Abstract
Background
Excessive gestational weight gain (EGWG), insufficient prenatal physical activity and sleep, and poor psychological wellbeing independently increase risks for adverse maternal and infant outcomes. A novel approach to mitigate these risks is utilizing peer support in a community-based prenatal intervention. This study assessed the feasibility (acceptability, demand, implementation, and practicality) of a remotely delivered prenatal physical activity intervention called My Baby, My Move + (MBMM +) that aims to increase prenatal physical activity, enhance mood and sleep hygiene, and reduce EGWG.
Methods
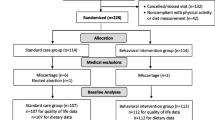
Participants were recruited through community organizations, local clinics, and social media platforms in the Fall of 2020 and Spring of 2021. Eligible pregnant women were randomized to either the MBMM + intervention or the control group. Each group met over Zoom for 16 sessions (twice weekly for 60 min over 8 weeks) to learn either behavioral change and wellbeing knowledge and skills (MBMM +) or knowledge and skills related to parenting (control group). Multiple methods of evaluation to better understand the feasibility of the intervention were conducted.
Results
A total of 49 women (25 MBMM + intervention, 24 control) completed both pre- and post-survey assessments and were included in the analyses. A subsample of 19 (39%) intervention participants completed a combination of semi-structured interviews/surveys to assess acceptability, demand, implementation, and practicality. Participants expressed positive feedback regarding acceptability (satisfaction and intent to continue use) and were extremely likely or likely to recommend the program to a friend (demand). Implementation metrics were assessed by observation and feedback forms completed by peer leaders and demonstrated high-quality control. Findings suggest that the intervention was practical due to remote sessions and cost-effectiveness.
Conclusion
The MBMM + intervention was deemed to be a feasible intervention with high acceptability, demand, implementation, and practicality. These findings can be used to inform the scalability of the intervention and implementation of a larger efficacy trial.
Trial registration
19–1366, initial date is on January 23, 2020.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Key messages regarding feasibility
-
The remote delivery platform of MBMM + may influence components of feasibility (especially practicality).
-
MBMM + showed high feasibility across acceptability, demand, implementation, and practicality.
-
Feasibility findings from this study will inform the testing of MBMM + in a larger efficacy trial to better understand its impact on indicators of maternal health.
Background
The USA has the highest rate of maternal mortality among high-income countries [1], and this rate is continuing to increase [2]. Contributors to maternal mortality include preventable adverse pregnancy and birth outcomes that may stem from excessive gestational weight gain (EGWG) [3, 4]. Approximately half of pregnant women in the USA gain more than the recommended weight during pregnancy based on the Institute of Medicine (IOM) guidelines [5]. EGWG increases the risk of complications throughout pregnancy such as gestational diabetes [6, 7], pre-eclampsia [8], and adverse birth outcomes including preterm birth [9] and the need for cesarean birth [10] and medical induction interventions [11]. EGWG also increases the risk of excessive maternal weight retention, obesity, and associated chronic diseases during the postpartum period and beyond [8, 12,13,14,15].
Traditional interventions aimed to reduce EGWG have focused primarily on nutrition/dietary changes [16,17,18]. However, results related to sustaining these behavior changes into the postpartum period are conflicting [13, 17, 19,20,21,22]. This may be due in part to the variation in health care provider recommendations, as well as understanding and compliance with recommendations [23, 24]. A recent review highlights the need to identify specific modifiable factors related to gestational weight gain to design more effective EGWG interventions [25]. For example, interventions that focus on physical activity have shown to be effective in the prevention of EGWG [19, 26, 27] and when physical activity is combined with dietary changes, there is greater potential for healthier outcomes and sustained habits.
Prenatal physical activity is an attractive intervention strategy for EGWG as it simultaneously promotes a multitude of maternal health benefits (e.g., reduction in risk of gestational diabetes, pre-eclampsia, depression, and body image dysphoria) [28,29,30]. Moreover, there is a clear need to identify effective strategies to increase prenatal physical activity as approximately 80% of pregnant women are not meeting recommended guidelines [31,32,33]. A combination of knowledge, skill building, motivation, and stress management may increase the likelihood of consistent engagement in regular physical activity throughout pregnancy. Studies have found that pregnant women often struggle with maintaining motivation to exercise during pregnancy due to lack of time and tiredness [30, 34]. Moreover, 10–51% of women experience mental distress and/or mood disorders [35,36,37] during pregnancy, exacerbating low energy and motivation to be active. Poor mood during pregnancy is also associated with compromised sleep quality [38, 39]. In turn, poor sleep quality and depressed mood may hinder the physical activity patterns that have been shown to significantly reduce depressive symptomatology and improve sleep quality during pregnancy [40, 41].
Little is known about the triadic relationship among physical activity, mood, and sleep during pregnancy and how they may collectively mitigate EGWG. Independently, studies have found that both poor sleep and mood are associated with EGWG [26, 42,43,44,45]. Additionally, women who exhibit high self-regulation have a better understanding of how physical activity benefits their mood and sleep and may be more motivated to continue with activity into the postpartum period [46, 47]. Given these inter-connected relationships, EGWG interventions may be more effective if they simultaneously target physical activity, mood, and sleep.
