Abstract
Bioactive glasses are a group of bioceramic materials that have extensive clinical applications. Their properties such as high biocompatibility, antimicrobial features, and bioactivity in the internal environment of the body have made them useful biomaterials in various fields of medicine and dentistry. There is a great variation in the main composition of these glasses and some of them whose medical usage has been approved by the US Food and Drug Administration (FDA) are called Bioglass. Bioactive glasses have appropriate biocompatibility with the body and they are similar to bone hydroxyapatite in terms of calcium and phosphate contents. Bioactive glasses are applied in different branches of dentistry like periodontics, orthodontics, endodontics, oral and maxillofacial surgery, esthetic and restorative dentistry. Also, some dental and oral care products have bioactive glasses in their compositions. Bioactive glasses have been used as dental implants in the human body in order to repair and replace damaged bones. Other applications of bioactive glasses in dentistry include their usage in periodontal disease, root canal treatments, maxillofacial surgeries, dental restorations, air abrasions, dental adhesives, enamel remineralization, and dentin hypersensitivity. Since the use of bioactive glasses in dentistry is widespread, there is a need to find methods and extensive resources to supply the required bioactive glasses. Various techniques have been identified for the production of bioactive glasses, and marine sponges have recently been considered as a rich source of it. Marine sponges are widely available and many species have been identified around the world, including the Persian Gulf. Marine sponges, as the simplest group of animals, produce different bioactive compounds that are used in a wide range of medical sciences. Numerous studies have shown the anti-tumor, anti-viral, anti-inflammatory, and antibiotic effects of these compounds. Furthermore, some species of marine sponges due to the mineral contents of their structural skeletons, which are made of biosilica, have been used for extracting bioactive glasses.
Similar content being viewed by others
Introduction
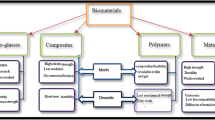
Over the past hundred years, investigations on materials used in dentistry have expanded dramatically [1]. Natural biomaterials such as collagen, fibrin, chitosan, hyaluronic acid, alginate, and agar as well as organic synthetic biomaterials such as polylactic acid (PLA), polyglycolic acid (PGA), poly lactide-co-glycolic acid (PLGA), and polycaprolactone (PCL), and on the other hand inorganic synthetic materials such as hydroxyapatite (HA), beta-tricalcium phosphate (β TCP) and compositions of silicate and phosphate glasses have been used in the field of dental tissue engineering [2]. Recently, new researches in the field of biomaterials have focused on tissue engineering and tissue regeneration [3]. Bioactive glass is one of the biomaterials that has revolutionized modern biomaterial-driven regenerative medicine by innovating applications in biomedicine, such as soft tissue repair and drug delivery and also, cases of its clinical applications have also been identified [4].
The first bioactive glass was invented by Larry L. Hench in 1969 [5]. According to L. Hench’s studies [6], if a substance produces a biological response that leads to a bond between the substance and tissues, it can be classified as bioactive material. Bioactive glass is based on silicate and its structure is composed of three-dimensional networks of silica when they are placed in the body they can be able to form strong chemical bonds with tissues, especially with bones [7]. Bioactive glasses dissolve when they are exposed to body fluids and then by forming the apatite crystals on their surface, they gain the ability to chemically bond with the apatite crystals which are present in bone and tooth tissues [8]. Bioactive glass has high biocompatibility and is also a type of ceramic presenting some properties of ceramics [9]. Ceramics are brittle, inorganic, and non-metallic biomaterials composed of metal-oxygen ionic bonds, and they are poor thermal conductors because they have no free electrons in their structure to transfer heat or electricity [9]. In addition, bioactive glass has several attractive properties including biocompatibility and antimicrobial properties that make it a suitable material for use as a scaffold in tissue engineering [10].
Nowadays, various biomaterials have been obtained from marine resources and attention to the seas as an accessible and natural source is increasing [11]. More than 25,000 biologically-active compounds have been identified from marine habitats [12, 13]. Marine sponges are simple invertebrate animals that are known as chemical factories in the sea because they can produce numerous different chemical compounds in water [14, 15]. Different compounds of various species of marine sponges have been studied so far [16]. Although the bioactive compounds of marine sponges show diverse chemical properties, they have great potential for application in the medical sciences [14]. The bioactive compounds of marine sponges are used in a wide range of treatments due to their antitumor, antiviral, anti-inflammatory, and antibiotic effects [17]. One of the prominent and distinguished features of the marine sponges is their ability to produce amorphous inorganic skeletal elements from hydrated silica (silica spicule) or calcium carbonate (calcareous spicule) [18]. In the skeleton of most sponges, there are silica spicules that stabilize the animal’s body structure and also play a defensive role against predators [19]. Marine sponges have been used in the production of bioactive glasses due to their mineral components such as biosilica [17, 20]. Marine sponges with silica spicules are found in the Persian Gulf [21]. These sponges can be considered as a suitable source for the production of bioactive glasses which can be used in various fields of dentistry.
Bioactive glasses and their chemical structures
Bioactive glasses have different types according to their constituents [22]. There are many variations in the main composition of these glasses, some of them are approved by the US Food and Drug Administration (FDA) for therapeutic applications and they are known as Bioglass [4]. For example, Bioglass 45S5 and S53P4 for clinical applications are approved by the FDA [23]. Bioactive glasses have good biocompatibility properties and are similar to bone hydroxyapatite in terms of calcium and phosphate contents [24]. Bioactive glasses make it possible to bond and integrate with bone tissues by forming a layer of silica gel which stimulates the proliferation and differentiation of osteoblast cells and initiates the synthesis and deposition of organic bone matrix [25]. Therefore, bioactive glasses are widely used in medicine and dentistry [22]. For example, the first clinical application of bioactive glass was reported after applying Bioglass 45S5 for the treatment of conductive hearing loss by reconstructing the bony structures of the middle ear [26]. Up to now, more than 1.5 million people worldwide have been treated with Bioglass 45S5 [27].
There are three types of bioactive glasses, including silicate-based glass (SiO2), phosphate-based glass (P2O5), and borate-based glass (B2O3) [9]. The main formulation commercially is called Bioglass 45S5 which contains 45% SiO2, 24.5% Na2O, 24.5% CaO, and 6% P2O5 [28]. In addition, bioactive glasses may contain well-known biocompatible and bioactive minerals such as fluorapatite, wollastonite, diopside, and tricalcium phosphate [29, 30]. For example, an alkali-free (Na-free) bioactive glass with a formulation of 70% diopside, 10% fluorapatite, and 20% tricalcium phosphate is commercially known as FastOs BG [30]. Much more researches have been focused on changing the composition of Bioglass 45S5 by adding or removing ions to make the materials more compatible for different clinical applications [8]. Recently a novel crystallized bioactive glass-ceramic with the formulation of SiO2 48.5%, Na2O 23.75%, CaO 23.75% and P2O5 4.0% has been presented and is called Biosilicate which has several applications in medical sciences [31]. Table 1 shows the chemical composition of bioactive glasses.
Application of bioactive glasses in dentistry
Bioactive glasses by having different advantages including having the ability to support the structure of biological tissues, being good scaffolds, and also preventing the growth of bacteria become so useful in different fields of dentistry [9]. Various applications of bioactive glasses in dentistry are mentioned in the following and briefly brought in Fig. 1. Also, some of the bioactive glasses used in dentistry are listed in Table 2.
Despite the widespread use of bioactive glass in dentistry, there are challenges to their widespread use. For example, repairing bone defects in orthopedic and dental surgery remains a major challenge. The mechanical limitations of existing glass scaffolding, along with related challenges and strategies for further improvement, need further study. In addition, emerging applications of bioactive glasses in contact with soft tissues require relative revision of biomechanical issues inorder to match the adaptation of delicate collagen tissues [49].
Application in oral care products
Bioactive glasses have been used in various dental products especially toothpaste [33, 50]. It has been observed that bioactive glasses are useful in the formulation of toothpaste because they can release antibacterial agents, stimulate remineralization and reduce hypersensitization [24]. One of the bioactive glasses is called NovaMin which is used as an active ingredient in toothpaste to increase remineralization and reduce tooth sensitivity [51]. NovaMin (calcium-sodium-phosphate silicate) can release calcium and phosphate ions. These ions raise the pH and lead to the deposit of calcium phosphate and its conversion to hydroxyapatite [52]. NovaMin in comparison to other calcium-based products which shows an initial burst of calcium provides continuous release of calcium [53]. BiominF is another commercial product of bioactive glass which includes fluoride and phosphate and induces the formation of fluorapatite (FAP) [54]. In 2021, the first toothpaste containing bioglass and fluoride received FDA approval [55]. This toothpaste can improve acid-resistant fluorapatite on the tooth surface and inside exposed dentine tubules by controlling the release of calcium, phosphate, and fluoride ions gradually for many hours after brushing [55].
