Abstract
Background
The purpose of this pilot study was to validate the feasibility of a definitive study aimed at determining if high-intensity physical activity during adolescence impacts the development of femoroacetabular impingement (FAI).
Methods
This prospective cohort pilot study had a sample size target of 50 volunteers between 12 and 14 years old at sites in Canada, South Korea, and the Netherlands. Participants were evaluated clinically and radiographically at baseline and at 2 years. The participants’ sport and physical activity were evaluated using the Habitual Activity Estimation Scale (HAES) and the American Orthopaedic Society for Sports Medicine (AOSSM) criteria for sport specialization. The primary outcome was feasibility and secondary outcomes included the incidence of radiographic FAI and hip range of motion, function (Hip Outcome Score, HOS), and quality of life (Pediatric Quality of Life questionnaire, PedsQL) at 24 months. Study groups were defined at the completion of follow-up, given the changes in participant activity levels over time.
Results
Of the 54 participants enrolled, there were 36 (33% female) included in the final analysis. At baseline, those classified as highly active and played at least one organized sport had a higher incidence of asymptomatic radiographic FAI markers (from 6/32, 18.8% at baseline to 19/32, 59.4% at 24 months) compared to those classified as low activity (1/4, 25% maintained at baseline and 24 months). The incidence of radiographic FAI markers was higher among sport specialists (12/19, 63.2%) compared to non-sport specialists (8/17, 47.1%) at 24 months. The HOS and PedsQL scores were slightly higher (better) among those that were highly active and played a sport compared to those who did not at 2 years (mean difference (95% confidence interval): HOS-ADL subscale 4.56 (− 7.57, 16.70); HOS-Sport subscale 5.97 (− 6.91, 18.84); PedsQL Physical Function 7.42 (− 0.79, 15.64); PedsQL Psychosocial Health Summary 6.51 (− 5.75, 18.77)).
Conclusion
Our pilot study demonstrated some feasibility for a larger scale, definitive cohort study. The preliminary descriptive data suggest that adolescents engaged in higher levels of activity in sports may have a higher risk of developing asymptomatic hip deformities related to FAI but also better quality of life over the 2-year study period.
Similar content being viewed by others
Key messages regarding feasibility
-
There were uncertainties regarding the feasibility of recruiting and following healthy volunteer participants for 2 years.
-
Participants were recruited over 12 months with a 10.4% loss to follow-up rate, with complete outcomes data, including study questionnaires and MRIs, collected for 75% (36/48) of participants at 2 years.
-
These feasibility findings led to protocol changes for the main study including involving additional international sites, implementing novel recruitment strategies, adding interim follow-up visits every 3 months, and introducing an activity log and wrist-worn tracker to improve the collection of physical activity data over the 2-year period.
Introduction
Femoroacetabular impingement (FAI) is a relatively newly recognized painful hip condition. The development of pain in this manner serves as an indicator of early damage to the hip and FAI has been implicated as the probable principal cause of idiopathic hip osteoarthritis (OA) later in life [1,2,3,4,5]. It is classically described as impingement between the femoral head and neck (FHN) junction and acetabular rim because of bony deformities in one or both of these regions [6]. Therefore, two morphologies have been classified: cam morphology—defined as femoral head asphericity or FHN convexity; and pincer morphology—where there is an overcoverage of the femoral head by the acetabulum. It is estimated that most cases of FAI are a mix of both cam and pincer-type morphology [3, 7].
Prior literature has estimated that FAI prevalence ranges from 14 to 23% in the asymptomatic general population and up to 95% in athletes [8,9,10,11]. Awareness of FAI among clinicians has caused a rise in its diagnosis across all age categories but more so in pediatric/adolescent populations [12]. Suggested causes of FAI have included genetics, subclinical hip disease, and stresses to the hip joint from repetitive and high intensity activities at a younger age [13]. According to Packer et al., the genetic implication is not clear, and in otherwise healthy children, there is growing evidence that participation in high level athletics during adolescence causes a higher prevalence of FAI, especially cam morphology [14].