Social support is another factor that may mitigate adverse perinatal outcomes [48, 49]. Social support may reduce the risk of postpartum depression [49] and stress in the perinatal period [50]. Social support further enhances the likelihood of engagement in regular physical activity in the perinatal period [51]. The My Baby My Move + (MBMM +) intervention provides social support by incorporating a peer-led intervention delivery platform. Peer-led support interventions are not only cost-effective [52] but may be a more accessible and/or attractive option for pregnant women and increase the feasibility of participation. This paper presents findings related to the survey and qualitative interview data that were collected to assess the feasibility of the MBMM + intervention based on the following constructs from Bowen’s feasibility framework: acceptability, demand, implementation, and practicality [53].
Methods
Study design
We conducted a pilot randomized controlled trial (RCT) to test the feasibility [53] of the MBMM + online intervention compared to an online childbirth education control. The pilot RCT included two cohorts totaling 49 participants. The first cohort (Fall Cohort) participated soon after the onset of the COVID-19 pandemic from August 2020 to November 2020 and included 21 participants (intervention = 11 and control = 10). The second cohort (Spring Cohort) consisted of 28 participants (intervention = 14 and control = 14) and was conducted between April 2021 and June 2021.
Recruitment
Pregnant women were recruited from healthcare clinics as well as through advertisements on social media (e.g., Facebook, parent groups, and community organizations) and listservs. Eligibility criteria for the first cohort included women 18–46 years of age; residing in Denver, Colorado, and surrounding areas with a singleton pregnancy between 8 and 14 weeks in gestation who were self-reportedly underactive (< 120 min of weekly moderate-intensity physical activity); willing to be randomized; and able to obtain medical clearance for physical activity during pregnancy. Given difficulties with recruiting pregnant women during the pandemic, eligibility criteria were expanded in the second cohort to a wider gestational age of 6–14 weeks and to include more active participants (< 150 min of weekly moderate-intensity physical activity). Eligibility was determined by a MBMM + study team member administering a brief screener by phone (questions included age, gestational age, physical activity, general health, and availability to participate) or an online screener through Research Electronic Data Capture electronic (REDCap), a secure, online data capture system [54].
Procedures
Study participants’ approval was obtained from the Colorado Multiple Institutional Review Board (COMIRB #19–1366). Eligible participants provided informed electronic consent and completed an online baseline assessment (T1) using REDCap and obtained medical clearance to exercise from their healthcare providers in the form of a signed letter, which was then either delivered in paper form or scanned and emailed to the study team. Following the completion of the consent form and baseline assessment, participants were randomly assigned to either the intervention (MBMM + program) or control arm (childbirth education group) using a pre-generated table program manual for either the intervention or control.
Due to the COVID-19 pandemic, the intervention and the control curriculum were adapted from their original in-person formats to be delivered online. Instead of asking participants to meet at a recreation center to distribute materials, study team members dropped off study-related materials to each participant’s home (both intervention and control participants) including a Tanita scale and study arm-specific program manual. MBMM + intervention participants also received a yoga mat and pedometer.
MBMM + intervention
The guiding theoretical framework for the MBMM + intervention was based on the social cognitive theory (SCT) and the social support theory [55]. These theories were selected as they include theoretical constructs such as self-efficacy, behavioral skills (e.g., self-regulation and problem-solving), and social support; all of which are strong change agents and shown to be effective in initiating and maintaining physical activity [56, 57]. Intervention activities included goal setting, which was supported by the daily tracking logs, to promote self-monitoring, which is associated with self-efficacy, and discussion around addressing barriers to regular physical activity (problem-solving). Intervention strategies and theoretical components are summarized in Table 1. These agents of behavioral change have been shown to not only increase physical activity but to sustain regular physical activity beyond the intervention. The intervention also promoted the connection between participants through live online conversations and group discussions.
Up to 4 weeks prior to the first online MBMM + session, intervention and control participants received a starter educational packet delivered to their homes by study team members. The packets included study-arm-related material. The intervention educational packet included basic information related to exercising and managing stress during pregnancy. The MBMM + intervention consisted of 16 online group sessions (60-–75-min session, two times a week for 8 weeks). Sessions were held on weekday evenings, as these times were preferred by recruited participants. Each online intervention group session consisted of a didactic portion in which educational materials were discussed live over Zoom, followed by an experiential physical activity component (i.e., walking or prenatal yoga facilitated by a certified prenatal yoga instructor). Live online didactic components covered information such as overcoming barriers to physical activity, goal setting, self-monitoring, problem-solving, topics related to mood (stress management, family/work balance, emotional eating, and the “wellness wheel”), sleep hygiene (setting routines, avoiding stimulants, and environmental supports), and additional physical activity topics (managing physical activity in postpartum and overcoming relapses). The second half of each session included an experiential component that involved a combination of meeting with peer leaders to discuss goals and barriers, designating time for walking at a moderate intensity based on national recommendations [58], and/or live online prenatal yoga (facilitated by a trained prenatal yoga teacher).
