Abstract
Background
Aflatoxins (AFs) are naturally occurring fungal metabolites produced by the Aspergilla species of fungi. The staple food grain, maize (Zea mays), is highly susceptible to AF contamination. In Kenya, contamination of maize supplies by AFs is a recognized public health problem which has resulted in over 600 human deaths. Human exposure to AFs can occur in utero, via breast milk, through weaning foods, and throughout an individual’s lifetime. Recent epidemiological studies have shown that exposure to AFs in early life through diet is a contributing factor to immune suppression, micronutrient deficiency, possible vaccine interference, and impaired growth in children. However, these results remain inconsistent and inconclusive due to lack of randomized controlled studies.
Methods
A randomized school-based cross-sectional study was designed to study AF exposure levels and associated health effects in children between ages 6 and 12 years. Participants were recruited from primary schools within Siaya and Makueni Counties of Kenya, East Africa. The Joint Ethics Committee of the University of Nairobi and Kenyatta National Hospital in Kenya approved the research protocol and procedures for the study. Both parental consent and child assent were obtained before enrollment in the study. Parents were requested to provide household grain samples and fill out questionnaires detailing their sociodemographic information, household dietary patterns, farming practices, and knowledge of AF contamination. Blood samples were collected from children participants, and sera were prepared for analysis of AFB1-lysine which is one of the validated biomarkers for AF exposure.
Discussion
This protocol describes a school-based, cross-sectional study whose objective is to comparatively evaluate the role of AF exposure on adverse health outcomes in children. Specifically, effects of cumulative AF exposure on nutritional status, immune markers, and growth parameters will be assessed.
Trial registration
This study is not a clinical trial, rather a cross-sectional study aimed at providing baseline data on AF exposures in children who live in presumably high versus low AF exposure regions. Results from the study can be used to design interventions and/or prospective cohort studies aimed at studying adverse health effects associated with cumulative AF exposure through diets. The study reference number is P741/12/2017 and registered with KNH-UoN Ethics and Research Committee.
Similar content being viewed by others
Background
Aflatoxins (AFs) are a group of naturally occurring mycotoxins produced by the common fungus Aspergillus flavus and the closely related Aspergillus parasiticus fungi [1,2,3]. Up to 4.5 billion people around the world are exposed to AFs through the diet and/or via occupational exposures during grain handling [4, 5]. AFs are common food contaminants which present a persistent challenge throughout the food chain. Food staples frequently contaminated with AFs include maize, peanuts, rice, cassava, spices, and other food items [1,2,3].
There are up to 14 different groups of naturally occurring AFs, but the commonly studied groups include B1, B2, G1, and G2 [1, 3]. Aflatoxin B1 (AFB1) is the most biologically potent because it is a confirmed human carcinogen classified into group I by the International Agency for Research on Cancer [2, 3]. AFB1 is a major risk factor associated with primary liver cancers as evident in many studies conducted in Africa and South East Asia [6,7,8]. Moreover, AFs are immune toxicants and have been associated with immune suppression in human populations [9, 10]. In children, recent epidemiology studies provide evidence that cumulative exposure to AFs in low concentrations contributes to micronutrient deficiency, possible vaccine interference, immune suppression, and growth impairments [11,12,13]. The adverse health outcomes associated with AF exposure may persist into adulthood if neither interventions nor corrective measures are undertaken. To date, comprehensive data on AF exposure is limited, and thus, assessment of adverse health outcomes is further hindered.
Contrary to long-term exposure to AFs where adverse health outcomes occur over time, dietary exposure to AFs exceeding 200 μg/kg in the short term can be fatal due to aflatoxicosis [14,15,16]. Aflatoxicosis is a medical condition characterized by jaundice, bile duct proliferation, edema, sudden liver failure, and ultimately death within 24 h of consumption of AF-contaminated maize [15,16,17,18].
In Kenya, AF contamination in maize supplies is a recognized public health problem, which has resulted in more than 600 documented human deaths attributed to aflatoxicosis [19,20,21]. The US Food and Drug Administration (USFDA) recommends that food destined for human consumption should not exceed total AFs of 20 μg/kg [22]. The European Union’s Codex Alimentarius recommends 15 μg/kg [23] while Kenya, given its troubled past with deaths associated with aflatoxicosis, stipulated a strict recommendation of 10 μg/kg [24]. These recommended exposure levels are significantly difficult to implement due to widespread subsistence farming which promotes higher AF exposure because maize produced in farms are consumed directly without prior testing for AF contamination levels.
