater than 1000 ETB, family size more than four, completed family size, having plan to delay next pregnancy beyond 2 years and prior use of LARC have increased chance of current immediate postpartum use of LARC methods.
Mothers who had monthly family income of 1000 ETB or more were 2.4 times more (AOR = 2.4, 95% CI: 1.08–7.20) likely to use LARC methods compared to mothers with monthly family income less than 1000 ETB. Mothers who had more than four alive kids were 2.6 times more (AOR = 2.6, 95% CI: 1.15–5.95) likely to use LARCs than mothers who had none or only one child. Women who completed family size (no desire for future fertility) were approximately two times more (AOR = 2.0, 95%CI: 1.12–3.15) likely to use LARC methods compared with women who need more children. Mothers who planned to extend next birth beyond 2 years were nearly four times more (AOR = 4.0, 95%CI: 1.60–9.28) likely to use LARC methods than mothers who planned next birth within next 2 years. Mothers who previously used LARC were three fold more (AOR = 3.0, 95% CI: 1.30–7.20) likely to use LARCs than mother who never tried it. Most importantly, mothers counseled for LARC during ANC visits were two fold higher (AOR = 2.0, 95%CI: 1.01–4.73) used LARC methods at immediate postpartum than mother who were not counseled (Table 4).
Discussion
We assessed the prevalence and associated factors for utilization of LARC methods among immediate postpartum mothers at JUMC, Southwest Ethiopia. The prevalence of current immediate postpartum LARC use was 53.2%. Over three-fourths (78%) used implanon followed by Jadelle/Sino Implant (11.5%) and IUD (10.5%). The commonest reported reason for not using LARC was preference of other contraceptive methods like short acting contraception. Being counseled at ANC, monthly income greater than 1000 ETB, family size more than four, completed family size, having plan to delay next pregnancy beyond 2 years and prior use of LARC have increased chance of current immediate postpartum use of LARC methods.
The prevalence estimated in our study was much higher than national estimates where only 10% of women used LARC as reported in EDHS 2016 [12]. This could be because of the fact that national estimate was for all reproductive age group women whether married or unmarried. But, our study was limited to specific group of women (immediate postpartum women) who are more likely to accept LARCs. The proportion of women who used IUD in our study was much lower than 21.9% prevalence of immediate postpartum IUD use reported by facility based cross-sectional study conducted in Southern Ethiopia [26]. Though there was similar proportion of ANC use (89.6% vs 84.2%), there was significantly lower proportion of counseling for LARCs at ANC (27% vs 72.3%) and all were counseled at postpartum in our study. Hence, the lower percentage of IUD use could be because of the combination of lower proportion of counseling at ANC and availability of alternative LARC options in our study but, only IUD in the case of study conducted in Southern Ethiopia [26]. However, it was similar to 12.4% prevalence of immediate IUD use reported by facility based cross-sectional study conducted in Bale zone, Southeast Ethiopia which reported similar proportion (87.6%) of ANC use [27].
Our finding was also higher than 36.7% [25] prevalence of LARC use in the extended postpartum period (42 days to 1 year) reported by community based cross-sectional study conducted in Southern Ethiopia. But the proportion of women counseled for LARC was significantly lower in our study (27% versus 51.5%). This indicates that LARC acceptance is better at immediate postpartum and mothers may change their mind and reject LARC offer at extended postpartum even if they were willing to use it at immediate postpartum.
Our finding was also higher than 22.9% [28] and 16% [29] prevalence of LARC use among family planning attendees of public health facilities in Jimma town, Southern Ethiopia. It was also higher than 38% [30], 29.1% [31], 37.7% [32], 25.2% [33], 28.3% [34], 30.3% [35] and 23.8% [36] prevalence of LARC use among family planning clients reported by community based studies conducted in different parts of Ethiopia. It was also higher than 33.7% [37], 16.4% [38], 33.7% [39], 16.3% [40], 28% [41], 17.6% [42] and 9.24% [43] prevalence of LARC use among family planning clients reported by facility based cross-sectional studies conducted in different parts of Ethiopia. The finding was also higher than 37.4% [44] prevalence of LARC use among HIV positive family planning attendees of public health facilities in Bahir Dar town, Northern Ethiopia. We also calculated 23.84% pooled prevalence from eighteen facility or community based cross-sectional studies conducted in different corners of Ethiopia [25, 28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44] and found that our finding was higher than pooled prevalence.
