Abstract
Background
Chronic neuropathic pain syndrome is associated with impaired quality of life and is poorly manageable. Alpha lipoic acid (ALA) is a powerful antioxidant and showed its effectiveness on diabetic neuropathy and other acute peripheral nerve injuries but it was not evaluated in the chronic neuropathic pain, chronic constriction injury (CCI) in rat model by using duloxetine (DLX) as standard.
Methodology
The main objective of the study was to expedite ALA effect on chronic peripheral neuropathy induced by CCI of sciatic nerve in rats. In this study, male Wister rats were randomly divided into six groups (n = 8) including, normal saline, sham operated, surgery control, DLX 30mg/kg treated, ALA treated 25mg/kg, and ALA+DLX. The CCI of sciatic nerve was conducted on all animals except normal saline group and studied for 21 days (i.e. 14 days treatment period & 7 days treatment free period) by using different behavioral, biochemical and, histopathology studies.
Results
ALA showed minor but significant decrease of thermal hyperalgesia, cold allodynia, malondialdehyde (MDA), total protein, lipid peroxidation, and nitric oxide levels and significant increase of motor coordination, glutathione level and decreased axonal degeneration significantly. These effects sustained even during treatment free period. ALA enhanced the effect of DLX when given in combination by showing sustained effect. In conclusion, ALA acted as potent antioxidant may be this activity is responsible for the potent neuroprotective effect.
Conclusion
Hence, ALA attenuated the nueroinflammation mediated by chronic peripheral neuropathy. Further studies are warranted with ALA to develop as a clinically relevant therapeutic agent for the treatment of neuropathic pain.
Similar content being viewed by others
Introduction
Neuropathic pain is due to the pain caused by lesion and/or disease of the somatosensory neurons [1]. Neuropathic pain is also described by the pain initiated or due to primary lesion occurs in peripheral or central nervous system. WHO explains around 22 % of the world’s primary care patients suffer from chronic neuropathic pain [2] and around 8 % of adults have neuropathic pain characteristics. Many of the patients with diabetes and HIV suffering from neuropathic pain [3]. Neuropathic pain generally characterized by stimulus-independent persistent pain [4, 5] and/or by sensory abnormalities such as abnormal unpleasant sensation (dysesthesia), increased intensity of response to painful stimuli (hyperalgesia) and pain in response to normally painless stimuli (allodynia) [6]. Due to its complex pathophysiology and heterogynous etiology the treatment is difficult and the drugs available to treat neuropathic pain are helpful to less patient population only with low efficacy and numerous side effects [7]. The patients with cancer, leprosy, cervical disc protrusion and foraminotomy generally suffers from neuropathic pain [8] and the major surgeries like thoracotomy and amputation may cause neuropathic pain. The animal models plays important role to explain the mechanisms responsible for the neuropathic pain [9]. The animal models of neuropathic pain describes that the hyperalgesia is related to the inflammatory response and inflammatory mediators are elevated in hyperalgesia in nerve injured rat models [10, 11]. The research studies explain that both peripheral and central mechanism(s) are involved in pathogenesis of neuropathic pain [12, 13]. A novel hypothesis explains that reactive oxygen species (ROS) responsible for central sensitization through unknown mechanisms [14], may be with secondary messenger system activity [15]. Neuropathic pain contributing ROS if reduced after peripheral nerve injury can reduce an intercellular signaling pathway and reduces the neuronal death.
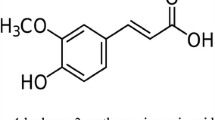
Alpha lipoic acid (ALA) also called thioctic acid, is a powerful antioxidant and metal ion chelator for metals that contained naturally in the body [16]. It was found to be useful in experimental models of various peripheral and central nervous system diseases such as diabetic neuropathy, multiple sclerosis, cerebral ischemia-reperfusion, excitotoxic amino brain cerebral ischemia, autoimmune encephalomyelitis [17]. It is also used in treating pain disorders such as diabetic neuropathy, sciatica and carpel tunnel syndrome in clinical practice [18, 19]. But, still now ALA was not reported to have beneficial effects with Chronic Constriction Injury (CCI) of sciatic nerve in rats. So, this study was designed to evaluate the effect of ALA, at a dose of 25 mg/kg.ip [20] on chronic neuropathic pain produced by CCI of sciatic nerve in rats.