Study hypotheses, objective, and specific aims
We hypothesize that children recruited from high AF exposure region of Makueni are more likely to suffer adverse health outcomes including micronutrient deficiency, immune suppression, and growth impairment compared to children recruited from low exposure region of Siaya County. This hypothesis will be tested against the null hypothesis of dietary exposure to AFs is not associated with adverse health outcomes in children.
The general objective of the study is to provide a comprehensive assessment of how dietary exposure to AFs contributes to micronutrient deficiency, immune suppression, and growth impairment in school-going children. Specific aims include the following: (1) to determine the cumulative levels of AF exposure in children of Makueni and Siaya Counties; (2) to determine the nutritional and immune status of children in Siaya and Makueni Counties; (3) to study the association between AF exposure, micronutrient deficiency, and immune suppression; and (4) to elucidate possible growth impairment, if any, in children with high AFB1-lysine adducts exceeding 10 pg/mg of albumin.
This study will be the first to provide baseline data on AF exposure in children between the ages of 6 and 12 years recruited from a high and low AF exposure regions of Kenya. The study is a collaborative project between the University of Nairobi’s KAVI Institute of Clinical Research and the University of Georgia in Athens in the USA. The study protocol is based on the SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) and CONSORT 2010 (Consolidated Standards of Reporting Trials) reporting guidelines.
Methods/design
The study design is school-based and cross-sectional to provide a snapshot of AF exposure levels among children recruited from Siaya and Makueni Counties. Cross-sectional study design was preferred due to its ability to generate factual information on AF exposure among children widespread over two geographic locations. To ensure samples are representative of both Makueni and Siaya Counties, primary schools without feeding programs were randomly selected in different constituencies per county.
Setting of the study
The selection of Makueni and Siaya Counties was made according to previous studies which reported high AF exposures in Makueni County while Siaya’s exposure levels were below the level of detection [15, 25]. Makueni County lies in Kenya’s former Eastern Province while Siaya County forms one of the six counties in the former Nyanza Province [25]. Siaya County is hot and humid with temperatures averaging from 21 to 25 °C while annual precipitation ranges between 1000 and 1750 mm [26]. Conversely, the climate of Makueni County is predominantly semi-arid characterized by long dry seasons interspersed by an annual rainfall of about 500 mm and ambient temperature ranges between 18 and 24 °C in the cold season and between 24 and 33 °C in the hot season [27]. Makueni County’s aridity has been implicated to be a significant contributing factor to AF contamination as a result of undue crop stress [15, 27]. The Luo ethnic groups are the main inhabitants of Siaya County while the Akamba community inhabits the high exposure regions of Makueni County [28]. The estimated poverty rate in Makueni and Siaya Counties is 64% and 48%, respectively, compared to the national average of 47% as of 2009 [26, 28]. Overall, the choice of Makueni and Siaya Counties as study location provides control for differences in weather conditions, ethnicity, and poverty levels.
Due to limited food diversity in sub-Saharan Africa, our study populations depend on maize and maize-based products for daily energy requirements [29, 30]. The dietary staples in Kenya include maize-based meals comprised of solid maize meal, commonly known as ugali in Swahili; porridge; roasted and boiled maize cobs; and/or maize boiled with beans [30]. Moreover, each household is estimated to consume maize-based meals at least two times a day because ugali is often served during lunch and/or dinner in accompaniment with a mix of vegetables and/or any kind of stew [30, 31]. Consuming a variety of foods from several food groups is a recommended approach to achieve necessary nutritional requirements and limit excessive exposure to AFs through the diet [32]. Diet diversification has been proposed to be instrumental in mitigating AF exposure and the associated adverse health outcomes. The International Food Policy Research Institute proposed that households with a dietary score less than 4.5 can be categorized as low dietary diversity, a score between 4.5 and 6 has medium dietary diversity, and a score greater than 6 can be considered both high and good dietary diversity [33]. In our study populations, past studies reported low dietary diversity with a score of less than 4 food groups each day [31, 34]. Therefore, food insecurity is paramount in our study populations due to low agricultural productivity that is characterized by unreliable rains, limited access to farm inputs, and hired labor which increases the cost of food production significantly [26]. Nonetheless, small-scale holder farmers undertake maize cultivation for household consumption despite low agricultural output and increased risk of AF contamination.