Regarding type of LARC use, birth control Implant was the method used by almost 9 out of ten mothers. This finding was in line with findings of most previous studies conducted in different parts of Ethiopia where Implant was used by at least three-fourths of mothers [25, 28,29,30,31,32,33,34, 36, 38, 40, 41, 43,44,45] and higher than findings of some studies [35, 37, 39]. This could be because of convenience and privacy as implants are inserted under the skin into the upper arm area whereas IUDs are inserted into the uterus. Thus, women may think that it’s painful while inserting IUDs into uterus especially during immediate postpartum and/or during sexual intercourse and/or while walking. They may also think that it can cause damage to the uterus. In facility based cross-sectional study conducted in Bale zone, Ethiopia, one-third of study participants agreed and only one-fifth disagreed that insertion and removal of IUD is highly painful. In the same study, more than one-third (37.6%) agreed that insertion of IUD causes loss of privacy and 41.6% agreed that IUDs may impair future fertility [27]. In another community based study cross-sectional study, nearly one-third (31%) of study participants disagreed with the statement “insertion of intrauterine contraceptive devices does not lead to loss of privacy”. Similarly, nearly half (46%) disagreed with the statement “using intrauterine contraceptive devices does not restrict normal activities” [36].
In this study, counseling at ANC was significantly associated with immediate postpartum LARC utilization. Studies conducted in different corners of Ethiopia reported that women counseled at ANC and/or during delivery and/or postpartum and/or received postnatal care were more likely to use LARC [25, 26, 34]. This could because women who received postnatal care were likely to be counseled for LARC and counseling increases women’s knowledge of LARC including its advantage and disadvantage and clears misconceptions increasing chance of LARC use. Previous studies have reported that women who heard [26], had awareness [40], had information [33] about LARC, had moderate or high knowledge of LARC [31, 37, 39, 45] or previously used it [25, 28, 41] were more likely to utilize it now. Prior use of LARC was also positively associated with current use of LARC in our study which was in line with literature. Studies have also reported that women with misconception [31, 36] and who heard myths [44] were less likely to use LARC. On the other hand, positive/supportive attitude towards LARC [31, 38], not hearing myths [29], health professionals being source of information [45] and discussion of LARC with providers [29] were positively associated LARC use. Similarly, maternal literacy was also positively associated with LARC use [25, 27, 28, 30,31,32, 34, 37, 39, 40, 42] because education is likely to enhance women’s autonomy and confidence to make decision regarding their own health and demand higher quality of life. The association between prior use of LARC and current acceptance is an indication of knowledge influence.
In general, counseling builds knowledge of LARC, clears misconception and myths about LARC, develops positive/supportive attitude and finally leads to increased use of LARC. However, although counseling for postpartum family planning is also acceptable during early labor and immediately postpartum, it should optimally begin during ANC according to WHO recommendations [46] and it is the ideal time to counsel women. In this study, however, only 27% of participants were counseled at ANC follow up though all were counseled at immediate postpartum. This finding indicates the importance of integrating counseling for post-partum family planning into ANC and/or early labor and/or the immediate postpartum period to increase postpartum LARC utilization.
Strength and limitations of study
Integrating counseling for post-partum family planning at immediate postpartum period increased postpartum LARC utilization.