High-impact activities, especially during physeal closure, have been shown to have the potential to cause hip damage [15, 16]. More specifically, high-impact activities have been shown to affect the development of the femur at the growth plate region and FHN junction [17, 18]. Children can suffer more consequences of injuries and shear forces that can cause premature physeal closure, apophyseal avulsion, and chondral injuries because of their open physes and growing cartilage [19]. Typical activities that have been implicated in FAI development include soccer, ice hockey, basketball, and football [10, 17, 20,21,22]. It has been posited that there is a dose-response relationship between the amount of hours of practice every week during adolescence and the eventual incidence of cam-type morphology in adulthood among athletes [15]. This is certainly of concern given the increasing trend toward year-round participation in youth sports with early specialization [23,24,25]. Consequently, research is needed to determine “how much is too much” sport activity in order to advocate for the young who cannot easily protect themselves from excesses [26].
As FAI is diagnosed more frequently in athletes, and with over 38 million young athletes participating in organized sports in the USA alone [19], it has become a priority to identify modifiable variables in order to mitigate the risk of developing FAI in children and adolescents. This is especially important due to the link between FAI and hip OA later in life [12]. The PREVIEW pilot study was initiated to evaluate the feasibility of a large-scale prospective cohort to evaluate the potential risk of developing FAI-related hip deformities based on the intensity, duration, and specialization of sport activity during adolescence.
Methods
Study design and participant selection
This study was a prospective cohort pilot with a sample size target of 50 healthy volunteers between the ages of 12–14 years. Participants were excluded if they had a closed physeal plate (i.e., a mature hip), hip complaints at the time of enrollment, previous hip trauma or surgery, any medical comorbidity that would limit activities of daily living (ADLs), any history of or ongoing pediatric hip disease, or were unwilling to undergo a magnetic resonance imaging (MRI). MRI was used because it does not involve any radiation. Participants were recruited by experienced hip surgeons and sports medicine researchers at 4 clinical sites in Canada (2), South Korea (1), and the Netherlands (1). All participating sites obtained ethics approval. Participants were evaluated clinically and radiographically at baseline and at 2 years.
Defining activity level and sport specialization
The participants’ duration and intensity of any sport and general physical activity were evaluated using the self-reported Habitual Activity Estimation Scale (HAES) and sport specialization was classified according to the American Orthopaedic Society for Sports Medicine (AOSSM) criteria [27]. The HAES quantifies the duration, in hours, of 4 levels of activity ranging from very inactive (lying down, napping), somewhat inactive (sitting, reading, watching television, playing video games), somewhat active (walking, light chores), to very active (running, bicycling, activities leading to sweating or breathing hard) over a complete waking day [28]. The cut-off of 180 min in a given category was used according to prior sport specialization criteria and plans for the definitive trial [29]. The HAES is designed for administration in the pediatric population and has been shown to be both a valid and reliable form of quantifying levels of physical activity [28]. Participants classified as “highly active” included those that scored “very active” on the HAES and reported playing at least one sport. Using the AOSSM criteria, a sport specialist was defined as someone who participated in intensive (i.e., HAES = “very active”) training and/or competition in one sport greater than 8 months per year [27]. Study groups were defined at the completion of follow-up given participant activity levels were expected to change over time.
Objectives and hypotheses
The primary outcome was to determine the feasibility of a large-scale prospective cohort study, based on the following thresholds established a priori: (1) 50 subjects recruited within 3 months, (2) 45 of 50 participants (90%) achieving full follow-up at 2 years, and (3) completion of at least 90% of all outcome measures including the Hip Outcome Score (HOS), Pediatric Quality of Life (PedsQL) questionnaire, hip MRI, and range of motion (ROM).
Secondary outcomes included the incidence of radiographic FAI as determined by a blinded, independent evaluation of an MRI of the dominant hip (planned primary outcome of the definitive study), ROM, hip function evaluated using the HOS, and health-related quality of life (HRQL) evaluated using the PedsQL questionnaire at 24 months. An additional secondary objective was to determine if the presence of FAI morphology at baseline was associated with differences in participant-reported hip function and HRQL at 24 months. We hypothesized that (1) participants engaging in specialized, high intensity sport activity would have a higher prevalence of FAI morphology diagnosed through MRI compared to non-sport specialists at varying activity levels in the same age group at 2 years; (2) participants diagnosed with any type of FAI (at baseline) would have decreased hip function and HRQL at 2 years compared to those without; and (3) participants with symptomatic FAI would have lower functional and HRQL scores at 2 years compared to participants that did not have FAI morphology or were asymptomatic.