Materials and methods
Animals
Adult male Wistar rats weighing 250–300 g were procured from Jeeva Agencies, Hyderabad. Animals were housed in plastic cages with husk bedding under standard laboratory conditions of light and dark cycles with laboratory diet and water ad libitum. Animals were acclimatized for a week to laboratory conditions before the experiment. This experimental protocol was approved by institutional animal ethical committee (IAEC/20/UCPSc/KU/2019), Kakatiya University, Warangal.
Drugs
ALA was purchased from Sigma Aldrich and Duloxetine was gifted sample from Dr. Reddy’s laboratories (Hyderabad, India). All the other chemicals used in the study were of analytical grade.
Induction of neuropathic pain by chronic constriction injury (CCI) method
According to method previously described the peripheral neuropathy in rats was induced by CCI [21]. In brief, the rats were anesthetized by using ketamine (60 mg/kg) and xylazine (8 mg/kg). The left hind thigh of anesthetized rat was shaved and the skin was sterilized. Then the common sciatic nerve was exposed on middle of the hind thigh by blunt dissection of biceps femoris muscle, proximal to the sciatic trifurcation, approximately 7-mm of nerve was freed of adhering tissue and 4 tight ligatures of 4 − 0 silk suture were tied around the nerve with 1mm spacing. Care was taken not to interrupt the epineural blood flow during tying the ligature. In sham operated rats same procedure was followed, the connective tissue was freed, without ligation of nerve.
Experimental design
Animals were allocated into 6 study groups and each group containing 8 rats were subjected to the following treatment:
Experimental protocol with treatment schedule
-
Group I: Normal Saline (NS) treated; CCI was not performed + rats treated with saline (P.O) for 15 days.
-
Group II: Sham Operated (SO), Rats were subjected to surgical CCI sciatic nerve without ligation and treated with saline (P.O).
-
Group III: Surgery control (SC), Rats were subjected to surgical CCI to expose sciatic nerve with ligations and treated with saline (P.O).
-
Group IV: Duloxetine (DLX) treated; rats were subjected to CCI + treated with DLX (30 mg/kg/p.o, for 14 days) [22].
-
Group V: Alpha Lipoid acid (ALA) treated; rats were subjected to CCI + treated with ALA (25 mg/kg/i.p, for 14 days).
-
Group VI: [DLX + ALA]; rats were subjected to CCI + treated with both drugs [DLX + ALA] for 14 days.
By maintaining aseptic conditions all the groups were subjected for surgery except the control group and the treatment was started after one day of surgery for 14 days and then study followed 7 days of treatment free period. Then different behavioral, biochemical and, histopathology studies were conducted.
Estimation of total protein content in nerve tissue homogenate
The total protein content of tissue homogenate was estimated [23] with slight modifications, using bovine serum albumin as standard. Briefly, to the tissue homogenate (0.2ml), 2ml of alkaline copper sulphate reagent was added and incubated for 10minutes at room temperature. Then 0.2ml of Folin-ciocalteau phenol reagent was added and again incubated for 30m at room temperature. Then the absorbance was read at 660nm against the blank reagent. Total protein content values were expressed in mg/ml.
Estimation of nitric oxide content in nerve tissue homogenate
Nitric oxide content was estimated [24] with some modifications. 0.2ml of tissue homogenate was taken and volume was adjusted to 1.5ml with 100mM Tris-HCl buffer (pH 7.4). To this 1.5ml of Griess reagent was added and incubated for 10m at room temperature and the absorbance was determined by spectrophotometer at 546nm using Systronics spectrophotometer and the values were expressed in µM/ml.
