Abstract
Background
Despite the decline in the rate of stunting in Ethiopia, the prevalence is still high and needs immense efforts to achieve the target set to reduce the prevalence. It varies between localities due to individual level factors and dominant livelihood practice in the community.
Thus, the aim of this study was to determine the prevalence of stunting and identify factors associated with it in Sodo Zuria district in South Ethiopia.
Methods
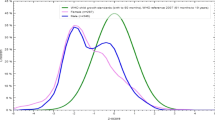
A community based cross sectional study was conducted among 342 children aged 6–59 months paired with mothers/caretakers. Households were selected using systematic sampling. Structured questionnaire was used and mothers/caregivers were interviewed face to face. Standardized anthropometric measurements were used to measure length, and weight and height of a child. Data were entered into Epi Info software version 3.5.1 and exported to SPSS version 20 for analysis. Height for age Z score data were analyzed using WHO Anthro software. Multivariate logistic regression analysis was conducted to identify predictor variables. Statistical significance was considered at p < 0.05.
Results
The prevalence of stunting in this study was 24.9% with 7.9% being severely stunted. Being female (AOR = 2.8; 95% CI: 1.5, 5.3), children aged 12–23 months (AOR = 7.1; 95% CI: 2.3, 21.9), mother’s who do not use family planning (AOR = 2.5; 95% CI: 1.1,5.7), children with diarrheal morbidity (AOR = 2.5; 95% CI: 1.2,5.3), income of 750–1500 ETB and > 1500, and children who received pre-lacteal feeding (AOR = 3.8; 95% CI: 1.2–12.2) became predictors for stunting.
Conclusion
Significant proportion of stunting was found where one third of them were severely stunted. Being female, children aged 12–23 months, using family planning, children with diarrheal morbidity, income and pre-lacteal feeding became predictors for stunting. So Gender-based policies should be enacted in child feeding practice, interventions should focus on the utilization of family planning and appropriate child caring and feeding practices. Water, sanitation and hygiene interventions need to be strengthened.
Similar content being viewed by others
Background
Stunting (low height-for-age) is a sign of chronic undernutrition that reflects failure to receive adequate nutrition over a long period. Children are regarded as stunted when their height-for-age Z-score (HAZ) is below minus two standard deviations (−2SD) from the median of the reference population [1]. Stunting reflects failure to get adequate nutrition over a long period of time and it can be affected by recurrent and chronic illness [2].
Malnutrition leads to serious public health and economic risks, and improvements in nutrition will contribute significantly to reducing poverty, and to achieving health, education, and employment goals [3]. Child undernutrition is highly prevalent in low and middle-income countries and substantially increases mortality and overall disease burden [4]. Globally, 161 million (25%) children under-5 years of age were estimated to be stunted and one third of all stunted children lived in Africa [2]. The highest prevalence of stunting is reported in South Asia (36%) and Sub-Saharan Africa (34%) [5]. In Ethiopia the prevalence of stunting is 38% [1], ranking the country among the top both in sub Saharan Africa and the World.
The World Health Organization [WHO] adopted a resolution with a target to reduce the number of stunted children under-five by 40% in 2025. However, at current rates of progress, stunting level will decrease by 26% in 2025 [6]. Similarly, despite the decline in the rate of stunting from 47% (2005) [7] to 38% (2016) [1] in Ethiopia, the prevalence is still high and needs immense efforts to achieve the target set to reduce the prevalence to 26% in 2020 [8]. Childhood stunting varies between localities due to individual and community-level factors [9, 10] and the factors associated with stunting vary by the dominant livelihood practice in the community [11]. However, there are no documented studies to identify the factors associated with stunting in the study area. Thus, the aim of this study was to determine the prevalence of stunting and identify factors associated with it in Sodo Zuria district in South Ethiopia.
Methods
Study design and setting
A community based cross sectional study was conducted from May to June 2017. Sodo Zuria is 380 km south of Addis Ababa and it has 30 kebeles (lowest administrative units) with a projected population of 394,772; 24,647 were children 6–59 months of age.
Population and sampling
The study population were randomly selected children, 6–59 months of age paired with their mothers/caregivers who resided in the district for at least 6 months. Children with physical disability who are not eligible for anthropometric measurements were excluded from the study. A sample size of 380 was calculated with 95% confidence level, 5% margin of error, an expected stunting prevalence of 38% [1] and non response rate of 5%. Sampling frame was developed for the randomly selected 4 kebeles and the total sample was proportionally allocated to the selected kebeles. Systematic sampling was used to select households and a child was selected randomly in households with more than one eligible children.
