Abstract
Background
The value of noninvasive assessment of carotid plaque composition in identifying patients with high coronary risk remains elusive. We sought to determine whether and which carotid plaque components are associated with prior coronary events independent of traditional risk factors and plaque burden.
Methods
Asymptomatic subjects with 50-79 % carotid stenosis by ultrasound were imaged with a multi-contrast carotid MRI protocol at 1.5 T. The independent associations between plaque components (fibrous tissue, calcification, lipid-rich necrotic core [LRNC] and intraplaque hemorrhage [IPH]) and prior coronary events, including myocardial infarction and coronary revascularization, were evaluated by controlling for traditional risk factors and plaque burden metrics.
Results
A total of 159 subjects (69.7 ± 9.0 years, 84 % males) were included. Prior coronary events were documented in 66 (42 %) subjects, and were associated with a larger carotid plaque burden consisting of more LRNC and calcification. Additionally, a higher prevalence of IPH was observed in subjects with prior coronary events (32 % vs. 15 %, p = 0.019). In multivariate analysis, the percent wall volume was an independent discriminator among plaque burden metrics after accounting for traditional risk factors (odds ratio per 1-SD increase: 1.7 [1.2, 2.6]); the presence of IPH remained as a significant discriminator after accounting for traditional risk factors and percent wall volume (odds ratio: 2.9 [1.1, 7.6]) while other compositional metrics did not.
Conclusions
IPH in the carotid artery was independently associated with prior coronary events. IPH imaging may provide incremental information on patients’ coronary risk beyond traditional risk factors and carotid plaque burden assessment.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Because of the systemic nature of atherosclerosis, subclinical carotid disease has long been used as a surrogate of coronary artery disease (CAD). Measurements on carotid plaque burden have been shown to predict the extent and clinical risk of underlying CAD [1–4], whereas the value of carotid plaque composition, although widely believed to indicate lesion instability, remains elusive for the evaluation of CAD risk.
Assessment of carotid plaque composition has been available via noninvasive imaging, which potentially can provide clinicians with incremental information on patients’ coronary risk. Recently, the echolucent carotid plaques by ultrasound [5] and those with high-intensity signals by T1-weighted magnetic resonance imaging (MRI) [6] were shown to predict future coronary events independent of clinical risk factors. However, compositional features are known to have positive relationships with plaque burden [7, 8], and their added value will not be clear unless tested against plaque morphological metrics.
In this study, we sought to test whether and which carotid plaque compositional metrics confer incremental values for discriminating prior coronary events in subjects with subclinical carotid disease. While all subjects in this study had imaging evidence of atherosclerosis, those with prior coronary events were considered to be at a much higher risk for future events [9]. We hypothesized that specific markers on carotid plaque composition could help identify subjects with prior coronary events and thus serve as novel markers for vulnerable patients. Carotid MRI provides comprehensive plaque morphological measurements, and is a validated tool for detecting major plaque components in vivo [10–12].
Methods
Study population
Subjects in a previously-established cohort were included in this retrospective study [13]. Briefly, asymptomatic subjects with substantial carotid plaques were recruited in this exploratory study to include a wide spectrum of compositional phenotypes. Specific criteria were: 1) 50-79 % stenosis by duplex ultrasound in at least one carotid artery; 2) neurologically asymptomatic defined as no cerebrovascular symptoms in the 6 months prior to enrollment; 3) no prior carotid endarterectomy (CEA), neck radiation or contraindications for MRI (e.g. metal implants, claustrophobia). Enrolled subjects completed a standardized health questionnaire covering demographics and cardiovascular risk factors (smoking, hypertension, hypercholesterolemia, and diabetes mellitus) [13]. Smoking was self-reported and included former smoking and current smoking. Hypertension was defined as systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg, or taking anti-hypertensive agents. Diabetes was defined as previously confirmed diagnosis and/or use of anti-diabetic agents. Hypercholesterolemia was defined as a history of total cholesterol > 5 mmol/l and/or low-density lipoprotein cholesterol (LDL-C) > 3 mmol/l, or taking lipid-lowering medications. Prior coronary events were collected and verified by chart review. A positive history of coronary events was defined as having one or more of the following events: 1) hospitalization for myocardial infarction; 2) coronary revascularization including angioplasty, stenting and coronary artery bypass graft (CABG). All study procedures were reviewed and approved by the institutional review board. Subjects provided informed consent before enrollment.