The MBMM + intervention was delivered by peers (i.e., women from the community who were either pregnant at the time and engaging in regular physical activity or a new mother (< 2 years postpartum) who regularly engaged in physical activity during a previous pregnancy. Peer leaders were recruited from local clinics, community centers, and through social media to facilitate intervention sessions. Eligible peer leaders participated in a hiring process (i.e., interviews) and were selected based on their community ties and ability to create positive atmospheres for pregnant participants. The PI and study team conducted peer leader training sessions (1.5–2 h, dependent on questions raised by peer leaders) before the onset of the intervention to cover topics including how to engage in safe and effective physical activity during pregnancy, an overview of behavioral change through social cognitive theory, the behavioral skills targeted by the intervention, and ways to garner social support, leadership and communication skills, and sensitivity training related to mental health. Each peer leader met with a small group of participants live over Zoom (an average of four participants per group) during each MBMM + session to help participants set physical activity goals, brainstorm ways to overcome potential barriers, and provide continual encouragement and motivation. Peer leaders recorded weekly goals for each participant in the small group on an online questionnaire submitted to the study team. The study team including the PI and program coordinator regularly met with the group peer leaders to debrief sessions and address any unanticipated issues that may have been submitted through participant feedback and to make any adaptations needed. Though the meetings were held online rather than the intended in-person format, all distributed materials and guided discussions remained the same.
Control group
The study team developed a childbirth education curriculum called “Baby Basics” for the control group to account for similar time and attention as the intervention group. A packet of online materials related to various prenatal topics included the biology of pregnancy, mitigating symptoms of pregnancy-related nausea, selecting a health care provider, and establishing a support system was distributed 4 weeks prior to the start of the 8-week online sessions. Though the control group also met online rather than the originally planned in-person format, all materials including the curriculum booklet remained the same. All control group participants were invited to attend 16 online sessions (2 × week for 8 weeks). Sessions lasted approximately 60 min and were held on weekday evenings at the same time and for the same duration as the intervention group, as these times were preferred by recruited participants. The control curriculum included evidence-based recommendations for birth planning, postpartum care, breastfeeding, and infant care from entities such as the American Academy of Pediatrics [59] and the American College of Obstetricians and Gynecologists [60]. The curriculum was reviewed by a board-certified obstetrician-gynecologist. The control group facilitator was a member of the study team and a trained Certified Lactation Counselor and Childbirth Educator who received research training in EGWG and perinatal health behaviors.
Assessment instruments
At baseline (T1), participants in both the intervention and control arms were asked to complete objective assessments by logging their weight for three consecutive days both pre-intervention (T1) and post-intervention (T3) via photos of the provided scales. Intervention participants were also asked to complete weekly intervention tracking logs, which consisted of daily reports of weight, physical activity, sleep, and mood patterns throughout participation in the MBMM + intervention. Tracking logs were collected weekly by the study team through email. Participants were also asked to complete a survey at T1 that included the following validated measures: the Leisure-Time Exercise Questionnaire [61] which is commonly used to measure exercise behavior in pregnant women, the Edinburgh Postnatal Depression Scale [62] which detects depressive symptoms in prenatal and postpartum women, and additional validated measures including the general anxiety disorder-7 scale (GAD-7) [63], the Perceived Stress Scale (PSS) [64], the Mindfulness Attention Awareness Scale-5 (MAAS-5) [65], and the Pittsburgh Sleep Quality Index (PSQI) [66].
A mid-point assessment (T2) was completed 6 weeks into the intervention for both intervention and control groups using REDCap and at their convenience. The T2 assessment contained a modified survey questionnaire measuring weight, as well as questions from the Godin, the EPDS, GAD-7, PSS, MAAS-5, and PSQI. Finally, participants from both the intervention and control groups completed the online survey consisting of the aforementioned validated measures and weight assessment at the end of the intervention (T3) (12 weeks post-baseline) using REDCap. Data from the weight measurements, tracking logs, and validated survey measures will be reported in subsequent manuscripts. Upon completion of the randomized controlled trial, participants had the opportunity to also participate in a survey that assessed the feasibility of the MBMM + intervention.
Feasibility survey
The feasibility survey was based on Bowen’s feasibility framework [53]. The constructs included acceptability, which assesses the reactions from the participants, demand, which estimates the use of the intervention, implementation, which focuses on the manner in which an intervention can be implemented as planned, and practicality, which explores the resources, time, and commitment required to successfully execute an intervention. The feasibility survey questionnaire consisted of 24 multiple choice and open-ended questions regarding different aspects of the program, including “What did you like most about The MBMM + Program?” (acceptability), "How helpful did you find the following program components: (i.e., electronic materials, daily tracking log, small group sessions with your peer leader)?” (implementation), and "How helpful did you find the following program components (i.e., attending program sessions, wearing the pedometer, setting goals)?” (practicality). After completion of the T1 and T2 assessment surveys, participants received a $30 electronic gift card.
