Abstract
Background
Excess weight and unhealthy behaviours (e.g. sedentariness, high alcohol) are common amongst women including those attending breast screening. These factors increase the risk of breast cancer and other diseases. We tested the feasibility and acceptability of a weight loss/behaviour change programme framed to reduce breast cancer risk (breast cancer prevention programme, BCPP) compared to one framed to reduce risk of breast cancer, cardiovascular disease (CVD) and diabetes (T2D) (multiple disease prevention programme, MDPP).
Methods
Women aged 47-73 years with overweight or obesity (n = 1356) in the NHS Breast Screening Programme (NHSBSP) were randomised (1:2) to be invited to join a BCPP or a MDPP. The BCPP included personalised information on breast cancer risk and a web and phone weight loss/behaviour change intervention. The MDPP also included an NHS Health Check (lipids, blood pressure, HbA1c and personalised feedback for risk of CVD [QRISK2] and T2D [QDiabetes and HbA1c]). Primary outcomes were uptake and retention and other feasibility outcomes which include intervention fidelity and prevalence of high CVD and T2D risk. Secondary outcomes included change in weight.
Results
The BCPP and MDPP had comparable rates of uptake: 45/508 (9%) vs. 81/848 (10%) and 12-month retention; 33/45 (73%) vs. 53/81 (65%). Both programmes had a high fidelity of delivery with receipt of mean (95% CI) 90 (88-98% of scheduled calls, 91 (86-95%) of scheduled e-mails and 89 (76-102) website entries per woman over the 12-month period. The MDPP identified 15% of women with a previously unknown 10-year CVD QRISK2 of ≥ 10% and 56% with 10-year Qdiabetes risk of ≥ 10%. Both groups experienced good comparable weight loss: BCPP 26/45 (58%) and MDPP 46/81 (57%) with greater than 5% weight loss at 12 months using baseline observation carried forward imputation.
Conclusions
Both programmes appeared feasible. The MDPP identified previously unknown CVD and T2D risk factors but does not appear to increase engagement with behaviour change beyond a standard BCPP amongst women attending breast screening. A future definitive effectiveness trial of BCPP is supported by acceptable uptake and retention, and good weight loss.
Trial registration
ISRCTN91372184, registered 28 September 2014.
Similar content being viewed by others
Uncertainties regarding feasibility that existed prior to this study
Can we recruit and engage breast screening attendees to a web and phone weight loss/behaviour change breast cancer or multiple disease prevention programmes?
What proportion of women have previously unidentified high risks of CVD and T2D?
The fidelity of delivery and patient satisfaction with the programmes
Are there any associated harms of the programmes, e.g. increased anxiety?
Which of the programmes should be tested further in a definitive large scale RCT within the NHSBSP?
Key feasibility findings from this study
The MDPP and BCPP web/phone programmes appeared feasible.
The MDPP identified previously unknown CVD and T2D risk factors but does not appear to increase engagement with behaviour change beyond a standard BCPP
No evidence of harms.
Implications of the findings on the design of the main study
A future definitive effectiveness trial of BCPP is supported by acceptable uptake and retention, and good weight loss.
Background
Women in the UK aged between 50 and 70 years are invited for breast screening as part of the National Health Service Breast Screening Programme (NHSBSP). In common with women of this age in the general population, many attendees have overweight or obesity (62%) [1], sedentariness (80%) [1], high alcohol intakes (11.5%) [1], sub-optimal diets (80%) [2] and smoke (16%) [3]. It is estimated that these factors combined may be responsible for 30% of breast cancers [4] and significant proportions of other multifactorial conditions including 70% of CVD [5], and 90% of T2D [6]. Unhealthy behaviours and the associated disease risks are not currently addressed within the NHSBSP.
There are currently moves to introduce breast cancer (BC) risk assessment to the NHSBSP in order to identify higher risk women for chemoprevention and risk adapted breast screening [7,8,9,10]. The Predicting Risk of Cancer at Screening (PROCAS) study reported up to 21% of 57,902 in the Greater Manchester NHSBSP are at either high or above average risk of BC (10-year risk of ≥ 5%), 50% are at average risk (10-year risk of 2-4.9%) and 29% are at low risk (10-year risk < 2%) [11].
Women of breast screening age in the UK are also eligible for assessment of CVD and T2D risk assessment as part of the NHS Health Check. Current coverage and outcomes for this programme are sub-optimal as it is mainly opportunistic [12]. Public Health England estimates that only 49% of adults with raised cholesterol and 57% with hypertension have been identified. Furthermore, low proportions of those with raised levels currently receive appropriate statin (35%) or anti-hypertensive (49%) medications [13]. The programme is currently being reviewed with an aim to improve delivery and outcomes of the checks [14]. Offering CVD and T2D risk assessment and a behaviour change programme at breast screening could provide systematic access to CVD and T2D care pathways due to high NHSBSP coverage and thus potentially better outcomes.
The PROCAS Lifestyle study reported here aimed to explore the feasibility of BCPP and MDPP for women with overweight/obesity following receipt of BC risk estimates as part of risk stratified screening. A sample of women with overweight/obesity participating in the PROCAS study were randomised to receive an invitation to join a standard web and phone Breast Cancer Prevention Programme (BCPP) which reminded women of their personal risk of BC or a Multiple Disease Prevention Programme (MDPP) which additionally included an NHS Health Check to assess lipids, blood pressure and Hba1c; provided personalised risk feedback for CVD, T2D and emphasised the links between health behaviours and dementia. The programmes asked women to follow either a daily or intermittent (5:2) energy restricted Mediterranean diet. Both approaches have found to be effective in our previous weight loss studies amongst high risk women [15], and are equally effective for long-term weight loss success in a variety of populations [16].