Estimation of reduced glutathione in nerve tissue homogenate
Reduced glutathione was estimated [25] by using glutathione as standard with slight modifications. Tissue homogenate (1ml) was precipitated with 4 % sulfosalicylic acid (1ml) and cold digested at 4℃ for 1hr and cold centrifuged at 1200 x g for 15 min at 4℃ and the supernatant was collected. Then 0.2ml of supernatant extracted from tissue homogenate was taken. To this, 2.3ml of phosphate buffer (0.1 M, pH 7.6) and 0.5ml of DTNB were added and incubated for 5m at room temperature. The absorbance of yellow color produced was measured at 412nm using Systronics spectrophotometer and the values were expressed as mM.
Estimation of lipid peroxidation in tissue homogenate
Malondialdehyde (MDA) in tissue homogenate was estimated [26] briefly, 0.2 ml of tissue homogenate was taken and to this 0.2ml of 8.1 %SDS, 1.5 ml of 20 % acetic acid and 1.5ml of aqueous TBA (0.8 %) were added and volume was made up to 5ml with distilled water and heated under oil bath at 95℃ for 1hr. Then mixture of n-butanol and pyridine (15:1 v/v) was added and shaken vigorously. Then mixture was centrifuged at 4000 rpm for 10 m, to separate the organic layer and absorbance was measured at 532nm. The tissue MDA levels are measured from the standard curve and expressed as µM.
Assessment of behavioral parameters
Behavioral studies were performed post-surgery on 1st, 15th and 22nd days of study.
Thermal hyperalgesia (hot plate test)
Thermal nociceptive threshold is the index for thermal hyperalgesia, which was performed using hot plate Eddy’s hot plate [27] with slight modifications. The hot plate was maintained at 55℃. Then the rat was placed on the plate and nociceptive threshold was obtained with respect to licking of paw, jumping and other responses. The paw withdrawal latency was recorded in seconds, by maintaining 15s cut off time in triplicates.
Cold allodynia (acetone drop test)
The cold allodynia test was performed and was assessed by spraying a 100µL of acetone onto the surface of the paw, without touching the skin, the response to acetone of rat was noted for 20s and was graded to a 4-point scale [28]. Acetone was applied thrice to the hind paw, with a gap of 5min between the acetone applications and the individual scores noted in 20s interval are added to obtain a single score over a cumulative period of 60s. The minimum score is 0, while the maximum possible score was 9.
Motor co‐ordination test (Rota Rod Test)
Motor co-ordination (grip strength) was evaluated by using Rota Rod Apparatus [29] in briefly the test rats were placed individually for one minute on the rotating rod (25 rpm). Fall of time from the rotating rod during one minute period was recorded.
Assessment of biochemical parameters
Biochemical parameters were performed by isolating the sciatic nerves on 1st, 15th, 22nd day of post-surgical CCI from rats by cervical dislocation. At the injury site, distal portions of sciatic nerve along with the tissue beneath the sciatic nerve were isolated quickly. The sciatic nerve homogenate (10 % W/V) was then prepared using 0.1 M Tris-HCL buffer (pH 7.4) for estimation of total protein content, nitric-oxide content, reduced glutathione, and lipid peroxidation [30].
Histopathology studies
On 1st ,15th and 22nd days of study, sciatic nerves in the proximity to ligation were removed from all the six groups and kept in 10 % neutralized formalin buffer solution in a container and were assigned with a code number. After leaving them in the fixative solution for approximately 24hrs, the samples were washed with running tap water for 4–6 hrs and then were rinsed with increasing concentrations of alcohol and xylene. Then tissues were processed through automatic tissue processor and were embedded in liquid paraffin. Then tissues were cut into 4–6µm thick and stained with haematoxylin and eosin dyes. Selected areas were examined under light microscope at 400X magnification and images were taken.