Justification of Makueni and Siaya Counties as study sites
In Kenya’s former Eastern Province, high level of AF contamination is concentrated in Makueni County as evident in multiple aflatoxicosis outbreaks previously reported [15, 18]. In 2004, a severe aflatoxicosis outbreak characterized by 317 cases of acute hepatic failure and subsequent 125 deaths was reported [17, 35, 36]. The Kenyan Ministry of Health worked collaboratively with experts from the US Center for Disease Control and Prevention to assess risk factors associated with the outbreak [18, 21]. While the cases were inhabitants of Makueni, Kitui, and Machakos Counties, inhabitants of Makueni County were the most affected, accounting for almost 50% of the cases [20, 37]. Consumption of AF-contaminated maize was linked to aflatoxicosis [21, 36].
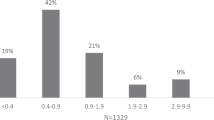
In a serological survey to evaluate regional variation of AF exposure in Kenya, 78% of archived serum samples had detectable AF levels [25]. The highest AF exposure was recorded in the former Eastern Province with a median of 7.87 pg/mg AF albumin adducts, while in the former Nyanza Province, the AF albumin adducts were below the limit of detection (< LOD) in human serum samples evaluated. The AF levels were much lower in all the other five provinces. The regional variation of AF exposure levels as reported by Yard et al. [25] is exhibited in Fig. 1 created using vector map outlines from Vemaps.com [38].
Sample size determination
According to the Kenya Population census of 2009, Siaya County had a population of 842,304 while Makueni County had 884,527 people [39]. The sample size was determined using Krejcie and Morgan’s methodology [40].
where s is the required sample size; X2= 3.841, which is the table value of chi-square for 1 degree of freedom at 95% confidence interval; N is the population size; P is the population proportion which is assumed to be 0.50 since this provides maximum sample size; and d is the degree of accuracy expressed as a proportion (0.05).
According to Krejcie and Morgan’s formula, the estimated sample size was determined to be 393 schoolchildren per county [40]. The estimated total number of participants required to achieve the study objectives was 786 across different schools from 2 counties.
Sampling
Makueni is confirmed to have the highest prevalence of AF exposure among Kenya’s 47 counties spread across former 8 provinces. In contrast, Siaya which is considered to be a low exposure region has had few studies conducted in the region. Siaya and Makueni Counties were chosen based on AF exposure levels reported on published literature [20, 25, 37]. Schools were randomly selected per constituency at the county level as long as the school did not have feeding programs and were located at least 3 km from a shopping center to limit the possibility of consuming market or store-bought maize products. In Siaya County, schools allow a 1-h lunch break where students go home for lunch and come back for afternoon classes. In Makueni, however, students bring lunch from home in the morning and have half-hour lunch break, before resuming classes in the afternoon. Participants enrolled in the study were randomly selected using the Kish Grid Method to avoid selection bias [41].
Human participants
School administrations were requested to convene parent meetings at a convenient time and location for participants. Community leaders including local area chiefs and members of the county assembly were invited to the meetings. The chairperson of the Parent Teachers Association was in attendance and presided over the meetings. The study purpose and significance were explained to school officials, teachers, support staff, and parents. The participants were given ample opportunity to ask questions during the meeting, before subject recruitment, and during the study to ensure full disclosure of study components. Informed consent forms were explained to parents in their local dialect, and all their questions were addressed before being asked to provide consent and fill out questionnaires.
The five-part questionnaire administered collected basic information including participants’ age, sex, weight, height, and mid-upper arm circumference; sociodemographic factors including marital status, education levels, living conditions, occupations of both the respondent and their spouse, household income levels, and information on home ownership and living conditions. Participants also reported farming practices which entail whether they grow or buy maize for household use, use of pesticides and/or fertilizers during farming, extent of AF knowledge, and how each household stores maize and other food supplies after harvest. In addition, the questionnaire collected information on dietary intake of different food groups, number of meals in a day, food choice, and nutrition practices. Information collected from questionnaires provided sufficient information to enable analysis of socioeconomic status and respective poverty levels. Moreover, these possible confounding factors can be easily controlled in statistical analyses.