We previously reported that higher BC risk predicted uptake retention and weight loss success across both BCPP and MDPP [17]. We now report on the main trial aim, which is to assess the feasibility of the intervention and trial methods. The primary objectives were uptake and retention. Other feasibility objectives included predictors of retention, completeness of data collection, the need for the programmes (the number of participants who have previously had an NHS Health Check, numbers at high risk of CVD and T2D and evidence of uptake equity across demographic groups), fidelity of intervention delivery, participant satisfaction and any associated harms of the programmes, e.g. anxiety and health status. We also report preliminary efficacy data for change in weight, which is the planned primary outcome for a subsequent definitive trial, and other lifestyle behaviours.
A final objective was to determine which of these programmes should be tested further in a definitive large scale RCT within the NHSBSP.
Method
Study design
We conducted a single centre prospective two arm randomised trial (1:2) of BCPP vs. MDPP amongst women attending the NHSBSP, and who had participated in the PROCAS study. Recruitment was between November 2014 and October 2015. This period was a median (range) 55 (5-72) months after completing BC risk assessments and 6.5 (0-63) months after receiving personalised BC risk feedback as part of the PROCAS study. The long lag between risk assessment and feedback was because of the need to validate the Tyrer-Cuzick risk assessment model amongst women attending the NHSBSP. All trial procedures were undertaken at the Prevent Breast Cancer Research Unit at Wythenshawe Hospital, Manchester University NHS Foundation Trust.
Patient and public involvement
The trial design and participant resources and pathway were designed in collaboration with a panel of women attending breast screening. Four members of this panel were part of the trial management group.
Recruitment and randomisation
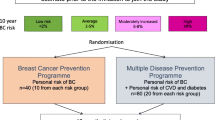
The study included women with overweight/obesity (BMI ≥ 25 kg/m2) aged 47–73 years who had been identified and informed they were at high (10-year risk ≥ 8%), above average (5-7.9%), average (2-4.9%) or low-risk (< 2%) of BC as described previously [1]. The personalised estimate of their risk of BC had been derived using the Tyrer-Cuzick model (version-8 which includes family history, hormonal risk factors, BMI and visually assessed mammographic density [11]). Women were randomised 1:2 to receive a mailed invitation to either the BCPP or MDPP programmes. We included a larger MDPP group to assess any issues that may arise when participants are given this novel programme. Randomisation to the two different invitations allowed us to assess uptake separately to the two programmes (Fig. 1). Interested women were asked to check their eligibility on the trial website, or to ring the trial office if they did not have immediate access to the internet. Women were excluded if they did not have access to a phone or the internet; had a previous diagnosis of cancer, T2D or CVD; were currently prescribed statins; had a major physical or psychiatric condition which made them unsuitable for a home based diet and physical activity (PA) programme or were current users of HRT since weight only affects risk of BC amongst non-HRT users [18]. The invitation letter included an opt-out slip to indicate reasons they were not eligible or not interested.
The sample size of 40 in the BCPP group allowed us to estimate an uptake of 10% (CI +/−9.5%) and a retention rate of 60% (CI +/−15.0%). We recruited double the number of participants in the novel MDPP group (n = 80). The final sample size of 120 (40 BCPP and 80 MDPP) included 10 women from each BC risk group to the BCPP and 20 from each BC risk group to the MDPP.
Participant randomisation was undertaken independently from the research team by an independent member of the Department of Statistics at Manchester University NHS Foundation Trust to ensure allocation concealment using nQuery Advisor 7.0. The first batch used a 1:2 randomisation of BCPP to MDPP across the four BC risk groups. Subsequent randomisations were adaptive to the response rate of each risk category in the two groups until 45 women were randomised to the BCPP group and 81 to the MDPP group.
The BCPP and MDPP programmes
The programmes are described in Table 1. Both programmes were delivered by research dietitians who had undergone training on communicating personalised risk of BC, CVD, T2D and dementia and the lifestyle prevention of these conditions. Both programmes reminded women of their personal BC risk. In addition, the MDPP provided personalised risk of developing CVD (10-year and lifetime risk and heart age from QRISK2 [19]) and T2D (10 year risk from QDiabetes [20] and measured HbA1c).
Both programmes promoted weight loss of ≥ 5% and communicated how weight loss and health behaviour change could reduce risk of breast cancer [21, 22], type 2 diabetes [23] and CVD [24]. This was presented as a gain-framed message to increase response efficacy [30].
The programmes were supported by a trial website which encouraged women to self-monitor and record their weight, diet (completion of restricted days in the 5:2 diet and actual food and drink intake) and PA (both cardiovascular and resistance). It hosted weekly menu plans, recipes, information about BC, CVD, T2D and dementia, tips for planning and managing emotional eating, online videos of the recommended exercises (Physiotec, Canada) and a monthly newsletter to maintain engagement. Women received tailored feedback on their self-reported behaviours from their allocated trial dietitian in scheduled phone calls (weeks 1, 4, 8) and weekly personalised e-mails for 6 months. They were invited to enter an optional continued weight loss/weight maintenance period between 6- and 12-month women when they received automated monthly e-mails in response to website entries.
Communicating personalised risk information without increasing self-efficacy or encouraging self-regulation is not likely to produce changes in behaviour [31]. Given this, both programmes included key behaviour change techniques as recommended in the UK NICE behaviour change guidance, including goal setting, planning, relapse prevention, self-monitoring and encouraging individuals to identify sources of social support for changing behaviours [32].
Primary outcome measures
Uptake and retention
For each programme, we recorded the number of women who were invited and consented to join the study, and who were not interested or not eligible to take part and the reasons for this. Also, retention to the programmes at 3, 6 and 12 months.