This study was institution based and the respondents were immediate postpartum mothers (48 hours before hospital discharge) who were counseled for LARC. Therefore, the study findings may be not be generalized to all reproductive age women in the community. Counseling for contraception options was done after delivery but is better addressed before delivery especially for IUD to be inserted just post-placental delivery in either vaginal or cesarean delivery. Another limitation of this study was some mothers might have been discharged from the hospital before counseled and interviewed though we were actively looking for all postpartum mothers. The study was done in 2016–2017. In addition, convenience consecutive sampling technique is used which affects generalization of the study.
Implications for research and policy
The findings of this study will be baseline data for future researchers and local policy makers working on the area of the study.
Conclusion and recommendations
The advantages of postpartum contraceptive use for wellbeing of mother and child cannot be overemphasized. The prevalence of immediate postpartum LARC use was promising with implant the most preferred method by mothers. Counseling at ANC follow up, monthly income greater than 1000 ETB, family size more than four kids, completed family size (no future desire for fertility), having plan to delay next pregnancy beyond 2 years and prior use of LARC were important factors associated with increased chance of uptake of LARC methods at immediate postpartum period. This is the indication of importance of knowledge on LARC methods that clears misconceptions or myths and builds positive/supportive attitude, ultimately leading to increased utilization of LARC methods. Therefore, it is recommended to consider counseling for LARC methods in continuum starting at ANC follow-up through postpartum period.
Availability of data and materials
All datasets on which the conclusions of the paper rely were presented in the main manuscript.
Abbreviations
- ACOG:
-
American College of Obstetricians and Gynecologists
- ANC:
-
Antenatal Care
- CHF:
-
Congestive heart failure
- CBE:
-
Community based education
- DVT:
-
Deep venous thrombosis
- EDHS:
-
Ethiopian Demographic and Health Survey
- ETB:
-
Ethiopian Birr
- IUDs:
-
Intra Uterine Devices
- JUMC:
-
Jimma University Medical Centre
- LARC:
-
Long reversible contraceptive
- MCH:
-
Maternal and child health
- OPD:
-
Outpatient department
- PPFP:
-
Postpartum family planning
- TFR:
-
Total fertility rate
- USAID:
-
United States Agency for International Development
- WHO:
-
World Health Organization
References
World Health Organization. From evidence to policy: expanding access to family planning – strategies to increase use of long-acting and permanent contraception. WHO Policy Brief, 2012. Available from: http://apps.who.int/iris/bitstream/10665/75161/1/ WHO_RHR_HRP_12.20_eng.pdf?ua=1.
Bekele D, Fantahun M, Gutema K, Getachew H, Lambiyo T, Yitayal M. Family planning module for the Ethiopian health center team. Ethiopia: Hawassa University, Ethiopia Public Health Training Initiative, The Carter Center, EMOH, EMOE; 2003.
World Health Organization. Department of Reproductive Health and Research (WHO RHR) and Johns Hopkins Bloomberg School of Public Health ,Center for Communication Programs (CCP). Geneva: Family Planning: A Global Handbook for Providers; 2007.
World Health Organization, UNICEF, UNFPA and The World Bank, UNICEF, UNFPA, The World Bank. Trends in maternal mortality: 1990 to 2008; Estimates developed by WHO, UNICEF, UNFPA and The World Bank. 2010.
Black KI, Bateson D, Harvey C. Australian women need increased access to long-acting reversible contraception. Med J Aust. 2013;199(5):317–8 [cited 2018 Nov 4]. Available from: https://www.mja.com.au/journal/2013/199/5/australian-women-need-increased-access-long-acting-reversible-contraception.
IUSSP Scientific Panel on Reproductive Health. Promoting postpartum and post-abortion family planning: challenges and opportunities. Cochin, India; 2014.
Cleland J, Shah IH, Benova LA. Fresh look at the level of unmet need for family planning in the postpartum period, its causes and program implications. Int Perspect Sex Reprod Health. 2015;41(3):155–62.
