Abstract
Background
Dietary iron intake is associated with bone metabolism in human and animals. Previous studies have suggested that iron deficiency diminishes bone formation and causes bone loss in rats, however, the detailed mechanisms remain unclear. To clarify the mechanism of the diminishing bone formation in iron deficiency, we examined the renal 25-hydroxyvitamin D3-1α-hydroxylase (1α-hydroxylase) activity and femoral expression of bone formation-related genes in iron-deficient rats.
Methods
Male Wistar rats (n = 18) at 3 weeks of age were divided into three groups of six rats each. Two groups of rats were given free access to a control diet or an iron-deficient diet for 4 weeks. Rats in the third group were pair-fed the control diet, calculated as the mean food intake of the iron-deficient group.
Results
Following the treatment, compared with the control and pair-fed groups, hemoglobin and liver iron concentrations were significantly lower and heart weight was significantly higher in the iron-deficient group. Serum 1,25-dihydroxyvitamin D3 concentration and renal 1α-hydroxylase activity were significantly lower in the iron-deficient group compared with the control and pair-fed groups. Serum osteocalcin concentration and bone mineral density of the femur were also significantly lower in the iron-deficient group compared with the control and pair-fed groups. Furthermore, iron-deficient diet decreased runt-related transcription factor 2, osteocalcin, and type I collagen mRNA expression in the femur.
Conclusions
Our findings indicate that iron deficiency reduces renal 1α-hydroxylase activity, leading to a decreased bone formation in rats.
Similar content being viewed by others
Background
Iron deficiency anemia is an important health problem throughout the world, and several researchers have studied the relationships between dietary iron and bone metabolism in human and animals. In human studies, iron intake was positively associated with bone mineral density (BMD) in postmenopausal women [1, 2]. In rats, bone mineral content (BMC), BMD, and bone strength were reduced in the iron-deficient rats [3, 4]. Therefore, it was concluded that iron deficiency affects not only anemia but also bone metabolism.
Parelman et al. [5] reported that the mineralization of hFOB 1.19 cells treated with deferoxamine, iron-chelating agent, in vitro was decreased [5], while Messer et al. demonstrated that the chronic deferoxamine treatment suppressed osteoblast phenotype development in primary rat calvaria-derived osteoblasts during differentiation [6]. Our previous study showed that iron deficiency decreases BMC, BMD, and bone strength in rats, together with diminishing bone formation [7]. Additionally, we demonstrated that iron deficiency diminishes bone formation rate, which was reflected in a decreased serum 1,25-dihydroxyvitamin D3 concentration in the iron-deficient rats [8]. Therefore, iron deficiency-induced bone loss may be due to the diminished bone formation, though the detailed mechanisms remain unclear. Furthermore, the influence of iron deficiency on the bone formation-related mRNA expression levels in rats have not been investigated.
Iron is a key factor of the enzymes related to bone metabolism. Prolyl and lysyl hydroxylases, which contain iron as a cofactor, play important roles in collagen synthesis [9]. Also, renal 25-hydroxyvitamin D3-1α-hydroxylase (1α-hydroxylase) converts 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D, the active form of vitamin D, and contains iron as a cofactor [10]. Therefore, as a consequence of iron deficiency, these iron-containing enzymes activity may be lowered, and hence metabolic disorder of collagen and vitamin D may occur. In previous studies, researchers hypothesized that abnormal metabolism of collagen and vitamin D might cause bone loss in iron deficiency; however, the detailed mechanisms remain unclear.
The purpose of this study was to clarify the effects of iron deficiency on vitamin D metabolism and bone formation in rats. We investigated renal 1α-hydroxylase activity and bone formation-related mRNA expression levels of the femur in rats fed an iron-deficient diet.
Methods
Experimental design
The experimental design has been previously described [8]. Briefly, male Wistar rats (Clea Japan, Tokyo, Japan) at 3 weeks of age were individually housed in stainless-steel wire-mesh cages and kept under a 12-hour light–dark cycle in a room maintained at 22 °C. Before the study period began, rats were given free access to a control diet for a 3 days. Afterward, rats were randomly divided into three groups of six rats each. Two groups of rats were given free access to the control diet or an iron-deficient diet. Rats in the third group were pair-fed the control diet at the same level of food intake as the iron-deficient group. The control and iron-deficient diets were prepared according to the composition of the AIN-93G diet (Additional file 1: Table S1) [11]. The rats were fed their respective diets and were given free access to deinonized water for 4 weeks. Metabolic cages allowed the urine collection from the experimental animals for 24 h, immediately before sacrifice. For bone histomorphometry, rats were subcutaneously injected with tetracycline hydrochloride (20 mg/kg body weight) and calcein (20 mg/kg body weight) at 5 days and 2 days prior to sacrifice, respectively. On the last day of the experimental period, rats were sacrificed under anesthesia, and blood samples and tissues were collected. Hemoglobin concentration was measured using a part of the blood sample (Hemoglobin B-test Wako, Wako Pure Chemical Industries, Osaka, Japan).