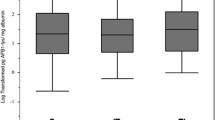
After the meeting at various schools, the researchers crosschecked all consent forms and questionnaires for accuracies. In cases where consent was not clear, the individual parent was contacted to confirm their decision. In addition, parents were required to provide additional consent by checking YES or NO on the questionnaire form to allow international shipping of samples, use of media files, storage of biospecimens, and publication of anonymized data summaries. Parents were also asked to provide about 150 g of household maize flour or kernels for AF measurements of household food. Only healthy children between the ages of 6 and 12 with no current active medication were enrolled in the study. After obtaining assent, the study personnel obtained anthropometric measurements including height, weight, and mid-upper arm circumference; 6–8 ml of venous blood; and 15 ml of urine samples. Collection of urine samples was discontinued due to budget constraints and the labor-intensive nature of collecting urine from children. Figure 2 shows a flow diagram showing the study participants’ recruitment and enrollment.
Laboratory and data analysis planned
Dietary exposure to AFs can be estimated by quantifying contamination levels in food samples, estimates from dietary intake surveys, and food frequency questionnaires. However, the heterogenous nature of AF contamination in food products does not provide accurate measurement of personal exposures. Therefore, in addition to estimating AF contamination in foods, combinations of AF biomarkers either in blood serum, plasma, tissues, or urine are recommended for studies to determine actual exposure in human sub-populations [42, 43]. Once ingested, AFs undergo metabolism and their metabolites are known to irreversibly bind to protein albumin to form AFB1-lysine adducts which are validated biomarkers of AF exposures [44, 45]. Laboratory analyses of this study are currently ongoing, and the study timeline is summarized in Table 1. In addition to quantification of AFB1-lysine adducts in serum samples and total AFs in household maize products, plans are underway to quantify other AF metabolites in urine using High Pressure Liquid Chromatography with Fluorescence Detection [44, 45]. STATA15 (College Station, TX), SAS v9.4 (Cary, NC), and R (Vienna, Austria) will be used in adjusting for socioeconomic factors and other possible confounding variables to model data that is likely to associate AF exposure to adverse health outcomes.
Discussion
This is the first study designed to establish a baseline AF exposure in children between the ages of 6 and 12 years. To date, studies to establish AF exposure have been completed in populations of children below the age of 5 years, adults between the ages of 18 and 65 years, vulnerable populations of pregnant women, and immunocompromised groups including individuals suffering from HIV/AIDS and hepatitis B virus [6, 12, 46, 47]. Moreover, these studies tend to address specific adverse health outcomes including immune suppression, micronutrient levels, possible growth impairment, and risks of carcinogenesis without controlling for related outcomes. For instance, studies aimed to assess the effect of AF exposure on children’s growth in Benin and Togo prioritized possible growth impairments and micronutrient levels in blood plasma while immune markers were not evaluated [48, 49]. Conversely, a study in Ghana prioritized evaluation of immune suppression as it relates to AF exposure while neither micronutrient markers nor growth indicators were considered [50]. Studies in farm animals and human sub-populations have reported downstream effects associated with AF exposure, malnutrition, immune suppression, vulnerability to infectious diseases, and consequently growth impairments [10, 12, 51]. Intervention studies such as use of enterosorbents like Novasil Clay to bind AF adducts in human blood have been evaluated for safety, palatability, and efficacy [52,53,54,55]. In a phase II clinical trial, 180 adults aged 18 to 58 years at risk of aflatoxicosis who received Novasil Clay capsules significantly had lower AFB1-lysine adducts in both blood and urine samples in a dose-dependent manner [55]. Other interventions involving use of green tea polyphenols [56] and chlorophyllin [57] have been shown to reduce AF biomarkers and may also form basis for future prospective studies. The current study protocol provides a multifaceted approach in addressing adverse health outcomes linked to dietary exposure to AFs while controlling for social, economic, and demographic factors. While the mechanism by which AFs contribute to adverse health outcomes is currently unknown, it is suspected to be biological [58].