Predictors of retention
Within the MDPP, we assessed whether being identified at different levels of CVD and T2D disease risk was associated with disengagement from behaviour change, evidenced by differences in withdrawal.
Completeness of weight and self-reported measures
We recorded the number of women with weight and body fat measures and who had completed self-report measures of physical activity (IPAQ) [33], alcohol intake and harms (AUDIT) [28], diet (7-day food diary), smoking status, health status (EQ-5D-5L) [34] and perceived self-rated anxiety (state trait anxiety) [35] during the study.
Need for the programmes
We assessed the prevalence of previously unknown raised CVD and T2D risk identified in the MDPP programme. Also, demographics of women recruited to the programmes including ethnicity and socioeconomic status using index of multiple deprivation (IMD) quintiles [36].
Fidelity of delivery and engagement to the programmes
We assessed the numbers of scheduled calls and e-mails received, engagement with the web site and the amount of dietitian time that was used to deliver the programmes. Also, the numbers of women in both groups referred to NHS behaviour change services (i.e. exercise on referral, alcohol and smoking cessation services) or commenced on statins or blood pressure medications.
Participant satisfaction
We collated anonymised 12-month participant questionnaires which rated satisfaction with the overall programme, study visits and the trial website. This included free text suggestions for how the programmes could be improved. A specific website feedback questionnaire was completed at 3 and 6 months to include feedback from women who might leave the programme before 12 months.
Potential harms of the programmes
Potential harms of both programmes were assessed in terms of serious or unexpected adverse events and changes in perceived self-rated anxiety (state trait anxiety) [35] and health status (EQ-5D-5L) [34].
Secondary outcomes
Weight loss and health-related behaviour change
We assessed change in weight and body fat (Tanita MC-180MA, Tanita Europe, Amsterdam, The Netherlands) and the number and percentage of women losing 5% of weight or greater at 12 months. Also, self-reported PA (IPAQ) [33], alcohol harms and intake (AUDIT [28]), saturated fat intake (7-day food diary analysed using Wisp version 3 (Tinuviel Software, Anglesey, Wales) [37]) and smoking status in both groups at 3 and 6 months.
Analysis
Descriptive statistics of uptake and retention, fidelity of the intervention, participant satisfaction and changes in weight and health behaviours in the MDPP and BCPP groups were undertaken. Multivariable logistic regression was used to assess the association between estimated level of CVD and T2D risk and the likelihood of withdrawal at 12 months within the MDPP group. This was assessed in terms of 10-year CVD QRISK2, heart age compared to actual age, having a first degree relative with CVD, 10-year QDiabetes and having a first degree relative with diabetes. A priori confounding variables included BC risk (high, above average, average and low), index of multiple deprivation (IMD quintiles; 1, 2 and 3-5) [36], smoking status (never, ex-smoker and current smoker), age and BMI at baseline.
Baseline observation carried forward (BOCF) values are reported for changes in weight (% and kg), body fat (kg), alcohol intake and PA. This provides an estimate of intention to treat assuming that people who leave an intervention are likely to revert to their baseline weight and behaviours. Completers only analysis was undertaken for state anxiety and self-rated health status.
Given the relatively large numbers in this feasibility trial, we undertook exploratory formal statistics to assess comparisons of changes in these parameters relative to baseline between the BCPP and MDPP conditions. The findings of these are reported as an indication of the effects of the two programmes with the caveat; there is multiple testing of secondary outcomes and the study is not necessarily powered to show differences.
P < 0.05 was considered statistically significant for all analyses. All statistical analyses were conducted using SPSS version 23 (IBM Corp., Armonk, NY, USA), R version 3.5.1 and Stata Statistical Software: Release 16.
Results
Recruitment and retention to the programmes
Uptake to the study was comparable with invitations to both the BCPP and MDPP (45/508 9%; vs. 81/848 10%, p = 0.7) (Fig. 2). An additional 57 women invited to the BCPP (11%) and 135 invited to the MDPP (16%) were interested in joining but were not eligible. This was mainly due to existing health problems such as previous CVD, cancer and raised cholesterol (7.1% BCPP, 12.0% MDPP). Other reasons for declining included lack of internet access (1.4% BCPP, 0.8% MDPP) and current use of HRT (1.0% BCPP, 1.2% MDPP). A further 8 women invited to the BCPP (2%) and 7 invited to the MDPP (1%) wished to enter the study but responded after recruitment was complete.
An additional 130 women (10%) invited to both programmes returned a response slip to say they were not interested in taking part. The most common reasons cited were lack of time (28%), issues travelling to the centre for trial appointments (18%), family illness or caring duties (12%). Uptake to both programmes was greater in women at high and above average BC risk compared to average and low risk as reported previously (Table 2) [17].
Five women in the BCPP (11%) and 16 women in the MDPP (20%) left the programme during the 6 months of phone and e-mail dietitian support (Fig. 2). A further 6 BCPP (14%) and 12 MDPP (15%) women left the programme during the automated e-mail support period between 6 and 12 months. Of the total women who left the programmes in the 12-month period, i.e. 11 (25%) in the BCPP and 28 (35%) in the MDPP groups, 7 BCPP (16%) and 20 MDPP (25%) asked to withdraw and a further 4 BCPP (9%) and 8 MDPP (10%) lost contact. The most commonly cited reasons for withdrawal included personal or family illness (n = 11, 43%), too busy (n = 5, 17%), and not able to adhere to the programme (n = 5, 17%) (Fig. 2).