Participants in both the intervention and control groups were also randomly selected to participate in semi-structured interviews at T3, in which 19 participants across both cohorts in the intervention and control groups participated. Interviews were conducted over Zoom by study team members (JL, RL, and JW) who are trained in collecting and analyzing qualitative data. Interviews included questions related to the feasibility of the intervention or control as well as the strengths and limitations of each program. For example, participants were asked, “Which part of the program did you enjoy the most, and why?” (acceptability) and “Were you able to attend the sessions with your work schedule?” (practicality). Interviews lasted approximately 25 min (12–37 min). After completion of each interview, participants received a $30 electronic gift card.
Peer leader assessments
Throughout the delivery of the intervention, the study team met weekly with the lead peer leader to debrief and address any arising issues. In addition to the weekly debriefing meetings, each peer leader completed session feedback forms that were monitored by the study team to assess the quality control and feasibility of the intervention. Peer leaders noted the group’s progress on meeting weekly goals, overall discussion related to identified barriers, recommended evidence-based strategies, and recommended action steps in weekly feedback forms. The study team reviewed these forms following each session and monitored the intervention’s delivery to inform program implementation. Peer leaders also completed a brief role-related survey at T3. This survey assessed their likelihood of returning as a peer leader in the future, the impact and usefulness of the programmatic components (e.g., tracking logs, small group sessions, and didactic presentations) as well as their preparedness in effectively building relationships with the participants (e.g., training and study team support).
Assessing feasibility
Feasibility was assessed using a combination of surveys, interviews, and programmatic records. Descriptive statistics from continuous and categorical survey data were computed using SPSS software [67]. Qualitative interviews were audio-recorded, transcribed verbatim, and stored on a password-protected computer. Transcripts were analyzed by members of the study team (RL, JW, and JL) using a deductive approach in ATLAS.ti [68] software based on constructs from Bowen’s feasibility framework [53]. Programmatic records were reviewed including attendance tracking, intervention tracking log completion, and peer leader feedback forms to inform findings related to demand and implementation of the MBMM + program.
Results
Demographics
Demographic data for the full sample can be found in Table 2. The average age of participants was 31.8 years, and the median age was 32. 64.3% of the total sample had no other children at home and 4.7% had 1 or more children. Approximately 22% of participants identified as Hispanic or Latino, 81.6% Caucasian, and 8.2% African American. Approximately 14.3% reported a household income of less than $49,999, 18.4% reported $50,000–$74,999, 65.3% reported $75,000 or more. The sample was highly educated with approximately 81% a recipient of a college degree or more and 18.4% more than a college degree. Most participants (81.6%) had full health care coverage, only 8.4% had partial coverage or Medicaid (federally and/or state-funded health care). The majority of the sample were married (81.6%), while 18.4% were single or partnered. Over half of the participants (53.1%) had a BMI placing them in the “normal weight” category, while 8.2% were underweight, 20.4% overweight, and 18.3% obese.
Feasibility survey and qualitative interview findings
A total of 14 MBMM + participants completed the feasibility survey, and 15 intervention and 4 control participants completed interviews at T3. Table 3 displays a detailed description of the survey and interview feasibility results.
Data analysis suggested high acceptability; 100% of participants stated they would recommend the program to another pregnant individual and all respondents were “somewhat satisfied” or “very satisfied” with the program. Participants appreciated how intervention materials were delivered in multiple formats (i.e., hard copies and electronically). Among peer leaders, the average score of enjoyment related to the facilitation of the group sessions was 4.6 (1 (not at all enjoyable) to 5 (highly enjoyable)). All peer leaders found it “very helpful” to have a member of the study team attend each session. The control intervention was also deemed to be acceptable; over 85% of control group participants were satisfied with the program and another 72% of participants were “likely” or “extremely likely” to recommend the control program to a friend.
Demand was measured by attendance and participation in the MBMM + intervention sessions. Approximately 2/3 (68%) of intervention tracking logs were completed throughout the intervention, leading to 68% of participants being categorized as “compliant” (attended 10 or more sessions) with the average compliant participant attending 85% of sessions. While the final sample was small, there were many women who showed interest in the intervention and were not eligible. Interested women that were outside the gestational age parameters, were physically active for more than 150 min per week, or did not receive medical clearance from their health care provider were not permitted to participate.
Implementation was measured by the ability of participants and peer leaders to implement all intervention activities. Participants qualitatively shared how the intervention materials (yoga mat, tracking logs, and manuals) enhanced their experience in the program and enabled them to participate in the weekly didactic and experiential portions of the program. Participants also mentioned how the incentives (diaper raffles and gift cards) were helpful tools to increase accountability and attendance. One participant expressed appreciation for the delivery of materials: “I was at home with my other kiddos, so it was nice to have the materials brought to me”. Additionally, all peer leaders completed 16/16 session feedback forms which suggest implementation success related to this component of the MBMM + program. The program coordinator was present for all intervention group meetings, and the PI attended approximately half of the MBMM + sessions and at least two sessions for each cohort for the control group to assess the quality of program delivery and implementation.