MRI Protocol
All scans were performed on a 1.5 T scanner (Signa Horizon EchoSpeed, GE Healthcare, Milwaukee, Wisconsin, USA) using phased-array surface coils (Pathway, Seattle, Washington, USA). A previously published standardized protocol [14, 15] was used to acquire cross-sectional, multi-contrast images (3-dimensional time-of-flight [TOF], T1-weighted, proton density-weighted [PD], and T2-weighted) that were centered at the carotid bifurcation of the side with 50-79 % stenosis. No contrast agent was used to increase patient recruitment and compliance. Previous studies have shown that this non-contrast protocol was able to characterize major plaque components [10, 13]. All images were obtained with field-of-view of 13 to 16 cm, matrix size of 256 × 256, and slice thickness of 2 mm. Scan coverage was 40 mm for TOF, 20–24 mm for T1-weighted, and 30 mm for proton density-weighted and T2-weighted sequences. Total acquisition time was approximately 30 min.
Image analysis
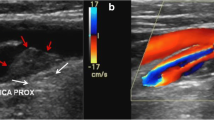
Eight reviewers with at least 1-year experience in MR plaque imaging participated in image analysis while blinded to clinical data using a custom-designed image analysis software package (CASCADE, University of Washington, Seattle, Washington, USA) [16]. Only the index artery, defined as the side with 50-70 % stenosis by ultrasound, was analyzed. The four contrast weightings (TOF, T1, PD, and T2) were registered using the carotid bifurcation as a landmark. Lumen and outer wall boundaries were outlined on each cross-sectional slice as well as plaque components that were determined using previous published criteria (Figure 1) [10, 12]. Briefly, calcification appears hypointense on all weightings; intraplaque hemorrhage (IPH) appears hyperintense on TOF and T1-weighted images; lipid-rich necrotic core (LRNC) usually appears hypointense on T2- and PD-weighted images but may have variations if it contains IPH [12]. Remaining wall areas were classified as fibrous tissue. Subsequently, maximum wall thickness, maximum percent wall area (100 % × wall area/total vessel area), percent wall volume (100 % × wall volume/total vessel volume), were calculated. Percent volumes of calcification and LRNC and the presence/absence of IPH were also calculated and/or recorded. All imaging data were based on consensus opinion of at least two reviewers.
Carotid plaque burden and composition detected by combined use of multiple MR weightings at 1.5 T. Arrows indicate lipid-rich necrotic core as hypointense areas on T2W images. Arrowheads indicate intraplaque hemorrhage as hyperintense areas on TOF images. PDW = proton-density-weighted; T1W = T1-weighted; T2W = T2-weighted; TOF = time-of-flight
Statistical analysis
All data are presented as mean ± standard deviation (SD) for continuous variables and count with percentage for categorical variables. Subjects were stratified according to a positive or negative history of prior coronary events. Clinical and imaging characteristics were compared between the two groups using the independent t-test, Mann–Whitney test, and Fisher’s exact test, as appropriate. The incremental values of: 1) carotid plaque morphological metrics over clinical variables; and 2) compositional metrics over clinical variables and morphological metrics, for discriminating prior coronary events, were examined using multivariate logistic regression analysis and presented as odds ratios (OR) with 95 % confidence interval (CI). To examine the influence of plaque burden on the ability of compositional metrics for discriminating prior coronary events, interactions between plaque morphological and compositional metrics were also tested. All data analyses were performed using R 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria). Statistical significance was defined as P < 0.05.
Results
Clinical and imaging characteristics
Table 1 summarizes the clinical and imaging characteristics of the study population (N = 159). Prior coronary events were documented in 66 (42 %) subjects. Compared to subjects without prior coronary events, those with prior coronary events had a higher prevalence of hypercholesterolemia (92 % vs. 70 %, p = 0.001), and were more frequently on statin therapy (82 % vs. 52 %, p < 0.001), but otherwise had similar clinical profiles (Table 1). Observed differences in carotid plaques included larger plaques, less fibrous tissue, and a higher prevalence of IPH in subjects with prior coronary events (Table 1).