Serum and urine analyses
Serum 1,25-dihydroxyvitamin D3 concentration was measured using 1,25(OH)2 vitamin D ELISA kit (Immundiagnostik AG, Bensheim, Germany). Serum osteocalcin (OC) was measured with Rat Osteocalcin (BGP) ELISA system (GE Healthcare Japan Corporation, Tokyo, Japan). Urinary deoxypyridinoline (DPD) was measured using METRA DPD EIA kit (Quidel, CA, USA), while urinary creatinine was measured by the Jaffe reaction, as previously reported by Lustgarten and Wenk [12]. Urinary DPD was normalized with respect to the urinary creatinine concentration.
Liver and kidney iron concentration measurements
After the sacrifice, livers were perfused with ice-cold 0.9 % NaCl solution via their portal veins until the blood color of the livers disappeared. In order to measure iron concentrations in liver and kidney, these samples were dried, ashed, and afterward demineralized with a 1 mol/l HCl solution. Iron was analyzed by atomic absorption spectrophotometry (A-2000; Hitachi, Ltd., Tokyo, Japan).
Renal 1α-hydroxylase activity
Renal 1α-hydroxylase activity was measured using the modified Vieth et al. [13] and Ishida et al. [14] methods. Right kidney was homogenized in 10 volumes of ice-cold homogenization buffer (250 mmol/l sucrose, 10 mmol/l HEPES, and 10 mmol/l KCl, pH 7.4). The homogenate was centrifuged at 4000 × g at 4 °C for 40 s, and the supernatant was centrifuged at 9000 × g at 4 °C for 20 min. The pellet, which consisted mainly of mitochondria, was resuspended in 10 volumes of ice-cold incubation buffer (125 mmol/l KCl, 20 mmol/l HEPES, and 2 mmol/l MgCl2, pH 7.4), and the protein concentration was measured with Protein Assay Rapid kit (Wako Pure Chemical Industries). The final mitochondrial protein concentration was 3–4 mg/ml. Each tube contained 1.98 ml of mitochondrial suspension and it was pre-incubated at 37 °C for 3 min. Afterward, the reaction was initiated by adding 25 nmol 25-hydroxyvitamin D3 in 0.02 ml of ethanol. The samples were incubated additionally for 10 min, and reaction was stopped by the addition of 0.2 ml 10 % trichloroacetic acid. The 1,25-dihydroxyvitamin D3 concentration in the final solutions was measured using 1,25(OH)2 vitamin D ELISA kit (Immundiagnostik AG). Renal lα-hydroxylase activity was expressed as the level of 1,25-dihydroxyvitamin D3 generated from 25-hydroxyvitamin D3.
Measurements of BMC, area, and BMD of the femur
BMC, area, and BMD of the left femur were measured using the dual-energy X-ray absorptiometry (DEXA; DCS-600EX, Aloka, Tokyo, Japan). BMD was calculated by the BMC of the measured area.
Bone histomorphometry
Bone histomorphometry was performed as described previously [8]. Briefly, the undecalcified second lumbar vertebra were embedded in methyl methacrylate and 5 μm sections were obtained using a microtome. The bone histomorphometry was performed using a semiautomatic image analyzing system (System Supply, Nagano, Japan) and a fluorescent microscope (Optiphot; Nikon, Tokyo, Japan). The area occupied by the trabecular bone was measured on each section. Standard bone histomorphometrical nomenclatures, symbols, and units were used in this study as described in the report of the American Society for Bone and Mineral Research [15].