Given the multifaceted aspects of this study, lessons that may be valuable to other scientists seeking to undertake research projects in low- or middle-income countries are outlined herein. First, plan the study at least 2 to 3 years in advance before actual fieldwork to give you and your team sufficient time to prepare, apply for ethics justification, follow up different requirements, and obtain additional permissions required to conduct field studies involving human subjects. Our study’s ethical approval was prolonged because it involved children.
In addition, travel to your country of interest to build social capital. Moreover, foreign scientists are likely to be more successful if they work collaboratively with local scientists in low- and middle-income countries. It is also important to familiarize oneself with myths and beliefs in a community as blood draw is a contentious issue in some communities. In our study populations, a common belief that blood products can used for financial profit by researchers was prohibitive. Moreover, study administrators must make it clear to participants that their samples will be shipped for analysis to a different location and obtain consent for shipment which must be approved a priori by the ethics committee. The paperwork associated with additional approvals for sample shipment, export, and import can be extensive and thorough. Last but not least, remuneration of field workers can exponentiate overhead costs.
Study limitations
The study administrators are not ethically allowed to contact participants in the future, and thus, study results cannot be used to analyze behavior change or determine cause and effect. Based on results from this study, a prospective cohort study will be valuable in further studies aimed at explaining adverse health effects associated with AF exposure.
We expect AF exposures to be high in May, June, and July because it is rainy and humid, and most farmers have a surplus of harvested grains from the earlier season which are highly susceptible to AF contamination. Nonetheless, this is not guaranteed as factors such as community education programs to promote AF awareness, diet diversification, and food security in some regions where study participants were recruited may be associated with decreased AF exposures.
Conclusions
This paper describes a protocol of the first school-based randomized cross-sectional study aimed at assessing health effects associated with exposure to AFs through the diet. Whether or not a relationship is found between AF exposure and adverse health outcomes, the results can be used to prioritize AF control efforts not only in Kenya but also in other developing countries.
The strength of the study is its multifaceted approach in assessing health effects in children exposed to AFs through the diet. In addition, recruiting subjects from both a high and a low exposure region is instrumental in elucidating the role of AF exposure specifically on micronutrient deficiency, immune suppression, and possible growth impairments.
In conclusion, exposure to AFs and other mycotoxins in low- and middle-income countries has been shown to contribute to immune suppression and growth impairment. Mycotoxins are also suspected to interfere with vaccine efficiency making children more vulnerable to increased risk of infectious diseases. Pediatricians and clinicians in developing nations should pay attention to the role of not only AFs but also other environmental factors that influence health in their practice to better serve their populations.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study. Only study investigators will have access to the final dataset.
References
CAST. Mycotoxins: risks in plant, animal, and human systems. Ames: Council for Agricultural Science and Technology; 2003.
IARC. Some naturally occurring substances: food items and constituents, heterocyclic aromatic amines and mycotoxins. IARC monographs on the evaluation of the carcinogenic risk of chemicals to humans. Geneva: World Health Organization; 1993.
IARC. Monographs on the evaluation of carcinogenic risks to humans. Vol. 82, some traditional herbal medicines, some mycotoxins, naphthalene and styrene. Phytochemistry. 2004;65(1):139.
Williams JH, Phillips TD, Jolly PE, Stiles JK, Jolly CM, Aggarwal D. Human aflatoxicosis in developing countries: a review of toxicology, exposure, potential health consequences, and interventions. Am J Clin Nutr. 2004;80(5):1106–22.
Liu Y, Wu F. Global burden of aflatoxin-induced hepatocellular carcinoma: a risk assessment. Environ Health Perspect. 2010;118(6):818–24.
Wang J-S, Huang T, Su J, Liang F, Wei Z, Liang Y, et al. Hepatocellular carcinoma and aflatoxin exposure in Zhuqing Village, Fusui County, People’s Republic of China. Cancer Epidemiol Biomarkers. 2001;10(2):143–6.
Kew MC. Aflatoxins as a cause of hepatocellular carcinoma. J Gastrointestin Liver Dis. 2013;22(3):305–10.
Magnussen A, Parsi MA. Aflatoxins, hepatocellular carcinoma and public health. World J Gastroenterol. 2013;19(10):1508–12.