Variables
Outcome variable
Stunting which was computed with height for age z-score (HAZ) of less than − 2 standard deviation (SD).
Exposure variables
Socio demographic and economic variables: Maternal age, marital status, religion, ethnicity, maternal education, paternal education, maternal occupation, paternal occupation, household income in Ethiopian birr (ETB), family size, decision making on household resource utilization and age of the child.
Obstetric and other maternal characteristics: Place of delivery, gestational age at birth, birth weight, birth order, pregnancy interval, age at first birth, antenatal care (ANC) follow up, one or more additional meal consumption than usual and utilization of family planning.
Child morbidity
Diarrhea, fever, acute respiratory infections and measles.
Child caring practice
Breast feeding, pre lacteal feeding, complementary feeding, dietary diversity and child vaccination.
Environmental health characteristic
Source and distance of drinking water, availability of latrine, hand washing practice, household waste disposal.
Data collection
Data collectors with prior experience of data collection interviewed mothers/caregivers face to face using pretested and structured questionnaire. The data collectors were trained on the procedures of data collection and were standardized on obtaining anthropometric measurements. A horizontal wooden length board was used to measure the length of children 6–23 months of age. On the other hand, a vertical wooden height board was used to measure the height of children aged 24–59 months. Digital seca weight scale was used to measure the weight of the children and read to the nearest 0.1 kg. All measurements were taken twice and the mean was used for analysis. The data collection was supervised and errors were corrected on spot in the field.
Data analysis
Epi Info software version 3.5.1 was used to enter data and the data were analyzed using SPSS version 20. WHO Anthro software was used to analyze HAZ data and it was compared with NCHS reference standard. Crude association was determined with bivariate analysis and a cut-off point of p < 0.25 was used to consider variables for multivariate analysis where confounders were controlled and predictor variables were identified.
Results
Socio-demographic characteristics
The response rate of this study was 90%. From the study participant mothers/caregivers, Majority 299 (87.43%) of the mothers/caregivers were married and 246 (71.93%) were protestant in their religion. About two third 224 (65.50%) of mothers and 183 (53.51%) fathers cannot read and write. About 239 (69.88%) of mothers and 244 (71.34%) of fathers were farmers. More than half 188 (54.97%) of the respondents had a family size of above five. Most 294 (85.97%) of the decision on use of money was made jointly (by husband and wife) (Table 1).
Obstetric, maternal and child morbidity related characteristics
Two third 229 (66.96%) of the children were born at term and majority 272 (79.53%) were born in the health facility. Two hundred fifty seven (75.15%) of the children had a normal birth weight. Forty eight (14.03%) mothers were in the age of < 20 years during their first delivery, 286 (83.63%) mothers had ANC follow up, 263 (76.90%) of the mothers did not take any additional meal than usual during their pregnancy and half 172 (51.30%) of the mothers did not use any type of family planning. More than one fourth 89 (26.02%) of the children had diarrheal morbidity in 2 weeks prior to this study, 23 (6.73%) had fever and 20 (5.85%) had cough during the study period (Table 2).
Child caring practice and environmental health characteristics
Two hundred and twenty eight (66.67%) of the children were initiated on breastfeeding within 1 hour after birth and nearly all 334 (97.66%) of the children were given colostrums. More than half of the children 195 (57.02%) were commenced on complementary feeding at 6 months of age and 264 (77.19%) eat 3 times a day. Source of drinking water for two hundred sixty nine (78.66%) of the households was protected well/spring. Two hundred forty nine households (72.81%) have latrine and 116 (33.92%) dispose waste in open field (Table 3).
Prevalence of stunting and its predictors
The prevalence of stunting in this study was 24.9%; 7.9% were severely stunted. The odd of being stunted was about three times higher for females (AOR = 2.8; 95% CI: 1.5, 5.3) and seven times higher for children aged 12–23 months (AOR = 7.1; 95% CI: 2.3, 21.9) compared with children 6–11 months. Children born from mother’s who do not use family planning and children with diarrheal morbidity in the last 2 weeks prior to the study had 2.5 times higher chance of being stunted (AOR = 2.5; 95% CI: 1.1,5.7) and (AOR = 2.5; 95% CI: 1.2,5.3). Children from households with an income of 750–1500 ETB and > 1500 ETB had less chance of being stunted. Children who received pre-lacteal feeding had 3.8 times higher chance of being stunted (AOR = 3.8; 95% CI: 1.2–12.2) (Table 4).