Outcomes
Clinical assessments at baseline and 2 years consisted of a hip ROM evaluation and response to both anterior and posterior hip impingement tests, as well as log roll test. We used a non-contrast 3D-volumetric interpolated breath-hold examination (VIBE) sequence for each MRI [30]. An independent, blinded adjudicator (a senior radiologist with more than 20 years of experience) evaluated all MRIs for FAI morphology using the criteria shown in Table 1. The scores for the individual domains for the HOS (ADL and sports subscale) and PedsQL (physical functioning, emotional functioning, social functioning, school functioning, psychosocial health summary) are presented [31,32,33,34,35].
Statistical analysis
Given this was a pilot study with a small sample size, the analyses were exploratory and descriptive. We present the data using means, mean difference (MD), and proportions with standard deviations and 95% confidence intervals (CI). All outcomes presented are based on 24-month data. All analyses were conducted using SAS version 9.4 (Cary, NC).
Results
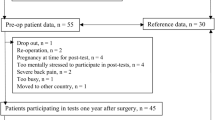
Of the 54 participants enrolled, there were 36 included in the final analysis, 66.7% of which were male and the mean age was 13.61 (± 0.81) years. Eighteen participants were excluded: 7 had incomplete data sets, 6 had a closed physeal plate identified at the baseline MRI, and 5 were lost to follow-up. The 6 participants with a closed physeal plate were all female and ranged in age between 12.9 and 14.5 years and activity level from none (2/6), to light (1/6), to vigorous (3/6) at the baseline evaluation. The majority of participants had a normal BMI, no comorbidities, and reported their baseline sport activity as “vigorous.” On average, participants played one or more sports for 3.53 (± 2.06) hours per week. The most commonly played sports among the participants in this study included soccer (44.4%), hockey (25.0%), and basketball (16.7%) (Table 2). Based on the AOSSM criteria, a total of 19 participants were categorized as sport specialists and 17 as non-sport specialists (Table 2). When grouped according to activity level, there were 32 participants classified as highly active who played at least one sport and 4 as low activity who played minimal or no sports (Additional Table 1).
Feasibility measures
The investigators recruited 54 participants in 12 months and of those 48 eligible (i.e., with open physeal plates) the loss to follow-up rate was 10.4% (5/48) with complete outcomes data, including study questionnaires and MRIs, collected for 75% (36/48) of participants at 2 years. Of the 5 participants lost to follow-up, 2 could not be contacted and 3 refused to return for their 2-year MRI due to fears/restrictions related to coming into the hospital during the COVID-19 pandemic.
Other outcome measures
At baseline, those classified as highly active and played at least one organized sport had a higher incidence of asymptomatic radiographic FAI markers (from 6/32, 18.8% at baseline to 19/32, 59.4% at 24 months) compared to those classified in the low activity, with or without playing a sport group (1/4, 25% maintained at baseline and 24 months). The incidence of radiographic FAI markers was higher among sport specialists (12/19, 63.2%) compared to non-sport specialists (8/17, 47.1%) at 24 months. There was one participant with pincer-type FAI in the high activity/sport specialist group while all other cases were cam-type. All participants with FAI morphology were asymptomatic.
Mean hip ROM measures were slightly reduced from baseline to 2 years across all activity levels (Table 3). The MRI measurements revealed there was a slightly higher proportion of labral tears in the highly active group (57%, 16/28) compared to the low activity group (50%, 1/2) at 24 months. Overall, among participants with radiographic FAI markers at 24 months, 43.3% (13/30) had a labral tear. Partial thickness cartilage lesions were present in 25% of participants 24 months (Table 4).
The HOS and PedsQL scores were slightly higher (better) among those that were highly active and played a sport compared to those who did not at 2 years [MD (95% CI): HOS-ADL subscale 4.56 (− 7.57, 16.70); HOS-Sport subscale 5.97 (− 6.91, 18.84); PedsQL Physical 7.42 (− 0.79, 15.64); PedsQL Emotional 11.87 (− 6.74, 30.49); PedsQL Social 5.94 (− 2.86, 14.74); PedsQL School 1.72 (− 17.32, 20.76); PedsQL Psychosocial 6.51 (− 5.75, 18.77)] (Additional Table 2). There was no difference in HOS and PedsQL scores at 2 years between participants with FAI morphology at baseline compared to those without (Additional Table 3).