Incremental value of carotid plaque morphology
All three morphological metrics of plaque burden were significantly associated with prior coronary events (Table 2). The OR for prior coronary events ranged from 1.4 to 1.8 per 1-SD increase in maximum wall thickness, maximum percent wall area, and percent wall volume. Percent wall volume not only appeared to be the strongest discriminator amongst the plaque morphological metrics for prior coronary events, but also remained significant after adjusting for demographics and clinical risk factors (OR: 1.7 [1.2, 2.6] per 1-SD increase, p = 0.005).
Incremental value of carotid plaque composition
Among carotid plaque compositional metrics, a lower percent volume of fibrous tissue and presence of IPH were associated with a positive history of coronary events (Table 3). After adjusting for clinical risk factors, as well as percent wall volume, the presence of IPH remained as a significant discriminator for prior coronary events (OR: 2.9 [1.1, 7.6], p = 0.033).
Plaque burden did not appear to influence the ability of IPH to discriminate subjects with prior coronary events (p-value ranged from 0.40 to 0.99 for interactions). Fig. 2 shows the association between IPH and prior coronary events in different subgroups defined by carotid plaque morphological metrics. Of note, all subjects in the lower half of maximum wall thickness and with IPH had prior coronary events.
Discussion
By using carotid MRI, we were able to evaluate and compare carotid plaque morphological and compositional metrics in relation to coronary plaque vulnerability, defined as having prior coronary events in this study. The most pronounced difference in carotid plaque morphology between subjects with and without prior coronary events was shown in percent wall volume. Furthermore, the incremental value of carotid plaque composition for discriminating prior coronary events, specifically the presence of IPH, was demonstrated by accounting for clinical risk factors as well as percent wall volume. In addition to some pathophysiological insights, our findings indicate that a combination of three-dimensional plaque characterization and IPH detection in the assessment of subclinical carotid atherosclerosis may offer the most promising information on patients’ coronary risk.
Carotid plaque detection by B-mode ultrasound has been shown to improve individual risk assessment compared to the intima-media thickness [4]. The introduction of novel ultrasound techniques provides additional opportunities to optimize this approach through improved plaque characterization [17, 18]. This concept is further supported by autopsy findings showing that vulnerable features tend to be present at multiple arterial beds within the same individual [19, 20]. To determine what information embedded in carotid plaque tissue composition are relevant to coronary risk, we used carotid MRI to compare carotid plaque compositional metrics between subjects with and without prior coronary events. Carotid MRI gives a comprehensive assessment of local plaque burden by capturing both luminal stenosis and outward remodeling. Additionally, combining MRI contrast weightings has been shown to be able to characterize plaque components [10, 11]. Therefore, multiple morphological and compositional metrics can be compared head-to-head in a single study.
The presence of IPH in the carotid artery was found to be an additional indicator for coronary vulnerability, with an odds ratio of 2.9 (95 % CI: 1.1-7.6) for prior coronary events after adjustment for clinical variables and percent wall volume. The observation is consistent with a previous histopathological study by Hellings et al. [21] in which carotid IPH identified by post-surgical examination of carotid endarterectomy specimens was associated with systemic cardiovascular outcomes. It was noted that the observed relationship between carotid IPH and coronary events alone was more marginal (hazard ratio: 1.6, 95 % CI: 0.9-3.0) [21]. Surgical patients have end-stage plaques and are frequently symptomatic whereas our study included only asymptomatic subjects with moderate carotid disease. After stratifying our study population by plaque size, there appeared to be no evidence that the relationship between IPH and prior coronary events varied in those with high or low plaque burden. Nonetheless, subjects with IPH but not much wall thickening may represent a unique group for further investigations (Fig. 2). Collectively, existing evidence suggests clinicians to note the increased coronary risk if IPH is detected in the carotid artery, particularly in those with asymptomatic carotid lesions.
In contrast to IPH, other plaque components did not show incremental discriminative power over plaque morphological assessment. Subjects with prior coronary events had significantly less fibrous tissue in the carotid plaque, due to increase in both calcification and lipid core. However, such an association was largely accounted for by clinical risk factors and concomitantly larger percent wall volume.