Statistical analysis
The results are presented as mean ± SEM, and were statistically analyzed by two-way ANOVA followed by Turkey’s multiple comparisons test. All of the statistical analysis was performed using GRAPHPAD Prism 8.3 version.
Results
Biochemical parameters
Total protein content
The total protein content in different groups on 1st, 15th and 22nd day post-surgery was conducted. In animals subjected to CCI, surgery control group there was a significant increase in protein level on 15th day and 22nd day compared to saline treated group. On 15th day SC, DLX, and DLX + ALA are from 0.898 ± 0.030 to 0.620 ± 0.007 and 0.33 ± 0.02 mg/ml respectively. There was significant decrease in protein levels on 15th day in groups treated with DLX, ALA and combination ALA + DLX drugs compared surgery control. Whereas on 22nd day there was significant decrease in ALA, DLX and in combination groups Fig. 1a.
Effect of ALA (25 mg/kg/i.p), DLX (30 mg/kg/p.o), Combination (ALA + DLX) (25 mg/kg; IP,30 mg/kg/p.o) on paw withdrawal latency in thermal hyperalgesia, flicking response in cold allodynia and grip strength in motor coordination test. Data expressed as mean ± SEM (n = 8) rats per group, analysed by two-way ANOVA followed by Tukey’s multiple comparisons test. p < 0.05 (*), p < 0.01 (**), p < 0.001 (***)
Reduced glutathione assay
Reduced glutathione levels in different groups on 1st, 15th and 22nd day of post-surgery were conducted. In animals subjected to CCI, surgery control group showed significant decrease in glutathione levels on 15th day compared to normal group, whereas the groups with SC, DLX, and DLA + ALA showed significant increase from 0.0140 ± 0.002 to 0.043 ± 0.003 and 0.086 ± 0.002 mM respectively in glutathione levels on 15th day compared to surgery control. Group treated with ALA showed a sustained effect throughout the study even up to treatment free period. There was significant increase observed in groups treated with DLX, ALA and in combination groups compared to surgery control Fig. 1b.
Nitric oxide assay
Nitric oxide assay in different groups on 1st, 15th and 22nd day of post-surgery was conducted. In animals subjected to CCI, surgery control group showed significant increase in nitric oxide levels on 15th and 22nd compared to saline treated group. Whereas the groups with SC, DLX, ALA + DLX showed significant decrease from 3.36 ± 0,18 to 1.44 ± 0.06 and 0.06 ± 0.16 µM/ml respectively in nitric oxide on 15th day compared to surgery control. On 22nd day DLX and ALA groups showed significant decrease in nitric oxide levels compared to surgery control and ALA group sustained the reduced levels of nitric oxide Fig. 1c.
Lipid peroxidation assay
Lipid peroxidation assay in different groups on 1st, 15th and 22nd day of post-surgery were conducted. In animals subjected to CCI, surgery control group showed significant increase in MDA levels on 15th day and 22nd day compared to saline treated group. With SC, DLX and DLX + ALA showed significant reduction from 0.862 ± 0.004 to 0.564 ± 0.002 and 0.205 ± 0.002 µM/g tissue respectively. There was a significant sustained decrease in MDA levels even on 22nd day compared to surgery control.
Behavioral studies
Thermal hyperalgesia test (hot plate method)
Thermal hyperalgesia in different groups on 1st, 15th and 22nd day were conducted. In animals subjected to CCI surgery control group showed significant reduction in latency period on 1st day and continued on day 15th and also 22nd day of post-surgery indicates the induction of thermal hyperalgesia. On 15th day of post-surgery paw withdrawal latency of SC, DLX and ALA + DLX was significantly increased from 1.300 ± 0.123 to 2.40 ± 0.20, 2.75 ± 0.300 respectively. On 22nd day combination ALA + DLX showed significant increase in latency time compared to surgery control group. No significant change observed in saline treated and sham operated groups Fig. 2a.