Application in periodontics and dental implants
Periodontitis is a common chronic multifactorial inflammatory disease of the periodontium that can cause clinical attachment loss, alveolar bone loss, periodontal pocket, and gingival bleeding because of loss of periodontal tissue support [56]. This condition can also lead to alveolar bone resorption and loosening of teeth [57]. Periodontitis can cause inflammation developments around dental implants which ultimately increases the risk of implant detachment and treatment failure [58]. To improve the prognosis of dental implants, reconstruction of bone defects is essential [59]. Research on dogs has shown that bioactive glass particles have the ability to treat periodontal defects by increasing bone mineralization [60]. One of the bioactive glasses that affects bone defects is PerioGlas which has a similar formulation to Bioglass 45S5 and is widely used as a grafting material in bone grafts to regenerate periodontal osseous defects [61, 62]. PerioGlas contains 90 to 710 μm bioactive glass particles, so it can penetrate into bone defects and stimulate bone regeneration in periodontal surgeries [63, 64]. The results of bone biopsies after using PerioGlas granules as fillers in the site of tooth extraction showed new bone augmentation and confirmed good bioactivity of PerioGlas and also after a two-year clinical follow-up successful loading of the implants and evidence for implant stability were shown [65]. Also, PerioGlas reduced probing depth significantly and gained clinical attachment level (CAL) in periodontal intrabony defects [66]. So that if the amount of the harvested bone is not sufficient for the treatment of moderate to severe chronic periodontitis the mixture of autogenous bone and PerioGlas can be effective because it had similar clinical attachment gain to autogenous graft [66]. PerioGlas as a bioactive alloplast was well-tolerated by the gingival tissues [67]. Radiographs of each periodontal osseous defect and measuring of defect depth from the alveolar crest to the base of the bone defects using a Williams graduated periodontal stent demonstrated the significant improvement in bone fill when the bioactive glass is used [67].
Additionally to the bone grafting application of bioactive glasses, silica-based bioactive glasses have been used for covering implants, too [68]. The use of nanotechnology in the synthesis of bioactive glass has enhanced its application as a coating material on the surfaces of dental implants [69]. A wide range of implants are made of titanium and in some studies, bioactive glass has been used on titanium implants [70]. Covering implants with bioactive glass prevents infection and inflammation around the implants due to their antimicrobial properties [71]. The bioactive glasses increase titanium implants bond to the bone and promote their bioinert nature of them so that they reduce the total time of treatment [72,73,74]. In vivo, animal studies demonstrate that the titanium implants coated with bioactive glasses show significantly more osseointegration than control dental implants [75, 76]. A clinical trial was performed on 31 patients to evaluate and compare the behavior of hydroxyapatite and bioactive glass-coated implants (62 implants) in bone tissue after implantation [74]. The results showed bioactive glass coating materials were biocompatible and nontoxic and bioactive glass-coated implants were as equally successful as hydroxyapatite in achieving osseointegration and supporting final restorations. so that glass-coated implants were a viable alternative coating material for dental implants, which may allow for wider case selection criteria together with improved integration rates even in the more challenging medically compromised and osteoporotic patients [74].
Application in orthodontics
In orthodontics, dental adhesives help to attach or bond a compound to another substance such as attachment of dental composites or orthodontic brackets to the natural tissue of the teeth [77]. The composite resin is hydrophobe and the tooth surface is hydrophile but the bonding of dental resin composite overcomes it. Thus, the adhesive acts as an interface between the two materials [77]. Adhesion of orthodontic brackets can make favorable conditions for the presence of bacteria which may lead to demineralization of the tooth and the formation of white spot lesions (WSLs) [77]. To prevent such conditions oral hygiene maintenance, regular and correct brushing, and use of fluoride toothpaste and mouthwashes are recommended [78]. Bioactive glasses have the ability to remineralize these white spot lesions [79]. Based on laboratory-based findings, the remineralization effects of bioactive glasses can be compared with topical fluoride and milk protein-derived casein phosphopeptide-amorphous calcium phosphate (CPP-ACP). These findings show that bioactive glasses enhance enamel remineralization more effectively and faster. However, clinical trials are needed to confirm their effectiveness [80]. One study found that orthodontic adhesives with bioactive glass and fluoride enhance the strength of apatite structure which may play a clinical role in preventing the formation of white spot lesions [24]. Another study found that orthodontic bonding agents containing bioactive glasses with silver or zinc elements have stronger antimicrobial and remineralizing effects compared to conventional orthodontic adhesives and the demineralization process after the pH cycling occurs at 200 to 300 μm away from orthodontic brackets [81].
The most important enamel damage due to orthodontic treatment occurs in removing the residual orthodontic adhesive after the operation. Slow-speed tungsten carbide is commonly used for this purpose [82]. QMAT3 is a novel bioactive glass. In one study, tungsten carbide bur, QMAT3-air-abrasion, and Bioglass 45S5-air-abrasion were examined in vitro to evaluate enamel damage during the processes of removing residual orthodontic adhesive. The results show that QMAT3 bioactive glass has minimal enamel damage in comparison with Bioglass 45S5 air abrasion and tungsten carbide bur. Therefore, QMAT3 seems to offer a conservative approach for orthodontic adhesive removal [82].
Application in endodontics
Bioactive glasses have also been used in root canal treatments [83, 84]. In dental pulp disorders, various treatment options such as pulpectomy, pulpotomy, and pulp capping are present and the materials that can be used in these treatments will play a very effective role in the prognosis of teeth and the success of the treatment [85]. In a study on rats, a novel bioactive glass was used as a pulp capping material after direct pulp capping. Then, results showed that bioactive glass stimulated the formation of heavy dentin bridges with inflammatory reactions similar to mineral trioxide aggregate (MTA) [86].
When microorganisms reach the pulp cavity, root canal treatment is prescribed in which it is necessary to use a root filler to prevent bacterial leakage as well as create a strong sealing [87, 88]. Gutta-percha in combination with Bioglass 45S5 (Bio-Gutta) can be used as an alternative to conventional gutta-percha in root canal treatments. Bio-Gutta can bond to dentin walls does not require any sealers and is also a biocompatible material [89, 90].
Also, bioactive glass can be used as a disinfectant because it has antimicrobial effects due to increasing the pH of an aqueous environment and calcium levels [91]. Bioglasses can act as topical root disinfectants in endodontics and have no effect on dentin stability [92].
Application in oral and maxillofacial surgery
The application of bioactive glass in maxillofacial surgeries compared to other calcium phosphate compounds such as hydroxyapatite and tricalcium phosphate increases bone formation both qualitatively and quantitatively and more rapidly [93]. Bioglass was approved by the US Food and Drug Administration in 2005 as a bone stimulant [94]. Bioglass has been used as a synthetic bone graft under the commercial names Novabone in orthopedics and Perioglass in maxillofacial surgeries [95, 96]. In vitro research has shown that bioactive glass can cause bone regeneration by having effects on bone stimulation [97].
Various commercial products of bioactive glasses including Bioglass 45S5, Biogran, 70S30C bioactive glass, BonAlive, and StronBone are mainly used in oral and maxillofacial surgeries. Biogran is widely used to treat maxillofacial injuries [98]. A clinical study on about 58 cases showed that Bioglass 45S5 can be used as secondary alveolar bone grafting in patients with clefts lip and palate [99]. These procedures are commonly performed with iliac crest bone harvesting which has harvesting morbidity [99]. So using Bioglass 45S5 as an acceptable alternative to iliac crest bone harvesting can reduce harvesting morbidity and simplifies the surgery procedure [99]. One study was done on Biogran effects on volumetric changes and the new bone microarchitecture in human maxillary sinuses augmentation [100]. In this study, it was demonstrated that the addition of 50% bioactive glass to autogenous bone graft decreased the resorption volume and improved the microarchitecture of the graft [100]. Therefore, when low amounts of bone tissue are available for sinus augmentation this mixture of autogenous bone and Biogran particles seems a promising alternative to the autogenous bone only [101]. The 70S30C bioactive glass with formulations of 70% SiO2 and 30% CaO is effective in bone regeneration and can be used as a scaffold in bone grafting [102]. BonAlive is another type of bioactive glass is used to treat large injuries such as mandibular, orbital floor and, mastoid fractures [103, 104]. StronBone is another bioactive glass containing SrO which is used clinically to reduce bone resorption [105]. Bioactive glass can be used as a scaffold for stem cells, too. Using bioactive glass scaffolds for adipose-derived stem cells in order to treat cranio-maxillofacial hard-tissue defects at anatomically different sites, including frontal sinus, cranial bone, mandible, and nasal septum showed successful integration of the construct to the surrounding skeleton [106].
Application in esthetic and restorative dentistry
Dentin hypersensitivity is characterized by short-term and severe toothache to thermal, chemical, or tactile stimuli. The most accepted theory for the cause of pain due to this dentin hypersensitivity is the hydrodynamic theory in which stimuli cause fluid to move in the dentinal tubules and after that, the mechanoreceptors which are near the pulp, stimulate the nerve endings of Aδ fibers resulting in sharp pain [107, 108]. According to hydrodynamic theory, dentin hypersensitivity pain can be reduced by blocking nerve endings or by sealing dentinal tubules [109, 110]. Bioactive glasses can relieve pain during dentin hypersensitivity by binding to collagen fibers and depositing hydroxyapatite in order to block dentin tubules [111]. PerioGlas tends to block dentin tubules and reduce dentin tenderness pain by bonding tightly to collagen [112].