Discussion
With respect to the feasibility objectives, this pilot study required a longer period of recruitment (12 months vs. target of 3 months), had a lower than expected outcomes completion rate (75% vs. target of 90%), but did meet the follow-up target of 90% for at least some 2-year data (based on the 48 participants that were eligible for the study). The available pilot data suggest that adolescents engaged in higher levels of activity in sports or who specialize in one sport may have a higher risk of developing asymptomatic FAI morphology (predominantly cam-type) at 2 years. Those in the high activity/sport specialist groups also reported higher HOS and PedsQL scores across all domains when compared to the low activity/non-sport specialist groups at 2 years. Where all participants with FAI morphology were asymptomatic, there was no difference in hip function (HOS) or HRQL (PedsQL) between those with FAI morphology at baseline compared to those without at 2 years.
Although not all of the feasibility objectives were met for this pilot study, it helped to inform important protocol changes for the definitive study which is currently underway. To address recruitment and enhance external validity, we involved additional international sites in the definitive study and implemented several important recruitment strategies including posting study flyers at each participating institution, distributing study flyers online and on paper to grades in the eligible age range at schools in the regions of the recruiting institutions, and having the co-investigators reach out to community coaches and competitive sport organizations and clubs. To promote complete data collection and improve participant retention, we added interim follow-up visits every 3 months and introduced an activity log and wrist-worn tracker to improve the collection of physical activity data over the 2-year period. The definitive study protocol has been published [29].
Although limited by a small sample size, the pilot study found that around 60% of high activity/sport specialist participants had radiographic FAI morphology at 24 months. Where approximately 20% had evidence of FAI at baseline, this a noteworthy increase as no participants in the low activity level group developed FAI. These results are similar to many cross-sectional studies that have found the prevalence of cam deformity in high impact sports to be between 26 and 89% [17, 20,21,22, 36, 37]. A recent longitudinal MRI study followed 25 high level (3 to 5 sessions per week) male ice hockey players aged 11 to 13 years old for 3 years and found that 50% of their cohort presented with FAI at the end of the study and that cam morphology appeared to develop at the beginning of the final growth spurt of the femoral head [18]. They also noted that four participants still had open physes at final follow-up, which could underestimate the final number of participants developing FAI [18]. A study from Agricola et al. followed 89 preprofessional soccer players for 2 years and found that boys aged 12 or 13 years old had a significant increase in presence of a flattened head and neck junction going from 13.6% at baseline to 50% at 24 months [38]. A study from Tak et al. found that football players who started playing before the age 12 at a high frequency had a statistically significant higher prevalence of cam deformities compared to players who started after 12 and played at lower frequency (64% vs 40%) [37].
A slightly higher percentage of participants in the highly active group presented with asymptomatic labral tears at 24 months (57% vs. 50%). It is now well accepted that cam-type FAI is a risk factor for labral tears [39]. A recent MRI study looking at young football players (mean age 26 years) found an association between cam morphology size and risk of chondrolabral damage. Interestingly, the relationship was similar in symptomatic and asymptomatic patients [40]. With chondrolabral damage being a continuum, it is likely too early for participants in this study to show any important cartilage damage that may cause hip pain [39].
While there may be an increased risk in developing FAI if playing high intensity sports in adolescence, there still appear to be benefits to quality of life and hip function. A survey and focus group study of University students and community members found that physical activity was a positive contributor to all aspects of HRQL and that emotional benefit was reported as equally important as physical health in younger participants and more important than physical health among community members [41]. Systematic reviews evaluating physical activity interventions or the impact of sedentary behavior have found that a higher prevalence of physical activity is associated with the psychological well-being of children and adolescents [42]. Interestingly, participants in the highly active group reported better hip function (according to the HOS scores) than their less active counterparts, despite having a higher proportion of radiographic FAI at 24 months. This is likely due to many factors including the fact that they were asymptomatic, had stronger hips due to increased activity, and potentially better access to training and rehabilitation. Ultimately, there has to be a balance between protecting the hip from developing FAI, while still promoting a high level of physical activity in adolescence given its other benefits.
This study had some limitations. Because this was a pilot to help determine feasibility and generate hypotheses, we were unable to make any definitive conclusions at this time due to the small sample size. We did not meet all of our pre-defined feasibility criteria but were able to adjust the protocol to help ensure the success of the definitive prospective cohort study [29]. In addition, we expect a higher follow-up rate as the definitive study continues post-COVID-19 pandemic.