Predictors of retention to the BCPP and MDPP
Retention appeared to be greater amongst women at higher risk BC risk in the BCPP group, but was more variable across BC risk categories for the MDPP group (Table 2). Within the MDPP, women informed they had a higher CVD QRISK2 score at baseline were more likely to leave the programme. Adjusted odds ratio for leaving (95% CI) 1.36 (1.08, 1.80) for each unit increase in 10 year CVD QRISK2 score (p = 0.02) and 1.22 (1.03, 1.46) for each year of predicted heart age greater than their actual age (p = 0.02) (Supplementary Table 1).
Completeness of weight and self-report measures
Weight measures were obtained in 100% of completers. There were high levels of completion for the self-report measures. The median response rate at 6 m for the self-report measures collected across both groups was 78% (Supplementary Table 2).
Need for the programmes
Baseline characteristics of participants are reported in Table 3. The BCPP and MDPP groups were comparable. Women were mainly from the three least deprived quintiles of the index of multiple deprivation and white British. Approximately one-third of the cohort had a family history of BC (BCPP 26.7%, MDPP 34.6%,). Sixty-two percent of the BCPP and 60.5% MDPP groups had previously undertaken a commercial weight loss programme, and there were few smokers (BCPP 6.7% vs. MDPP 7.4%).
Ten women (12.3%) in the MDPP group had previously had an NHS Health Check more than 6 months prior to joining the study. Relatively high numbers of women in the MDPP group had previously unknown increased risks for CVD (14.8% with ≥ 10% 10 year risks of CVD and 14.8% with total cholesterol ≥ 7.5 mmol/L) and for T2D (56% with ≥ 10% 10-year risk of T2D, and 6.2% with HbA1c > 42 mmol/mmol) (Table 4). Some of these women were subsequently commenced on medications for blood pressure (n = 2) and raised cholesterol (n = 1) by their family doctor.
Fidelity of programme delivery
Dietitian time for delivery of the intervention and fidelity of delivery are described in Table 5.
Across both groups, women received mean (95% CI) 90 (88-98) % of their scheduled week 1, 4 and 8 calls and 91 (86-95%) of their scheduled e-mails. Mean (95% CI) 90 (88-98) % of scheduled calls, 91 (86-95%). There was good engagement with the self-monitoring website. Ninety-seven percent of women used the website at least once in the first 3 months, 87% 3-6 months, 83% 6-9 months and 79% 9-12 months. A number of women in the BCPP and MDPP groups were referred to NHS behaviour change services; PA referral services 8 (18%) BCPP and 23 (28.4%) MDPP, smoking cessation 1 out of 3 smokers BCPP and 5 out of 6 smokers MDPP, and alcohol services 0/8 BCPP and 4/22 (4.9%) with an AUDIT score of greater than or equal to 8 MDPP by their allocated dietitian.
Participant satisfaction
Anonymous satisfaction questionnaires for the overall programme were completed by 71/88 (81%) of those who completed the study at 12 months (26, 57% of the BCPP group and 45, 55% of the MDPP group) (Tables 6 and 7).
Website evaluation was completed by 109/126 (87%) of women. The phone and e-mail feedback was well received. Women understood and positively evaluated the CVD and T2D risk feedback and dietary elements of the programme. However, they were less confident to follow the PA plans.
Free text feedback showed that women felt their self-efficacy to undertake PA would increase with a demonstration class or DVD. They emphasised the need for review calls to be scheduled, and that feedback e-mail should be personalised and not generic. They valued the advice from the dietitian who was considered a credible source of information. A number of changes to the website were suggested including a forum to facilitate peer-to-peer communication and support, an ‘ask the expert’ function, and adding an average weight loss line to their weight tracker so they could compare their weight loss with the average of the other participants.
Adverse events and harms associated with the programmes
No study or intervention related serious or unexpected adverse events occurred. Completer-only analysis showed a small reductions in state anxiety score with the BCPP (n = 37) −0.7 (−4.6 to 3.2) and MDPP (n = 60) −3.5 (−6.7 to −0.4), and an increase in EQ-5D-5L scores in the BCPP (n = 40) 4.1 (0.6 to 7.6) and MDPP groups (n = 60) 7.3 (3.6 to 11.1) (Table 8). The proportion reporting a high state anxiety score (≥ 40) at baseline was 6 (16.2%) BCPP and 18 (30%) MDPP compared to 7 (18.9%) BCPP and 15 (25%) MDPP and at 6 months.
Primary outcome for the planned definitive trial
Both programmes achieved good and comparable reductions in weight (Table 8). Mean (95% CI) BOCF percentage weight loss at 12 months were −7.6 (−9.8 to −5.4) % in the BCPP group and −7.4 (−9.1 to −5.7) % in the MDPP group (p = 0.952). BOCF weight loss at 12-months was −6.01 (−7.87 to −4.1) kg in the BCPP group and −6.2 (−7.8 to −4.71) kg in the MDPP group (p = 0.673), with respectively 58 and 57% and achieving weight loss of ≥ 5% (P = 0.915). The level of weight loss associated with reduced risk of disease [21,22,23,24].
Changes in other self-reported health behaviours
The proportion reporting at risk drinking (AUDIT score ≥ 8) reduced from 8 (17.5%) in the BCPP and 22 (27.2%) in the MDPP at baseline to respectively 4 (8.9%) and 14 (17.3%) at 6 months. Likewise, the proportion of women reporting saturated fat intakes above the recommended intake of 20 g/day reduced from 29 (87.9%) in the BCPP and 40 (72.7%) in the MDPP at baseline to respectively 12 (36.4%) and 19 (34.5%) at 6 months. Both groups also reported modest increases in moderate intensity PA at 6 months. One woman from each group had stopped smoking by 6 months and was still not smoking at the 12-month follow-up.