Jackson E, Glasier A. Return of ovulation and menses in postpartum nonlactating women: a systematic review. Obstet Gynecol. 2011;117(3):657 [cited 2018 Nov 6]. Available from: https://journals.lww.com/greenjournal/Abstract/2011/03000/Return_of_Ovulation_and_Menses_in_Postpartum.20.aspx.
Brito MB, Ferriani RA, Quintana SM, MEHD Y, de Sá MFS, Vieira CS. Safety of the etonogestrel-releasing implant during the immediate postpartum period: a pilot study. Contraception. 2009c;80(6):519–26 [cited 2018 Nov 6]. Available from: https://www.contraceptionjournal.org/article/S0010-7824(09)00277-7/fulltext.
Connolly A, Thorp J, Pahel L. Effects of pregnancy and childbirth on postpartum sexual function: a longitudinal prospective study. Int Urogynecol J. 2005;16(4):263–7 [cited 2018 Nov 6]. Available from: https://link.springer.com/article/10.1007/s00192-005-1293-6.
Alene GD, Worku A. Estimation of the total fertility rates and proximate determinants of fertility in north and South Gondar zones, Northwest Ethiopia: an application of the Bongaarts’ model. EthiopJHealth Dev. 2009;23(1):19–27.
Central statistical agency (CSA) [Ethiopia] and ICF. Ethiopia demographic and health survey 2016: key indicators report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016.
Zapata LB, Murtaza S, Whiteman MK, Jamieson DJ, Robbins CL, Marchbanks PA, et al. Contraceptive counseling and postpartum contraceptive use. Am J Obstet Gynecol. 2015 Feb;212(2):171.e1–8.
Long-acting reversible contraception: implants and interuterine devices. ACOG Practice Bulletin No. 121, 2015.
Winner B, Peipert JF, Zhao Q, Buckel C, Madden T, Allsworth JE, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366(21):1998–2007.
Guttmacher institute. Contraceptive Use in the United States: Fact Sheet 2015.
Committee on adolescent health care long-acting reversible contraception working group, the American College of Obstetricians and Gynecologists. Committee opinion no. 539: adolescents and long-acting reversible contraception: implants and intrauterine devices. Obstet Gynecol. 2012;120(4):983–8.
Kempner M. Providing LARCs to young women: effectiveness, acceptability, and efforts to increase Use [internet]. Advocates for youth; 2012. Available from: https://www.advocatesforyouth.org/storage/advfy/documents/providinglarcstoyoungwomen.pdf.
PRB staff. World population highlights: key findings from PRB’s 2009 world population data sheet. Popul Bull. 2009;64(3).
Committee on Adolescent Health Care Long-Acting Reversible Contraception Working Group, The American College of Obstetricians and Gynecologists. Committee Opinion No. 642: Increasing Access to Contraceptive Implants and Intrauterine Devices to Reduce Unintended Pregnancy. Obstet Gynecol. 2015;126(4):e44.
Committee on Adolescent Health Care Long-Acting Reversible Contraception Working Group, The American College of Obstetricians and Gynecologists. Committee Opinion No. 670: Immediate Postpartum Long-Acting Reversible Contraception. Obstet Gynecol. 2016;128(2):e32.
Washington CI, Jamshidi R, Thung SF, Nayeri UA, Caughey AB, Werner EF. Timing of postpartum intrauterine device placement: a cost-effectiveness analysis. Fertil Steril. 2015;103(1):131–7.
FMoH, planning and prorating department, Ministry of health Ethiopia. Health and health related indicator Addis Ababa Ethiopia. 2010.
DKT Ethiopia. long-acting methods: Ethiopia’s Next Family Planning Success Story [Internet]. Available from: http://www.dktethiopia.org/content/long-acting-methods-ethiopia%E2%80%99s-next-family-planning-success-story
Tamrie YE, Hanna EG, Argaw MD. Determinants of long acting reversible contraception method Use among mothers in extended postpartum period, Durame town, southern Ethiopia: a cross sectional community based survey. Health (N Y). 2015;30(07):1315.