Effect of ALA (25 mg/kg/i.p), DLX (30 mg/kg/p.o), Combination (ALA + DLX) (25 mg/kg; IP,30 mg/kg/p.o) on total protein levels, tissue glutathione levels, tissue nitric oxide and tissue MDA levels. Data expressed as mean ± SEM (n = 3) rats per group, analysed by two-way ANOVA followed by Tukey’s multiple comparisons test. p < 0.05 (*), p < 0.01 (**), p < 0.001 (***)
Cold allodynia (acetone drop test)
Cold allodynia test in different groups on 1st, 15th, 22nd day were conducted. In animals subjected to CCI surgery control group showed significant decrease in the flicking response on 1st day compared to saline treated group and continued to decrease on 15th day and 22nd day of post-surgery indicates the induction of cold allodynia. No significant change was observed in saline treated and sham operated groups. On 15th day of post-surgery the flicking response of SC. DLX and ALA + DLX was increased from 1.600 ± 0.470 to 2.59 ± 0.27, 3.37 ± 0.36 respectively. The Criteria of response in 4-point scale is, 0 no response,1 quick withdrawal, flick or stamp of the paw, 2 prolonged withdrawal or repeated flicking, 3 repeated flicking with licking of the paw Fig. 2b.
Motor coordination test (rota rod test)
Motor coordination test in different groups on 1st, 15th, 22nd day were conducted. In animals subjected to CCI surgery control group showed a significant decrease in motor coordination (grip strength) on 1st day compared to saline treated group, the same continued on 15th and 22nd day of post-surgery. There was significant increase in grip strength with SC, DLX, ALA + DLX increase from 2.40 ± 0.212 to 8.47 ± 0.40, 9.22 ± 0.29 respectively. On 22nd day the effect was sustained when compared to surgery control Fig. 2c.
Histopathology
In both normal and sham operated groups, histopathology images of nerves taken on 1st, 15th and 22nd day showed myelin covering and axons within normal limits. The histopathology of surgery control 1st day showed severe foci of inflammation in endoneurium and DLX, ALA and combination 1st day showed inflammation and axonopathy similar to that of surgery control 1st day. On 15th day decreased axonopathy is seen in DLX, ALA and combination groups compared to that of surgery control group. Whereas on 22nd day the treatment groups showed axonopathy with slight gliosis of nerve tissue, but ALA showed less inflammation on 22nd day compared to that of Surgery control and DLX Fig. 3.
Histopathology of sciatic nerve section (400 X) of normal, sham operated, surgery control, DLX, ALA and, DLX + ALA groups taken on 1st, 15th and 22nd days of study. The arrows indicate the appearance of axons and myelin sheaths of different groups. The graph below indicates the percentage (%) of axonopathy in different groups on 1st, 15th and 22nd days of study
Discussion
Chronic pain is an unrelenting condition and at present there are few drugs are available to treat with more side effects. So, searching new strategies with new compounds became essential in the effective treatment of neuropathic pain [31]. Peripheral neuropathy is characterized by nerve damage and its compressive nature is explained in radiculopathy or sciatica which involves lower extremities and is related to disc herination [32]. Neuropathic pain is associated with oxidative stress and is induced by imbalance of the cellular redox system based on ROS excessive production or dysfunction of the endogenous antioxidant system. Many studies explain about that, oxidative stress is responsible for neuropathic pain and antioxidants are effectively managing the neuropathic pain in rats [33, 34]. ALA was chosen as antioxidant in this study and proven as strong antioxidant with neuroprotective effect occurring naturally in the body and is also present in some foods. In present study, the effect of ALA (25 mg/kg/i.p) and DLX (30 mg/kg/p.o) and combination of both is evaluated in chronic neuropathic pain model induced by CCI by different behavioral, biochemical parameters and histopathology studies. Inducible nitric oxide levels are over expressed in the CCI of sciatic nerve [35] and anti oxidants reduced the levels of nitric oxide to attenuate neuropathic pain [36] and the similar reduction of nitric oxide levels are observed in this study. CCI model is the good paradigm used in the entrapment (compressive) neuropathy that leads to massive nerve degeneration, with changes in axonal and myelin component. Sciatic Nerve Ligation causes histological aberrations and these were decreased by antioxidant [37] treatment and our study results related this findings.