Discussion
Main findings
The BCPP and MDPP appear feasible with good uptake, retention, fidelity, patient satisfaction and no evidence of harms. The MDPP highlighted previous unknown risk of CVD and T2D but does not appear to increase engagement with behaviour change beyond a standard BCPP amongst women attending breast screening. Both programmes showed good weight loss.
Overall uptakes to the mailed invitation to both programmes were around 10%. This is comparable to previously reported uptakes to behaviour change programmes when written invitations are given to women when they attend the NHSBSP, or when postal invitations are sent to women at increased risk of BC [38]. This feasibility study highlights potential strategies to increase recruitment to weight loss programmes within the NHSBSP. Firstly, focussing on women at high or above average BC risk who had uptakes of 14-20% compared to 4-10% for women at average or low BC risk reported herein and previously within this cohort [17]. Higher risk women will also derive a greater absolute risk reduction from changes in health behaviours compared to low risk women [39, 40].
Future programmes could include women with existing health conditions. Significant proportions of women who were interested to join the programmes were ineligible due to pre-existing weight-related health conditions (7.1% BDPP and 12.0% of the MDPP group). We presume these weight-related health conditions were not currently being addressed within existing NHS weight loss/behaviour change services. Inclusion of these women would have given uptakes of 18.1 to BCPP and 23.0% to MDPP. Lastly, recruiting women at their mammogram appointments and using remote collection of outcome measures such as weight would overcome identified barriers of time and travel around additional appointments reported by women who declined to join this study.
Both programmes appear highly effective for weight loss and behaviour change. The mean weight loss at 12 months over 6 kg using baseline carried forward imputation compares favourably with outcomes from group-based commercial (2-4 kg), internet (1.9 kg) and primary care programmes (0.7-3.6 kg) [41].
There was good engagement with the website and phone-supported programmes. This hybrid face-to-face and remotely delivered programme allowed women to receive initial individual face-to-face advice from a health care professional combined with the website that allows self-monitoring and prompt regular feedback from the health care professional. Such programmes have been found to be both more and less effective compared to standard face-to-face programmes, dependent on the level of user engagement achieved [42].
Most previous website programmes have been tested amongst younger cohorts. The few studies amongst older women concur with our findings of good engagement [43,44,45], and the potential for their utility amongst women of breast screening age. The 2018 Office of National Statistics bulletin reported large increases in internet usage amongst older women. In 2018, 98% of women aged 44-54 years had used the internet in the past 3 months, compared to 92% of 55-64 year olds and 80% of 65-74 year olds [46].
There has been minimal research on the feasibility or efficacy of multiple disease prevention programmes. It was thought that multiple disease risk information could be personally relevant to a larger group of women than just providing risk information on a single disease such as BC, increasing the likelihood of having a positive effect on behaviours [47]. Alternatively, it was possible multiple disease risk information could reduce motivation and self-efficacy and threaten self-integrity to change health behaviours in some individuals. We found no difference in engagement and behaviour change with a supervised MDPP compared to the BCPP.
There was no evidence of harm with the MDPP such as increased anxiety, or lower self-rated health assessed with the EQ-5D as a result of being provided with personalised risk of CVD and T2D. This is an important finding which is in line with other studies of providing risk information, despite concerns about adverse effects [48, 49]. The higher drop out in women at higher baseline risk of CVD in the MDPP group may be an incidental finding. CVD risk information by itself has minimal effect on health behaviours [50]. In the recent INFORM trial, neither genotypic nor phenotypic coronary heart disease risk information influenced the efficacy of a web-based lifestyle programme for changes in PA, diet or weight [51]. Future studies should assess whether CVD risk information impacts on engagement and the efficacy of weight loss programmes.
Strengths and limitations
This is one of the few studies to test the feasibility and acceptability of a BC prevention and multiple disease prevention programmes in women in the breast screening programme. Also, one of the few to test website and phone programmes amongst middle-aged women. Twelve-month data including 6 months of website-only support provides an indication of the long-term effects of the programmes for weight loss maintenance.
Key limitations that a future effectiveness trial should address are as follows. The study invited a selected group of women who had previously been recruited to the PROCAS study, who were recruited some time after their attendance at breast screening. Studies need to test uptake to the programmes in an unselected cohort at the time of breast screening. In addition, all trial procedures were conducted at a research unit. The future trial should ideally be in a screening site or a nearby community location to inform how these programmes could be integrated within the NHSBSP or be fully remote or online. It should also include a number of centres, and not just one as tested in this feasibility study.
The 68% retention at 12 month compares favourably with weight loss studies which often have retention rates of below 50%. However, our attrition rate of 32% is above the recommended level of 20% and so raises concerns about attrition bias and the validity of the study [52]. Future studies would be conducted with a clinical trials unit where enhanced; administrative support could help reduce attrition. Further strategies to reduce attrition bias could include financial incentives and additional contact with participants in the weight loss maintenance phase of the intervention [53]. We did not include a control group, so we do not know the likely uptake and retention in a control group, and how best they could be kept engaged.
Secondary trial end-points (e.g. weight) were assessed by members of the research team which sometimes included the research dietitians delivering the intervention who were not blinded to the intervention. The study included two intervention groups and did not include a no intervention control group which would be required in a definitive randomised trial.
Further participant involvement and engagement (PPIE) work can help refine the invitation and recruitment strategy to the programmes. This could include a personalised letter of endorsement of the trial from their family doctor [54]. PPIE work is specifically required to promote uptake amongst women from black, Asian, minority ethnic and socially deprived groups who had low uptakes to this study, as seen with previous breast screening and cancer trials [55]. Other potential strategies, such as face-to-face introduction to the trial at the time of screening and telephone follow-up after the mailed invite [56] are unlikely to be feasible due to the size of the target population.