Tefera LB, Abera M, Fikru C, Tesfaye DJ. Utilization of immediate post-partum intra uterine contraceptive device and associated factors: a facility based cross sectional study among mothers delivered at public health facilities of Sidama zone, South Ethiopia. J Pregnancy Child Health. 2017;4(3):1–8.
Gonie A, Worku C, Assefa T, Bogale D, Girma A. Acceptability and factors associated with post-partum IUCD use among women who gave birth at bale zone health facilities, Southeast-Ethiopia. Contracept Reprod Med. 2018;6:3 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6219260/.
Tebeje B, Workneh D. Prevalence, perceptions and factors contributing to long acting reversible contraception Use among family planning clients, Jimma town, Oromiya region, South-West Ethiopia. J Womens Health Care. 2017;6(1):1–10.
Taye A, Woldie M, Sinaga M. Predictors of long acting reversible contraceptive use among married women visiting health facilities in Jimma town. J Womens Health Care. 2015;4(1):1–7.
Shiferaw K, Musa A. Assessment of utilization of long acting reversible contraception and associated factors among women of reproductive age in Harar City, Ethiopia. Pan Afr Med J. 2017;28 [cited 2018 Nov 8]. Available from: http://www.panafrican-med-journal.com/content/article/28/222/full/.
Biza N, Abdu M, Reddy PS. Long Acting Reversible Contraceptive Use and Associated Factors Among Contraceptive Users in Amhara Region, Ethiopia, 2016. A community based cross sectional study. Medico Research Chronicles. 4(5):469–80.
Kabalo MY. Utilization of reversible long acting family planning methods among married 15-49 years women in Areka town, Southern Ethiopia. Int J Sci Rep. 2016;2(1):1–6.
Meleko A, Sileshi S, Bekele Y, Daniel A, Getawey A, Amare D, et al. Utilization of long acting reversible contraceptive methods and its associated factors among women of reproductive age groups in Mizan – Aman town, bench Maji zone, south West Ethiopia. J Womens Health Issues Care. 2018; [cited 2018 Nov 18];2017. Available from: https://www.scitechnol.com/peer-review/utilization-of-long-acting-reversible-contraceptive-methods-and-its-associated-factors-among-women-of-reproductive-age-groups-in-m-BbS9.php?article_id=7041.
Abraha TH, Teferra AS, Gelagay AA. Postpartum modern contraceptive use in northern Ethiopia: prevalence and associated factors. Epidemiol Health. 2017;39:e2017012.
Fekadu H, Kumera A, Yesuf E, Hussien G, Tafa M. Prevalence and determinant factors of long acting contraceptive utilization among married women of reproductive age in Adaba town, West Arsi Zone, Oromia, Ethiopia. J Womens Health Care. 2017;06(01) Available from: https://www.omicsgroup.org/journals/prevalence-and-determinant-factors-of-long-acting-contraceptive-utilizationamong-married-women-of-reproductive-age-in-adaba-town-w-2167-0420-1000360.php?aid=86627.
Yemaneh Y, Birie B. Assessment of Knowledge, Attitude and Utilization of Long Acting Family Planning Method among Women of Reproductive Age Groupe in Mizan-Aman Twon, Bench-Majizone, South West Ethiopia, 2016. Integr J Glob Health [Internet]. 2017 Aug. 1(2): 16. [cited 2018 Nov 18]. Available from: http://www.imedpub.com/abstract/assessment-of-knowledge-attitude-and-utilization-of-long-acting-family-planning-method-among-women-of-reproductivernage-groupe-in-mizanaman-twon-benchmajizone-south-west-ethiopia-2016-19988.html.
Tulu AS, Gebremariam T. Utilization of reversible long acting contraceptive methods and associated factors among women getting family planning Service in Governmental Health Institutions of Gondar City Administration, Northwest Ethiopia. Int J Health Sci Res. 2018;8(2):178–87.