Natural history studies have revealed that most coronary events were preceded by rapid plaque expansion that was unusual and unrelated to baseline plaque burden [22–24]. IPH, with the capability to induce changes in plaque behavior [25], may play a critical role in the pathogenesis of coronary events. In a postmortem study, Fleiner et al. described that the hyperplasia of vasa vasorum was a systemic feature of symptomatic patients [20]. As adventitial vasa vasorum is a major source of IPH [26], the finding by Fleiner et al. supports the conjecture that carotid IPH indicates increased probability of coronary IPH. Another study by Moreno et al. also sheds light by showing that genotypes related to hemoglobin clearance may determine one’s susceptibility to IPH-induced detrimental effects [27]. It is possible that the presence of carotid IPH by MRI indicates certain genetic vulnerabilities related to IPH metabolism. Nonetheless, given the limited understanding of the pathophysiology of IPH in the current literature, although IPH in the carotid artery appears to indicate additional systemic factors that contribute to plaque instability, the exact mechanisms remain to be investigated.
Singh et al. [28] also noted a higher prevalence of carotid IPH in patients with prior coronary events. That study included subjects referred for carotid MRI due to suspected neurovascular disease, so the study population appears to be a mixture of symptomatic and asymptomatic subjects. It is conceivable that there would be a wider range of carotid plaque burden in the previous report compared to the present data. As IPH is known to be associated with a larger plaque burden [29], a wider range of plaque burden in study population makes it difficult to argue that the observed relationship is not due to the higher plaque burden associated with IPH but related to the unique pathophysiology of IPH. In the present study, by including subjects with similar extent of carotid disease and quantifying plaque burden in a three-dimensional fashion, we were able to test the independent association between carotid IPH and coronary events rigorously. In this study, plaque morphological measurements were derived from MRI rather than ultrasound which is more widely used in clinical practice. However, MRI provides multiple plaque morphological metrics, and therefore the incremental value of carotid plaque composition could be rigorously tested. The maximum wall thickness measures plaque burden at a single location. The maximum percent wall area measures a single slice and essentially indicates luminal narrowing after taking into account outward remodeling, which is similar to stenosis measurement on black-blood carotid MRI proposed by Babiarz et al. [30]. The percent wall volume, as a 3-dimensional metric, is similar to the percent atheroma volume that is used in intravascular ultrasound studies of coronary vasculature [31]. Among the three morphological metrics, the percent wall volume was the best discriminator for prior coronary events, supporting the pursuit of 3-dimensional carotid plaque characterization as a future tool in CAD management [32].
Implications
Findings from this study have implications both for understanding the pathophysiology of vulnerable patients and for optimizing clinical management in individuals. Although atherosclerosis becomes highly prevalent as people get older, certain patients are at a particular high risk for clinical events. Our data suggest that carotid IPH was associated with increased risk for coronary events and the association was not explained by differences in traditional risk factors and plaque burden. Thus, it is conceivable that additional systemic factors that relate to the pathogenesis of IPH may be the underlying players, such as the hyperplasia of vasa vasorum and haptoglobin genotype [20, 27]. Accordingly, there is potential for using carotid IPH as a novel marker for high coronary risk in developing medical treatment strategies, which may include more stringent treatment goals for lipid-lowering and anti-hypertensive agents as well as novel agents that can target IPH and its detrimental effects on plaque progression.
Study limitations
There are several limitations of the present study. Our study population is selective in that it only included neurologically asymptomatic subjects with 50-79 % carotid stenosis by ultrasound. Despite the relatively narrow range in stenosis, a wide range in plaque composition was observed and offered a good opportunity to test the incremental value of plaque composition in discriminating prior coronary events. However, it remains to be seen whether the independent association of IPH with coronary events applies to the general population. Due to the retrospective nature of the design, patients with severe coronary events such as coronary death could not be included. We do not expect this selection bias that is present in most clinical research to affect our study findings. But the prevalence of carotid IPH in those with more severe coronary events could be higher than what was seen in this study. In addition, circulating biomarkers, such as C-reactive protein, which have been shown to improve risk appraisal in individuals [33], were not examined in the present study. Therefore, we could not exclude the possibility that the association between IPH and coronary events may be mediated by biomarkers. It is worth mentioning that epidemiological studies using carotid MRI are still sparse, and no biomarkers have been linked with IPH to date.
Conclusions
In conclusion, subjects with prior coronary events had a high prevalence of IPH. The association could not be explained by differences in traditional risk factors and plaque burden. IPH may provide incremental information on patients’ coronary risk, possibly by indicating additional systemic factors that contribute to plaque instability.