Jiang Y, Jolly PE, Ellis WO, Wang JS, Phillips TD, Williams JH. Aflatoxin B1 albumin adduct levels and cellular immune status in Ghanaians. Int Immunol. 2005;17(6):807–14.
Githanga D, Wangia RN, Mureithi MW, Wandiga S, Mutegi C, Ogutu B, et al. The effects of aflatoxin exposure on hepatitis B-induced immunity in Kenyan children. Curr Probl Pediatr Adolesc Health Care. 2019;49:117-30.
IARC Working Group Reports. Mycotoxin control. In: Wild CP, Miller JD, Groopman J, editors. Low and middle income countries. International Agency for Research on Cancer: Lyon; 2015. p. 54.
Khlangwiset P, Shephard GS, Wu F. Aflatoxins and growth impairment: a review. Crit Rev Toxicol. 2011;41(9):740–55.
Obuseh FA, Jolly PE, Kulczycki A, Ehiri J, Waterbor J, Desmond RA, et al. Aflatoxin levels, plasma vitamins A and E concentrations, and their association with HIV and hepatitis B virus infections in Ghanaians: a cross-sectional study. J Int AIDS Soc. 2011;14:53.
Kamala A, Shirima C, Jani B, Bakari M, Sillo H, Rusibamayila N, et al. Outbreak of an acute aflatoxicosis in Tanzania during 2016; 2018. p. 311–20.
Ngindu A, Johnson BK, Kenya PR, Ngira JA, Ocheng DM, Nandwa H, et al. Outbreak of acute hepatitis caused by aflatoxin poisoning in Kenya. Lancet. 1982;1(8285):1346–8.
Narsimha Reddy B, Raghu Raghavender C. Outbreaks of aflatoxicoses in india. Afr J Food Agricult Nutr Dev. 2007;7:1-15.
Mwanda OW, Otieno CF, Omonge E. Acute aflatoxicosis: case report. East Afr Med J. 2005;82(6):320–4.
United States CDC. Outbreak of aflatoxin poisoning--eastern and central provinces, Kenya, January-July 2004. MMWR Morb Mortal Wkly Rep. 2004;53(34):790–3.
Wangia RN. Deaths from consumption of contaminated maize in eastern province, Kenya.https://www.researchgate.net/profile/Wangia_Ruth/publication/330566740_DEATHS_FROM_CONSUMPTION_OF_CONTAMINATED_MAIZE_IN_EASTERN_PROVINCE/links/5c48c4ea92851c22a38b6c85/DEATHS-FROM-CONSUMPTION-OF-CONTAMINATED-MAIZE-IN-EASTERN-PROVINCE.pdf Accessed 15 Aug 2019.
Lewis L, Onsongo M, Njapau H, Schurz-Rogers H, Luber G, Kieszak S, et al. Aflatoxin contamination of commercial maize products during an outbreak of acute aflatoxicosis in Eastern and Central Kenya; 2005. p. 1763.
Daniel JH, Lewis LW, Redwood YA, Kieszak S, Breiman RF, Flanders WD, et al. Comprehensive assessment of maize aflatoxin levels in Eastern Kenya, 2005-2007. Environ Health Perspect. 2011;119(12):1794–9.
USFDA. Guidance for industry: action levels for poisonous or deleterious substances in human food and animal feed. College Park; 2000. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-action-levels-poisonous-or-deleterious-substances-human-food-and-animal-feed#afla. Accessed 15 Feb 2019.
European Commission. Commission regulation (EC) no 1881/2006 setting maximum levels for certain contaminants in foodstuffs. 2006.
East African Community. Maize grains - specifications. Arusha; 2013. https://d3n8a8pro7vhmx.cloudfront.net/eatradehub/pages/754/attachments/original/1432219607/EAS_2-2013__Maize_grains_-_Specification_(1).pdf?1432219607. Accessed 10 Feb 2019.
Yard EE, Daniel JH, Lewis LS, Rybak ME, Paliakov EM, Kim AA, et al. Human aflatoxin exposure in Kenya, 2007: a cross-sectional study. Food Addit Contam A. 2013;30(7):1322–31.