The tooth preparation for composite restorations leads to forming a smear layer including tooth tissue debris as well as bacteria on the tooth surface. The smear layer can occlude the dentinal tubule, so it should be removed in order to enhance better bonding of the resin components. Acid-etching is performed to remove the smear layer and expose the dentinal tubules for this purpose. However, the acid-etching process activates the matrix metalloproteinases (MMPs) which destroy the collagen network of dentin and can cause microleakage [113,114,115,116]. Bonding systems containing bioactive glass in comparison with bonding systems without bioactive glass can reduce microleakages by remineralizing the mineral-deficient areas and increasing the modulus of elasticity and hardness properties at the dentin interface [117].
Biosilicate is another bioactive glass. In a clinical study, the effectiveness of Biosilicate in the treatment of dentin hypersensitivity was confirmed over a period of 6 months [31]. In fact, the particles of Biosilicate in contact with dentin reacts with the tissue inside the dentinal tubules and lead to dentinal occlusion by hydroxyapatite, thus creating a stronger bond [31]. Another study also showed that the use of suspension of Biosilicate microparticles on dentin increases the bond strength of the adhesive system [118].
The role of complementary ions in increasing the efficiency of bioactive glasses in dentistry
Bioactive glasses have good strength, stiffness, and hardness but like other glasses, they are brittle and cannot be used in load-bearing areas [9]. Adding ions such as strontium, zinc, phosphorus, fluoride, cobalt, and silver can affect the different properties of bioactive glasses. Improving the angiogenesis with the addition of cobalt in bone grafting and increasing antimicrobial properties with the addition of silver have been observed [119, 120]. The addition of fluoride can provide numerous benefits to bioactive glasses and ceramics [121]. Fluoride decreases tooth decay by preventing demineralization of enamel and dentin and also increases remineralization and inhibits bacterial enzymes [122]. Fluoride is able to form fluorapatite (FAP) instead of carbonated hydroxyapatite and fluorapatite is more resistant to acid. Therefore, adding fluoride to bioactive glass can improve oral health [123]. Phosphate can be present as orthophosphate in bioactive glass [124]. Increasing the amount of P2O5 and other cations in fluoride-containing glasses helps to maintain network connections and increase the formation of fluorapatite [54]. This kind of bioactive glass is more desirable for clinical applications in dentistry [54]. The strontium is a bone-seeking agent similar to calcium and it is found naturally in the liver, physiological fluids, muscles, and bones [125]. The strontium-containing bioactive glass increases osteoblast proliferation and decreases osteoclast activity in cell culturing [126]. Zinc can improve the bond between glass and bone [127].
Bioactive glass extraction from marine sponges
Considering the different applications of bioactive glass in different fields of dentistry mentioned in the previous sections, it is important to know how to obtain this material and find natural, abundant, and available sources of it. So far, various methods for extracting bioactive glass have been introduced. The melt quenching technique has been used to prepare bioactive glasses traditionally [128]. In the melt quenching process, high temperature commonly above 1000 °C is needed in order to melt ingredients, and after that rapidly quenched for freezing and fabricating the atomic structure [129]. However, the melt quenching technique provides high mechanical properties but is not able to make porous scaffolds, and also the high temperatures reduce bioactivity of the glasses [129]. Heat treatment techniques can overcome some limitations of melt quenching. For example, it can reduce thermomechanical stresses due to rapid cooling or fabricating porous scaffolds but it reduces bioactivity, too [130]. An alternative technique for bioactive glass synthesis is the sol-gel technique that uses hydrolysis and condensation reactions with low-temperature heat treatments [131]. In this way, it will be possible to produce a wide variety of glass compositions and shapes also having glasses with higher porosity [3]. Since 2006, the foam replica method has been used to produce bioactive glass scaffold that is an affordable, relatively easy, and effective technique for the development of highly porous and interconnected 3D scaffolds [132].
Natural marine sponges by having a high interconnected porous structure, the result of their evolution for 1000 years in water filtration can be used as sacrificial templates in the foam replica method to achieve superior mechanical properties [133]. Marine sponges by having various compounds such as biosilica, polyphosphate, and spongin are considered to be used in tissue engineering and reconstructive medicine [17]. Marine sponges are considered to be the earliest multicellular animals that exist at least since the late Proterozoic [134, 135]. Marine sponges are known as the members of the phylum Porifera, and they live in the oceans for about 580 million years and also more than 15, 000 species of them have been identified so far [136]. The sponges are made of an extracellular matrix containing fibrillar collagen, cells, and skeletal components, and this matrix is surrounded by a single-celled epithelial layer called pinacoderm [17]. Marine sponges have four classes and three of them, which contain more than 90% of the species, produce silica spicules. These spicules are different in the number of axis of symmetry [18]. Marine sponges naturally used biosilica for their spicule formation so that biosilica concentration is high in sponges [137]. Biosilica is enzymatically isolated from silicatein proteins of siliceous sponges [138, 139]. Sponges are the only organisms that can polymerize silica enzymatically and produce large siliceous spicules [140]. In 2021, Dudik et al. succeeded to isolated biosilica from five different Atlantic deep-sea sponges Geodia atlantica, Geodia barretti, Stelletta normani, Axinella infundibuliformis, and Phakellia ventilabrum [141].
In fact, the skeletons of sponges include inorganic spicules which are composed of non-crystalline hydrated amorphous silica (SiO2 / H2O) in the classes of Demospongiae, Homoscleromorpha, and Hexactinellida and calcium carbonate (CaCO3) in the class Calcarea [142,143,144,145]. So far, various sea sponges have been identified around the world, and a list of known species of Persian Gulf sponges is given in Table 3. As shown in Table 3, several species of the class Demospongiae and one species of the class Homoscleromorpha are present in the Persian Gulf. Nowadays, different biomaterials with osteogenic effects are demonstrated but natural-originated biomaterials compared to synthetic biomaterials are the better choice because they are more biocompatible and provide a more appropriate surface for cell attachment and growth [137, 209,210,211].
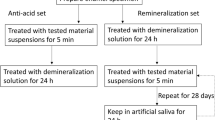
Recently, Kaya et al. [20] extracted natural bioactive glass microspheres from spicules of marine sponge Geodia macandrewii. In the first step of bioactive glass extraction from the sponge, non-silicate minerals in the sponge structure should remove so that the samples are treated with HCl (2 M) aqueous solution at room temperature for 2 hours. Then the samples are washed with distilled water using Whatman filter paper to reach the neutral pH. At this stage, minerals and other similar substances are removed from the sponge samples. In the second step, the samples are placed in NaOH (2 M) aqueous solution in the reflux system at a temperature of 100 °C for 2 hours. After that, the samples are washed again with distilled water to reach a neutral pH. This basic hydrolysis method removes proteins and other similar substances. In the third step, in order to decolorize and depigmentation sponge samples are treated with 10% ethyl alcohol solution for 1 hour at room temperature to remove pigments and then washed with distilled water to reach a neutral pH. This procedure removes any pigments or similar structures that may remain in the resulting samples. After these steps, biosilica fibers and sterraster structures of sponge samples are obtained. The glass beads are placed in hydrofluoric acid solutions (v/v) 20–40% at room temperature for 20 minutes and then washed with distilled water until they reach a neutral pH. Finally, the samples are dried by gradually increasing the temperature from 25 to 100 °C. Exposure to hydrofluoric acid leads to the surface abrasion of the beads and eventually, porous biosilica beads are achieved (Fig. 2) [20]. Porous biosilica beads have been shown to be bioactive, and they form hydroxyapatite when exposed to body fluids [20]. This example clearly demonstrates that it is possible to extract bioactive glass components from marine sponges and sponges can be used as a cheap and rich natural source of bioactive glass.
Conclusions
Since bioactive glasses have a wide range of applications in different fields of dentistry, finding an available and inexpensive resource of bioactive glass is important. Many species of marine sponges have been identified and available in the Persian Gulf which produces various types of compounds. Recent studies have shown that marine sponges can be used to produce bioactive glasses due to the presence of minerals in their structural skeletons, which are made of biosilica. Therefore, marine sponges can be scientifically and economically good choices for extracting bioactive glass. So by finding new methods and sources of bioactive glass it would be possible to enhance their applications in dentistry.
Availability of data and materials
Not applicable.
References
Yelick PC, Sharpe PT. Tooth bioengineering and regenerative dentistry. J Dent Res. 2019;98(11):1173–82.
Sharma S, Srivastava D, Grover S, Sharma V. Biomaterials in tooth tissue engineering: a review. J Clin Diagn Res. 2014;8(1):309–15.
Fernandes HR, Gaddam A, Rebelo A, Brazete D, Stan GE, Ferreira JMF. Bioactive glasses and glass-ceramics for healthcare applications in bone regeneration and tissue engineering. Materials. 2018;11(12):2530.
Baino F, Hamzehlou S, Kargozar S. Bioactive glasses: where are we and where are we going? J Funct Biomater. 2018;9(1):25.
Hench LL. The story of bioglass®. J Mater Sci Mater Med. 2006;17(11):967–78.
Hench LL, Splinter RJ, Allen W, Greenlee T. Bonding mechanisms at the interface of ceramic prosthetic materials. J Biomed Mater Res. 1971;5(6):117–41.
Abbasi Z, Bahrololoom M, Shariat M, Bagheri R. Bioactive glasses in dentistry: A review. J Dent Biomater. 2015;2(1):1–9.