Practicality was assessed by the ease with which participants could realistically participate in terms of time, space, and materials. Participants gave positive feedback regarding the timing of the sessions. For example, a fall cohort intervention participant stated: “I did like the sessions later in the day, just because they fit with my work schedule”. Additionally, the online format enabled participation, as one member of the fall cohort explained: “I wouldn’t have been able to be part of the group if it wasn’t on Zoom”. Those with older children expressed that the flexibility of the remote model made it easier to attend because they did not have to find childcare.
Peer leader component
Peer leaders reported a pre-post change in prenatal exercise and weight gain knowledge following the training with the study team. In addition to increased knowledge from the trainings, peer leaders enjoyed participating in the MBMM + intervention; 100% of peer leaders stated they would be peer leaders in the future and would recommend this program to pregnant women in their communities, as either a participant or a leader.
Discussion
Our findings suggest that the MBMM + intervention is feasible. High acceptability was reported by both participants and peer leaders, suggesting that community-based intervention delivery through peer mentors may be an effective strategy in translating prenatal physical activity programs into a community setting [69,70,71,72,73]. Extant studies indicate peer-delivered interventions (i.e., trained volunteer peers) may be as effective as clinical staff-delivered interventions in helping women improve and maintain physical activity [71, 72]. Pregnant women have reported valuing interpersonal interactions with other pregnant women (i.e., peers they can identify with) to motivate and support behavior change such as increased physical activity [71, 73, 74].
Similar to prior research findings [75,76,77], our MBMM + participants conveyed that peer leaders provided a sense of support and guidance for participants. A recent study measuring perceived social support during pregnancy and early childhood also found positive effects of peer support on improving mood and reducing anxiety, stress, and isolation during pregnancy [78]. This was particularly true for primiparous participants in our study, who appreciated the peer leaders and veteran mother’s lived experiences of pregnancy and the postpartum period. In addition to the social and motivational support they offer, peer leaders from the community may be key in encouraging and translating prenatal health behaviors recommended by healthcare providers such as weight, exercise, sleep and stress management guidelines, and referral follow-ups.
The MBMM + intervention also demonstrated high demand among pregnant women due to high attendance and completion of assessments. Many existing EGWG interventions focus on testing clinical interventions in healthcare settings only [42, 79,80,81]. However, a recent systematic overview found that women who participated in group prenatal care (provider- and facilitator-led) had improved attendance rates of prenatal visits [82]. Additionally, utilizing peer leaders may mitigate reliance upon study team members and provide a low-cost opportunity for dissemination [71, 72] of evidence-based practices, improving the likelihood of future scalability. Interventions such as MBMM + that utilize a peer-led approach may translate to increased accessibility of prenatal care interventions that support the adoption of positive health behaviors and mitigate EGWG.
Implementation of the MBMM + was successful in this pilot study. The intervention was originally developed to be delivered in-person at community recreation centers but was adapted for online delivery due to the COVID pandemic. A recent study comparing in-person and online health coaching that targeted physical activity, weight change, and healthy eating demonstrated no significant differences between group formats for physical activity and weight change outcomes [83]. With an increasing demand for virtual programming following the COVID pandemic, a delivery modality of both online and in-person sessions (hybrid) may best support expectant parents while also increasing social support during pregnancy and the postpartum period [84, 85].
Additionally, the idea of a hybrid format translated into high practicality related to participation in the MBMM + intervention. While participants expressed that in-person sessions may have fostered more social support, they also acknowledged the convenience of online sessions, eliminating potential barriers to in-person participation (e.g., transportation, transportation costs, and cost of childcare), which have been cited as barriers to prenatal physical activity even before the pandemic [30].
Findings from this feasibility study suggest that the MBMM + intervention is feasible and also highlight ways to enhance the future refinement of MBMM + . Overall, participants reported that they enjoyed the small group discussions with their peer leaders. Some participants voiced a need for having even more time for a small group discussion in future programming. Additionally, participants suggested that they really enjoyed the stress management activities and desired more examples to be shared. A few participants suggested varying times when sessions were held would be helpful, particularly with some sessions being offered in the afternoons. Lastly, many participants conveyed a desire to meet again in the postpartum period.
Limitations
There are several limitations to this feasibility study. First, due to the COVID-19 pandemic, the intended curriculum was created for in-person facilitation, which had to be adapted for the safety of participants and study team members, causing the need for the program curriculum to be adjusted to an online platform and virtual sessions via Zoom. This online programming changed the delivery of the experiential component (e.g., in-person walking and yoga sessions). In addition to the restructuring of the program, the recruitment of pregnant women presented a challenge. During the first cohort (Fall of 2020), COVID-19 vaccines were not yet available, and many pregnant women were unable to see their OBGYNS as early as recommended in their pregnancy for safety concerns, thus limiting patient-clinic relations. The limited access to clinics/providers hindered the ability to obtain medical clearance forms. Recruitment issues resulted in a small, relatively homogeneous sample size.