Central sensitization of neurons is a result of the motor as well as sensory fibers thus causes decrease in thermal withdrawal latency and increase in flicking response. Various transection, ligation and crushing of sciatic nerve and its branches induces ipsilateral cold, heat hyperalgesia and allodynia thereby indicating the induction of peripheral neuropathic pain [38, 39]. These behavioral alterations are constantly present and last over 2–3 weeks, but their time course varying upon the model and species [40]. In study, the tissue MDA levels, Nitrite levels are raised and fall in reduced glutathione level was resulted after nerve injury [41]. The decrease in the level of GSH increases susceptibility to oxidative damage [42]. In another study, nerve ligation increases oxidative stress, documented by increased levels of MDA, increased oxidation state of proteins [43]. In present study animals subjected to CCI, surgery control group showed significant decrease in thermal withdrawal latency, grip strength and increase in flicking response this indicates induction of neuropathic pain. DLX, ALA and combination of both DLX and ALA showed significant increase in thermal withdrawal latency, grip strength and decrease in flicking response results related to previous findings and indicates ALA is effective as neuroprotective and comparable to that of DLX treated group in behavioral studies.
In biochemical parameters the surgery control group showed significant increase in Protein levels, MDA levels, nitric oxide levels and decrease in glutathione levels on 15th and 2nd day of study as that described above in nerve injury, this indicates the induction of neuropathic pain. DLX, ALA and combination treated groups showed significant decrease of protein levels, MDA levels, nitric oxide levels and increase in glutathione levels, this shows that ALA because of its antioxidant potential increased the levels of glutathione and decreased other oxidation causing parameters. Histopathological findings showed increase in axonopathy in surgery control group on 15th and 22nd day. Treatment groups showed decreased axonopathy compared to that of surgery control. ALA showed neuroprotective effect and maintained the decreased levels of MDA, protein content, nitric oxide, increased glutathione levels. This was evidenced during the treatment free period and same as that of combination treated group.
Conclusions
ALA attenuated the neuropathic chronic pain induced by CCI mimicking entrapment neuropathy. This attenuation is attributed to antioxidant and anti-inflammatory effects of ALA. This suggests that antioxidant effect represents the therapeutic approach in the treatment of chronic peripheral neuropathy. ALA enhanced the action of DLX, when given in combination by showing a sustained effect even after treatment was stopped. This indicates the supplementation and/or combination with DLX will give better relief from the pain. Further pharmacokinetic studies are recommended, for dose adjustments of DLX when given along with ALA to develop as a potential clinically relevant drug of interest in treatment of chronic neuropathic pain.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
IASP. Taxonomy. Pain terms. Neuropathic pain. 2017.
Lépine JP, Briley M. The epidemiology of pain in depression. Hum Psychopharmacol. 2004;19(Suppl 1):3–7.
Smith BH, Torrance N. Epidemiology of neuropathic pain and its impact on quality of life. Curr Pain Headache Rep. 2012;16(3):191–8.
Daousi C, Benbow SJ, MacFarlane IA. Electrical spinal cord stimulation in the long-term treatment of chronic painful diabetic neuropathy. Diabet Med. 2005;22(4):393–8.
Sandkühler J. Models and mechanisms of hyperalgesia and allodynia. Physiol Rev. 2009;89(2):707–58.
Woolf CJ, Mannion RJ. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet. 1999;353(9168):1959–64.
Mendell JR, Sahenk Z. Clinical practice. Painful sensory neuropathy. N Engl J Med. 2003;348(13):1243–55.
R G, M D. Leprosy: a participating factor for complex regional pain syndrome. Minerva Anaesth. 2010;76(9):758–60.