Conclusion
Our pilot study demonstrated some feasibility for a larger scale, definitive cohort study. The preliminary descriptive data suggest that adolescents engaged in higher levels of activity in sports may have a higher risk of developing asymptomatic hip deformities related to FAI, but also better HRQL over the 2-year study period. The results of this pilot were used to refine the protocol for the ongoing definitive PREVIEW study (N = 200, NCT03891563).
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and its additional files.
Abbreviations
- ADLs:
-
Activities of daily living
- AOSSM:
-
American Orthopaedic Society for Sports Medicine
- CI:
-
Confidence intervals
- FAI:
-
Femoroacetabular impingement
- FHN:
-
Femoral head and neck
- HAES:
-
Habitual Activity Estimation Scale
- HOS:
-
Hip Outcome Score
- HRQL:
-
Health-related quality of life
- MD:
-
Mean difference
- MRI:
-
Magnetic resonance imaging
- OA:
-
Osteoarthritis
- PedsQL:
-
Pediatric Quality of Life questionnaire
- VIBE:
-
Volumetric interpolated breath-hold examination
References
Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013;72(6):918–23.
Kowalczuk M, Yeung M, Simunovic N, Ayeni OR. Does femoroacetabular impingement contribute to the development of hip osteoarthritis? A systematic review. Sports Med Arthrosc Rev. 2015;23(4):174–9.
Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg (Br). 2005;87(7):1012–8.
Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:263–9.
Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat R. 2004;429:170–7.
Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat R. 2004;418:61–6.
Kaya M, Suzuki T, Emori M, Yamashita T. Hip morphology influences the pattern of articular cartilage damage. Knee Surg Sport Tr A. 2016;24(6):2016–23.
Frank JM, Harris JD, Erickson BJ, Slikker W, Bush-Joseph CA, Salata MJ, et al. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy. 2015;31(6):1199–204.
Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P. The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol. 2008;49(4):436–41.
Kapron AL, Anderson AE, Aoki SK, Phillips LG, Petron DJ, Toth R, et al. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS Exhibit Selection. J Bone Joint Surg Am. 2011;93(19):e111(1-10).
Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92(14):2436–44.
Philippon MJ, Patterson DC, Briggs KK. Hip arthroscopy and femoroacetabular impingement in the pediatric patient. J Pediatr Orthop. 2013;33 Suppl 1:S126–30.
Pathy R, Sink EL. Femoroacetabular impingement in children and adolescents. Curr Opin Pediatr. 2016;28(1):68–78.
Packer JD, Safran MR. The etiology of primary femoroacetabular impingement: genetics or acquired deformity? J Hip Preserv Surg. 2015;2(3):249–57.
Carsen S, Moroz PJ, Rakhra K, Ward LM, Dunlap H, Hay JA, et al. The Otto Aufranc Award. On the etiology of the cam deformity: a cross-sectional pediatric MRI study. Clin Orthop Relat R. 2014;472(2):430–6.
Stull JD, Philippon MJ, LaPrade RF. “At-risk” positioning and hip biomechanics of the Peewee ice hockey sprint start. Am J Sports Med. 2011;39 Suppl:29S–35S.
Siebenrock KA, Behning A, Mamisch TC, Schwab JM. Growth plate alteration precedes cam-type deformity in elite basketball players. Clin Orthop Relat R. 2013;471(4):1084–91.
Hanke MS, Schmaranzer F, Steppacher SD, Reichenbach S, Werlen SF, Siebenrock KA. A cam morphology develops in the early phase of the final growth spurt in adolescent ice hockey players: results of a prospective MRI-based study. Clin Orthop Relat R. 2021;479(5):906–18.
Frank JS, Gambacorta PL, Eisner EA. Hip pathology in the adolescent athlete. J Am Acad of Orthop Surg. 2013;21(11):665–74.
Philippon MJ, Ho CP, Briggs KK, Stull J, LaPrade RF. Prevalence of increased alpha angles as a measure of cam-type femoroacetabular impingement in youth ice hockey players. Am J Sports Med. 2013;41(6):1357–62.
Agricola R, Bessems JH, Ginai AZ, Heijboer MP, van der Heijden RA, Verhaar JA, et al. The development of cam-type deformity in adolescent and young male soccer players. Am J Sports Med. 2012;40(5):1099–106.
Siebenrock KA, Kaschka I, Frauchiger L, Werlen S, Schwab JM. Prevalence of cam-type deformity and hip pain in elite ice hockey players before and after the end of growth. Am J Sports Med. 2013;41(10):2308–13.