Discussion
The prevalence of stunting documented in this study was 24.9%, which is lower than the national prevalence (38%) and the prevalence level of South Ethiopia (39%) [1]. Higher prevalence levels were reported in Eastern Ethiopia (45.8%) [12], Northwest Ethiopia (38.3%) [13], Nigeria (36.7%) [14] and Nepal (38%) [15]. This difference might be because we used NCHS growth standard and those studies used WHO growth standard (which is known to increase the prevalence of under nutrition specially stunting as compared to NCHS growth standard) [16].
Unlike many other study findings, this study documented that the odds of being stunted was higher for females as compared to males. This finding is different from other study findings from Ethiopia, Nigeria, Tanzania and Uganda where males have higher risk of being stunted [14, 17,18,19]. On the other hand, in favor of our finding a study from Eastern Ethiopia reported that females had higher chance of being stunted [20]. This may be due to cultural issues, gender preference and differential feeding practice which neglects girls [21,22,23]. Girls are more likely than boys to experience food insecurity due to selective availability of the limited food for boys than girls in Ethiopia [24]. However, a study in India and Pakistan found no statistically significant association between gender and stunting [25, 26].
We have found that the odd of being stunted was higher for children above 12 months as compared to children 6–11 months. Other similar studies conducted in Nigeria, Ethiopia and Pakistan reported that stunting was significantly associated with age above 12 months [26,27,28,29]. The trend of stunting peaks for each group of children age up to 35 months and then declines for children 36–47 months of age. The possible explanations are when children are becoming mobile; they are exposed to contaminants in water, food and soil and they ingest them. Inappropriate complementary feeding and introducing children directly to household diet is another possible reason.
Children from middle- and high-income households had less chance of being stunted. This was in agreement with similar study findings in Southwest Ethiopia [30], Northwest Ethiopia [28, 31], Tanzania [18], Nigeria [14] and Nepal [30] where children from the poor wealth quintile had higher odds of being stunted compared with children from the rich wealth quintiles. Children from poorest households had a higher risk of being stunted compared to those from middle- and high-income households [18, 27, 31, 32]. Increased income improves dietary diversity, which in turn improves nutrient intake and nutritional status [33]. Poor wealth status also negatively affects household food access, sanitation and availability of improved water sources.
Children born to mothers who do not use family planning methods had a higher odds of being stunted compared to those mothers who use family planning methods. Mothers who do not use family planning will have large family size and a short birth interval. Studies from South and Southwest Ethiopia [30, 34], Northern Ethiopia [35], Mozambique [36] and Ghana [37] documented that children living in large family size had an increased risk of being stunted as compared to those from small family size. The possible explanations are that having large family size affects intra-household availability of resources and child caring practice. Short birth interval also has an adverse effect on child nutrition and quality of care. It also leads to intrauterine growth retardation, preterm birth and low birth weight which in turn lead to stunting.
In consistence with studies from Nigeria, South and Northwest Ethiopia, children with diarrheal morbidity 2 weeks prior to the study had a higher chance of being stunted [14, 19, 38, 39]. Diarrhea results in poor appetite, digestion problem and malabsorption and malnutrition children on the other hand have severe episodes of diarrhea.
We have found that pre-lacteal feeding was a predictor of stunting. This is consistent with a study from Southern and Northern Ethiopia [19, 39, 40]. The plausible reason may be stunted children are less likely to be introduced to complementary feeding at appropriate age [18]. The other likely reason is that pre-lacteal feeding has a negative effect on breastfeeding which in turn places children at higher risk of under-nourishment.
Limitations
This study used cross-sectional data. The estimate might be better representative if a longitudinal follow-up data were used. Certain level of recall bias was expected in age estimate of children; the data collectors used different local events to reduce the recall bias.
Conclusion
The magnitude of stunting in the current study was low. Stunting was significantly associated with being female, age above 12 months, low household income status, mother’s not using family planning and pre-lacteal feeding. Gender-based policies should be enacted in child feeding practice. Interventions should focus on the utilization of family planning and appropriate child caring and feeding practices should be implemented according to the infant and young child feeding recommendations. Water, sanitation and hygiene interventions need to be strengthened to reduce the occurrence of diarrheal morbidity and poverty alleviation interventions should be implemented.
Abbreviations
- ANC:
-
Antenatal care
- AOR:
-
Adjusted odds ratio
- BMI:
-
Body mass index
- CI:
-
confidence interval
- COR:
-
Crudes odds ratio
- ETB:
-
Ethiopian Birr
- HAZ:
-
height-for-age Z-score
- NCHS:
-
National child health
- SD:
-
Standard deviation
- SPSS:
-
statistical package for social sciences
- WHO:
-
World health organization
References
CSA, ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA ICF; 2016.