Gebremichael H, Haile F, Dessie A, Birhane A, Alemayehu M, Yebyo H. Acceptance of long acting contraceptive methods and associated factors among women in Mekelle City, northern Ethiopia. Sci J Public Health. 2014;2(4):349.
Mariam T, Kebede Y, Shibiru A. Utilization of reversible long acting contraceptive methods and associated factors among women getting family planning Service in Governmental Health Institutions of Gondar City, Northwest Ethiopia 2015. Austin J Public Health Epidemiol. 2018;5(1):1069.
Megersa K, Kumera Y, Gudissa T, James A. Assessment of long acting contraceptive methods utilization and associated factors among reproductive age group women attending maternal and child health Clinic of Ambo Town Health Facilities, Oromia region. Central Ethiopia J Pregnancy Child Health. 2018;5(1):1–5.
Mohammed E, Tadese L, Agero G. Acceptance of long acting reversible contraceptive methods and associated factors among reproductive age women in Adama town, Oromia regional state, Ethiopia. Clin Med Res. 2017;6(2):53.
Sahilemichael A. Determinants of long acting reversible contraceptives Use among child bearing age women in Dendi District, Western Ethiopia. J Womens Health Care [Internet]. 2015;04(04) Available from: http://www.omicsgroup.org/journals/determinants-of-long-acting-reversible-contraceptives-use-among-childbearing-age-women-in-dendi-district-western-ethiopia-2167-0420-1000242.php?aid=57527.
Yalew SA, Zeleke BM, Teferra AS. Demand for long acting contraceptive methods and associated factors among family planning service users, Northwest Ethiopia: a health facility based cross sectional study. BMC Res Notes. 2015;4:8 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4340161/.
Gelagay AA, Koye DN, Yeshita HY. Demand for long acting contraceptive methods among married HIV positive women attending care at public health facilities at Bahir Dar City, Northwest Ethiopia. Reprod Health. 2015;27:12 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4551468/.
Birhane K, Tsegaye W, Mulaw A, Nemomsa C, Abebe G, Derese G, et al. Utilization of long acting reversible contraceptive methods and associated factors among female college students in Debre Berhan town, Ethiopia. Adv Appl Sci. 2016;1(1):18.
World Health Organization. Medical eligibility criteria for contraceptive use. 2015.
Acknowledgements
We would like to extend our gratitude to Jimma University for the opportunity and financial assistance. We are also grateful to participants of this study and data collectors and supervisors. We are also grateful to The American College of Obstetricians and Gynecologists for giving us the opportunity to present the abstract at the conference and publish it in their journal.
Conflict of interest
The abstract of this paper was presented at The American College of Obstetricians and Gynecologists as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Obstetrics & Gynecology; May 2018 - Volume 131 - Issue - p 68S: https://journals.lww.com/greenjournal/Abstract/2018/05001/Prevalence,_and_Pattern_of_LARC_Use_in_Immediate.235.aspx.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors made a significant contribution to this study. They participated in study conception, design, execution, analysis, and interpretation effectively. Moreover, they took part in drafting, revising, or critically reviewing the first draft. Furthermore, they gave their approval for the final version to be published. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval of the study was obtained from Institutional Review Board (IBR) of Institute of Health, Jimma University. Before interview, Informed, voluntary, written and signed consent was obtained from study participants after telling them the objective and procedure of data collection. Participants were also told that they can withdraw from the study at any time and as their responses would not result in any harm to them. Name and other personal identifiers were not requested and participants were given unique code to assure confidentiality. Collected information was not disclosed to anyone who is not member of research team.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is not any conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Arero, W.D., Teka, W.G., Hebo, H.J. et al. Prevalence of long-acting reversible contraceptive methods utilization and associated factors among counseled mothers in immediate postpartum period at Jimma University medical center, Ethiopia. Contracept Reprod Med 7, 17 (2022). https://doi.org/10.1186/s40834-022-00184-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40834-022-00184-x