Koltzenburg M. Painful neuropathies. Curr Opin Neurol. 1998;11(5):515–21.
Bennett GJ. A neuroimmune interaction in painful peripheral neuropathy. Clin J Pain. 2000;16(3 Suppl):139-43.
Tracey DJ, Walker JS. Pain due to nerve damage: Are inflammatory mediators involved. Inflamm Res. 1995;44(10):407–11.
Backonja MM. Neuropathic pain therapy: from bench to bedside. Semin Neurol. 2012;32(3):264–8.
Campbell JN, Meyer RA. Mechanisms of neuropathic pain. Neuron. 2006;52(1):77–92.
Ji G, Li Z, Neugebauer V. Reactive oxygen species mediate visceral pain-related amygdala plasticity and behaviors. Pain. 2015;156(5):825–36.
Kim HK, Park SK, Zhou JL, Taglialatela G, Chung K, Coggeshall RE, et al. Reactive oxygen species (ROS) play an important role in a rat model of neuropathic pain. Pain. 2004;111(1–2):116–24.
Lee WY, Orestes P, Latham J, Naik AK, Nelson MT, Vitko I, et al. Molecular mechanisms of lipoic acid modulation of T-type calcium channels in pain pathway. J Neurosci. 2009;29(30):9500–9.
Emmez H, Yildirim Z, Kale A, Tönge M, Durdağ E, Börcek AO, et al. Anti-apoptotic and neuroprotective effects of α-lipoic acid on spinal cord ischemia-reperfusion injury in rabbits. Acta Neurochir (Wien). 2010;152(9):1591–600. discussion 600-1.
Costantino M, Guaraldi C, Costantino D, De Grazia S, Unfer V. Peripheral neuropathy in obstetrics: efficacy and safety of α-lipoic acid supplementation. Eur Rev Med Pharmacol Sci. 2014;18(18):2766–71.
Memeo A, Loiero M. Thioctic acid and acetyl-L-carnitine in the treatment of sciatic pain caused by a herniated disc: a randomized, double-blind, comparative study. Clin Drug Investig. 2008;28(8):495–500.
Nagamatsu M, Nickander KK, Schmelzer JD, Raya A, Wittrock DA, Tritschler H, et al. Lipoic Acid Improves Nerve Blood Flow, Reduces Oxidative Stress, and Improves Distal Nerve Conduction in Experimental Diabetic Neuropathy. Diabetes Care. 1995;18(8):1160.
Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain. 1988;33(1):87–107.
Iyengar S, Webster AA, Hemrick-Luecke SK, Xu JY, Simmons RM. Efficacy of duloxetine, a potent and balanced serotonin-norepinephrine reuptake inhibitor in persistent pain models in rats. J Pharmacol Exp Ther. 2004;311(2):576–84.
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951;193(1):265–75.
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR. Analysis of nitrate, nitrite, and [15 N]nitrate in biological fluids. Anal Biochem. 1982;126(1):131–8.
Ellman GL. Tissue sulfhydryl groups. Arch Biochem Biophys. 1959;82(1):70–7.
Ohkawa H, Ohishi N, Yagi K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem. 1979;95(2):351–8.
Hargreaves K, Dubner R, Brown F, Flores C, Joris J. A new and sensitive method for measuring thermal nociception in cutaneous hyperalgesia. Pain. 1988;32(1):77–88.
Flatters SJ, Bennett GJ. Ethosuximide reverses paclitaxel- and vincristine-induced painful peripheral neuropathy. Pain. 2004;109(1–2):150–61.
Jones BJ, Roberts DJ. The quantitative measurement of motor inco-ordination in naive mice using an accelerating rotarod. J Pharm Pharmacol. 1968;20(4):302–4.
Aswar M, Kute P, Mahajan S, Mahajan U, Nerurkar G, Aswar U. Protective effect of hesperetin in rat model of partial sciatic nerve ligation induced painful neuropathic pain: an evidence of anti-inflammatory and anti-oxidative activity. Pharmacol Biochem Behav. 2014;124:101–7.