Isolation of total RNA and real-time PCR
For the extraction of total RNA, the right femur was homogenized using TRIzol reagent (Life Technologies, CA, USA), and total RNA was isolated from the lysate according to the manufacturer’s instructions. The amount and purity of the RNA were assessed using NanoDrop 2000c (Thermo Fisher Scientific, MA, USA). cDNA was synthesized using the High-Capacity RNA-to-cDNA Kit (Applied Biosystems, CA, USA). Real-time PCR was carried out with the TaqMan Gene Expression Master Mix (Applied Biosystems) and TaqMan gene expression assays (Applied Biosystems) for rat runt-related transcription factor 2 (Runx2) (Assay ID: Rn01512298_m1), rat Osterix (Assay ID: Rn02769744_s1), rat alkaline phosphatase (ALP) (Assay ID: Rn01516028_m1), rat OC (Assay ID: Rn00566386_g1), rat type I collagen (Col1a1) (Assay ID: Rn01463848_m1), and rat β-actin (Assay ID: Rn00667869_m1). Real-time PCR reaction was performed using a StepOne Real-Time PCR System (Applied Biosystems), and mRNA expression levels were normalized to β-actin mRNA levels. The value of control group was considered to be 1.00.
Statistical analysis
Results are expressed as the mean ± SE for each group of 6 rats. Following one-way analysis of variance (ANOVA), Fisher’s PLSD test was used to analyze statistically significant differences between the groups. Differences were considered significant when p value was less than 0.05.
Results
Body weight, food intake, and iron deficiency indicators
As previously reported [8], we have shown that final body weight and food intake were significantly lower in the iron-deficient and pair-fed groups compared with the control group, and there were no significant differences in these parameters between the iron-deficient and pair-fed groups (Additional file 1: Table S2). Also, we have showed that iron-deficient diet caused severe anemia, which resulted in a greater decrease in hemoglobin and liver iron concentrations, and in an increase in heart weight.
Bone turnover markers and BMC, area, and BMD of the femur
Similar to our previous study [8], iron deficiency decreased bone formation and resorption, from the results of bone turnover markers (Additional file 1: Table S3). Also, iron-deficient diet decreased BMC, area, and BMD of the femur.
Serum 1,25-dihydroxyvitamin D3 concentration, renal iron concentration, and renal 1α-hydroxylase activity
Serum 1,25-dihydroxyvitamin D3 concentration was significantly lower in the iron-deficient group in comparison with the control and pair-fed groups, and there was no significant difference in the concentration levels between the control and pair-fed groups (Fig. 1). Renal iron concentration and 1α-hydroxylase activity were significantly lower in the iron-deficient group compared with the control and pair-fed groups, and there were no significant differences in these factors between the control and pair-fed groups.
Serum 1,25-dihydroxyvitamin D3 concentration (a), renal iron concentration (b), and 1α-hydroxylase activity (c) of the control (C), iron-deficient (ID), and pair-fed (PF) groups. The data are presented as the mean ± SE for each group of 6 rats. a,bThe different letters denote significant differences (p < 0.05)
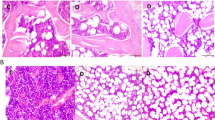
Bone histomorphometry
Bone volume (BV/TV) and mineral apposition rate (MAR) did not differ between the groups (Fig. 2). Mineralizing surface (MS/BS) was significantly lower in the iron-deficient group in comparison with the control and pair-fed groups, and there was no significant difference between the control and pair-fed groups. Compared with the pair-fed group, bone formation rate (BFR/BS) was significantly lower in the iron-deficient group. Osteoblast surface (Ob.S/BS) was significantly lower in the iron-deficient group than in the control group. Osteoclast surface (Oc.S/BS) was significantly lower in the iron-deficient group compared with the pair-fed group. Osteoclast number (N.Oc/BS) tended to be lower in the iron-deficient group compared with the control (p = 0.05) and pair-fed (p = 0.08) groups.
Bone histomorphometric parameters of the lumbar vertebra of the control (C), iron-deficient (ID), and pair-fed (PF) groups. a BV/TV; b MS/BS; c MAR; d BFR/BS; e Ob.S/BS; f Oc.S/BS; g N.Oc/BS. The data are presented as the mean ± SE for each group of 6 rats. a,bThe different letters denote significant differences (p < 0.05)
The expression of the bone formation-related genes in the femur
The expression of Runx2 and OC was demonstrated to be significantly decreased in the iron-deficient group compared with the control and pair-fed groups (Fig. 3). Osterix and ALP mRNA levels were significantly decreased in the iron-deficient and pair-fed groups compared with the control group. Col1a1 mRNA expression was significantly lower in the iron-deficient and pair-fed groups compared with the control group, and tended to be lower in the iron-deficient group compared with the pair-fed group (p = 0.06).