References
Kallikazaros I, Tsioufis C, Sideris S, Stefanadis C, Toutouzas P. Carotid artery disease as a marker for the presence of severe coronary artery disease in patients evaluated for chest pain. Stroke. 1999;30:1002–7.
Sabeti S, Schlager O, Exner M, et al. Progression of carotid stenosis detected by duplex ultrasonography predicts adverse outcomes in cardiovascular high-risk patients. Stroke. 2007;38:2887–94.
Rundek T, Arif H, Boden-Albala B, Elkind MS, Paik MC, Sacco RL. Carotid plaque, a subclinical precursor of vascular events: the Northern Manhattan Study. Neurology. 2008;70:1200–7.
Brook RD, Bard RL, Patel S, et al. A Negative Carotid Plaque Area Test Is Superior to Other Noninvasive Atherosclerosis Studies for Reducing the Likelihood of Having Underlying Significant Coronary Artery Disease. Arterioscler Thromb Vasc Biol. 2006;26:656–62.
Honda O, Sugiyama S, Kugiyama K, et al. Echolucent carotid plaques predict future coronary events in patients with coronary artery disease. J Am Coll Cardiol. 2004;43:1177–84.
Noguchi T, Yamada N, Higashi M, Goto Y, Naito H. High-Intensity Signals in Carotid Plaques on T1-Weighted Magnetic Resonance Imaging Predict Coronary Events in Patients With Coronary Artery Disease. J Am Coll Cardiol. 2011;58:416–22.
AbuRahma AF, Wulu JT, Crotty B. Carotid Plaque Ultrasonic Heterogeneity and Severity of Stenosis. Stroke. 2002;33:1772–5.
Turc G, Oppenheim C, Naggara O, et al. Relationships between recent intraplaque hemorrhage and stroke risk factors in patients with carotid stenosis: the HIRISC study. Arterioscler Thromb Vasc Biol. 2012;32:492–9.
Cho E, Rimm EB, Stampfer MJ, Willett WC, Hu FB. The impact of diabetes mellitus and prior myocardial infarction on mortality from all causes and from coronary heart disease in men. J Am Coll Cardiol. 2002;40:954–60.
Saam T, Ferguson MS, Yarnykh VL, et al. Quantitative evaluation of carotid plaque composition by in vivo MRI. Arterioscler Thromb Vasc Biol. 2005;25:234–9.
Cappendijk VC, Cleutjens KBJM, Kessels AGH, et al. Assessment of Human Atherosclerotic Carotid Plaque Components with Multisequence MR Imaging: Initial Experience1. Radiology. 2005;234:487–92.
Yuan C, Mitsumori LM, Ferguson MS, et al. In vivo accuracy of multispectral magnetic resonance imaging for identifying lipid-rich necrotic cores and intraplaque hemorrhage in advanced human carotid plaques. Circulation. 2001;104:2051–6.
Takaya N, Yuan C, Chu BC, et al. Association between carotid plaque characteristics and subsequent ischemic cerebrovascular events: a prospective assessment with MRI - initial results. Stroke. 2006;37:818–23.
Cai JM, Hatsukami TS, Ferguson MS, Small R, Polissar NL, Yuan C. Classification of human carotid atherosclerotic lesions with in vivo multicontrast magnetic resonance imaging. Circulation. 2002;106:1368–73.
Yarnykh VL, Yuan C. High-Resolution Multi-Contrast MRI of the Carotid Artery Wall for Evaluation of Atherosclerotic Plaques, in Current Protocols in Magnetic Resonance Imaging. Wiley: New York; 2004.
Kerwin WS, Xu D, Liu F, et al. Magnetic resonance imaging of carotid atherosclerosis: plaque analysis. Top Magn Reson Imaging. 2007;18:371–8.
Landry A, Spence JD, Fenster A. Measurement of Carotid Plaque Volume by 3-Dimensional Ultrasound. Stroke. 2004;35:864–9.
Kim K, Huang SW, Hall TL, Witte RS, Chenevert TL, O'Donnell M. Arterial vulnerable plaque characterization using ultrasound-induced thermal strain imaging (TSI). IEEE Trans Biomed Eng. 2008;55:171–80.
Vink A, Schoneveld AH, Richard W, et al. Plaque burden, arterial remodeling and plaque vulnerability: determined by systemic factors? J Am Coll Cardiol. 2001;38:718–23.