Myer GD, Jayanthi N, Difiori JP, Faigenbaum AD, Kiefer AW, Logerstedt D, et al. Sport Specialization, Part I: Does early sports specialization increase negative outcomes and reduce the opportunity for success in young athletes? Sports Health. 2015;7(5):437–42.
Myer GD, Jayanthi N, DiFiori JP, Faigenbaum AD, Kiefer AW, Logerstedt D, et al. Sports Specialization, Part II: Alternative solutions to early sport specialization in youth athletes. Sports Health. 2016;8(1):65–73.
Feeley BT, Agel J, LaPrade RF. When is it too early for single sport specialization? Am J Sports Med. 2016;44(1):234–41.
Siebenrock KA. Editor's spotlight/take 5: Growth plate alteration precedes cam-type deformity in elite basketball players (DOI 10.1007/s11999-012-2740-6). Interview by Seth S. Leopold. Clin Orthop Relat R. 2013;471(4):1081–3.
LaPrade RF, Agel J, Baker J, Brenner JS, Cordasco FA, Côté J, et al. AOSSM Early Sport Specialization Consensus Statement. Orthop J Sports Med. 2016;4(4):2325967116644241.
Hay JA, B. University, Cairney J. Development of the habitual activity estimation scale for clinical research: a systematic approach. Pediatr Exerc Sci. 2006;18(2):193–202.
Öhlin A, Simunovic N, Duong A, Ayeni OR. Protocol for a multicenter prospective cohort study evaluating sport activity and development of femoroacetabular impingement in the adolescent hip. BMC Musculoskelet Disord. 2020;21(1):221.
Li AE, Jawetz ST, Greditzer HG, Burge AJ, Nawabi DH, Potter HG. MRI for the preoperative evaluation of femoroacetabular impingement. Insights Imaging. 2016;7(2):187–98.
d'Entremont AG, Cooper AP, Johari A, Mulpuri K. What clinimetric evidence exists for using hip-specific patient-reported outcome measures in pediatric hip impingement? Clin Orthop Relat R. 2015;473(4):1361–7.
Roposch A. CORR Insights ®: What clinimetric evidence exists for using hip-specific patient-reported outcome measures in pediatric hip impingement? Clin Orthop Relat R. 2015;473(4):1368–9.
Lodhia P, Slobogean GP, Noonan VK, Gilbart MK. Patient-reported outcome instruments for femoroacetabular impingement and hip labral pathology: a systematic review of the clinimetric evidence. Arthroscopy. 2011;27(2):279–86.
Thorborg K, Roos EM, Bartels EM, Petersen J, Hölmich P. Validity, reliability and responsiveness of patient-reported outcome questionnaires when assessing hip and groin disability: a systematic review. Br J Sports Med. 2010;44(16):1186–96.
Hullmann SE, Ryan JL, Ramsey RR, Chaney JM, Mullins LL. Measures of general pediatric quality of life: Child Health Questionnaire (CHQ), DISABKIDS Chronic Generic Measure (DCGM), KINDL-R, Pediatric Quality of Life Inventory (PedsQL) 4.0 Generic Core Scales, and Quality of My Life Questionnaire (QoML). Arthritis Care Res. 2011;63 Suppl 11:S420–30.
Nepple JJ, Brophy RH, Matava MJ, Wright RW, Clohisy JC. Radiographic findings of femoroacetabular impingement in National Football League Combine athletes undergoing radiographs for previous hip or groin pain. Arthroscopy. 2012;28(10):1396–403.
Tak I, Weir A, Langhout R, Waarsing JH, Stubbe J, Kerkhoffs G, et al. The relationship between the frequency of football practice during skeletal growth and the presence of a cam deformity in adult elite football players. Br J Sports Med. 2015;49(9):630–4.
Agricola R, Heijboer MP, Ginai AZ, Roels P, Zadpoor AA, Verhaar JA, et al. A cam deformity is gradually acquired during skeletal maturation in adolescent and young male soccer players: a prospective study with minimum 2-year follow-up. Am J Sports Med. 2014;42(4):798–806.
Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat R. 2003;417:112–20.
Heerey J, Kemp J, Agricola R, Srinivasan R, Smith A, Pizzari T, et al. Cam morphology is associated with MRI-defined cartilage defects and labral tears: a case-control study of 237 young adult football players with and without hip and groin pain. BMJ Open Sport Exerc Med. 2021;7(4):e001199.