The expression of the bone formation-related genes in the femur of the control (C), iron-deficient (ID), and pair-fed (PF) groups. a Runx2; b Osterix; c ALP; d OC; e Col1a1. The data are presented as the mean ± SE for each group of 6 rats. a,bThe different letters denote significant differences (p < 0.05). The value of the C group is considered as 1.00
Discussion
Our previous studies showed that iron-deficient diet causes a decline in bone formation in rats [7, 8]. Additionally, iron-deficient diet decreased the concentration of serum N-terminal propeptide of type I collagen, which is one of the sensitive bone formation marker in rats [16]. An in vitro study demonstrated that the chronic deferoxamine treatment suppressed bone sialoprotein, ALP, and OC mRNA expression in primary rat calvaria-derived osteoblasts during differentiation [6]. These results support the hypothesis that iron deficiency results in adverse effects on osteoblastic bone formation, which can cause bone loss. In this study, serum OC concentrations were determined to be significantly lower in the iron-deficient group compared with the control and pair-fed groups. Furthermore, bone histomorphometric parameters indicated a decrease in bone formation in rats fed the iron-deficient diet. MS/BS was significantly lower in the iron-deficient group in comparison with the control and pair-fed groups, BFR/BS was significantly lower in the iron-deficient group compared with the pair-fed group, and Ob.S/BS was significantly lower in the iron-deficient group in comparison with the control group. These results suggest that iron deficiency leads to reduced bone formation, which can cause a decline in BMC and BMD in this study, as previously reported [8].
Iron deficiency was related to vitamin D status in humans, and it was known as one of the risk factors for vitamin D deficiency [17]. However, Díaz-Castro et al. reported that no significant difference was observed in circulating 25-hydroxyvitamin D3 concentrations between normal rats and iron-deficient rats [16]. The active form of vitamin D is 1,25-dihydroxyvitamin D3, and in this study, we showed that serum 1,25-dihydroxyvitamin D3 concentrations were significantly lower in the iron-deficient group than in the control and pair-fed groups. This may suggest that iron deficiency resulted in a mild vitamin D deficiency, and these results agree with the results obtained in our previous study [8]. Dietary vitamin D restriction decreased the linear rate of bone mineral apposition in rats [18], and vitamin D receptor knockout mice showed a decrease in bone formation rate [19]. Thus, a lower serum 1,25-dihydroxyvitamin D3 concentration caused by iron deficiency may have led to a decrease in BFR/BS and Ob.S/BS observed in this study.
The conversion from 25-hydroxyvitamin D3 to 1,25-dihydroxyvitamin D3 requires hydroxylation by 1α-hydroxylase in the kidneys. Renal 1α-hydroxylase is located in mitochondria, and contains iron as a cofactor [10]. We speculated that iron deficiency may influence the activity of this enzyme, and consequently, a decline in 1,25-dihydroxyvitamin D3 may cause a decrease in BMC and BMD. Here, renal iron concentration and 1α-hydroxylase activity were significantly lower in the iron-deficient group in comparison with the control and pair-fed groups. These results indicate that iron deficiency decreases renal iron concentration, which further diminishes 1α-hydroxylase activity, leading to a decrease in serum 1,25-dihydroxyvitamin D3 concentration.
During the osteoblast differentiation, Runx2 and Osterix act as essential transcription factors [20, 21], and here we showed that Runx2 mRNA level was significantly decreased in the iron-deficient group compared with the control and pair-fed groups, while Osterix mRNA was significantly lower in the iron-deficient group in comparison with the control group. These results indicate that iron deficiency diminishes Runx2 and Osterix expression, which results in Ob.S/BS decrease. Furthermore, Runx2 regulates the several osteoblastic genes expression, including osteopontin, bone sialoprotein, OC, and Col1a1 [22]. We observed that iron deficiency induces downregulation of OC and Col1a1. We previously showed that iron deficiency might cause abnormal collagen synthesis in rats, resulting from a decrease in hydroxyproline content of the femur [23]. We report here that Col1a1 mRNA expression levels were lower in the iron-deficient group compared with the control group. Downregulation of Col1a1 could be a result of hydroxyproline content decrease observed in the previous study.