Implications and future research
We assessed the feasibility and acceptability of a BCPP or MDPP amongst women in the breast screening programme and whether there were any additional benefits with the MDPP programme, to determine which programme was worthy of further investigation in a large scale RCT within the NHSBSP. Both programmes met the NICE criteria for the efficacy of weight loss programmes, i.e. at least 60% of participants are likely to complete, average weight loss is at least 3%, and at least 30% of participants lose ≥ 5% of their initial weight [57]. The simpler, lower cost BCPP would be the preferred test programme to assess long-term behaviour change and weight loss and reduced risk of BC vs. standard care and other weight- and health-behaviour-related conditions.
Increased coverage and appropriate medication are current targets for the NHS Health Check programme [13]. Given this, future trials could assess the impact of offering a MDPP around the time of breast screening to increase coverage of CVD and T2D risk assessment and whether a one-stop shop can increase NHS efficiency and potential uptake to the NHSBSP.
Dietitians delivered the test programmes. Future programmes could consider provision of original dietary advice by a dietitian as a trusted source of knowledge, with ongoing support from a health trainer to reduce costs. This model of delivery has been favourably evaluated in other weight loss settings [58] and likely to be more effective than programmes which are entirely delivered by non-specialists which have achieved only modest weight loss [59]. Further work is required to improve the PA component of the programme which had modest effects on PA.
Conclusion
The MDPP identified previously unknown CVD and T2D risk factors but does not appear to increase engagement with behaviour change beyond a standard BCPP amongst women attending breast screening. The results suggest a definitive effectiveness trial of the BCPP intervention is warranted. Weight loss achieved with a BCPP will reduce risk of BC as well as CVD and T2D and other weight-related cancers and health conditions.
Availability of data and materials
The trial protocol and all datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BC:
-
Breast cancer
- CVD:
-
Cardiovascular disease
- T2D:
-
Type 2 diabetes
- NHSBSP:
-
NHS Breast Screening Programme
- BMI:
-
Body mass index
- BOCF:
-
Baseline observation carried forward
- PROCAS:
-
Predicting of Cancer at Screening
- BCPP:
-
Breast cancer prevention programme
- MDPP:
-
Multiple disease prevention programme
References
Evans DG, Astley S, Stavrinos P, Harkness E, Donnelly LS, Dawe S, et al. Improvement in risk prediction, early detection and prevention of breast cancer in the NHS Breast Screening Programme and family history clinics: a dual cohort study. NIHR J Library. Programme Grants for Applied Research, No. 4.11. 2016.
Public Health England and the Food Standards Agency. National diet and nutrition survey results from years 7 and 8 (combined) of the rolling programme 2014/2015 to 2015/2016. 2018.
Green J, Reeves GK, Floud S, Barnes I, Cairns BJ, Gathani T, et al. Cohort profile: the million women study. Int J Epidemiol. 2019;48(1):28–29e. https://doi.org/10.1093/ije/dyy065.
Arthur R, Wassertheil-Smoller S, Manson JE, Luo J, Snetselaar L, Hastert T, et al. The combined association of modifiable risk factors with breast cancer risk in the women’s health initiative. Cancer Prev Res. 2018;11(6):317–26.
Chomistek AK, Chiuve SE, Eliassen AH, Mukamal KJ, Willett WC, Rimm EB. Healthy lifestyle in the primordial prevention of cardiovascular disease among young women. J Am Coll Cardiol. 2015;65(1):43–51.
Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001;345(11):790–7.
Shieh Y, Eklund M, Madlensky L, Sawyer SD, Thompson CK, Stover FA, et al. Breast cancer screening in the precision medicine era: risk-based screening in a population-based trial. J Natl Cancer Inst 2017;109(5):djw290. https://doi.org/10.1093/jnci/djw290.
Evans DG, Donnelly LS, Harkness EF, Astley SM, Stavrinos P, Dawe S, et al. Breast cancer risk feedback to women in the UK NHS breast screening population. Br J Cancer. 2016;114(9):1045–52.
Mango V, Bryce Y, Morris EA, Gianotti E, Pinker K. Commentary ACOG practice bulletin July 2017: breast cancer risk assessment and screening in average-risk women. Br J Radiol. 2018;91(1090):20170907.
French DP, Astley S, Brentnall AR, Cuzick J, Dobrashian R, Duffy SW, et al. What are the benefits and harms of risk stratified screening as part of the NHS breast screening Programme? Study protocol for a multi-site non-randomised comparison of BC-predict versus usual screening (NCT04359420). BMC Cancer. 2020;20(1):570.
van Veen EM, Brentnall AR, Byers H, Harkness EF, Astley SM, Sampson S, et al. Use of single-nucleotide polymorphisms and mammographic density plus classic risk factors for breast cancer risk prediction. JAMA Oncol. 2018;4(4):476–82.
Patel R, Barnard S, Thompson K, Lagord C, Clegg E, Worrall R, et al. Evaluation of the uptake and delivery of the NHS Health Check programme in England, using primary care data from 9.5 million people: a cross-sectional study. BMJ Open. 2020;10(11):e042963.
Public Health England. Health matters: preventing cardiovascular disease. 2019.
Duddy C, Wong G, Gadsby EW, Krska J, Hibberd V. NHS Health Check programme: a protocol for a realist review. BMJ Open. 2021;11(4):e048937.
Harvie M, Wright C, Pegington M, McMullan D, Mitchell E, Martin B, et al. The effect of intermittent energy and carbohydrate restriction v. daily energy restriction on weight loss and metabolic disease risk markers in overweight women. Br J Nutr. 2013;110(8):1534–47.