Ali S, Farooq I, Iqbal K. A review of the effect of various ions on the properties and the clinical applications of novel bioactive glasses in medicine and dentistry. Saudi Dent J. 2014;26(1):1–5.
Tabatabaei FS, Torres R, Tayebi L. Biomedical materials in dentistry. In: Tayebi L, editor. Applications of biomedical engineering in dentistry. Switzerland: Springer; 2020. p. 3–20.
Rahaman MN, Day DE, Bal BS, Fu Q, Jung SB, Bonewald LF, et al. Bioactive glass in tissue engineering. Acta Biomater. 2011;7(6):2355–73.
Wan M-c, Qin W, Lei C, Li Q-h, Meng M, Fang M, et al. Biomaterials from the sea: future building blocks for biomedical applications. Bioact Mater. 2021;6(12):4255–85.
Blunt JW, Carroll AR, Copp BR, Davis RA, Keyzers RA, Prinsep MR. Marine natural products. Nat Prod Rep. 2018;35(1):8–53.
Corinaldesi C, Barone G, Marcellini F, Dell'Anno A, Danovaro R. Marine microbial-derived molecules and their potential use in cosmeceutical and cosmetic products. Marine Drugs. 2017;15(4):118.
Barros AA, Aroso IM, Silva TH, Mano JF, Duarte AR, Reis RL. In vitro bioactivity studies of ceramic structures isolated from marine sponges. Biomed Mater. 2016;11(4):045004.
Ruppert EE, Barnes RD, Fox RS. Invertebrate zoology: a functional evolutionary approach. 2nd ed. Sunderland: Sinauer Associates, Inc.; 2004.
Seradj SH, Hashemi SZ, Zomorodian K, Moein MR. Antimicrobial effects of some Persian gulf marine sponges. Iranian South Med J. 2020;23(5):494–504.
Granito RN, Custodio MR, Renno ACM. Natural marine sponges for bone tissue engineering: the state of art and future perspectives. J Biomed Mater Res B Appl Biomater. 2017;105(6):1717–27.
Dudik O, Leonor I, Xavier JR, Rapp HT, Pires RA, Silva TJQLH, et al. Sponge-derived silica for tissue regeneration: bioceramics of deep-sea sponge. Mater Today. 2018;21(5):577–8.
Uriz MJ, Turon X, Becerro MA, Agell G. Siliceous spicules and skeleton frameworks in sponges: origin, diversity, ultrastructural patterns, and biological functions. Microsc Res Tech. 2003;62(4):279–99.
Kaya M, Bilican I, Mujtaba M, Sargin I, Erginer Haskoylu M, Toksoy Oner E, et al. Sponge-derived natural bioactive glass microspheres with self-assembled surface channel arrays opening into a hollow core for bone tissue and controlled drug release applications. Chem Eng J. 2021;407:126667.
Marami Zonouz S, Ardalan Ashja A, Eidi M. Differential identification of five marine sponges in the inter-tidal zone of Hormuz island (Persian gulf) by the microstructure of the spicules. Iranian J Biol Sci. 2017;11(1):45–54.
Abbasi Z, Bahrololoom M, Shariat M, Bagheri R. Bioactive Glasses in Dentistry: A Review. J Dent Biomater. 2015;2(1):1–9.
Vallittu PK. Bioactive glass-containing cranial implants: an overview. J Mater Sci. 2017;52(15):8772–84.
Skallevold HE, Rokaya D, Khurshid Z, Zafar MS. Bioactive glass applications in dentistry. Int J Mol Sci. 2019;20(23):5960.
Odatsu T, Azimaie T, Velten MF, Vu M, Lyles MB, Kim HK, et al. Human periosteum cell osteogenic differentiation enhanced by ionic silicon release from porous amorphous silica fibrous scaffolds. J Biomed Mater Res A. 2015;103(8):2797–806.
Greenspan DC. Developments in biocompatible glass compositions. Med Device Diagn Industry. 1999;21:150–9.
Jones JR, Brauer DS, Hupa L, Greenspan DC. Bioglass and bioactive glasses and their impact on healthcare. Int J Appl Glas Sci. 2016;7(4):423–34.
Kobayashi M, Saito H, Mase T, Sasaki T, Wang W, Tanaka Y, et al. Polarization of hybridized calcium phosphoaluminosilicates with 45S5-type bioglasses. Biomed Mater. 2010;5(2):25001.
Lowe B, Ottensmeyer MP, Xu C, He Y, Ye Q, Troulis MJ. The regenerative applicability of bioactive glass and Beta-Tricalcium phosphate in bone tissue engineering: A transformation perspective. J Funct Biomater. 2019;10(1):16.
Ferreira MM, Brito AF, Brazete D, Pereira IC, Carrilho E, Abrantes AM, et al. Doping beta-TCP as a strategy for enhancing the regenerative potential of composite beta-TCP-alkali-free bioactive glass bone grafts. Exper Stud Rats Mater. 2018;12(1):4.
Tirapelli C, Panzeri H, Lara EH, Soares RG, Peitl O, Zanotto ED. The effect of a novel crystallised bioactive glass-ceramic powder on dentine hypersensitivity: a long-term clinical study. J Oral Rehabil. 2011;38(4):253–62.
Kumar A, Singh S, Thumar G, Mengji A. Bioactive glass nanoparticles (NovaMin®) for applications in dentistry. J Dent Med Sci. 2015;14:30–5.
Tai BJ, Bian Z, Jiang H, Greenspan DC, Zhong J, Clark AE, et al. Anti-gingivitis effect of a dentifrice containing bioactive glass (NovaMin®) particulate. J Clin Periodontol. 2006;33(2):86–91.
Kulal R, Jayanti I, Sambashivaiah S, Bilchodmath S. An in-vitro comparison of nano hydroxyapatite, novamin and proargin desensitizing toothpastes-A SEM study. J Clin Diagn Res. 2016;10(10):ZC51.
Wang Z, Sa Y, Sauro S, Chen H, Xing W, Ma X, et al. Effect of desensitising toothpastes on dentinal tubule occlusion: a dentine permeability measurement and SEM in vitro study. J Dent. 2010;38(5):400–10.
West N, Macdonald E, Jones S, Claydon N, Hughes N, Jeffery P. Randomized in situ clinical study comparing the ability of two new desensitizing toothpaste technologies to occlude patent dentin tubules. J Clin Dentistry. 2011;22(3):82–9.
Rajesh K, Hedge S, Kumar MA, Shetty DG. Evaluation of the efficacy of a 5% calcium sodium phosphosilicate (Novamin®) containing dentifrice for the relief of dentinal hypersensitivity: a clinical study. Indian J Dent Res. 2012;23(3):363.
Mohapatra S, Kumar RP, Arumugham IM, Sakthi D, Jayashri P. Assessment of microhardness of enamel carious like lesions after treatment with Nova min, bio min and Remin pro containing toothpastes: an in vitro study. Indian J Public Health Res Dev. 2019;10:10.
Alhussain AM, Alhaddad AA, Ghazwi MM, Farooq I. Remineralization of artificial carious lesions using a novel fluoride incorporated bioactive glass dentifrice. Dent Med Problems. 2018;55(4):379–82.
Khan AS, Farooq I, Alakrawi KM, Khalid H, Saadi OW, Hakeem AS. Dentin tubule occlusion potential of novel dentifrices having fluoride containing bioactive glass and zinc oxide nanoparticles. Med Princ Pract. 2020;29(4):338–46.
Patel VR, Shettar L, Thakur S, Gillam D, Kamala DN. A randomised clinical trial on the efficacy of 5% fluorocalcium phosphosilicate-containing novel bioactive glass toothpaste. J Oral Rehabil. 2019;46(12):1121–6.
Gupta V, Bains VK, Singh G, Jhingran R. Clinical and cone beam computed tomography comparison of NovaBone dental putty and PerioGlas in the treatment of mandibular class II furcations. Indian J Dent Res. 2014;25(2):166.
Chacko NL, Abraham S, Rao HS, Sridhar N, Moon N, Barde DH. A clinical and radiographic evaluation of periodontal regenerative potential of PerioGlas®: a synthetic, resorbable material in treating periodontal infrabony defects. J Int Oral Health. 2014;6(3):20.
Wadhawan A, Gowda TM, Mehta DS. Gore-tex(®) versus resolut adapt(®) GTR membranes with perioglas(®) in periodontal regeneration. Contemp Clin Dent. 2012;3(4):406–11.
Kontonasaki E, Zorba T, Papadopoulou L, Pavlidou E, Chatzistavrou X, Paraskevopoulos K, et al. Hydroxy carbonate apatite formation on particulate bioglass in vitro as a function of time. Crystal Res Technol. 2002;37(11):1165–71.
Lee HW. Effect of various residual adhesive removal methods on enamel surface after bracket debonding: a systematic Review; 2018.
Taha AA, Fleming PS, Hill RG, Patel MP. Enamel Remineralization with novel bioactive glass air abrasion. J Dent Res. 2018;97(13):1438–44.
Hench LL. Chronology of bioactive glass development and clinical applications; 2013.
Kaur G, Kumar V, Baino F, Mauro JC, Pickrell G, Evans I, et al. Mechanical properties of bioactive glasses, ceramics, glass-ceramics and composites: state-of-the-art review and future challenges. Mater Sci Eng C. 2019;104:109895.