Conclusion
In summary, these findings demonstrate that MBMM + is a feasible peer-led intervention with a high degree of acceptance, demand, implementation, and practicality. Future research that tests a hybrid delivery of MBMM + with a larger sample size is needed. Findings from this feasibility study will inform the future refinement of My Baby My Move + to be tested in a larger, well-powered RCT, as well as may inform the future development of other perinatal behavioral interventions that include peer-based facilitation.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to sensitive data and sharing agreements but are available from the corresponding author upon reasonable request.
Abbreviations
- MBMM + :
-
My Baby My Move +
- GWG:
-
Gestational weight gain
- EGWG:
-
Excessive gestational weight gain
References
Gunja MZ, et al. Health and health care for women of reproductive age: how the United States compares with other high-income countries., C. Fund, Editor. 2022.
Declercq E, Zephyrin L. Maternal mortality in the United States: a primer. , C. Fund, Editor. 2020.
Singh GK. Trends and social inequalities in maternal mortality in the United States, 1969–2018. Int J Matern Child Health AIDS. 2021;10(1):29.
Ukah UV, et al. Association between gestational weight gain and severe adverse birth outcomes in Washington State, US: a population-based retrospective cohort study, 2004–2013. PLoS Med. 2019;16(12):e1003009.
Goldstein RF, et al. Gestational weight gain across continents and ethnicity: systematic review and meta-analysis of maternal and infant outcomes in more than one million women. BMC Med. 2018;16(1):1–14.
Lewandowska M, Więckowska B, Sajdak S. Pre-pregnancy obesity, excessive gestational weight gain, and the risk of pregnancy-induced hypertension and gestational diabetes mellitus. J Clin Med. 2020;9(6):1980.
Barnes RA, et al. Excessive weight gain before and during gestational diabetes mellitus management: what is the impact? Diabetes Care. 2020;43(1):74–81.
McDowell M, Cain MA, Brumley J. Excessive gestational weight gain. J Midwifery Womens Health. 2019;64(1):46–54.
Farpour-Lambert NJ, et al. Obesity and weight gain in pregnancy and postpartum: an evidence review of lifestyle interventions to inform maternal and child health policies. Front Endocrinol. 2018;9:546.
Branger B, et al. Cesarean after labor induction: risk factors and prediction score. Gynecologie, Obstetrique, Fertilite & Senologie. 2018;46(5):458–65.
Swift EM, et al. Trends in labor induction indications: a 20-year population-based study. Acta Obstet Gynecol Scand. 2022;101(12):1422–30. https://doi.org/10.1111/aogs.14447.
Voerman E, et al. Association of gestational weight gain with adverse maternal and infant outcomes. JAMA. 2019;321(17):1702–15.
Makama M, et al. Reducing postpartum weight retention: a review of the implementation challenges of postpartum lifestyle interventions. J Clin Med. 2021;10(9):1891.
Kiel DW, et al. Gestational weight gain and pregnancy outcomes in obese women: how much is enough? Obstet Gynecol. 2007;110(4):752–8.
Samura T, et al. Factors associated with excessive gestational weight gain: review of current literature. Global Adv Health Med. 2016;5(1):87–93.
Hoffmann J, et al. Associations between prenatal physical activity and neonatal and obstetric outcomes—a secondary analysis of the cluster-randomized geliS trial. J Clin Med. 2019;8(10):1735.
Lamminpää R, Vehviläinen-Julkunen K, Schwab U. A systematic review of dietary interventions for gestational weight gain and gestational diabetes in overweight and obese pregnant women. Eur J Nutr. 2018;57(5):1721–36.
Spencer L, et al. The effect of weight management interventions that include a diet component on weight-related outcomes in pregnant and postpartum women: a systematic review protocol. JBI Evidence Synthesis. 2015;13(1):88–98.
Gardner B, et al. Changing diet and physical activity to reduce gestational weight gain: a meta-analysis. Obes Rev. 2011;12(7):e602–20.
Pearce EE, et al. Strategies to promote physical activity during pregnancy. Am J Lifestyle Med. 2013;7(1):38–50.
Phillips JK, Higgins ST. Applying behavior change techniques to weight management during pregnancy: impact on perinatal outcomes. Prev Med. 2017;104:133–6.
Tanentsapf I, Heitmann BL, Adegboye AR. Systematic review of clinical trials on dietary interventions to prevent excessive weight gain during pregnancy among normal weight, overweight and obese women. BMC Pregnancy Childbirth. 2011;11(1):1–12.
Delgado A, et al. Provider and patient knowledge and views of office practices on weight gain and exercise during pregnancy. Am J Perinatol. 2018;35(02):201–8.
Dieterich R, Demirci J. Communication practices of healthcare professionals when caring for overweight/obese pregnant women: a scoping review. Patient Educ Couns. 2020;103(10):1902–12.
Hill B, Skouteris H, Fuller-Tyszkiewicz M. Interventions designed to limit gestational weight gain: a systematic review of theory and meta-analysis of intervention components. Obes Rev. 2013;14(6):435–50.
Ruchat S-M, et al. Effectiveness of exercise interventions in the prevention of excessive gestational weight gain and postpartum weight retention: a systematic review and meta-analysis. Br J Sports Med. 2018;52(21):1347–56.