Schwingshackl L, Z+ñhringer J, Nitschke K, Torbahn G, Lohner S, K++hn T, et al. Impact of intermittent energy restriction on anthropometric outcomes and intermediate disease markers in participants with overweight and obesity: systematic review and meta-analyses.(1549-7852 (Electronic)).
Harvie M, Pegington M, French D, Cooper G, McDiarmid S, Howell A, et al. Breast cancer risk status influences uptake, retention and efficacy of a weight loss programme amongst breast cancer screening attendees: two randomised controlled feasibility trials. BMC Cancer. 2019;19(1):1089.
World Cancer Research Fund. Diet, nutrition, physical activity and breast cancer. 2018.
University of Nottingham and EMIS. Q Risk. 2018.
Hippisley-Cox J, Coupland C. Development and validation of QDiabetes-2018 risk prediction algorithm to estimate future risk of type 2 diabetes: cohort study. BMJ. 2017;359:j5019.
Harvie M, Howell A, Vierkant RA, Kumar N, Cerhan JR, Kelemen LE, et al. Association of gain and loss of weight before and after menopause with risk of postmenopausal breast cancer in the Iowa women’s health study. Cancer Epidemiol Biomarkers Prev. 2005;14(3):656–61.
Catsburg C, Miller AB, Rohan TE. Adherence to cancer prevention guidelines and risk of breast cancer. Int J Cancer. 2014;135:2444–52.
Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, Brenneman AT, et al. 10-year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. Lancet. 2009;374(9702):1677–86.
Ebrahim S, Taylor F, Ward K, Beswick A, Burke M, Davey SG. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst Rev. 2011;(1):CD001561. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001561.pub3/full.
Jarrett RJ, Keen H, Murrells T. Changes in blood pressure and body weight over ten years in men selected for glucose intolerance. J Epidemiol Community Health. 1987;41(2):145–51.
Aucott L, Gray D, Rothnie H, Thapa M, Waweru C. Effects of lifestyle interventions and long-term weight loss on lipid outcomes - a systematic review. Obes Rev. 2011;12(5):e412–25.
UK Department of Health. Start active, stay active: a report on physical activity for health from the four home countries’ Chief Medical Officers. 2011.
Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived alcohol use disorders identification test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin Exp Res. 2005;29(5):844–54.
Professor Kevin Norton, Dr Lynda Norton. Pre-exercise screening: guide to the Australian adult pre-exercise screening system. 2011.
O’Keefe DJ, Jensen JD. The relative persuasiveness of gain-framed and loss-framed messages for encouraging disease prevention behaviors: a meta-analytic review. J Health Commun. 2007;12(7):623–44.
French DP, Cameron E, Benton JS, Deaton C, Harvie M. Can communicating personalised disease risk promote healthy behaviour change? A systematic review of systematic reviews. Ann Behav Med. 2017;51(5):718–29. https://doi.org/10.1007/s12160-017-9895-z.
National Institute for Health and Care Excellence (NICE). Behaviour change: individual approaches. NICE 14 A.D. January 2 [cited 28 Dec 2018]; Available from: URL: https://www.nice.org.uk/guidance/ph49/resources/behaviour-change-individual-approaches-pdf-1996366337989.
International Physical Activity Questionnaire (IPAQ) long version. Karolinska Institutet 2014 [cited 13 A.D. Jan 31]; Available from: URL: www.ipaq.ki.se.
Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight participant groups: a multi-country study. Qual Life Res. 2013;22(7):1717–27.
Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI). Br J Clin Psychol. 1992;31(Pt 3):301–6.
Department for Communities and Local Government. The English indices of deprivation 2010. Department for Communities and Local Government 2011 March 1 [cited 19 Aug 2020]; Available from: URL: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/6320/1870718.pdf.
NIHR Cambridge Biomedical Research Centre. DAPA measurement toolkit. NIHR Cambridge Biomedical Research Centre 2020 [cited 2020 Sep 25]; Available from: URL: https://dapa-toolkit.mrc.ac.uk/diet/subjective-methods/estimated-food-diaries.
Evans DG, Harvie M, Bundred N, Howell A. Uptake of breast cancer prevention and screening trials. J Med Genet. 2010;47(12):853–5.
Hopper JL, Dite GS, MacInnis RJ, Liao Y, Zeinomar N, Knight JA, et al. Age-specific breast cancer risk by body mass index and familial risk: prospective family study cohort (ProF-SC). Breast Cancer Res. 2018;20(1):132.
Maas P, Barrdahl M, Joshi AD, Auer PL, Gaudet MM, Milne RL, et al. Breast cancer risk from modifiable and nonmodifiable risk factors among white women in the United States. JAMA Oncol. 2016;2(10):1295–302.
Hartmann-Boyce J, Johns DJ, Jebb SA, Summerbell C, Aveyard P. Behavioural weight management programmes for adults assessed by trials conducted in everyday contexts: systematic review and meta-analysis. Obes Rev. 2014;15(11):920–32.
Sorgente A, Pietrabissa G, Manzoni GM, Re F, Simpson S, Perona S, et al. Web-based interventions for weight loss or weight loss maintenance in overweight and obese people: a systematic review of systematic reviews. J Med Internet Res. 2017;19(6):e229.
O’Brien T, Jenkins C, Amella E, Mueller M, Moore M, Hathaway D. An internet-assisted weight loss intervention for older overweight and obese rural women: a feasibility study. Comput Inform Nurs. 2016;34(11):513–9.