CIAT. Kenya county climate risk profile series. Informing sub-national climate smart agriculture investments in Kenya. Wageningen: Consultative Group for International Agricultural Research [CGIAR]; 2016. Available at https://ccafs.cgiar.org/publications/kenya-county-climate-risk-profiles. Accessed 10 Feb 2019.
Kilonzo RM, Imungi JK, Muiru WM, Lamuka PO, Njage PM. Household dietary exposure to aflatoxins from maize and maize products in Kenya. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2014;31(12):2055–62.
Kenya Bureau of Statistics. Kenya demographic and health survey. 2015.
Ekpa O, Palacios-Rojas N, Kruseman G, Fogliano V, Linnemann AR. Sub-Saharan African maize-based foods: technological perspectives to increase the food and nutrition security impacts of maize breeding programmes. Glob Food Secur. 2018;17:48–56.
De Groote H, Kimenju SC. Consumer preferences for maize products in urban Kenya. Food Nutr Bull. 2012;33(2):99–110.
Bukania ZN, Mwangi M, Karanja RM, Mutisya R, Kombe Y, Kaduka LU, et al. Food insecurity and not dietary diversity is a predictor of nutrition status in children within semiarid agro-ecological zones in Eastern Kenya. J Nutr Metab. 2014;2014:907153.
Kennedy LG. Evaluation of dietary diversity scores for assessment of micronutrient intake and food security in developing countries. Wageningen: Wageningen University; 2009.
Vhurumuku E. Food security indicators. Nairobi, Food and Agriculture Organization; 2014.
Wangia RN, Githanga DP, Xue KS, Tang L, Anzala OA, Wang JS. Validation of urinary sphingolipid metabolites as biomarker of effect for fumonisins exposure in Kenyan children. Biomarkers. 2019;24:379-88.
Azziz-Baumgartner E, Lindblade K, Gieseker K, Rogers HS, Kieszak S, Njapau H, et al. Case-control study of an acute aflatoxicosis outbreak, Kenya, 2004. Environ Health Perspect. 2005;113(12):1779–83.
Probst C, Njapau H, Cotty PJ. Outbreak of an acute aflatoxicosis in Kenya in 2004: identification of the causal agent. Appl Environ Microbiol. 2007;73(8):2762–4.
Muture BN, Ogana G. Aflatoxin levels in maize and maize products during the 2004 food poisoning outbreak in Eastern Province of Kenya. East Afr Med J. 2005;82(6):275–9.
Vemaps.com. Kenya with Provinces - Multicolor. In: KE-EPS-01-0002, editor. online2017. https://vemaps.com/kenya/ke-07. Accessed 13 Oct 2017.
Kenya National Bureau of Statistics. The 2009 Kenya Population and housing Census 2010.
Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970;30(3):607–10.
Leslie K. A procedure for objective respondent selection within the household. J Am Stat Assoc. 1949;44(247):380.
Strickland PT, Groopman JD. Biomarkers for assessing environmental exposure to carcinogens in the diet. Am J Clin Nutr. 1995;61(3 Suppl):710s–20s.
Hall AJ, Wild CP. Aflatoxin biomarkers. Lancet. 1992;339(8806):1413–4.
Qian G, Tang L, Liu W, Wang JS. Development of a non-antibody method for rapid detection of serum aflatoxin b1-lysine adduct. Toxicologist. 2010;114:248.
Wang JS, Abubaker S, He X, Sun G, Strickland PT, Groopman JD. Development of aflatoxin B(1)-lysine adduct monoclonal antibody for human exposure studies. Appl Environ Microbiol. 2001;67(6):2712–7.
Turner PC, Sylla A, Gong YY, Diallo MS, Sutcliffe AE, Hall AJ, et al. Reduction in exposure to carcinogenic aflatoxins by postharvest intervention measures in West Africa: a community-based intervention study. Lancet. 2005;365(9475):1950–6.
Williams JH, Grubb JA, Davis JW, Wang JS, Jolly PE, Ankrah NA, et al. HIV and hepatocellular and esophageal carcinomas related to consumption of mycotoxin-prone foods in sub-Saharan Africa. Am J Clin Nutr. 2010;92(1):154–60.
Gong YY, Cardwell K, Hounsa A, Egal S, Turner PC, Hall AJ, et al. Dietary aflatoxin exposure and impaired growth in young children from Benin and Togo: cross sectional study. BMJ. 2002;325(7354):20–1.