Farooq I, Imran Z, Farooq U, Leghari A, Ali H. Bioactive glass: a material for the future. World J Dent. 2012;3(2):199–201.
Gjorgievska E, Nicholson JW. Prevention of enamel demineralization after tooth bleaching by bioactive glass incorporated into toothpaste. Aust Dent J. 2011;56(2):193–200.
Burwell AK, Litkowski LJ, Greenspan DC. Calcium sodium phosphosilicate (NovaMin): remineralization potential. Adv Dent Res. 2009;21(1):35–9.
Burwell A, Jennings D, Muscle D, Greenspan DC. NovaMin and dentin hypersensitivity--in vitro evidence of efficacy. J Clin Dent. 2010;21(3):66–71.
Brauer DS, Karpukhina N, O'Donnell MD, Law RV, Hill RG. Fluoride-containing bioactive glasses: effect of glass design and structure on degradation, pH and apatite formation in simulated body fluid. Acta Biomater. 2010;6(8):3275–82.
First ever fluoride-containing bioglass toothpaste wins FDA approval. Br Dent J. 2021;230(3):179. https://www.nature.com/articles/s41415-021-2714-8#rightslink.
Romandini M, Baima G, Antonoglou G, Bueno J, Figuero E, Sanz M. Periodontitis, Edentulism, and risk of mortality: A systematic review with Meta-analyses. J Dent Res. 2020;100(1):37–49.
Hirschfeld L, Wasserman B. A long-term survey of tooth loss in 600 treated periodontal patients. J Periodontol. 1978;49(5):225–37.
Renvert S, Persson GR. Periodontitis as a potential risk factor for peri-implantitis. J Clin Periodontol. 2009;36(Suppl 10):9–14.
Reynolds MA, Aichelmann-Reidy ME, Branch-Mays GL, Gunsolley JC. The efficacy of bone replacement grafts in the treatment of periodontal osseous defects. A systematic review. Ann Periodontol. 2003;8(1):227–65.
Felipe ME, Andrade PF, Novaes AB Jr, Grisi MF, Souza SL, Taba M Jr, et al. Potential of bioactive glass particles of different size ranges to affect bone formation in interproximal periodontal defects in dogs. J Periodontol. 2009;80(5):808–15.
Lovelace TB, Mellonig JT, Meffert RM, Jones AA, Nummikoski PV, Cochran DL. Clinical evaluation of bioactive glass in the treatment of periodontal osseous defects in humans. J Periodontol. 1998;69(9):1027–35.
Singh M, Mehta D. Clinical evaluation of Biogran as a graft material in the treatment of periodontal osseous defects. J Indian Soc Periodontol. 2000;3:69–72.
Profeta AC, Huppa C. Bioactive-glass in Oral and maxillofacial surgery. Craniomaxillofac Trauma Reconstr. 2016;9(1):1–14.
Profeta AC, Prucher GM. Bioactive-glass in periodontal surgery and implant dentistry. Dent Mater J. 2015;34(5):559–71.
Gatti AM, Simonetti LA, Monari E, Guidi S, Greenspan D. Bone augmentation with bioactive glass in three cases of dental implant placement. J Biomater Appl. 2006;20(4):325–39.
Yadav VS, Narula SC, Sharma RK, Tewari S, Yadav R. Clinical evaluation of guided tissue regeneration combined with autogenous bone or autogenous bone mixed with bioactive glass in intrabony defects. J Oral Sci. 2011;53(4):481–8.
Subbaiah R, Thomas B. Efficacy of a bioactive alloplast, in the treatment of human periodontal osseous defects-a clinical study; 2011.
Al-Harbi N, Mohammed H, Al-Hadeethi Y, Bakry AS, Umar A, Hussein MA, et al. Silica-based bioactive glasses and their applications in hard tissue regeneration: A review. Pharmaceuticals (Basel, Switzerland). 2021;14(2):75.
Zafar MS, Farooq I, Awais M, Najeeb S, Khurshid Z, Zohaib S. Bioactive surface coatings for enhancing osseointegration of dental implants. In: Kaur G, editor. Biomedical, therapeutic and clinical applications of bioactive glasses: Elsevier; 2019. p. 313–29.
Koller G, Cook RJ, Thompson ID, Watson TF, Di Silvio L. Surface modification of titanium implants using bioactive glasses with air abrasion technologies. J Mater Sci Mater Med. 2007;18(12):2291–6.
López-Píriz R, Solá-Linares E, Rodriguez-Portugal M, Malpica B, Díaz-Güemes I, Enciso S, et al. Evaluation in a dog model of three antimicrobial glassy coatings: prevention of bone loss around implants and microbial assessments. PLoS One. 2015;10(10):e0140374.
Talreja PS, Gayathri G, Mehta D. Treatment of an early failing implant by guided bone regeneration using resorbable collagen membrane and bioactive glass. J Indian Soc Periodontol. 2013;17(1):131.
Civantos A, Martinez-Campos E, Ramos V, Elvira C, Gallardo A, Abarrategi A. Titanium coatings and surface modifications: toward clinically useful bioactive implants. ACS Biomater Sci Eng. 2017;3(7):1245–61.
Mistry S, Kundu D, Datta S, Basu D. Comparison of bioactive glass coated and hydroxyapatite coated titanium dental implants in the human jaw bone. Aust Dent J. 2011;56(1):68–75.
Moritz N, Rossi S, Vedel E, Tirri T, Ylänen H, Aro H, et al. Implants coated with bioactive glass by CO 2-laser, an in vivo study. J Mater Sci Mater Med. 2004;15(7):795–802.
Wheeler D, Montfort M, McLoughlin S. Differential healing response of bone adjacent to porous implants coated with hydroxyapatite and 45S5 bioactive glass. J Biomed Mater Res. 2001;55(4):603–12.
Gange P. The evolution of bonding in orthodontics. Am J Orthod Dentofac Orthop. 2015;147(4):S56–63.
Berlin-Broner Y, Levin L, Ashkenazi M. Awareness of orthodontists regarding oral hygiene performance during active orthodontic treatment. Eur J Paediatr Dent. 2012;13(3):187–91.
Milly H, Festy F, Watson TF, Thompson I, Banerjee A. Enamel white spot lesions can remineralise using bio-active glass and polyacrylic acid-modified bio-active glass powders. J Dent. 2014;42(2):158–66.
Taha AA, Patel MP, Hill RG, Fleming PS. The effect of bioactive glasses on enamel remineralization: A systematic review. J Dent. 2017;67:9–17.
Kim YM, Kim DH, Song CW, Yoon SY, Kim SY, Na HS, et al. Antibacterial and remineralization effects of orthodontic bonding agents containing bioactive glass. Korean J Orthod. 2018;48(3):163–71.
Taha AA, Hill RG, Fleming PS, Patel MP. Development of a novel bioactive glass for air-abrasion to selectively remove orthodontic adhesives. Clin Oral Investig. 2018;22(4):1839–49.
Gholami S, Labbaf S, Houreh AB, Ting H-K, Jones JR, Esfahani M-HN. Long term effects of bioactive glass particulates on dental pulp stem cells in vitro. Biomed Glasses. 2017;3(1):96–103.
Macwan C, Deshpande A. Mineral trioxide aggregate (MTA) in dentistry: A review of literature. J Oral Res Rev. 2014;6(2):71.
Hilton TJ. Keys to clinical success with pulp capping: a review of the literature. Oper Dent. 2009;34(5):615–25.
Long Y, Liu S, Zhu L, Liang Q, Chen X, Dong Y. Evaluation of pulp response to novel bioactive glass pulp capping materials. J Endod. 2017;43(10):1647–50.
Mandke L. Importance of coronal seal: preventing coronal leakage in endodontics. J Restorative Dentistry. 2016;4(3):71.
Tay FR, Pashley DH. Monoblocks in root canals: a hypothetical or a tangible goal. J Endod. 2007;33(4):391–8.
Belladonna FG, Calasans-Maia MD, Novellino Alves AT, de Brito Resende RF, Souza EM, Silva EJ, et al. Biocompatibility of a self-adhesive gutta-percha-based material in subcutaneous tissue of mice. J Endod. 2014;40(11):1869–73.
Mehrvarzfar P, Dahi-Taleghani A, Saghiri MA, Karamifar K, Shababi B, Behnia A. The comparison of MTA, Geristore(R) and amalgam with or without bioglass as a matrix in sealing the furcal perforations (in vitro study). Saudi Dent J. 2010;22(3):119–24.
Allan I, Newman H, Wilson M. Antibacterial activity of particulate bioglass® against supra-and subgingival bacteria. Biomaterials. 2001;22(12):1683–7.
Doyon GE, Dumsha T, von Fraunhofer JA. Fracture resistance of human root dentin exposed to intracanal calcium hydroxide. J Endod. 2005;31(12):895–7.
Peltola MJ, Aitasalo KM, Suonpaa JT, Yli-Urpo A, Laippala PJ, Forsback AP. Frontal sinus and skull bone defect obliteration with three synthetic bioactive materials. A comparative study. J Biomed Mater Res B Appl Biomater. 2003;66(1):364–72.
Hench LL. Bioceramics, a clinical success. Am Ceram Soc Bull. 1998;77(7):67–74.