Fleiner M, Kummer M, Mirlacher M, et al. Arterial neovascularization and inflammation in vulnerable patients: early and late signs of symptomatic atherosclerosis. Circulation. 2004;110:2843–50.
Hellings WE, Peeters W, Moll FL, et al. Composition of carotid atherosclerotic plaque is associated with cardiovascular outcome: a prognostic study. Circulation. 2010;121:1941–50.
Glaser R, Selzer F, Faxon DP, et al. Clinical progression of incidental, asymptomatic lesions discovered during culprit vessel coronary intervention. Circulation. 2005;111:143–9.
Stone GW, Maehara A, Lansky AJ, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364:226–35.
Narula J, Nakano M, Virmani R, et al. Histopathologic characteristics of atherosclerotic coronary disease and implications of the findings for the invasive and noninvasive detection of vulnerable plaques. J Am Coll Cardiol. 2013;61:1041–51.
Sun J, Underhill HR, Hippe DS, Xue Y, Yuan C, Hatsukami TS. Sustained acceleration in carotid atherosclerotic plaque progression with intraplaque hemorrhage: a long-term time course study. J Am Coll Cardiol Img. 2012;5:798–804.
Virmani R, Kolodgie FD, Burke AP, et al. Atherosclerotic plaque progression and vulnerability to rupture: angiogenesis as a source of intraplaque hemorrhage. Arterioscler Thromb Vasc Biol. 2005;25:2054–61.
Moreno PR, Purushothaman KR, Purushothaman M, et al. Haptoglobin genotype is a major determinant of the amount of iron in the human atherosclerotic plaque. J Am Coll Cardiol. 2008;52:1049–51.
Singh N, Moody AR, Rochon-Terry G, Kiss A, Zavodni A. Identifying a high risk cardiovascular phenotype by carotid MRI-depicted intraplaque hemorrhage. Int J Cardiovasc Imaging. 2013;29:1477–83.
Zhao X, Underhill HR, Zhao Q, et al. Discriminating Carotid Atherosclerotic Lesion Severity by Luminal Stenosis and Plaque Burden: A Comparison Utilizing High-Resolution Magnetic Resonance Imaging at 3.0 Tesla. Stroke. 2011;42:347–53.
Babiarz LS, Astor B, Mohamed MA, Wasserman BA. Comparison of gadolinium-enhanced cardiovascular magnetic resonance angiography with high-resolution black blood cardiovascular magnetic resonance for assessing carotid artery stenosis. J Cardiovasc Magn Reson. 2007;9:63–70.
Nicholls SJ, Hsu A, Wolski K, et al. Intravascular ultrasound-derived measures of coronary atherosclerotic plaque burden and clinical outcome. J Am Coll Cardiol. 2010;55:2399–407.
Sillesen H, Muntendam P, Adourian A, et al. Carotid plaque burden as a measure of subclinical atherosclerosis: comparison with other tests for subclinical arterial disease in the High Risk Plaque BioImage study. JACC Cardiovasc Imaging. 2012;5:681–9.
Koenig W, Lowel H, Baumert J, Meisinger C. C-reactive protein modulates risk prediction based on the Framingham Score: implications for future risk assessment: results from a large cohort study in southern Germany. Circulation. 2004;109:1349–53.
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
DSH reports grants from GE Healthcare and Philips Healthcare. CY receives research grants from the NIH and Philips Healthcare, and serves as a Member of Radiology Advisory Network, Philips. TSH receives research grants from the NIH and Philips Healthcare. The other authors declare that they have no competing interests.
Authors’ contributions
JS performed the design of the study, analyzed the data, interpreted the data, and drafted the manuscript. DSH participated in study design, contributed to statistical analysis, data interpretation, and revised the manuscript. HRU, BC, TS, NT, JC, MW, WY, LD participated in image analysis, data interpretation, and manuscript revision. CY assisted in the study design, data interpretation, and manuscript revision. TSH carried out the design of the study, interpreted the data and revised the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Sun, J., Hippe, D.S., Underhill, H.R. et al. Incremental value of carotid intraplaque hemorrhage for discriminating prior coronary events. Neurovasc Imaging 1, 5 (2015). https://doi.org/10.1186/s40809-015-0005-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40809-015-0005-y