Gong Y, Hounsa A, Egal S, Turner PC, Sutcliffe AE, Hall AJ, et al. Postweaning exposure to aflatoxin results in impaired child growth: a longitudinal study in Benin, West Africa. Environ Health Perspect. 2004;112(13):1334–8.
Jolly PE, Shuaib FM, Jiang Y, Preko P, Baidoo J, Stiles JK, et al. Association of high viral load and abnormal liver function with high aflatoxin b1-albumin adduct levels in hiv-positive ghanaians: Preliminary observations. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2011;(28):1224-34.
Owaga E, Muga R, Mumbo H, Aila F. Chronic dietary aflatoxins exposure in Kenya and emerging public health concerns of impaired growth and immune suppression in children. Int J Biol Chem Sci. 2011;5(3):1325-36.
Awuor AO, Yard E, Daniel JH, Martin C, Bii C, Romoser A, et al. Evaluation of the efficacy, acceptability and palatability of calcium montmorillonite clay used to reduce aflatoxin B1 dietary exposure in a crossover study in Kenya. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2017;34(1):93–102.
Mitchell NJ, Kumi J, Aleser M, Elmore SE, Rychlik KA, Zychowski KE, et al. Short-term safety and efficacy of calcium montmorillonite clay (UPSN) in children. Am J Trop Med Hyg. 2014;91(4):777–85.
Afriyie-Gyawu E, Ankrah NA, Huebner HJ, Ofosuhene M, Kumi J, Johnson NM, et al. NovaSil clay intervention in Ghanaians at high risk for aflatoxicosis. I. Study design and clinical outcomes. Food Addit Contam. 2008;25(1):76–87.
Wang P, Afriyie-Gyawu E, Tang Y, Johnson NM, Xu L, Tang L, et al. NovaSil clay intervention in Ghanaians at high risk for aflatoxicosis: II. Reduction in biomarkers of aflatoxin exposure in blood and urine. Food Addit Contam. 2008;25(5):622–34.
Luo H, Xu L, Tang L, Tang M, Cox SB, Gao W, et al. Modulation of aflatoxin biomarkers in human blood and urine by green tea polyphenols intervention. Carcinogenesis. 2008;29(2):411–7.
Egner PA, Wang JB, Zhu YR, Zhang BC, Wu Y, Zhang QN, et al. Chlorophyllin intervention reduces aflatoxin-DNA adducts in individuals at high risk for liver cancer. Proc Natl Acad Sci U S A. 2001;98(25):14601–6.
Hoffmann V, Jones K, Leroy J. Mitigating aflatoxin exposure to improve child growth in eastern Kenya: study protocol for a randomized controlled trial. Trials. 2015;16:552.
Acknowledgements
We thank the county governments and communities in Siaya and Makueni Counties for supporting this study. We also thank all the different school administrations and field assistants without whom this work may not be possible.
Funding
Field work and data collection was supported through small grants from the University of Georgia namely Interdisciplinary and Innovative Research Grant and the Tipton Golias Travel Award. Ongoing laboratory analyses are supported by research grant ECG-A-00-07-00001-00 from US Agency for International Development (USAID) Feed the Future Peanut and Mycotoxin Innovation Laboratory. The funders had no role in the design of the study, data collection, laboratory analyses, interpretation of data, writing of this manuscript, and decision to publish the results.
Author information
Authors and Affiliations
Contributions
RNW conceptualized the study and drafted the manuscript in consultation with DPG, OAA, and JSW. All authors read the manuscript for accuracy and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Joint Ethics Committee of the University of Nairobi and Kenyatta National Hospital in Kenya approved the research protocol and procedure for study referenced P741/12/2017. Study purpose, objectives, and expected outcomes were explained in local dialect to participants, and all concerns were addressed before enrollment. Both parental consent and child assent were obtained from participants.
Consent for publication
Only participants who agreed to the publication of de-identified data were enrolled in the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wangia, R.N., Githanga, D.P., Wang, JS. et al. Aflatoxin exposure in children age 6–12 years: a study protocol of a randomized comparative cross-sectional study in Kenya, East Africa. Pilot Feasibility Stud 5, 141 (2019). https://doi.org/10.1186/s40814-019-0510-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-019-0510-x