Meotti FC, Luiz AP, Pizzolatti MG, Kassuya CAL, Calixto JB, Santos ARS. Analysis of the Antinociceptive Effect of the Flavonoid Myricitrin: Evidence for a Role of the Arginine-Nitric Oxide and Protein Kinase C Pathways. J Pharmacol Experimental Therapeutics. 2006;316(2):789.
Laporte C, Albert J-D, Duvauferrier R, Bertaud V, Gouillou M, Guillin R. MRI Investigation of Radiating Pain in the Lower Limbs: Value of an Additional Sequence Dedicated to the Lumbosacral Plexus and Pelvic Girdle. Am J Roentgenol. 2014;203(6):1280–5.
Low PA, Nickander KK, Tritschler HJ. The roles of oxidative stress and antioxidant treatment in experimental diabetic neuropathy. Diabetes. 1997;46(Suppl 2):38–42.
Tal M. A novel antioxidant alleviates heat hyperalgesia in rats with an experimental painful peripheral neuropathy. Neuroreport. 1996;7(8):1382–4.
Lin H, Hou C, Chen D. Altered expression of inducible nitric oxide synthase after sciatic nerve injury in rat. Cell Biochem Biophys. 2011;61(2):261–5.
Bhat RA, Lingaraju MC, Pathak NN, Kalra J, Kumar D, Kumar D, et al. Effect of ursolic acid in attenuating chronic constriction injury-induced neuropathic pain in rats. Fundam Clin Pharmacol. 2016;30(6):517–28.
Kandhare AD, Mukherjee AA, Bodhankar SL. Neuroprotective effect of Azadirachta indica standardized extract in partial sciatic nerve injury in rats: Evidence from anti-inflammatory, antioxidant and anti-apoptotic studies. Excli j. 2017;16:546–65.
Jaggi AS, Jain V, Singh N. Animal models of neuropathic pain. Fundam Clin Pharmacol. 2011;25(1):1–28.
Kaur G, Jaggi AS, Singh N. Ameliorative potential of pralidoxime in tibial and sural nerve transection-induced neuropathic pain in rats. Biol Pharm Bull. 2010;33(8):1331–6.
Crisp T, Giles JR, Cruce WLR, McBurney DL, Stuesse SL. The effects of aging on thermal hyperalgesia and tactile-evoked allodynia using two models of peripheral mononeuropathy in the rat. Neurosci Lett. 2003;339(2):103–6.
Jain V, Pareek A, Bhardwaj YR, Singh N. Attenuating effect of standardized fruit extract of Punica granatum L in rat model of tibial and sural nerve transection induced neuropathic pain. BMC Complement Altern Med. 2013;13:274-.
Vallianou N, Evangelopoulos A, Koutalas P. Alpha-lipoic Acid and diabetic neuropathy. Rev Diabet Stud. 2009;6(4):230–6.
Varija D, Kumar KP, Reddy KP, Reddy VK. Prolonged constriction of sciatic nerve affecting oxidative stressors & antioxidant enzymes in rat. Indian J Med Res. 2009;129(5):587–92.
Acknowledgements
We thank Dr. AV Rao for their expert help in the histopathology studies.
Funding
This study was not supported by any funding body.
Author information
Authors and Affiliations
Contributions
PN has involved in conceptualization, data curation, investigation, methodology, Software, Supervision, Validation, Visualization and writing - review & editing. NKM has take part in formal analysis writing draft and project handling. The author(s) read and approved the final manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Consent for publication
Not applicable.
Competing interests
No competing interests declared in this publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Neerati, P., Prathapagiri, H. Alpha lipoic acid attenuated neuropathic pain induced by chronic constriction Injury of sciatic nerve in rats. Clin Phytosci 7, 21 (2021). https://doi.org/10.1186/s40816-021-00263-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40816-021-00263-7