Fetner A, Hartigan M, Low S. Periodontal repair using PerioGlas in nonhuman primates: clinical and histologic observations. Compendium. 1994;15(7):935–8.
Elshahat A. Correction of craniofacial skeleton contour defects using bioactive glass particles. Egypt J Plast Reconstr Surg. 2006;30(2):113–9.
Hench LL. Chronology of bioactive glass development and clinical applications. New J Glass Ceramics. 2013;3(2):67–73.
Tadjoedin ES, de Lange GL, Lyaruu DM, Kuiper L, Burger EH. High concentrations of bioactive glass material (BioGran) vs. autogenous bone for sinus floor elevation. Clin Oral Implants Res. 2002;13(4):428–36.
Graillon N, Degardin N, Foletti JM, Seiler M, Alessandrini M, Gallucci A. Bioactive glass 45S5 ceramic for alveolar cleft reconstruction, about 58 cases. J Cranio-Maxillofac Surg. 2018;46(10):1772–6.
Pereira R, Menezes J, Bonardi J, Griza G, Okamoto R, Hochuli-Vieira E. Comparative study of volumetric changes and trabecular microarchitecture in human maxillary sinus bone augmentation with bioactive glass and autogenous bone graft: a prospective and randomized assessment. Int J Oral Maxillofac Surg. 2018;47(5):665–71.
Tadjoedin ES, De Lange GL, Holzmann PJ, Kuiper L, Burger EH. Histological observations on biopsies harvested following sinus floor elevation using a bioactive glass material of narrow size range. Clin Oral Implants Res. 2000;11(4):334–44.
Midha S, Kim TB, van den Bergh W, Lee PD, Jones JR, Mitchell CA. Preconditioned 70S30C bioactive glass foams promote osteogenesis in vivo. Acta Biomater. 2013;9(11):9169–82.
Gosain AK. Plastic surgery Educational Foundation DC. Bioactive glass for bone replacement in craniomaxillofacial reconstruction. Plast Reconstr Surg. 2004;114(2):590–3.
Peltola M, Aitasalo K, Suonpaa J, Varpula M, Yli-Urpo A. Bioactive glass S53P4 in frontal sinus obliteration: a long-term clinical experience. Head Neck. 2006;28(9):834–41.
Fujikura K, Karpukhina N, Kasuga T, Brauer D, Hill R, Law R. Influence of strontium substitution on structure and crystallisation of bioglass® 45S5. J Mater Chem. 2012;22(15):7395–402.
Sándor GK, Numminen J, Wolff J, Thesleff T, Miettinen A, Tuovinen VJ, et al. Adipose stem cells used to reconstruct 13 cases with cranio-maxillofacial hard-tissue defects. Stem Cells Transl Med. 2014;3(4):530–40.
Brannstrom M, Astrom A. The hydrodynamics of the dentine; its possible relationship to dentinal pain. Int Dent J. 1972;22(2):219–27.
West NX, Lussi A, Seong J, Hellwig E. Dentin hypersensitivity: pain mechanisms and aetiology of exposed cervical dentin. Clin Oral Investig. 2013;17(Suppl 1):S9–19.
Absi EG, Addy M, Adams D, Dentine hypersensitivity. A study of the patency of dentinal tubules in sensitive and non-sensitive cervical dentine. J Clin Periodontol. 1987;14(5):280–4.
Orchardson R, Gillam DG. The efficacy of potassium salts as agents for treating dentin hypersensitivity. J Orofac Pain. 2000;14(1):9–19.
Gillam DG. Clinical trial designs for testing of products for dentine hypersensitivity--a review. J West Soc Periodontol Periodontal Abstr. 1997;45(2):37–46.
Montazerian M, Zanotto ED. A guided walk through Larry Hench’s monumental discoveries. J Mater Sci. 2017;52(15):8695–732.
Borsatto MC, Corona SA, Dibb RG, Ramos RP, Pecora JD. Microleakage of a resin sealant after acid-etching, Er:YAG laser irradiation and air-abrasion of pits and fissures. J Clin Laser Med Surg. 2001;19(2):83–7.
Hashimoto M, Tay FR, Ohno H, Sano H, Kaga M, Yiu C, et al. SEM and TEM analysis of water degradation of human dentinal collagen. J Biomed Mater Res B Appl Biomater. 2003;66(1):287–98.
Mazzoni A, Pashley DH, Nishitani Y, Breschi L, Mannello F, Tjaderhane L, et al. Reactivation of inactivated endogenous proteolytic activities in phosphoric acid-etched dentine by etch-and-rinse adhesives. Biomaterials. 2006;27(25):4470–6.
Tay FR, Pashley DH, Yiu C, Cheong C, Hashimoto M, Itou K, et al. Nanoleakage types and potential implications: evidence from unfilled and filled adhesives with the same resin composition. Am J Dent. 2004;17(3):182–90.
Sauro S, Osorio R, Watson TF, Toledano M. Therapeutic effects of novel resin bonding systems containing bioactive glasses on mineral-depleted areas within the bonded-dentine interface. J Mater Sci Mater Med. 2012;23(6):1521–32.
de Morais RC, Silveira RE, Chinelatti MA, Pires-de-Souza FCP. Biosilicate as a dentin pretreatment for total-etch and self-etch adhesives: in vitro study. Int J Adhes Adhes. 2016;70:271–6.
Hoppe A, Jokic B, Janackovic D, Fey T, Greil P, Romeis S, et al. Cobalt-releasing 1393 bioactive glass-derived scaffolds for bone tissue engineering applications. ACS Appl Mater Interfaces. 2014;6(4):2865–77.
Rokaya D, Srimaneepong V, Sapkota J, Qin J, Siraleartmukul K, Siriwongrungson V. Polymeric materials and films in dentistry: an overview. J Adv Res. 2018;14:25–34.
Hench L, Spilman D, Hench J. Inventors; University of Florida, assignee. Fluoride-modified bioactive glass (Bioglass) and its use as implant material US patent; 1988. p. 4775646.
Thuy TT, Nakagaki H, Kato K, Hung PA, Inukai J, Tsuboi S, et al. Effect of strontium in combination with fluoride on enamel remineralisation in vitro. Arch Oral Biol. 2008;53(11):1017–22.
Brauer DS, Karpukhina N, Law RV, Hill RG. Structure of fluoride-containing bioactive glasses. J Mater Chem. 2009;19(31):5629–36.
Elgayar I, Aliev A, Boccaccini A, Hill R. Structural analysis of bioactive glasses. J Non-Cryst Solids. 2005;351(2):173–83.
D'Haese PC, Van Landeghem GF, Lamberts LV, Bekaert VA, Schrooten I, De Broe ME. Measurement of strontium in serum, urine, bone, and soft tissues by Zeeman atomic absorption spectrometry. Clin Chem. 1997;43(1):121–8.
Gentleman E, Fredholm YC, Jell G, Lotfibakhshaiesh N, O'Donnell MD, Hill RG, et al. The effects of strontium-substituted bioactive glasses on osteoblasts and osteoclasts in vitro. Biomaterials. 2010;31(14):3949–56.
Aina V, Perardi A, Bergandi L, Malavasi G, Menabue L, Morterra C, et al. Cytotoxicity of zinc-containing bioactive glasses in contact with human osteoblasts. Chem Biol Interact. 2007;167(3):207–18.
Chen Q, Xu JL, Yu L, Fang X-Y, Khor KA. Spark plasma sintering of sol–gel derived 45S5 bioglass®-ceramics: mechanical properties and biocompatibility evaluation. Mater Sci Eng C. 2012;32(3):494–502.
Peitl Filho O, LaTorre GP, Hench LL. Effect of crystallization on apatite-layer formation of bioactive glass 45S5. J Biomed Mater Res. 1996;30(4):509–14.
Prasad S, Vyas VK, Ershad M, Pyare R. Crystallization and mechanical properties of (45S5-HA) biocomposite for biomedical implantation; 2017.
Wu C, Fan W, Gelinsky M, Xiao Y, Simon P, Schulze R, et al. Bioactive SrO-SiO2 glass with well-ordered mesopores: characterization, physiochemistry and biological properties. Acta Biomater. 2011;7(4):1797–806.
Fiume E, Ciavattini S, Verné E, Baino F. Foam replica method in the manufacturing of bioactive glass scaffolds: out-of-date technology or still underexploited potential? Materials. 2021;14(11):2795.
Boccardi E. Natural marine derived bioactive glass based scaffolds with improved functionalities: Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU); 2017.
Xiao S, Yuan X, Knoll AH. Eumetazoan fossils in terminal proterozoic phosphorites? Proc Natl Acad Sci U S A. 2000;97(25):13684–9.
Rosenberg E, Sharon G, Atad I, Zilber-Rosenberg I. The evolution of animals and plants via symbiosis with microorganisms. Environ Microbiol Rep. 2010;2(4):500–6.
Loori M, Sourinejad I, Nazemi M. Identification and investigation of antibacterial effects of steroidal fraction from the marine sponge Axinella sinoxea Alvarez & Hooper, 2009 in Larak island, the Persian Gulf. J Fish Sci Technol. 2021;10(2):164–72.
Wang X, Schröder HC, Grebenjuk V, Diehl-Seifert B, Mailänder V, Steffen R, et al. The marine sponge-derived inorganic polymers, biosilica and polyphosphate, as Morphogenetically active matrices/scaffolds for the differentiation of human multipotent stromal cells: potential application in 3D printing and distraction Osteogenesis. Marine Drugs. 2014;12:2.