Notes H. World hunger and poverty facts and statistics; 2016.
Organization WH. Globan Nutrition Report 2014.
Black R, Allen LH, Bhutta ZA, Caulfield LE, Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243–60.
UNICEF. The state of the World’s children 2017.
de Onis M, Dewey KG, Borghi E, Onyango AW, Blossner M, Daelmans B, et al. The World Health Organization's global target for reducing childhood stunting by 2025: rationale and proposed actions. Matern Child Nutr. 2013;9(Suppl 2):6–26.
CSA, Macro O. Ethiopia Demographic and Health Survey 2005. Addis Ababa, Ethiopia, and Calverton, Maryland, USA: Central Statistical Agency and ORC Macro; 2006.
Ethiopia FDRo. National Nutrition Program II. In: Body NNC, editor. Addis Ababa, Ethiopia 2016.
Haile D, Azage M, Mola T, Rainey R. Exploring spatial variations and factors associated with childhood stunting in Ethiopia: spatial and multilevel analysis. BMC Pediatr. 2016;16:49.
Adekanmbi VT, Uthman OA, Mudasiru OM. Exploring variations in childhood stunting in Nigeria using league table, control chart and spatial analysis. BMC Public Health. 2013;13:361.
Woodruff BA, Wirth JP, Bailes A, Matji J, Timmer A, Rohner F. Determinants of stunting reduction in Ethiopia 2000–2011. Matern Child Nutr. 2017 Apr;13:2.
Yisak H, Gobena T, Mesfin F. Prevalence and risk factors for undernutrition among children under five at Haramaya district, Eastern Ethiopia. BMC pediatrics. 2015;15:212.
Motbainor A, Worku A, Kumie A. Stunting is associated with food diversity while wasting with food insecurity among Underfive children in east and West Gojjam zones of Amhara region. Ethiopia PLoS One. 2015;10(8):e0133542.
Akombi BJ, Agho KE, Hall JJ, Merom D, Astell-Burt T, Renzaho AM. Stunting and severe stunting among children under-5 years in Nigeria: a multilevel analysis. BMC Pediatr. 2017;17(1):15.
Dorsey JL, Manohar S, Neupane S, Shrestha B, Klemm RDW, West KP, Jr. Individual, household, and community level risk factors of stunting in children younger than 5 years: Findings from a national surveillance system in Nepal. Matern Child Nutr. 2018 Jan;14(1).
Md O, Onyango AW, Borghi E, Garza C, Yang H. Comparison of the World Health Organization (WHO) child growth standards and the National Center for Health Statistics/WHO integrated reference: implications for child health programmes. Public Health Nutr. 2006;9(7):942–7.
Asfaw M, Wondaferash M, Taha M, Dube L. Prevalence of undernutrition and associated factors among children aged between six to fifty nine months in Bule Hora district, South Ethiopia. BMC Public Health. 2015;15:41.
Chirande L, Charwe D, Mbwana H, Victor R, Kimboka S, Issaka AI, et al. Determinants of stunting and severe stunting among under-fives in Tanzania: evidence from the 2010 cross-sectional household survey. BMC Pediatr. 2015;15:165.
Bukusuba J, Kaaya AN, Atukwase A. Predictors of stunting in children aged 6 to 59 months: a case-control study in Southwest Uganda. Food Nutr Bull. 2017;38(4):542–53.
Ma'alin A, Birhanu D, Melaku S, Tolossa D, Mohammed Y, Gebremicheal K. Magnitude and factors associated with malnutrition in children 6–59 months of age in Shinille Woreda, Ethiopian Somali regional state: a cross-sectional study. BMC Nutr. 2016;2:44.
Koohi-Kamali F. Intrahousehold inequalities and child gender Bias in Ethiopia: policy research working paper 4755. In: Department TWBARPRaEM, editor.2008.
Belachew T, Hadley C, Lindstrom D, Gebremariam A, Michael KW, Getachew Y, et al. Gender differences in food insecurity and morbidity among adolescents in Southwest Ethiopia. Pdiatrics. 2011;127(2):398–405.
Hadley C, Lindstrom D, Tessema F, Belachew T. Gender Bias in the food insecurity experience of Ethiopian adolescents. Soc Sci Med. 2008;66(2):427–38.
Belachew T, Hadley C, Lindstrom D, Gebremariam A, Michael KW, Getachew Y, et al. Gender differences in food insecurity and morbidity among adolescents in Southwest Ethiopia. Pediatrics. 2011;127(2):e398–405.
Deshmukh PR, Sinha N, Dongre AR. Social determinants of stunting in rural area of Wardha, Central India. Med J Armed Forces India. 2013;69(3):213–7.