Urinary DPD excretion was significantly lower in the iron-deficient group compared with the control and pair-fed groups, Oc.S/BS was significantly lower in the iron-deficient group compared with the pair-fed group, and N.Oc/BS tended to be lower in the iron-deficient group than in the control and pair-fed groups. These results indicate that iron deficiency causes a decrease in bone resorption, which is consistent with the results of our previous study [8]. However, Díaz-Castro et al. reported that iron deficiency increases the serum concentrations of tartrate-resistant acid phosphatase and C-terminal telopeptides of type I collagen in rats [16], which leads to the opposite conclusions about the influence of iron deficiency on bone resorption process. Díaz-Castro et al. reported that hemoglobin concentration of the iron-deficient rats was decreased to ~60 % compared with the control rats. In contrast, this study showed that the hemoglobin concentrations of the iron-deficient group were greatly decreased to ~26 % compared with the control group and to ~24 % compared with the pair-fed group. These results showed that the degree of iron deficiency anemia might have been more severe in the iron-deficient rats of this study than in those of the study of Díaz-Castro et al. [16]. Therefore, we suggest that the differences in bone resorption between our study and the study of Díaz-Castro et al. [16] were caused by the different degrees of anemia, but detailed studies are needed in the future, in order to clarify bone resorption mechanisms resulting from the iron deficiency.
Iron deficiency anemia as severe as in the iron-deficient rats of this study is perhaps rare in human subjects. However, iron deficiency has been one of the risk factors for impaired vitamin D metabolism in humans [17]. Therefore, even in humans, continuous lower iron intake and/or severe iron deficiency may affect vitamin D metabolism, resulting in substantial bone loss. Iron deficiency is an important worldwide health problem and bone disorders such as osteoporosis and osteopenia are also highly prevalent. Thus, our findings might be expected to provide further beneficial information for prevention of bone disorders.
Conclusions
We examined the effects of iron-deficient diet on renal 1α-hydroxylase activity and femoral mRNA expression of bone formation-related genes in rats. Decrease in renal 1α-hydroxylase activity caused a decline in serum 1,25-dihydroxyvitamin D3 levels, which diminished bone formation in iron-deficient rats. Furthermore, iron deficiency-induced downregulation of Runx2 and Osterix may influence osteoblast differentiation.
Abbreviations
1α-hydroxylase, 25-hydroxyvitamin D3-1α-hydroxylase; ALP, alkaline phosphatase; ANOVA, analysis of variance; BFR/BS, bone formation rate; BMC, bone mineral content; BMD, bone mineral density; BV/TV, bone volume; Col1a1, type I collagen; DEXA, dual-energy X-ray absorptiometry; DPD, deoxypyridinoline; MAR, mineral apposition rate; MS/BS, mineralizing surface; N.Oc/BS, osteoclast number; Ob.S/BS, osteoblast surface; OC, osteocalcin; Oc.S/BS, osteoclast surface; Runx2, runt-related transcription factor 2
References
Harris MM, Houtkooper LB, Stanford VA, Parkhill C, Weber JL, Flint-Wagner H, Weiss L, Going SB, Lohman TG. Dietary iron is associated with bone mineral density in healthy postmenopausal women. J Nutr. 2003;133:3598–602.
Maurer J, Harris MM, Stanford VA, Lohman TG, Cussler E, Going SB, Houtkooper LB. Dietary iron positively influences bone mineral density in postmenopausal women on hormone replacement therapy. J Nutr. 2005;135:863–9.
Medeiros DM, Plattner A, Jennings D, Stoecker B. Bone morphology, strength and density are compromised in iron-deficient rats and exacerbated by calcium restriction. J Nutr. 2002;132:3135–41.
Medeiros DM, Stoecker B, Plattner A, Jennings D, Haub M. Iron deficiency negatively affects vertebrae and femurs of rats independently of energy intake and body weight. J Nutr. 2004;134:3061–7.
Parelman M, Stoecker B, Baker A, Medeiros D. Iron restriction negatively affects bone in female rats and mineralization of hFOB osteoblast cells. Exp Biol Med. 2006;231:378–86.
Messer JG, Cooney PT, Kipp DE. Iron chelator deferoxamine alters iron-regulatory genes and proteins and suppresses osteoblast phenotype in fetal rat calvaria cells. Bone. 2010;46:1408–15.
Katsumata S, Tsuboi R, Uehara M, Suzuki K. Dietary iron deficiency decreases serum osteocalcin concentration and bone mineral density in rats. Biosci Biotechnol Biochem. 2006;70:2547–50.
Katsumata S, Katsumata-Tsuboi R, Uehara M, Suzuki K. Severe iron deficiency decreases both bone formation and bone resorption in rats. J Nutr. 2009;139:238–43.
Tuderman L, Myllyla R, Kivirikko KI. Mechanism of the prolyl hydroxylase reaction. 1. Role of co-substrates. Eur J Biochem. 1977;80:341–8.