Schroder HC, Wang X, Tremel W, Ushijima H, Muller WE. Biofabrication of biosilica-glass by living organisms. Nat Prod Rep. 2008;25(3):455–74.
Schroder HC, Perovic-Ottstadt S, Grebenjuk VA, Engel S, Muller IM, Muller WE. Biosilica formation in spicules of the sponge Suberites domuncula: synchronous expression of a gene cluster. Genomics. 2005;85(6):666–78.
Müller WE, Wang X, Cui F-Z, Jochum KP, Tremel W, Bill J, et al. Sponge spicules as blueprints for the biofabrication of inorganic–organic composites and biomaterials. Appl Microbiol Biotechnol. 2009;83(3):397–413.
Dudik O, et al. Bioactivity of biosilica obtained from North Atlantic deep-sea sponges. Front Marine Sci. 2021;8:637810.
Hooper JN, van Soest RW. Systema Porifera: a guide to the classification of sponges. New York: Kluwer Academic / Plenum; 2002.
Leys SP, Nichols SA, Adams ED. Epithelia and integration in sponges. Integr Comp Biol. 2009;49(2):167–77.
Muller WE. Silicon biomineralization: biology - biochemistry - molecular biology - biotechnology. Germany: Springer Science & Business Media; 2003.
Müller WE, Müller IM. In: Custódio MR, Lôbo-Hajdu G, Hajdu E, Muricy G, editors. Porifera: an enigmatic taxon disclosed by molecular biology/cell biology. Rio de Janeiro: Museu Nacional, Rio de Janeiro; 2007. p. 89–106.
Kornprobst J-M. Sponges in Qatari waters A new source of marine natural products for biological applications. Qatar Univ Sci J. 1999;19:5–23.
Sadeghi P, Savari A, Yavari V, Devin ML. First record of sponge distribution in the Persian Gulf, (Hengam Island, Iran). Pak J Biol Sci. 2008;11(21):2521–4.
Maghsoudlou A, Shokri MR, Momtazi F. Taxonomy and biogeography of the Persian Gulf subtidal sponges: an estimate of α and β diversity. Oceanography. 2014;5:10–9.
Genin E, Wielgosz-Collin G, Njinkoue JM, Velosaotsy NE, Kornprobst JM, Gouygou JP, et al. New trends in phospholipid class composition of marine sponges. Comp Biochem Physiol B Biochem Mol Biol. 2008;150(4):427–31.
Njinkoue J, Barnathan G, Al-Muftah A, Al-Aeasa H, Vacelet J, Kornprobst J. Phospholipid fatty acid composition of nine marine sponges from Qatar. Marine lipids Proceedings of the symposium held in Brest, France, 19–20 November 1998; 2000: IFREMER.
Derakhshesh N, Savari A, Dostahenas B, Dehghan Madise S, Doraghi A. Comparison productivity of class Desmospongiae (phylum Porifera) on artificial reefs (ARs) in northwest Persian gulf. J Anim Environ. 2015;7(3):165–74.
Khoshkhoo Z. Identification and distribution of sponges from Larak Island in Persian gulf. J Anim Environ. 2017;9(4):363–70.
Hassanzadeh Y, Bahador N, Baseri SM. Isolation and identification of symbiotic vibrio alginolyticus from Persian gulf sponges with API 20NE kit. J Marine Biol. 2014;6(3):61–8.
Khoshkhoo Z, Nazemi M, Motalebi A, Mahdabi M, Ardalan AA, Hemati MR. First record of siliceous and calcareous sponges from Larak Island, Persian Gulf–Iran. Middle-East J Sci Res. 2012;11(7):887–93.
Eisapor S, Safaeian SH. Identification of sponges of inter tidal zone in north of Hengam. Int J Marine Sci Environ. 2013;3(3):141–8.
Ghafourian H, Khodadad Hosseini E, Rabbani M. A novel GH-92 Nano-adsorbent using the sponge from the Persian Gulf for Lead and cadmium removal. J Water Wastewater; Ab va Fazilab ( in persian ). 2015;26(2):2–12.
Hosseini EK, Ghafourian H, Rabbani M. Selective separation of Lead ions using new Nano-adsorbent GH-92. Int J Computat Theoret Chem. 2018;6(1):14.
Golfakhrabadi F, Khaledi M, Nazemi M, Safdarian M. Isolation, identification, and HPTLC quantification of dehydrodeoxycholic acid from Persian gulf sponges. J Pharm Biomed Anal. 2021;197:113962.
Gozari M, tamadoni jahromi S, pourmozaffar S, Behzadi S. Selective isolation of the Persian Gulf sponge-associated Actinobacteria and evaluation of cytotoxic and antioxidant activity of their metabolites. J Oceanogr. 2020;11(41):39–48.
Heidary Jamebozorgi F, Yousefzadi M, Firuzi O, Nazemi M, Jassbi AR. In vitro anti-proliferative activities of the sterols and fatty acids isolated from the Persian Gulf sponge; Axinella sinoxea. Daru. 2019;27(1):121–35.
Heidary Jamebozorgi F, Yousefzadi M, Firuzi OR, Nazemi M, Jassbi AR. Cytotoxic activity of hexane and dichloromethane parts of methanol extract of Ircinia mutans sponge on three human cancer cell lines. Iranian Sci Fisheries J. 2018;27(2):105–14.
Mahdian D, Iranshahy M, Shakeri A, Hoseini A, Yavari H, Nazemi M, et al. Cytotoxicity evaluation of extracts and fractions of five marine sponges from the Persian Gulf and HPLC fingerprint analysis of cytotoxic extracts. Asian Pac J Trop Biomed. 2015;5(11):896–901.
Mohsenian Kouchaksaraee R, Moridi Farimani M, Li F, Nazemi M, Tasdemir D. Integrating molecular networking and (1) H NMR spectroscopy for isolation of bioactive metabolites from the Persian Gulf sponge Axinella sinoxea. Mar Drugs. 2020;18(7):366.
Nazemi M. Review of the cytotoxic activity (anticancer) of marine sponges. Utilization Cultivation Aqua. 2016;5(4):71–80.
Nazemi M, Pishehvarzad F, Motallebi A, Ahmadzadeh O. Investigation of antibacterial activities of sponge Axinella sinoxea’s extracts from Larak Island. Persian Gulf J Aqua Ecol. 2012;1(4):65–54.
Pourahmad J, Salimi A, Saharkhiz M, Motallebi A, Seydi E, Mohseni A, et al. Standardized extract of the Persian Gulf sponge, Axinella Sinoxea selectively induces apoptosis through mitochondria in human chronic lymphocytic leukemia cells. J Analytic Oncol. 2015;4(4):132–40.
Seradj H, Moein M, Eskandari M, Maaref F. Antioxidant activity of six marine sponges collected from the Persian Gulf. Iranian J Pharm Sci. 2012;8(4):249–55.
Erpenbeck D, Gholami A, Hesni MA, Ranjbar MS, Galitz A, Eickhoff B, et al. Molecular biodiversity of Iranian shallow water sponges. Syst Biodivers. 2020;18(2):192–202.
Eisapor SS, Safaeian S, Esmaeili A, Vakili Amini H, Bavandi R. Identification of sponges of off shore zone in north-West of Hengam Island, Persian gulf. J Marine Sci Technol Res. 2012;6(4):80–91.
Hamayeli H, Hassanshahian M, Mohammadi M. The anti-biofilm effects of sponge (Callyspongia sp.) and two sea anemones (Zoanthus sansibaricus and Cerianthus lloydii) collected from the Persian Gulf. J Kerman Univ Med Sci. 2018;25(6):493–504.
Giraldes BW, Goodwin C, Al-Fardi NAA, Engmann A, Leitao A, Ahmed AA, et al. Two new sponge species (Demospongiae: Chalinidae and Suberitidae) isolated from hyperarid mangroves of Qatar with notes on their potential antibacterial bioactivity. PLoS One. 2020;15(5):e0232205.
Gutekunst V, AU MÜ, Pohl T, BrÜmmer F, Malik H, Fawzi N, et al. A new fistulose demosponge species from the Persian Gulf. Zootaxa. 2018;4450(5):565–74.
Najafi A, Moradinasab M, Nabipour I. First record of microbiomes of sponges collected from the Persian Gulf, using tag pyrosequencing. Front Microbiol. 2018;9(1500):1500.
Alidoost Salimi M, Ghavam Mostafavi P, Aeby G, Fatemi SMR. The presence of Clathria sp. on living coral colonies in Kish Island, Persian gulf. J Anim Environ. 2019;11(4):377–80.
Nazemi, M, et al. First record on the distribution and abundance of three sponge species from Hormoz island, Persian Gulf-Iran. Biol Forum. Res Trend. 2015;72.
Jafari MA, Seyfabadi J, Shokri MR. Internal bioerosion in dead and live hard corals in intertidal zone of Hormuz Island (Persian gulf). Mar Pollut Bull. 2016;105(2):586–92.
Futterer DK. Significance of the boring sponge Cliona for the origin of fine grained material of carbonate sediments. J Sediment Res. 1974;44(1):79–84.