Adekanmbi VT, Kayode GA, Uthman OA. Individual and contextual factors associated with childhood stunting in Nigeria: a multilevel analysis. Matern Child Nutr. 2013;9(2):244–59.
Mushtaq MU, Gull S, Khurshid U, Shahid U, Shad MA, Siddiqui AM. Prevalence and socio-demographic correlates of stunting and thinness among Pakistani primary school children. BMC Public Health. 2011;11:790.
Derso T, Tariku A, Biks GA, Wassie MM. Stunting, wasting and associated factors among children aged 6-24 months in Dabat health and demographic surveillance system site: a community based cross-sectional study in Ethiopia. BMC Pediatr. 2017;17(1):96.
Hagos S, Hailemariam D, WoldeHanna T, Lindtjorn B. Spatial heterogeneity and risk factors for stunting among children under age five in Ethiopia: a Bayesian geo-statistical model. PLoS One. 2017;12(2):e0170785.
Assefa H, Belachew T, Negash L. Socio-demographic factors associated with underweight and stunting among adolescents in Ethiopia. The Pan African medical journal. 2015;20:252.
Tariku A, Biks GA, Derso T, Wassie MM, Abebe SM. Stunting and its determinant factors among children aged 6-59 months in Ethiopia. Ital J Pediatr. 2017;43(1):112.
Tiwari R, Ausman LM, Agho KE. Determinants of stunting and severe stunting among under-fives: evidence from the 2011 Nepal demographic and health survey. BMC Pediatr. 2014;14:239.
Taruvinga A, Muchenje V, Mushunje A. Determinants of rural household dietary diversity: the case of Amatole and Nyandeni districts, South Africa. Journal of Development and Sustainability. 2013;2(4):2233–47.
Fikadu T, Assegid S, Dube L. Factors associated with stunting among children of age 24 to 59 months in Meskan district, Gurage zone, South Ethiopia: a case-control study. BMC Public Health. 2014;14:800.
Gebregyorgis T, Tadesse T, Atenafu A. Prevalence of thinness and stunting and associated factors among adolescent school girls in Adwa town, North Ethiopia. Int J Food Sci. 2016;2016:8323982.
Cruz LMG, Azpeitia GG, Suarez DR, Rodriguez AS, Ferrer JFL, Serra-Majem L. Factors associated with stunting among children aged 0 to 59 months from the central region of Mozambique. Nutrients. 2017;12:9(5).
Darteh EK, Acquah E, Kumi-Kyereme A. Correlates of stunting among children in Ghana. BMC Public Health. 2014;14:504.
Darsene H, Geleto A, Gebeyehu A, Meseret S. Magnitude and predictors of undernutrition among children aged six to fifty nine months in Ethiopia: a cross sectional study. Archives of Public Health. 2017;75:29.
Teshome B, Kogi-Makau W, Getahun Z, Zeleke G. Magnitude and determinants of stunting in children under- five years of age in food surplus region of Ethiopia: The case of West Gojam Zone 2010.
Tessema M, Belachew T, Ersino G. Feeding patterns and stunting during early childhood in rural communities of Sidama, South Ethiopia. The Pan African medical journal. 2013;14:75.
Acknowledgements
We would like to thank Wolaita Sodo University for ethical clearance, Sodo Zuria office for facilitating the data collection and nurses for data collection and processing.
Funding
The funding for this study was personal cost from investigators.
Availability of data and materials
The data that support the findings of this study are available. Anyone interested can get upon reasonable online request by writing to efifit@yahoo.com.
Author information
Authors and Affiliations
Contributions
SK, EG: Conceived the study, SK, FS, HA, TM, and EG: Participated in the design of the study and performed the statistical analysis, SK, HA, EG: Interpreted the data: HA: Obtained ethical clearance and permission for study: FS: Supervised data collectors: SK, FS, HA, TM, EG: Drafting the article or revisiting it critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We received ethics clearance from the ethical review committee at Wolaita Sodo University in Ethiopia. The committee justified for verbal informed consent since uneducated or less educated caretakers would face difficulty in reading and comprehending the consent form. Thus informed verbal consent was obtained from the study participants. The parents/caretakers also provided consent on behalf of the children.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Dake, S.K., Solomon, F.B., Bobe, T.M. et al. Predictors of stunting among children 6–59 months of age in Sodo Zuria District, South Ethiopia: a community based cross-sectional study. BMC Nutr 5, 23 (2019). https://doi.org/10.1186/s40795-019-0287-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40795-019-0287-6