Wiebe HW, et al. The effect of supervised prenatal exercise on fetal growth: a meta-analysis. Obstet Gynecol. 2015;125(5):1185–94.
Russo LM, et al. Physical activity interventions in pregnancy and risk of gestational diabetes mellitus: a systematic review and meta-analysis. Obstet Gynecol. 2015;125(3):576–82.
Phelan S, et al. Randomized trial of a behavioral intervention to prevent excessive gestational weight gain: the fit for delivery study. Am J Clin Nutr. 2011;93(4):772–9.
Harrison CL, et al. The role of physical activity in preconception, pregnancy and postpartum health. In: Seminars in reproductive medicine. (Vol. 34, No. 02). Thieme Medical Publishers; 2016. p. e28–37. https://doi.org/10.1055/s-0036-1583530.
Piercy KL, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–8.
Borodulin K, Evenson KR, Herring AH. Physical activity patterns during pregnancy through postpartum. BMC Womens Health. 2009;9(1):1–7.
Zhang J, Savitz DA. Exercise during pregnancy among US women. Ann Epidemiol. 1996;6(1):53–9.
Bauer C, et al. Reasons, motivational factors, and perceived personal barriers to engagement in physical activity during pregnancy vary within the BMI classes: The Prenatal Prevention Project Germany. J Phys Act Health. 2018;15(3):204–11.
McKee K, et al. Perinatal mood and anxiety disorders, serious mental illness, and delivery-related health outcomes, United States, 2006–2015. BMC Womens Health. 2020;20(1):1–7.
Dagher RK, et al. Perinatal depression: challenges and opportunities. J Womens Health. 2021;30(2):154–9.
Hahn-Holbrook J, Cornwell-Hinrichs T, Anaya I. Economic and health predictors of national postpartum depression prevalence: a systematic review, meta-analysis, and meta-regression of 291 studies from 56 countries. Front Psychiatry. 2017;8:248.
Yang Y, et al. Prevalence of poor sleep quality in perinatal and postnatal women: a comprehensive meta-analysis of observational studies. Front Psych. 2020;11:161.
Sedov ID, et al. Sleep quality during pregnancy: a meta-analysis. Sleep Med Rev. 2018;38:168–76.
Youngstedt SD. Effects of exercise on sleep. Clin Sports Med. 2005;24(2):355–65.
Dunn AL, et al. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005;28(1):1–8.
Bennett CJ, et al. Interventions designed to reduce excessive gestational weight gain can reduce the incidence of gestational diabetes mellitus: a systematic review and meta-analysis of randomised controlled trials. Diabetes Res Clin Pract. 2018;141:69–79.
Jiang H, et al. Can physical activity reduce excessive gestational weight gain? Findings from a Chinese urban pregnant women cohort study. Int J Behav Nutr Phys Act. 2012;9(1):1–7.
Matthews J, et al. Psychosocial predictors of gestational weight gain and the role of mindfulness. Midwifery. 2018;56:86–93.
Gay CL, et al. Sleep disruption and duration in late pregnancy is associated with excess gestational weight gain among overweight and obese women. Birth. 2017;44(2):173–80.
Harrison AL, et al. Attitudes, barriers and enablers to physical activity in pregnant women: a systematic review. J Physiother. 2018;64(1):24–32.
Hamilton K, et al. Being active in pregnancy: theory-based factors associated with physical activity among pregnant women. Women Health. 2019;59(2):213–28.
Bedaso A, et al. The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Reprod Health. 2021;18(1):1–23.
Evans M, Donelle L, Hume-Loveland L. Social support and online postpartum depression discussion groups: a content analysis. Patient Educ Couns. 2012;87(3):405–10.
Zachariah R. Social support, life stress, and anxiety as predictors of pregnancy complications in low-income women. Res Nurs Health. 2009;32(4):391–404.
Kim C, et al. Self-efficacy, social support, and associations with physical activity and body mass index among women with histories of gestational diabetes mellitus. Diabetes Educ. 2008;34(4):719–28.
Huang R, et al. Effectiveness of peer support intervention on perinatal depression: a systematic review and meta-analysis. J Affect Disord. 2020;276:788–96.
Bowen DJ, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–7.
Harris PA, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Glanz K, R.B., Viswanath K., Health Behavior and Health Education. San Francisco. CA: Jossey-Bass; 2008.
Dunn AL, Andersen R, Jakicic JM. Lifestyle physical activity interventions. History, short- and long-term effects, and recommendations. Am J Prev Med. 1998;15(4):398–412.
Stevens AR, Leiferman J. Psychosocial mediators to physical activity during the perinatal period: a systematic review of the literature. J Investig Med. 2011;59(1):143–143. Philadelphia: Lippencott Williams & Wilkins.
DHHS. Physical Activity Guidelines for Americans. 2008.
Eisenberg SR, et al. Maternal report of advice received for infant care. Pediatrics. 2015;136(2):e315–22.
Afshar Y, et al. Birth plans and childbirth education: what are provider attitudes, beliefs, and practices? J Perinat Educ. 2019;28(1):10–8.
Godin G, Shephard R. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10(3):141–6.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;782–786.