DeLuca HF. Metabolism of vitamin D: current status. Am J Clin Nutr. 1976;29:1258–70.
Reeves PG, Nielsen FH, Fahey GC. AIN-93 purified diets for laboratory rodents: final report of the American Institute of Nutrition ad hoc writing committee on the reformulation of the AIN-76A rodent diet. J Nutr. 1993;123:1939–51.
Lustgarten JA, Wenk RE. Simple, rapid, kinetic method for serum creatinine measurement. Clin Chem. 1972;18:1419–22.
Vieth R, Fraser D. Kinetic behavior of 25-hydroxyvitamin D-1-hydroxylase and -24-hydroxylase in rat kidney mitochondria. J Biol Chem. 1979;254:12455–60.
Ishida M, Bulos B, Takamoto S, Sacktor B. Hydroxylation of 25-hydroxyvitamin D3 by renal mitochondria from rats of different ages. Endocrinology. 1987;121:443–8.
Parfitt AM, Drezner MK, Glorieux FH, Kanis JA, Malluche H, Meunier PJ, Ott SM, Recker RR. Bone histomorphometry: standardization of nomenclature, symbols, and units. Report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res. 1987;2:595–610.
Díaz-Castro J, López-Frías MR, Campos MS, López-Frías M, Alférez MJ, Nestares T, Ojeda ML, López-Aliaga I. Severe nutritional iron-deficiency anaemia has a negative effect on some bone turnover biomarkers in rats. Eur J Nutr. 2012;51:241–7.
McGillivray G, Skull SA, Davie G, Kofoed SE, Frydenberg A, Rice J, Cooke R, Carapetis JR. High prevalence of asymptomatic vitamin D and iron deficiency in East African immigrant children and adolescents living in a temperate climate. Arch Dis Child. 2007;92:1088–93.
Tam CS, Heersche JN, Jones G, Murray TM, Rasmussen H. The effect of vitamin D on bone in vivo. Endocrinology. 1986;118:2217–24.
Masuyama R, Nakaya Y, Katsumata S, Kajita Y, Uehara M, Tanaka S, Sakai A, Kato S, Nakamura T, Suzuki K. Dietary calcium and phosphorus ratio regulates bone mineralization and turnover in vitamin D receptor knockout mice by affecting intestinal calcium and phosphorus absorption. J Bone Miner Res. 2003;18:1217–26.
Komori T, Yagi H, Nomura S, Yamaguchi A, Sasaki K, Deguchi K, Shimizu Y, Bronson RT, Gao YH, Inada M, Sato M, Okamoto R, Kitamura Y, Yoshiki S, Kishimoto T. Targeted disruption of Cbfa1 results in a complete lack of bone formation owing to maturational arrest of osteoblasts. Cell. 1997;89:755–64.
Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, Behringer RR, de Crombrugghe B. The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell. 2002;108:17–29.
Ducy P, Zhang R, Geoffroy V, Ridall AL, Karsenty G. Osf2/Cbfa1: a transcriptional activator of osteoblast differentiation. Cell. 1997;89:747–54.
Matsumoto N, Katsumata S, Uehara M, Suzuki K. Effect of dietary iron deficiency on femoral hydroxyproline content in rats. J Clin Biochem Nutr. 2008;43 Suppl 1:582–5.
Acknowledgments
The authors thank Dr. Yoshiko Ishimi (National Institute of Health and Nutrition, Tokyo, Japan) for support in measuring BMC, area, and BMD of the femur.
Funding
This work was partially supported by KAKENHI (Grant-in-Aid for Young Scientists (B), 20700598).
Availability of data and materials
All the data supporting our findings is in the manuscript and Additional file 1.
Authors’ contributions
SK and MU conceived and designed the study. Substantial contributions to acquisition, analysis, and interpretation of data were made by SK, RK, NM, HI, and NT. SK drafted the manuscript and MU revised it. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Tokyo University of Agriculture Animal Use Committee approved this study, and this study was undertaken in accordance with the university guidelines for the care and use of laboratory animals.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
Composition of the experimental diets. Table S2. Body weight, food intake, hemoglobin, heart weight, and liver iron concentration. Table S3. Bone turnover markers and BMC, area, and BMD of the femur. (DOC 32 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Katsumata, S., Katsumata, R., Matsumoto, N. et al. Iron deficiency decreases renal 25-hydroxyvitamin D3-1α-hydroxylase activity and bone formation in rats. BMC Nutr 2, 33 (2016). https://doi.org/10.1186/s40795-016-0072-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40795-016-0072-8