Pullen CH, Hageman PA, Boeckner L, Walker SN, Oberdorfer MK. Feasibility of Internet-delivered weight loss interventions among rural women ages 50-69. J Geriatr Phys Ther. 2008;31(3):105–12.
van der Mark M, Jonasson J, Svensson M, Linne Y, Rossner S, Lagerros YT. Older members perform better in an internet-based behavioral weight loss program compared to younger members. Obes Facts. 2009;2(2):74–9.
Office of National Statistics. Internet users, UK: 2018. 2018 May 31.
Cooke R, Sheeran P. Moderation of cognition-intention and cognition-behaviour relations: a meta-analysis of properties of variables from the theory of planned behaviour. Br J Soc Psychol. 2004;43(Pt 2):159–86.
Marteau TM, Kinmonth AL, Thompson S, Pyke S. The psychological impact of cardiovascular screening and intervention in primary care: a problem of false reassurance? British Family Heart Study Group. Br J Gen Pract. 1996;46(411):577–82.
French DP, Southworth J, Howell A, Harvie M, Stavrinos P, Watterson D, et al. Psychological impact of providing women with personalised 10-year breast cancer risk estimates. Br J Cancer. 2018;118:1648–57.
Sheridan SL, Viera AJ, Krantz MJ, Ice CL, Steinman LE, Peters KE, et al. The effect of giving global coronary risk information to adults: a systematic review. Arch Intern Med. 2010;170(3):230–9.
Silarova B, Sharp S, Usher-Smith JA, Lucas J, Payne RA, Shefer G, et al. Effect of communicating phenotypic and genetic risk of coronary heart disease alongside web-based lifestyle advice: the INFORM Randomised Controlled Trial. Heart. 2019;105(13):982–9.
Sackett DL, Richardson WS, Rosenberg W, Haynes RB. Evidence based medicine: how to practice and teach EBM. New York: Churchill Livingstone; 1997.
Pirotta S, Joham A, Hochberg L, Moran L, Lim S, Hindle A, et al. Strategies to reduce attrition in weight loss interventions: a systematic review and meta-analysis. Obes Rev. 2019;20(10):1400–12.
Crocker JC, Ricci-Cabello I, Parker A, Hirst JA, Chant A, Petit-Zeman S, et al. Impact of participant and public involvement on enrolment and retention in clinical trials: systematic review and meta-analysis. BMJ. 2018;363:k4738.
Evans DG, Brentnall AR, Harvie M, Astley S, Harkness EF, Stavrinos P, et al. Breast cancer risk in a screening cohort of Asian and white British/Irish women from Manchester UK. BMC Public Health. 2018;18(1):178.
Treweek S, Pitkethly M, Cook J, Fraser C, Mitchell E, Sullivan F, et al. Strategies to improve recruitment to randomised trials. Cochrane Database Syst Rev. 2018;2:MR000013.
NICE. Weight management: lifestyle services for overweight or obese adults. NICE 2014 May 1 [cited 2018 Nov 2];Available from: URL: https://www.nice.org.uk/guidance/PH53.
Zizzi S, Kadushin P, Michel J, Abildso C. Client experiences with dietary, exercise, and behavioral services in a community-based weight management program. Health Promot Pract. 2016;17(1):98–106.
Nanchahal K, Power T, Holdsworth E, Hession M, Sorhaindo A, Griffiths U, et al. A pragmatic randomised controlled trial in primary care of the Camden Weight Loss (CAMWEL) programme. BMJ Open. 2012;2(3). https://bmjopen.bmj.com/content/bmjopen/2/3/e000793.full.pdf.
Acknowledgements
We acknowledge the work of David Preece for the set up and management of the trial website; Sarah Sampson, Paula Stavrinos and Jake Southworth (Manchester University NHS Foundation Trust) for their help with recruitment; Julie Pickford, Alison Morgan (Public Health Manchester), Basil Issa, Ed Gambol, Joyce Yeo (Manchester University NHS Foundation Trust) and Christi Deaton (University of Cambridge) for their advice and support for assessing and communicating CVD, T2D and dementia risk; the Prevent Breast Cancer participant Public Involvement panel for their advice and invaluable insights.
Funding
This project was funded by Prevent Breast Cancer (registered charity number 1109839) and supported by the NIHR Manchester Biomedical Research Centre (IS-BRC-1215-20007) infrastructure. The funders had no role in the design, conduct, analysis or write up of the study. DGE, MH, MP, DPF, CJA and AH are supported by the NIHR Manchester Biomedical Research Centre (IS-BRC-1215-20007). CJA is supported by NIHR Greater Manchester Participant Safety Translational Research Centre.
Author information
Authors and Affiliations
Contributions
Conception: MH, DF, AH, LD, DGE and CJA. Data collection: MP, GC, SM, CB, HR and KS. Data analysis: MH, MP, GC and EB. Manuscript writing: MH, MP, DF, GC, SM, AH, LD, HR and DGE. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the NRES Committee West Midlands–Solihull, reference 13/WM/1088. Informed written consent was obtained from all subjects, and the study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Multivariable logistic regression of the association between baseline risk of type 2 diabetes and cardiovascular disease and withdrawal and percentage weight loss within the multiple disease prevention group (n = 81). Adjusting for age, Townsend deprivation vation, smoking status, BMI and breast cancer risk category
Additional file 2: Supplementary Table 2.
Completeness of weight and self -reported lifestyle, anxiety and health status endpoints
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Harvie, M., French, D.P., Pegington, M. et al. Testing a breast cancer prevention and a multiple disease prevention weight loss programme amongst women within the UK NHS breast screening programme—a randomised feasibility study. Pilot Feasibility Stud 7, 220 (2021). https://doi.org/10.1186/s40814-021-00947-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-021-00947-4