Spitzer RL, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Cohen S, Kamarck T, Mermelstein R. Perceived stress scale, in measuring stress: a guide for health and social scientists. 1994. p. 1–2.
MacKillop J, Anderson EJ. Further psychometric validation of the mindful attention awareness scale (MAAS). J Psychopathol Behav Assess. 2007;29(4):289–93.
Buysse DJ, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Verma J. Data analysis in management with SPSS software. Springer Science & Business Media. 2012.
ATLAS.ti Scientific Software Development GmbH, in ATLAS.ti.
Dorgo SKG, Brickey G. The application of peer monitoring to improve fitness in older adults. J Aging Phys Act. 2009;17(3):344–61.
Dorgo SRKaBJ. The effectiveness of a peer-mentored older adult fitness program on perceived physical, mental, and social function. J Am Acad Nurse Pract. 2009;21(2):116–22.
Buman M, G.J.P, Dzierzewski J, McCrae C, Roberts B, Marsiske M. Peer volunteers improve long-term maintenance of physical activity with older adults: a randomized controlled trial. J Phys Act Health. 2011;8:257–66.
Castro C, P.L, Buman M, King A. Physical activity program delivery by professionals versus volunteers: the TEAM randomized trial. Health Psychology. 2011;30(3):285.
Martin Ginis K, N.C, Smith A. Peer-delivered physical activity interventions: An overlooked opportunity for physical activity promotion. Transl Behav Med. 2013;3(4):434–43.
Leiferman JA, S.T, Koiness K, Marshall JA, Dunn AL. My Baby, My Move: examination of perceived barriers and motivating factors related to antenatal physical activity. J Midwifery Womens Health. 2011;56:33–40.
Pekkala J, et al. Key considerations for implementing group prenatal care: lessons from 60 practices. J Midwifery Womens Health. 2020;65(2):208–15.
Novick G, et al. The intersection of everyday life and group prenatal care for women in two urban clinics. J Health Care Poor Underserved. 2012;23(2):589.
Clark A. An analysis of group prenatal care in a high-risk obstetric population. University of Kansas; 2019. PhD diss.
McLeish J, Redshaw M. Mothers’ accounts of the impact on emotional wellbeing of organised peer support in pregnancy and early parenthood: a qualitative study. BMC Pregnancy Childbirth. 2017;17(1):1–14.
Shieh C, et al. Intervention strategies for preventing excessive gestational weight gain: systematic review and meta-analysis. Obes Rev. 2018;19(8):1093–109.
Ronnberg A, Nilsson K. Interventions during pregnancy to reduce excessive gestational weight gain: a systematic review assessing current clinical evidence using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) system. BJOG. 2010;117(11):1327–34.
Altazan AD, et al. Mood and quality of life changes in pregnancy and postpartum and the effect of a behavioral intervention targeting excess gestational weight gain in women with overweight and obesity: a parallel-arm randomized controlled pilot trial. BMC Pregnancy Childbirth. 2019;19(1):1–12.
Byerley BM, Haas DM. A systematic overview of the literature regarding group prenatal care for high-risk pregnant women. BMC Pregnancy Childbirth. 2017;17(1):1–9.
Bus K, et al. Comparison of in-person and online motivational interviewing–based health coaching. Health Promot Pract. 2018;19(4):513–21.
Mousavi SR, et al. Comparing the effect of childbirth preparation courses delivered both in-person and via social media on pregnancy experience, fear of childbirth, birth preference and mode of birth in pregnant Iranian women: a quasi-experimental study. PLoS ONE. 2022;17(8):e0272613.
Gold KJ, Normandin MM, Boggs ME. Are participants in face-to-face and internet support groups the same? Comparison of demographics and depression levels among women bereaved by stillbirth. Arch Womens Ment Health. 2016;19(6):1073–8.
Acknowledgements
The authors would like to thank the perinatal women who participated in the study as well as the providers who referred them to the study.
Funding
The study was funded by the National Institute of Health 5R21HD097450-02, FAIN: R21HD097450).
Author information
Authors and Affiliations
Contributions
JL was the principal investigator on this grant and the main contributor (and corresponding author) to this manuscript. RL was the study coordinator for the project and was a major contributor to writing the manuscript. JW led the control group and was a major contributor to writing the manuscript. MD, DD, SF, CF, JH, JP, and SS were co-investigators and were major contributors to the writing of the manuscript, specifically in their respective areas of expertise. All authors read and approved this manuscript. Additionally, all authors have agreed to ensure the accuracy and integrity of the entirety of the work and to be personally accountable for each of their own contributions. All authors agree to respond to questions about the manuscript to ensure it is appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics was obtained by the Colorado Multiple Institutional Review Board (COMIRB) (COMIRB #19–1366).
Consent for publication
All authors consent to publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Leiferman, J.A., Lacy, R., Walls, J. et al. My Baby, My Move+: feasibility of a community prenatal wellbeing intervention. Pilot Feasibility Stud 9, 134 (2023). https://doi.org/10.1186/s40814-023-01368-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-023-01368-1