Ilkhani M, Nejat Khah Manavi P, Sadat Sadeghi M, Rabani M. Identification species of Demospongiae sponge at Assaluyeh Persian gulf. Mar Biol. 2020;12(4):1–10.
Ebadi K, Sanati AM. Biodegrading crude oil from the native sponges of the Persian Gulf Dictyonella sp. J Oceanogr. 2016;7(27):59–68.
Khakshoor MS, Pazooki J. Bactericidal and fungicidal activities of different crude extracts of Gelliodes carnosa (sponge, Persian gulf). Iran J Fish Sci. 2014;13(3):776–84.
Pazooki J, Khakshoor MS. Evaluation of the anti-microbial properties of Gelliodes carnosa sponge alkaloid compounds antimicrobial properties of marine sponge. Int J Aqua Sci. 2015;6(1):84–95.
Safaeian S, Hosseini H, Abbas Pour Asadolah A, Farmohamadi S. Antimicrobial activity of marine sponge extracts of offshore zone from nay Band Bay. Iran J de Mycol Méd. 2009;19(1):11–6.
Kazempoor S, Ashja Ardalan A, Eidi M. Identification of sponges in tidal zone of Hormoz Island, Persian Gulf. J Anim Environ. 2017;9(1):189–94.
Nazemi M, Alidoust Salimi M, Alidoust Salimi P, Motallebi A, Tamadoni Jahromi S, Ahmadzadeh O. Antifungal and antibacterial activity of Haliclona sp. from the Persian Gulf, Iran. J Mycol Med. 2014;24(3):220–4.
Derakhshesh N, Savari A, Dostahenas B, Dehghan Madise S, Doraghi A. Biomass and production of the marine sponge family: haliclonidae (Haliclona simulans and Haliclona oculata) on artificial reefs in northwest of the Persian Gulf. J Oceanogr. 2013;4(14):77–84.
Seydi E, Motallebi A, Dastbaz M, Dehghan S, Salimi A, Nazemi M, et al. Selective toxicity of Persian Gulf Sea cucumber (Holothuria parva) and sponge (Haliclona oculata) Methanolic extracts on liver mitochondria isolated from an animal model of hepatocellular carcinoma. Hepat Mon. 2015;15(12):e33073.
Salamat N, Derakhshesh N. Histological study of two sponge species with and without spicules in class Demospongiae. Aqua Physiol Biotechnol. 2014;1(2):55–70.
Zarei M, Jahedi M. Determination of antifungal activity of staphylococcus haemolyticus and Bacillus sp. isolated from native sponge of Persian gulf. J Anim Environ. 2018;10(4):559–66.
Karimpoor M, Kamrani E, Yousefzadi M, Nazemi M. Antibacterial and antioxidant potential of Haliclona caerulea extracts from Tidal Island Larak, Persian Gulf. Modares J Biotechnol. 2018;9(3):347–53.
Norouzi E, Bahramifar N, Abolmaali S, Esmaeli sari A, Alizadeh A. Bioaccumulation of copper, iron and zinc in marine sponges Haliclona sp. in Qeshm and lark islands. J Environ Sci Technol. 2017;19(5):497–506.
Shushizadeh MR, Behroozi S, Behfar A-A, Nazemi M. Antibacterial activity and Gc-mass analysis of organic extract from Persian gulf Haliclona SP. Pharmacophore. 2018;9(2):19–24.
Nazemi M, Khoshkhoo Z, Motalebi A, Firozjaee HK. Identification nonpolar component andantibacterial activities of Iophon laevistylusfrom Persian gulf. Int J Environ Sci Dev. 2010;1(2):107.
Nazemi M, Moradi Y, Rezvani Gilkolai F, Ahmaditaba MA, Gozari M, Salari Z. Antimicrobial activities of semi polar-nonpolar and polar secondary metabolites of sponge Dysidea pallescens from Hengam Island, Persian gulf. Iran J Fish Sci. 2017;16(1):200–9.
Ebadi K, Zarei M, Sanati AM. Isolation and molecular identification of oil degrading bacteria associated with Pachychalina sp sponge. J Mar Sci Technol. 2019;17(4):22–35.
Doroudi MS. Infestation of the pearl oysters by the boring and fouling organisms in the northern coast of Persian gulf. Indian J Med Sci. 1995;25(2):168–9.
Aghvami M, Keshavarz A, Nazemi M, Zarei MH, Pourahmad J. Selective cytotoxicity of α-santonin from the persian gulf sponge Dysidea avara on pediatric ALL B-lymphocytes via mitochondrial targeting. Asian Pac J Cancer Prev. 2018;19(8):2149–54.
Gozari M, Bahador N, Mortazavi MS, Eftekhar E, Jassbi AR. An “olivomycin A” derivative from a sponge-associated Streptomyces sp. strain SP 85. 3. Biotech. 2019;9(12):1–11.
Khaledi M, Sharif Makhmal Zadeh B, Rezaie A, Nazemi M, Safdarian M, Nabavi MB. Chemical profiling and anti-psoriatic activity of marine sponge (Dysidea avara) in induced imiquimod-psoriasis-skin model. PLoS One. 2020;15(11):e0241582.
Nazemi M, Khaledi M, Golshan M, Ghorbani M, Amiran MR, Darvishi A, et al. Cytotoxicity activity and Druggability studies of Sigmasterol isolated from marine sponge Dysidea avara against Oral epithelial Cancer cell (KB/C152) and T-lymphocytic leukemia cell line (Jurkat/ E6-1). Asian Pac J Cancer Prev. 2020;21(4):997–1003.
Nazemi M, Moradi Y, Sadrian M, Lekzaee F. Cytotoxic activity of natural components soluble in methanol and diethyl ether of Dysidea pallescens from Hengam Island, Persian Gulf. Iranian Sci Fisheries J. 2016;24(4):1–8.
Nazemi M, Mohebbi Nozar SL, Seddiq Mortazavi M, Jamili S, Aghasadeghi MR, Ahmaditaba MA, et al. Extraction, identification and biological activities (antibacterial, antifungal and cytotoxic) of terpenoid from sponge Dysidea spp. in Hengam Island, Persian gulf for antibiotic and anticancer drugs. Iranian Fisheries Sci Res Institute. 2018. https://aquadocs.org/handle/1834/14142.
Hamayeli H, Hasanshahian M, Namaki Shoshtari A, Askari HM. Study the antimicrobial effect of three marine sponges (Dysidea sp.) collected at Persian gulf on some pathogenic bacteria in planktonic and biofilm forms. Iranian J Med Microbiol. 2017;11(4):45–56.
Hamayeli H, Hassanshahian M, Askari HM. Identification of bioactive compounds and evaluation of the antimicrobial and anti-biofilm effect of Psammocinia sp. and Hyattella sp. Sponges Persian Gulf Thalassas. 2020;37(1):357–66.
Nazemi M, Motallebi Moghanjoghi AA, Jamili S, Mashinchian A, Ghavam MP. Comparison of antibacterial activities of Ircinia mutans extracts in two different seasons from Kish Island, Persian gulf, Iran. Iranian J Fisheries Sci. 2014;13(4):823–33.
Arast Y, Pourahmad J. Selective toxicity of standardized extracts of persian gulf sponge (Ircinia mutans) on skin cells and mitochondria isolated from melanoma induced mouse. Int Pharm Acta. 2019;2(1):2e5.
Heidary Jamebozorgi F, Yousefzadi M, Firuzi O, Nazemi M, Zare S, Chandran JN, et al. Cytotoxic furanosesquiterpenoids and steroids from Ircinia mutans sponges. Pharm Biol. 2021;59(1):575–83.
Jassbi A. Biological active natural products from marine organisms and terrestrial plants of Iran. Planta Medica. 2016;82(S 01):P548.
Najafi A, Moradinasab M, Seyedabadi M, Haghighi MA, Nabipour I. First molecular identification of symbiotic Archaea in a sponge collected from the Persian Gulf, Iran. Open Microbiol J. 2018;12:323–32.
Matassi F, Nistri L, Chicon Paez D, Innocenti M. New biomaterials for bone regeneration. Clin Cases Miner Bone Metab. 2011;8(1):21–4.
Lin Z, Solomon KL, Zhang X, Pavlos NJ, Abel T, Willers C, et al. In vitro evaluation of natural marine sponge collagen as a scaffold for bone tissue engineering. Int J Biol Sci. 2011;7(7):968–77.
Müller WE, Schröder HC, Schlossmacher U, Neufurth M, Geurtsen W, Korzhev M, et al. The enzyme carbonic anhydrase as an integral component of biogenic ca-carbonate formation in sponge spicules. FEBS Open Bio. 2013;3:357–62.
Acknowledgments
Not applicable.
Funding
This work was supported financially by Bushehr University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
A.T., N.T., and N.J. conceived and designed the format of the manuscript. N.J., M.S.H., A.H., and R.S. drafted and edited the manuscript. A.T., and N.T. reviewed the manuscript. All authors contributed to the critical reading and discussion of the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Author Amin Tamadon was employed by PerciaVista R&D Co. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jafari, N., Habashi, M.S., Hashemi, A. et al. Application of bioactive glasses in various dental fields. Biomater Res 26, 31 (2022). https://doi.org/10.1186/s40824-022-00274-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40824-022-00274-6