Gill DL, Hammond CC, Reifsteck EJ, Jehu CM, Williams RA, Adams MM, et al. Physical activity and quality of life. J Prev Med Public Health. 2013;46 Suppl 1:S28–34.
Rodriguez-Ayllon M, Cadenas-Sánchez C, Estévez-López F, Muñoz NE, Mora-Gonzalez J, Migueles JH, et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med. 2019;49(9):1383–410.
Acknowledgements
PREVIEW Pilot Investigators (authorship)
Writing committee: Pierre-Olivier Jean MD, FRCSC (McMaster University), Nicole Simunovic MSc (McMaster University), Andrew Duong MSc (McMaster University), Gary Foster PhD (McMaster University), Olufemi R. Ayeni MD, PhD, FRCSC (McMaster University)
Steering committee: Olufemi R. Ayeni MD, PhD, FRCSC (chair, McMaster University), Volker Musahl MD (University of Pittsburgh), Yan Sim MD (McMaster University), Lehana Thabane PhD (McMaster University)
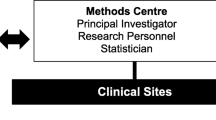
Methods Centre: Olufemi R. Ayeni MD, PhD, FRCSC (principal investigator); Nicole Simunovic MSc (research manager); Andrew Duong MSc, Callum MacLeay, Matthew Skelly MSc, Ajay Shanmugaraj BSc, Dana Ghanem BSc (project management); Diane Heels-Ansdell MSc (statistical analysis); Lisa Buckingham BSc (data management) (McMaster University)
Adjudication: Vasco V. Mascarenhas MD, MBA, PhD (Hospital da Luz, Lisbon, Portugal)
Participating clinical sites
Canada
McMaster University Medical Centre (Hamilton, ON) – Olufemi R. Ayeni MD, PhD, FRCSC; Andrew Duong MSc; Nicole Simunovic MSc; Callum MacLeay, BSc, Dana Ghanem BSc, Andrea Ponniah BSc CHU de Québec-Université Laval (Quebec City, QC) – Etienne L. Belzile MD, FRCSC; Sylvie Turmel RN
International
Erasmus University Medical Centre Rotterdam (Rotterdam, The Netherlands) – Rintje Agricola MD, PhD
Kyungpook National University Hospital (Daegu, South Korea) – Seung-Hoon Baek MD, PhD; Hoseok Lee MD, PhD; Ae-Sun Chang RN
Funding
Research grants for this trial were received from the Arthroscopy Association of North America, ConMed Research Grant, McMaster Surgical Associates, and the Canadian Institutes of Health Research (CEBA-223174). None of the previously mentioned funding bodies contributed to the design of the study, collection, analysis, and interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
The Methods Centre at McMaster University (ORA, NS, AD, CM, MS AS, DG, DHA, LB) coordinated the trial. The Methods Centre was responsible for programming and maintaining the study database, data validation, data analyses, and study-center coordination. The Steering Committee (ORA, VM, YS, LT) designed the trial and some members assisted with developing the statistical analysis plan and vouch for the completeness and accuracy of the data and analyses. POJ and NS wrote the first draft of the manuscript and the writing committee made revisions. The independent adjudicator (VVM) evaluated all imaging for the study. The participating clinical sites (ORA, AD, NS, CM, DG, AP, ELB, ST, RA, SHB, HL, ASC) were responsible for local participant recruitment and follow-up. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for the study was granted by Hamilton Integrated Research Ethics Board (HIREB #2574), and informed assent and consent was obtained from all participants and their guardians.
Consent for publication
Not applicable.
Competing interests
ORA declares a non-financial conflict of interest due to association with the Speakers Bureau for Conmed and Stryker Canada. LT was the Senior Statistician for this study and is also the Co-Editor in Chief of Pilot and Feasibility Studies.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Additional Table 1.
Participant demographics by activity level. Additional Table 2. Hip function and health-related quality of life outcomes by activity level. Additional Table 3. Hip function and health-related quality of life outcomes by baseline FAI.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ayeni, O.R., PREVIEW Pilot Investigators. Prospective evaluation of sport activity and the development of femoroacetabular impingement in the adolescent hip (PREVIEW): results of the pilot study. Pilot Feasibility Stud 8, 201 (2022). https://doi.org/10.1186/s40814-022-01164-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-022-01164-3